The quality of CPR and chest compressions are key factors for survival from cardiac arrest.1 Over the past 50 years, there has been a progressive increase in the recommended rate of chest compressions during CPR.
In 1960, the recommended rate was 60 compressions/ minute; this increased to at least 100 compressions/ minute in the latest guidelines from the American Heart Association (AHA) in 2010.1–4 However, guidance is not provided for a maximum chest compression rate.
In this article, I’ll review key studies and gaps in our knowledge about chest compression rate, including the study recently published in the journal Circulation and how it can be used to guide clinical practice.5 I’ll also review what further studies need to be done regarding chest compression rate and quality of CPR in general.
One of the most fundamental things that we have learned from research over the past 10 years is that survival from out-of-hospital cardiac arrest depends mostly on the quality of BLS (including defibrillation) that is given in the field before the patient arrives at a hospital. In Dallas-Fort Worth, and at least one other Resuscitation Outcomes Consortium (ROC) site, less than 1% of patients who are not resuscitated in the field will leave the hospital alive.

The recommended rate of chest compressions during CPR has increased over the past 50 years, but recent research shows that we must also consider the ideal maxmium rate and avoid exceeding 125 compressions/minute.
DISCOVERING THE QUESTION
The AHA and the International Liaison Committee on Resuscitation (ILCOR) jointly review guidelines for CPR every five years to determine if new science published since the last review provides evidence strong enough to justify changing a guideline or adding a new guideline.
In 2006, AHA and ILCOR asked me and two other investigators to review the guideline for chest compression rate during CPR in preparation for the 2010 CPR Consensus on Science Conference (the last CPR guidelines had been published in 2005).
I began the review of chest compression rates by searching for appropriate articles in such databases as PubMed and repeated it several times until November 2009. The final review included 22 articles that were a variety of human, animal and manikin studies, few of which tested different chest compression rates. The studies showed that when compression rates of EMS providers were measured in the prehospital setting, the rates were faster than 100 compressions/minute, generally averaging about 110–120 compressions/minute.
Animal studies showed that blood flow and survival increased with faster chest compression rates.6–10 Some studies compared 60 with 120 compressions/minute and some compared 60, 100, 120 and 150 compressions/ minute. These studies showed better blood flow occurred at 120–150 compressions/minute. One animal survival study compared 60 and 120 compressions/ minute and found greater survival with the faster rate.8
Two human studies compared 80 with 120 compressions/minute. 11,12 These studies found improved blood flow and pressure, or increased end-tidal carbon dioxide levels (an indirect measure of blood flow), with the faster rate.
In summary, these studies provided consistent evidence for improved blood flow at rates of 120–150 compressions/minute. However, this is only indirect evidence regarding optimal rates because none of the studies observed the influence of chest compression rates on return of spontaneous circulation (ROSC), or survival, in humans.
The bottom line: This was a huge gap in the scientific literature of resuscitation for something as fundamental as chest compression rates during CPR.
Identifying gaps in scientific knowledge is one of the functions of the guideline review process, so that investigators can be directed to important areas of future research. The review prompted me to take up the question: What is the ideal chest compression rate range (low and high) for survival?
METHODS
Fortunately, as an investigator in the ROC, I was in a position to do something about it. The ROC is a network of regional research centers that are focused on two main problems: severe traumatic injury and non-traumatic cardiac arrest. The regional research sites include:
Birmingham, Ala.
Dallas-Fort Worth
Milwaukee
Pittsburgh
Portland, Ore.
San Diego
Seattle-King County
Ottawa, Ontario
Toronto, Ontario
Vancouver, British Columbia
The ROC maintains a registry for cardiac arrest that was started in December 2005 and continues today. The registry enrolls about 22,000 out-of-hospital cardiac arrest cases annually. Such patients receive CPR by paramedics and firefighters and are then often transported to a hospital. The registry data starts with the 9-1-1 call and ends with vital status at the time of hospital discharge, including in-hospital data.13,14
Most importantly for my study, the registry collects data from electronic files that defibrillator-monitors record during CPR. These files record chest compressions, shocks, and interruptions in chest compression and some also record the depth of each chest compression, ventilation, and end-tidal carbon dioxide.15 The files are a detailed record of the entire resuscitation and are the next best thing to actually being there (possibly better than being there because of the detailed second-to-second measurements found in these files).
