Abstract
Background
Degenerative lumbar spinal stenosis is increasingly being diagnosed in persons over age 65. In 2011, 55 793 older people with this condition were treated as inpatients in German hospitals. Among physicians, there is much uncertainty about the appropriate treatment strategy.
Method
Selective literature review
Results
Lumbar spinal stenosis in older people is characterized by spinal claudication and neurological deficits. A precise clinical history and physical examination and ancillary radiological studies are the necessary prerequisites for treatment. Magnetic resonance imaging is the radiological study of choice. Conservative treatment consists of physiotherapy, drugs, and local injections; various surgical treatments can be considered, depending on the severity of the problem. The main purpose of surgery is to decompress the spinal canal. If the lumbar spine is demonstrably unstable, an instrumented fusion should be performed in addition. There is, however, only moderately good evidence supporting the superiority of surgery over conservative treatment. In a prospective study, the complication rate of purely decompressive surgery was found to be 18%. The utility of the current operative techniques cannot be definitively assessed, because they are applied to a wide variety of patients in different stages of the disease and at different degrees of severity, and the reported results are thus not comparable from one trial to another.
Conclusion
No evidence-based recommendation on the diagnosis and treatment of lumbar spinal stenosis in older people can be formulated at present because of the lack of pertinent randomized trials.
Because of the aging of the population, neurosurgeons, orthopedists, trauma surgeons, and spine surgeons are now increasingly confronted with a very wide variety of degenerative changes of the lumbar spine. The treatment of symptomatic lumbar spinal stenosis is surely among the major clinical challenges of this kind. As the available scientific evidence on the diagnosis and treatment of this entity is not very reliable (1, 2), there is no currently valid overall assessment of treatment strategies for older patients (i.e., persons over age 65).
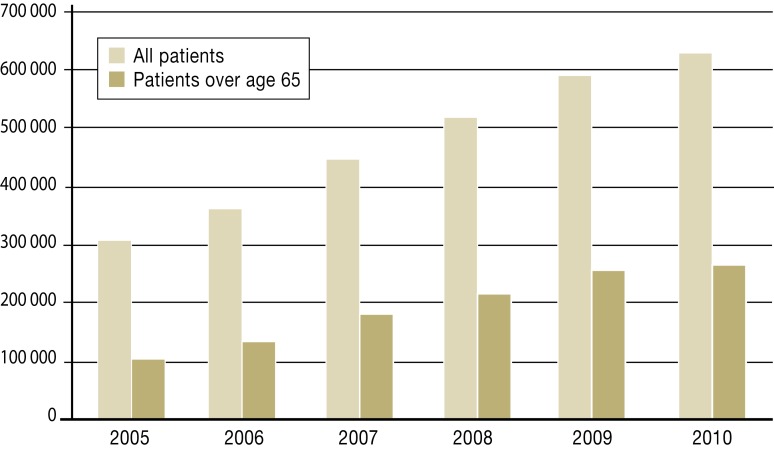
Not only do older people make up a higher percentage of the population than before; there has also been a disproportionate rise in the frequency of lumbar spinal surgery in this age group (3) (Figure 1). The precise nature of this rise is hard to determine, however, because of the broad range of spinal procedures that are performed, with widely varying degrees of complexity. In 2005, lumbar spinal stenosis (ICD-10 code M48.06) was given as the main admitting diagnosis of 28 001 hospitalized patients over age 65 in Germany. By 2011, this figure had more than doubled, to 55 793 (3).
Figure 1.
The number of
spinal operations performed annually in Germany from 2005 to 2010. Overall increase, 105%; increase in persons over age 65, 162%.(Source: Federal Statistical Office, Bonn)
Osteoporosis and other typical spinal problems of advanced age, multiple comorbidities, and the lessened physical performance that goes along with age are now accompanied, at least as far as our experience suggests, by markedly heightened expectations on the part of our older patients. Thus, the value of different treatment strategies needs to be rationally assessed. In this article, we ask what the existing scientific evidence tells us about the current methods of diagnosis and treatment of symptomatic lumbar spinal stenosis in older people. Possible treatment strategies are indicated.
Spinal stenosis.
Neurosurgeons, orthopedists, trauma surgeons, and spine surgeons are now increasingly confronted with a very wide variety of degenerative changes of the lumbar spine.
Learning objectives
The goal of this article is to acquaint readers with
the specific therapeutic situation of spinal stenosis in older people,
the pathophysiology, clinical manifestations, and clinical course of the condition,
conservative treatment options, and
the different operations that can be performed for this disease and the risks associated with each.
The prevalence of degenerative lumbar spinal changes.
Degenerative changes of the lumbar spine that are visible by MRI become more common with age and are present in nearly 100% of persons over age 60 (4).
Methods
This article is based on a comprehensive, selective literature search in the main medical databases (Medline, Ovid, Cochrane Library, Web of Sciences), with particular attention to clinical trials, randomized controlled trials, reviews, and meta-analyses and to the search terms “lumbar spinal stenosis,” “lumbar degenerative spine disease,” “lumbar degenerative spondylolisthesis,” and “spinal spondylosis.”
The prevalence of lumbar spinal stenosis.
By radiological criteria alone, 21% of all persons over age 60 have lumbar spinal stenosis.
Definition and pathogenesis
Even the definition of “lumbar spinal stenosis” is problematic. The term, standing alone, is a morphological description of imaging findings (anteroposterior [AP] diameter by computed tomography [CT] of less than 10 mm); it has no pathological significance in itself. Degenerative changes of the lumbar spine that are visible on magnetic resonance imaging (MRI) become more common with age and are present in nearly 100% of persons over age 60 (4). By radiological criteria alone, 21% of all persons over age 60 have lumbar spinal stenosis (5). The main radiological criteria for spinal stenosis are bony narrowing, obliteration of epidural fat, and deformities of the spine in the sagittal and frontal imaging planes.
The main cause of lumbar spinal stenosis is progressive segmental degeneration. From a patho-anatomical and pathophysiological point of view, disc degeneration is presumed to lead to loss of segmental height, with disc protrusion and ensuing narrowing of the spinal canal. The loss of segmental height also narrows the neural foramina and causes increasing protrusion of the dorsal ligamentous structures into the spinal canal. The altered biomechanical situation promotes progressive arthrosis of the intervertebral joints. Reactive hypertrophy of the ligamenta flava additionally narrows the spinal canal and the lateral recesses, so that, in the end, the spinal canal is hemmed in on all sides. Progressive changes of these kinds can bring about a secondary degenerative instability with the development of a pseudo-spondylolisthesis, i.e. a chronic degenerative slippage of the vertebral bodies, which narrows the spinal canal still further. Disc degeneration also promotes the formation of secondary curvatures in the frontal plane, leading to (for example) rotational slippage or a multisegmental deformity. A role for vascular factors in the pathophysiological process has been proposed, but not yet proved (6).
Clinical manifestations
Lumbar spinal stenosis typically manifests itself clinically in spinal claudication, a symptom complex including exercise-related pain in the back and sometimes radicular, but more often pseudoradicular radiation of pain into the lower limbs. As the condition progresses, neurological deficits can arise in the lower limbs, including autonomic disturbances. The symptoms are typically worst when the patient walks in a body posture with marked lumbar lordosis, e.g., when the patient walks downhill; conversely, they are less severe when the lumbar spine is kyphotic, e.g., when the patient walks uphill or rides a bicycle. A further typical feature is that the older person stoops forward while walking. This can be thought of as a compensatory measure for the narrowing of the spinal canal (7).
Particularly in older people, the clinical picture may be blurred by accompanying illnesses. For example, it has been reported that 26% of elderly patients with lumbar spinal stenosis also have peripheral arterial occlusive disease (PAOD) (8), and a comparable percentage suffers from coxarthrosis (9). Meanwhile, a study from the Far East suggests that 100% of over 70-year-old patients with lumbar stenosis have either osteoporosis or osteopenia, although this finding clearly cannot be directly applied to the Central European population without further study (10). Potential differential diagnoses are listed in Box 1, the more common ones in boldface type. Patients (particularly older ones) often present with mixed clinical pictures that complicate diagnostic assessment and treatment planning.