These files have provided crucial data that has been used in a number of studies regarding various aspects of CPR, including chest compression rates, which collectively can be termed “quality of CPR” studies.16,17
Our study of chest compression rates included more than 3,000 adult patients from ROC sites in the U.S. and Canada who had out-of-hospital cardiac arrest and CPR provided by EMS rescuers (firefighters and paramedics). All of the study patients had electronic recordings of chest compressions available.5
The study included data from the first five minutes of CPR; this data was analyzed using a logistic regression model.18 The model adjusted for the following factors that are known to affect outcome:
Age
Sex
First known rhythm
Witnessed cardiac arrest
Bystander CPR
Location (home vs. public)
These factors are also called Utstein predictors and should be used in most cardiac arrest studies where outcome is an end-point.
The model also adjusted for ROC site. Chest compression rate was measured only during intervals when chest compressions were being performed and excluded intervals in which there was a pause in chest compressions.
Average patient age was 67 years; 1,082 had ROSC (35%) and 265 (8.6%) survived to hospital discharge. The study found that the average chest compression rate used by EMS providers across ROC sites was 112 compressions/ minute. One-third of patients received a rate greater than 120/minute, and 7% had a rate greater than 140/minute. Remarkably, we measured rates up to 180 compressions/ minute at many sites.
SIGNIFICANT RESULTS
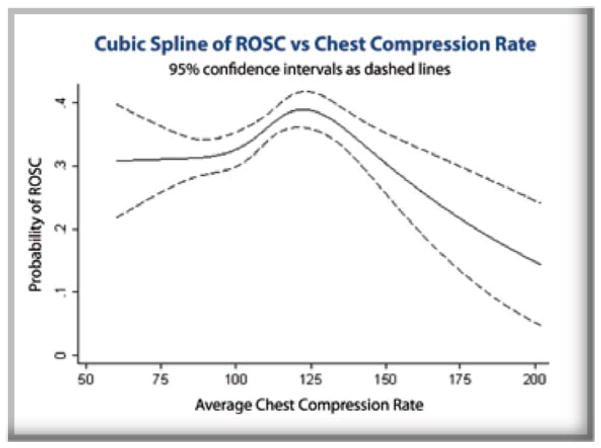
We found that ROSC peaked at a chest compression rate of about 125 compressions/ minute and then declined sharply at higher rates (Figure 1). In addition, survival-to-hospital discharge also peaked between 100–120 compressions per minute and then declined at faster rates, although this was not statistically significant after adjustment for the covariates listed above (Figure 2).
Figure 1.
Unadjusted cubic spline of the relationship between chest compression rates (x-axis) and the probability of return of spontaneous circulation (ROSC) (y-axis).
Figure 2.
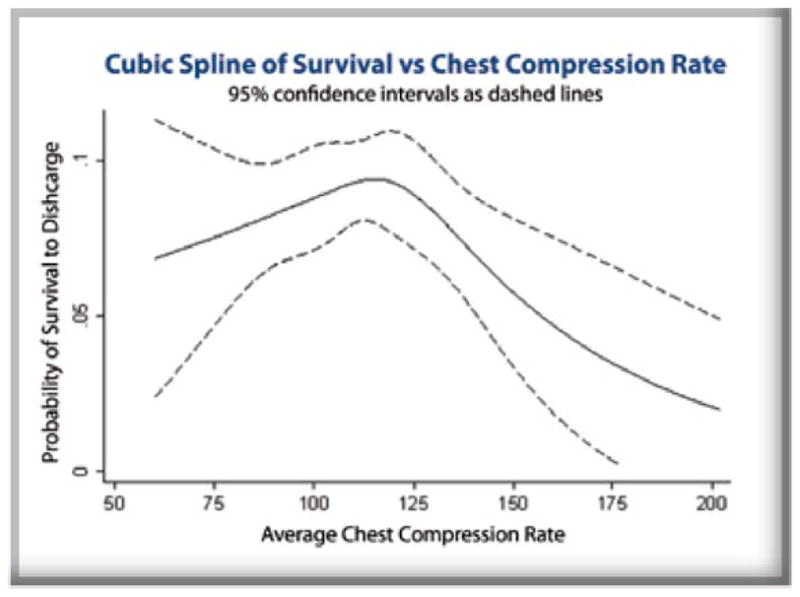
Unadjusted cubic spline of the relationship between chest compression rates (x-axis) and the probability of survival to hospital discharge (y-axis).
Another important finding: Chest compression depth became less as chest compression rates became faster, especially with rates above 140/minute. Adequate depth of chest compressions is thought to be a very important determinant of outcome from cardiac arrest; so loss of depth at high compression rates may be one mechanism accounting for the decreased success of resuscitation.
Two principal mechanisms are thought to be responsible for producing blood flow during external chest compression: direct cardiac compression and increased intrathoracic pressure.19,20 In either case, forward blood flow depends on venous blood filling the heart or lungs during diastole or the release phase of external chest compression. If this phase is too brief, blood available for forward flow during the compression phase will be limited.
Such mechanisms may account for findings in animal models and in the present study that 120 compressions/ minute is a rate that appears to be optimal for blood flow as well as for survival, but that rates faster than 120/minute are associated with decreased blood flow and survival.
Implicit in the guidance for rescuers to “push hard, push fast” may be the belief that rescuers don’t push fast enough. That they don’t push hard enough has been documented in a number of studies. However, at least for professional rescuers, the tendency is to push too fast. This tendency may be because of the surge of adrenaline and excitement that occurs during a code, but may also be a function of the elastic properties of the human chest, which makes higher chest compression rates feel more natural to the rescuer.
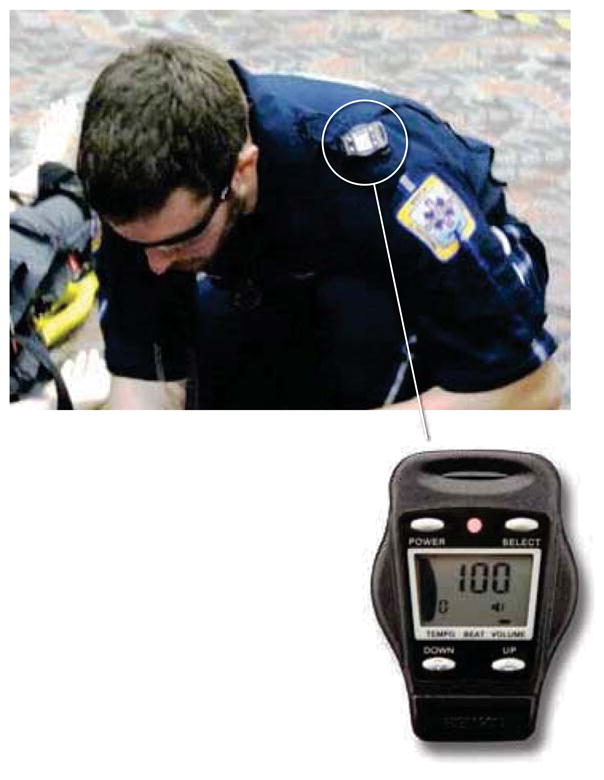
Above: Metronomes can help EMS providers maintain a correct chest compression rate.
Right: The 2010 American Heart Association Guidelines for CPR and ECCU set a minimum of 100 compressions per minute.
This phenomenon may be similar to the natural bounce frequency of a trampoline. Thus, compressing the chest at a frequency of 100–120 compressions/minute may require a conscious effort to counteract higher compression rates that seem more natural.
Metronome devices that emit a tone can be set to a desired rate to provide guidance during chest compression. Metronomes have been found useful as an aide to maintain correct chest compression rate.21
We have used metronomes in Dallas EMS agencies with great success. We measured chest compression rates for several years and found it to average about 135 compressions/minute.
After we introduced metronomes on all EMS AEDs and monitor-defibrillators, the average rate decreased to 107 compressions/minute, a rate that’s right in the middle of the cardiac compression “sweet spot.” This improvement in chest compression rates and other aspects of basic CPR coincided with a substantial increase in survival rates in Dallas.
Moreover, we have been teaching lay rescuers to use the song “row, row, row your boat, gently down the stream” (first proposed by my colleague Ray Fowler, MD) as an aide to help maintain the proper chest compression rate. Almost everyone knows this song and we have found that it aids in calming some rescuers during a stressful event, such as cardiac arrest.