Box 1. The differential diagnosis of spinal claudication.
vascular claudication (peripheral arterial occlusive disease, PAOD)
lumbar disc herniation
coxarthrosis and/or gonarthrosis
somatization disorder
cervical and/or thoracic spinal stenosis
metabolic or inflammatory neuropathy
osteoporotic compression fracture
spinal infections, tumors, or status post osteoporotic fracture
myelopathy
vascular cerebral or spinal processes
spinal deformity
myopathy
systemic diseases of the nervous system
chronic inflammatory diseases of the central nervous system (borreliosis, multiple sclerosis)
necrosis of the femoral head
non-dislocated fracture of the femoral neck
retroperitoneal or pelvic process affecting the lumbosacral plexus
peripheral angiopathy or thrombosis
aneurysm
The commonest differential diagnoses are given in boldface type
Diagnostic evaluation
History
Precise history-taking from patients with degenerative spinal diseases is very important, never more so than in the older patient. A sensible treatment can only be proposed when the clinical situation and the imaging findings are jointly considered. Specific history-taking should include the catalogue of questions and investigations that is given in Box 2.
Box 2. Questions and tests for the clinical history and physical examination.
-
General examination
stooped gait? hip mobility? flexion contracture of hip?
-
Pain
onset, duration, site, exercise dependence, maximum walkable distance?
Pain on leaning backward? Pain on foraminal occlusion test?
-
Paresis and/or hypesthesia
onset, duration, site, exercise dependence, reflexes?
-
Autonomic disturbances
bladder and bowel problems? fever?
-
Past medical history
trauma? cancer? degenerative disease of the spine? peripheral vascular disease? diabetes? cardiovascular disease? cerebrovascular disease? osteoporosis?
Clinical manifestations.
Lumbar spinal stenosis typically manifests itself clinically in spinal claudication, a symptom complex including exercise-related pain in the back and sometimes radicular, but more often pseudoradicular radiation of pain into the lower limbs.
Common differential diagnoses.
Vascular claudication, lumbar disc herniation, cox-/gonarthrosis, somatization disorder, cervical/thoracic spinal stenosis, neuropathy, osteoporotic compression fracture, spinal infections & tumors
Physical examination
The comprehensive physical examination should include a symptom-directed examination, a general physical examination (pedal pulses, pain on hip rotation, and further tests), and a thorough neurological examination. The possibility of accompanying systemic diseases of the nervous system—including old or recent stroke—should be considered and actively sought. Particularly when advanced degenerative changes are found in the lumbar spine, clinically relevant cervical spinal stenosis must be ruled out, as this can cause overlapping symptoms.
Especially in surgical candidates, a psychological evaluation is indicated as well. A psychopathological component may turn out to be an (accessory) cause of the patient’s symptoms.
Clinical history.
general examination, past medical history
pain?
pain leaning backward / in foramen-occlusion test?
paresis, hypesthesia?
autonomic disturbances?
Imaging studies
Imaging studies are indispensable for diagnostic evaluation and treatment planning in symptomatic patients. There are many morphometric methods for the description of the spinal canal. Such terms as absolute and relative spinal stenosis are defined by purely radiological criteria and lack any clinical correlation in themselves. They thus convey no more than auxiliary information to be considered in treatment planning.
Lumbar MRI is the standard procedure for the demonstration of stenosis and cauda equina compression. As reported in the literature, its sensitivity is 87% to 96% and its specificity is 68% to 75% (11). As a rule, T1- and T2-weighted images should be obtained in both the sagittal and the transverse planes. It is now possible for MRI to be performed with the patient standing upright; this type of study will be increasingly useful in the future, as it enables visualization of the patho-anatomical changes that come about under axial loading.
Plain films of the lumbar spine can yield clues to the origin of exertional back pain and demonstrate degenerative changes. They should be obtained with the patient standing upright, because the pathological changes in the frontal and sagittal views are visible only under axial loading. When these changes are found, views of the entire spinal column in the standing position must be obtained in order to detect any instability due to the abnormal static conditions. In recent years, the role of functional x-ray studies has declined. Conventional films often reveal plentiful evidence of osteoporotic changes that need further work-up.