FUTURE STUDIES
This compression range study should be repeated with a larger number of patients with data from electronic CPR files to determine if chest compression rate is significantly associated with survival to hospital discharge. A study with su$cient power to determine optimal chest compression depth for survival should be also be conducted.
Optimal chest compression rates may also differ depending on whether manual compression is performed or whether a mechanical chest compression device or a device that affects circulation during chest compression is used. Such devices should be studied to determine optimal chest compression rates.
Studies addressing the following questions are also needed: When should ventilation be started during CPR, and how much ventilation is needed to improve survival to hospital discharge?
CONCLUSION
Although additional studies are needed, this study shows that the likelihood of ROSC after out-of-hospital cardiac arrest was greatest with use of chest compression rates between 100–120 compressions/minute and ROSC declined when compression exceeded 125 compressions/minute.
Acknowledgments
We are indebted to the firefighters and paramedics participating in the ROC for their hard work and dedication. We would also like to thank the data coordinators at each ROC site for their extraordinary diligence and focus in abstracting the data for this study. Finally, I would like to thank Danielle Guffey, BS, and Siobhan Brown, PhD, who performed the statistical analyses in this study.
FUNDING SOURCES
This study was supported by a series of cooperative agreements to 10 regional clinical centers and one Data Coordinating Center:
5U01 HL077863-University of Washington Data Coordinating Center
HL077865-University of Iowa
HL077866-Medical College of Wisconsin
HL077867 University of Washington
HL077871 -University of Pittsburgh
HL077872-St. Michael’s Hospital
HL077873-Oregon Health and Science University
HL077881-University of Alabama at Birmingham
HL077885-Ottawa Health Research Institute
HL077887-University of Texas Southwestern Medical Center at Dallas
HL077908-University of California San Diego
Other cooperative agreements include:
National Heart, Lung and Blood Institute in partnership with the National Institute of Neurological Disorders and Stroke
American Heart Association
U.S. Army Medical Research & Materiel Command
Canadian Institutes of Health Research - Institute of Circulatory and Respiratory Health
Heart, Stroke Foundation of Canada
Defence Research and Development Canada
Footnotes
Disclosure: Idris is an unpaid consultant for Philips Healthcare and a volunteer for the National Emergency Cardiovascular Care Committee of the American Heart Association. He receives grant funding from the National Heart, Lung, and Blood Institute, National Institutes of Health.
References
- 1.Berg RA, Hemphill R, Abella BS, et al. Part 5: Adult basic life support. 2010 American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2010;122(suppl 3):S685–S705. doi: 10.1161/CIRCULATIONAHA.110.970939. [DOI] [PubMed] [Google Scholar]
- 2.Kouwenhoven WB, Jude JR, Knickerbocker GG. Closed-chest cardiac massage. JAMA. 1960;173(10):1064–1067. doi: 10.1001/jama.1960.03020280004002. [DOI] [PubMed] [Google Scholar]
- 3.Cardiopulmonary resuscitation: Statement by the Ad Hoc Committee on Cardiopulmonary Resuscitation of the Division of Medical Sciences, National Academy of Sciences— National Research Council. JAMA. 1966;198:138–145. [Google Scholar]
- 4.Standards and guidelines for cardiopulmonary resuscitation (CPR) and emergency cardiac care (ECC) JAMA. 1986;255(21):2905–2984. [PubMed] [Google Scholar]