Lumbar CT may be useful for the assessment of bone condition and potential osteoporosis with a view toward the planning of surgery. If the use of implants is under consideration and osteoporosis is suspected, then either dual x-ray absorptiometry (DEXA) or a quantitative CT (qCT) should be performed. On the other hand, lumbar myelography with post-myelographic CT should now only be performed in exceptional cases. The main indications for this invasive study are the presence of metal implants in the lumbar spine that would make MRI uninterpretable because of artefacts, the need for dynamic assessment, and any residual diagnostic uncertainty after the relevant non-invasive tests have been performed.
Electrophysiological studies
Electrophysiological studies are mainly useful in that they can reveal potential differential diagnoses, e.g., spinal cord lesions or systemic disorders of the nervous system, but they may also help identify the segment that requires treatment when the patient presents with diffuse, multisegmental symptoms. The performance and interpretation of such studies are often complicated by coexisting non-pathological changes of advanced age, such as loss of the somatosensory evoked potential (SEP) of the tibial nerve, and/or by common age-related pathological conditions, such as diabetes mellitus and polyneuropathy affecting the tibial nerve.
Imaging studies.
Lumbar MRI is the gold standard for the demonstration of stenosis and cauda equina compression.
Further diagnostic evaluation
Further ancillary testing may be needed to rule in or out the various differential diagnoses mentioned above. When PAOD is suspected, the test that is generally performed is Doppler-assisted measurement of the ankle-brachial index (ABI). Degenerative or traumatic diseases of the hips and pelvis need further radiological evaluation. Laboratory tests can help rule out inflammatory etiologies and can also provide evidence of an acute or chronic metabolic disturbance as the cause of symptoms: In particular, a complete blood count, C-reactive protein concentration, renal function tests, blood glucose concentration, and HbA1c level should be obtained. Suspected polyneuropathy can be confirmed by electrophysiological testing, as mentioned above, and a diagnostic lumbar puncture should be performed if there is suspicion of a chronic inflammatory disease of the nervous system, such as borreliosis or multiple sclerosis.
Differential diagnosis.
When PAOD is suspected, the test that is generally performed is Doppler-assisted measurement of the ankle-brachial index (ABI). Degenerative or traumatic diseases of the hips and pelvis need further radiological evaluation.
Polyneuropathy / CNS diseases.
Suspected polyneuropathy can be confirmed by electrophysiological testing, and a diagnostic lumbar puncture is indicated if there is suspicion of a chronic inflammatory disease of the nervous system, such as borreliosis or multiple sclerosis.
Treatment
It can be stated as a rule that only symptomatic patients should be treated. A “pathological” radiological finding is not, in itself, an indication for treatment. The treatment options range from analgesic medication as needed all the way to extensive dorsoventral surgery. The scientifically valid studies that have been performed in this area to date are few, and none of them had a clear age limit or age restriction. Direct comparisons of conservative and surgical treatment are further complicated by the fact that patients with mild stenoses generally undergo the former, while those with severe stenoses generally undergo the latter. Chou et al., in a review of this topic, concluded that moderately good evidence indicates the superiority of surgical over conservative treatment in the first two years. The available evidence is hard to assess, however, because the six randomized trials whose findings were presented involved different surgical methods (laminectomy vs. interspinous spacers) and variable follow-up intervals (12).
Atlas et al. (13) prospectively followed patients for eight to ten years and found better results in the first four years in the patients who had undergone surgery. At the end of the follow-up period, however, the two groups no longer differed with respect to low back pain or overall satisfaction, while all patients had a marked reduction of the leg-pain component. It must be noted, however, that 37% of the patients who were initially treated conservatively went on to have surgery. Radicular symptoms were improved in 67% of the patients who had surgery and in 41% of those treated conservatively. Chang et al. (14), too, found that surgery yielded better results than conservative treatment after ten years of follow-up. Analogously to the observations of Atlas et al. (13), the two groups did not differ significantly at five or ten years with respect to spinal symptoms or overall satisfaction, but the surgical patients had greater improvements in functional status and leg pain.
Treatment options.
The treatment options range from analgesic medication as needed all the way to extensive dorso-ventral surgery.
A functionally limiting neurological deficit (paresis) is a clear-cut surgical indication. The indication is urgent if the deficit is acute and severe, particularly if there is a disturbance of bladder and/or bowel function.
Our search revealed no valid evidence regarding potential surgical indications for patients without any neurological deficit. The individual decisions that are made in such cases are based mainly on the patient’s degree of suffering and impairment of quality of life. The surgical indication is hard to confirm objectively, though the maximal distance the patient can walk without pain is a potential measure of the patient’s impairment.
Given the high frequency of degenerative changes in imaging studies of the lumbar spine, surgery should only be performed if the clinical manifestations are clearly correlated with the radiological findings.
The potential predictors of a favorable outcome are foraminal stenosis, predominant leg pain, and neurological deficits.
Clear-cut surgical indications.
A functionally limiting neurological deficit (paresis) is a clear-cut surgical indication. The indication is urgent if the deficit is acute and severe, particularly if there is a disturbance of bladder and/or bowel function.
Interestingly, it has been clearly demonstrated that non-smokers benefit more from surgery than smokers do; thus, smoking cessation is recommended before surgery. Persons who have had symptoms for less than a year also seem to have a better outcome (15).
Conservative treatment
Conservative treatment is mainly aimed at alleviating the major clinical manifestation of degenerative instability and may, in fact, bring some patients long-lasting relief. There has been criticism of the long-term use of non-steroidal anti-inflammatory drugs and muscle relaxants, the use of steroids and antidepressants, and the use of long-acting opioids (16, 17). The main pillars of conservative treatment, above all in older people, are intensive physiotherapy with muscle-relaxing techniques in the acute phase, and strengthening of the back muscles in the later course to preserve function and mobility. Local injections (facet infiltrations, epidural injections of local anesthetic and/or steroids) may be helpful in individual cases but are not supported by any hard scientific evidence, even though multiple randomized trials have been performed (18, 19). The available data are insufficient to document the efficacy of treatment with remedial gymnastics, back immobilization, posture training, or orthoses (16, 17).
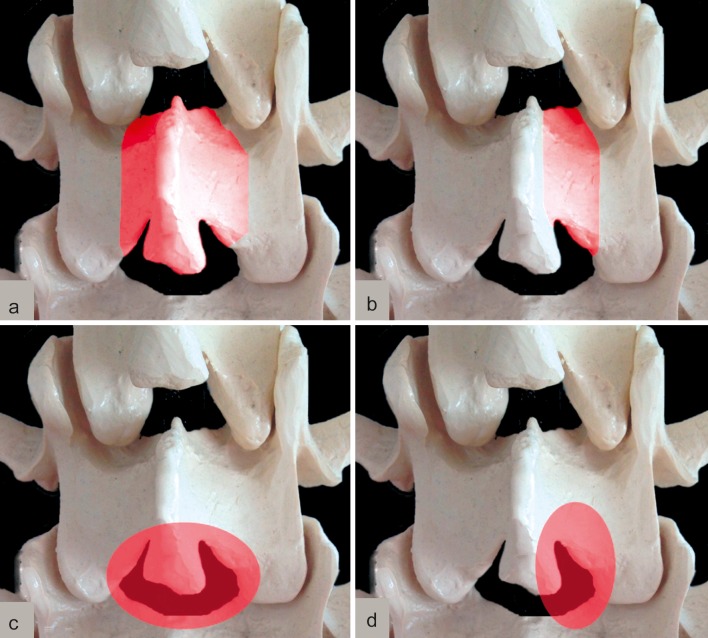
Surgery—decompression
The goal of surgery is to decompress the nerve roots, dura mater, and vessels without impairing segmental stability. It must first be determined whether the patient is suffering from spinal stenosis alone or from segmental instability in addition. Possible decompressive techniques include laminectomy, hemilaminectomy, uni- or bilateral hemilaminotomy, foraminotomy, and fenestration with undercutting decompression (Figures 2 and 3). Laminectomy involves removal of the dorsal “tension boom” and is thus considered to promote instability, while hemilaminectomy permits better stability with preservation of the dorsal tension boom as well as all of the contralateral ligamentous structures. In hemilaminotomy, portions of two neighboring hemilaminae are removed on one side or both; in bilateral hemilaminotomy, the midline structures are preserved (20). Hardly any scientific evidence supports the use of any particular type of surgery over any other, but there has been one randomized trial showing laminotomy to be superior to laminectomy (21).
Figure 2.