- 5.Idris AH, Guffey D, Aufderheide TP, et al. Resuscitation Outcomes Consortium Investigators. The relationship between chest compression rates and outcomes from cardiac arrest. Circulation. 2012;125(24):3004–3012. doi: 10.1161/CIRCULATIONAHA.111.059535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Harris LC, Kirimli B, Safar P. Ventilation-cardiac compression rates and ratios in cardiopulmonary resusucitation. Anesthesiology. 1967;28(5):806–813. doi: 10.1097/00000542-196709000-00006. [DOI] [PubMed] [Google Scholar]
- 7.Maier GW, Tyson GS, Jr, Olsen CO, et al. The physiology of external cardiac massage: highimpulse cardiopulmonary resuscitation. Circulation. 1984;70(1):86–101. doi: 10.1161/01.cir.70.1.86. [DOI] [PubMed] [Google Scholar]
- 8.Feneley MP, Maier GW, Kern KB, et al. Influence of compression rate on initial success of resuscitation and 24 hour survival after prolonged manual cardiopulmonary resuscitation in dogs. Circulation. 1988;77(1):240–250. doi: 10.1161/01.cir.77.1.240. [DOI] [PubMed] [Google Scholar]
- 9.Fitzgerald KR, Babbs CF, Frissora HA, et al. Cardiac output during cardiopulmonary resuscitation at various compression rates and durations. Am J Physiol. 1981;9;241(3):H442–H448. doi: 10.1152/ajpheart.1981.241.3.H442. [DOI] [PubMed] [Google Scholar]
- 10.Wolfe JA, Maier GW, Newton JR, et al. Physiologic determinants of coronary blood flow during external cardiac massage. J Thorac Cardiovasc Surg. 1988;95(3):523. [PubMed] [Google Scholar]
- 11.Swenson RD, Weaver WD, Niskanen RA, et al. Hemodynamics in humans during conventional and experimental methods of cardiopulmonary resuscitation. Circulation. 1988;78(3):630–639. doi: 10.1161/01.cir.78.3.630. [DOI] [PubMed] [Google Scholar]
- 12.Kern KB, Sanders AB, Raife J, et al. A study of chest compression rates during cardiopulmonary resuscitation in humans. The importance of rate-directed chest compressions. Arch Int Med. 1992;152(1):145–149. [PubMed] [Google Scholar]
- 13.Davis DP, Garberson LA, Andrusiek DL, et al. A descriptive analysis of Emergency Medical Service Systems participating in the Resuscitation Outcomes Consortium (ROC) network. Prehosp Emerg Care. 2007;11(4):369–382. doi: 10.1080/10903120701537147. [DOI] [PubMed] [Google Scholar]
- 14.Morrison LJ, Nichol G, Rea TD, et al. Rationale, development and implementation of the Resuscitation Outcomes Consortium Epistry-Cardiac Arrest. Resuscitation. 2008;78(2):161–169. doi: 10.1016/j.resuscitation.2008.02.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Stecher FS, Olsen JA, Stickney RE, et al. Transthoracic impedance used to evaluate performance of cardiopulmonary resuscitation during out of hospital cardiac arrest. Resuscitation. 2008;79(3):432–437. doi: 10.1016/j.resuscitation.2008.08.007. [DOI] [PubMed] [Google Scholar]
- 16.Wik L, Kramer-Johansen J, Myklebust H, et al. Quality of cardiopulmonary resuscitation during out-of-hospital cardiac arrest. JAMA. 2005;293(3):299–304. doi: 10.1001/jama.293.3.299. [DOI] [PubMed] [Google Scholar]
- 17.Christenson J, Andrusiek D, Everson-Stewart S, et al. Resuscitation Outcomes Consortium Investigators. Chest compression fraction determines survival in patients with out-of hospital ventricular fibrillation. Circulation. 2009;120(13):1241–1247. doi: 10.1161/CIRCULATIONAHA.109.852202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chambers JM, Hastie T. Statistical Models in S. Pacific Grove, Calif: Wadsworth & Brooks/ Cole Advanced Books & Software; 1992. [Google Scholar]
- 19.Weisfeldt ML, Chandra N. Physiology of cardiopulmonary resuscitation. Annu Rev Med. 1981;32:435–442. doi: 10.1146/annurev.me.32.020181.002251. [DOI] [PubMed] [Google Scholar]
- 20.Halperin HR, Tsitlik JE, Guerci AD, et al. Determinants of blood flow to vital organs during cardiopulmonary resuscitation in dogs. Circulation. 1986;73(3):539–550. doi: 10.1161/01.cir.73.3.539. [DOI] [PubMed] [Google Scholar]
- 21.Fletcher D, Galloway R, Chamberlain D, et al. Basics in advanced life support: A role for download audit and metronomes. Resuscitation. 2008;78(2):127–134. doi: 10.1016/j.resuscitation.2008.03.003. [DOI] [PubMed] [Google Scholar]