Methods of simple decompression:
a) laminectomy
b) hemilaminectomy
c) bilateral and
d) unilateral interlaminar fenestration with undercutting
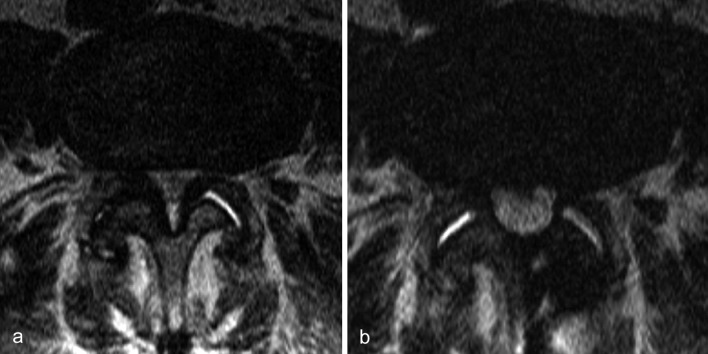
Figure 3.
Bilateral, severe spinal canal and lateral recess stenosis
a) Preoperative axial T2-weighted MRI at the L3 and L4 levels
b) An MRI six months after surgery reveals the extent of decompression, performed in this case as a unilateral interlaminar decompression from the left with undercutting on the right. The typical spinal claudication that was present before surgery resolved completely. Back pain on movement remained to some extent but did not cause any significant impairment. (With kind permission of the Neuroradiology Division at the Universitätsklinikum Jena)
In the absence of neurological deficits.
The individual treatment decision made in a patient without any neurological deficit are based mainly on the patient’s degree of suffering and impairment of quality of life.
Surgical methods.
The goal of surgery is to decompress the nerve roots, dura mater, and vessels without impairing segmental stability. It must first be determined whether the patient has spinal stenosis alone, or segmental instability in addition.
The complication rate after surgical treatment of spinal stenosis is considerable. In a prospective study published in 2010, 101 patients over the age of 70 who underwent purely decompressive procedures had an 18% complication rate. The most common complication was a dural injury without further clinical consequences (9%). Two patients had deep wound infections, and three died of concomitant, unrelated illnesses 26 days, 9 months, and 11 months after surgery (22).
Inadequate decompression may leave a significant degree of recurrent stenosis. Jansson et al. (23) documented a reoperation rate of 11% over ten years of follow-up.
Surgical technique—instrumentation in addition to decompression
A meta-analysis revealed that there is good evidence favoring the addition of a fusion to a decompressive operation for spinal stenosis if spondylolisthesis is also present (24). Schulte et al. (25) chose to perform a non-instrumented fusion for multimorbid patients but expressly noted that they recommend instrumentation in cases of multisegmental decompression. A Cochrane report dated 2005 (26) documented a better fusion rate for instrumented than for non-instrumented fusion, which, however, was associated with an only slightly better clinical outcome. Van Tulder et al. (27) found no evidence for the superiority of instrumentation over posterolateral fusion alone with respect to the end result of treatment.
Possible approaches to decompression.
laminectomy
hemilaminectomy
hemilaminotomy (uni- or bilateral)
foraminotomy
fenestration with undercutting decompression
Complication rates.
The complication rate after surgical treatment of spinal stenosis is considerable. In a prospective study published in 2010, 101 patients over the age of 70 who underwent purely decompressive procedures had an 18% complication rate.
Indications for interspinous spacers and dynamic stabilization—Conventional fusion techniques are intended to immobilize one or more motion segments. In recent years, however, alternative methods have been devised, arising from the conviction that it is only non-physiological motion, not normal motion, that gives these patients pain (28). Implants such as the “dynamic” fixator and the interspinous spacer are intended to stabilize the segment only partially without eliminating functional movement (29, 30). They are said to lower intradiscal pressure, lessen mechanical stress on the intervertebral joints, and widen the spinal neural foramina and spinal canal by distracting the vertebral bodies. Zucherman et al. found in a randomized trial (31) that patients treated with an interspinous spacer experienced a 45% reduction of symptoms at two years, compared to 7% in a group treated non-operatively. Grob et al. (32), Sapkas et al. (33), and Schnake et al. (34) carried out retrospective follow-up studies and concluded that dynamic instrumentation yields results comparable to, but no better than, those of fusion surgery.
Indications for fusion—Documented lumbar spinal instability is a universally accepted indication for fusion. This indication is present in cases with symptomatic lumbar scoliosis, rotational instability with slippage, demonstrable sagittal deformities such as lordosis-associated facet joint degeneration with corresponding symptoms, or severe lumbosacral kyphosis and demonstrated spondylolisthesis with intense low back pain (Figures 4– 7).
Figure 4.

This otherwise healthy 79-year-old woman presented in 2011 with severe pain and could not walk more than 200 m without pausing. She also had marked radicular symptoms. Imaging revealed lumbar scoliosis with rotational slippage and consequent spinal stenosis, along with typical age-associated degenerative changes at all of the spinal levels depicted
Figure 7.

A lateral view of the same patient reveals a correct implant configuration without any evidence of loosening or dislocation. There are unaltered signs of degeneration at the adjacent levels. No instability has arisen
The differential indications for various types of surgery for spinal stenosis can be roughly delineated as follows. The indication depends on the degree of instability of the segment that is to be decompressed, as well as on the severity of preoperative low back pain. The surgical techniques that can be used range from non-instrumented posterolateral fusion to dorsoventral instrumented fusion. Instrumented fusion is considered a modern technique; it can be performed as an anterior, posterior, or transforaminal lumbar intercorporeal fusion (ALIF, PLIF, or TLIF), or else dorsoventrally. Any of these methods can directly decompress the spinal canal through distraction of the affected segment. The neural elements can also be further decompressed by application of the surgical techniques discussed in the preceding paragraphs. In multisegmental fusion surgery, particularly when multisegmental stenosis or rotational instability is present, an excellent decompression can be obtained with laminectomies at the vertebral levels that are to be fused, without any compromise of spinal stability.
Differential indications.
The indication depends on the degree of instability of the segment that is to be decompressed, as well as on the severity of preoperative low back pain.
Moreover, spondylodesis is clearly indicated if decompressive surgery alone would exacerbate instability, or if the patient’s symptoms are mainly instability-related (35). In one of the few randomized trials that have been performed in this field, Weinstein et al. (36) found that patients with degenerative spondylolisthesis obtain better pain relief and functional improvement from surgery than from conservative treatment. Fusion surgery increases the mechanical stress on the motion segments adjacent to the fusion, accelerating their degeneration (37). Min et al. (38) emphasize the lack of correlation between the radiological and clinical outcomes. More studies will be needed to determine whether percutaneous TLIF and PLIF (so-called PTLIF and PPLIF) (39) actually improve the outcome still further, as reported by Gepstein et al. (40).
Conclusion
Although the number of persons over age 65 with lumbar spinal stenosis is rising, there is still no evidence-based treatment approach that takes the specific problems of older patients into account. In our view, the wholesale application to older patients of treatment strategies that are suitable for younger ones is problematic. Moreover, the decision to treat surgically or conservatively should be made individually in each case.
Although the evidence base on conservative treatment is sparse for want of clinical trials, all cases of spinal stenosis are treated conservatively at first, except those with high-grade instability. In particular, conservative treatment is best for patients with accompanying illnesses that heighten the risks of surgery and anesthesia.
The purpose of surgery for symptomatic lumbar spinal stenosis is to decompress the spinal canal. In choosing the appropriate treatment, the surgeon must take account of the diminished physical and mental performance of older people, the poorer condition of their muscles, and the physiological aging of their spines. The surgeon must not aim for a cosmetic radiological result that restores the spinal anatomy of a 30-year-old. Rather, the best form of treatment is an age-adapted one that maximally preserves the independence of the older patient after surgery. (This may not be the case, for example, after extensive, multisegmental fusions.) Further studies are needed, particularly in patients of advanced age.
Conservative treatment.
Although the evidence base on conservative treatment is sparse for want of clinical trials, all cases of spinal stenosis are treated conservatively at first, except those with high-grade instability.
The state of the evidence.
There is still no evidence-based treatment approach that takes the specific problems of older patients into account.
Figure 5.

A lateral view of the same patient reveals loss of height of all of the lumbar discs, with vacuum phenomena at L2/3, L4/5, and L5/S1 and corresponding osteochondrosis. The double contours of the posterior edges of the L2 and L3 vertebral bodies indicate that these two vertebrae are rotated
Figure 6.
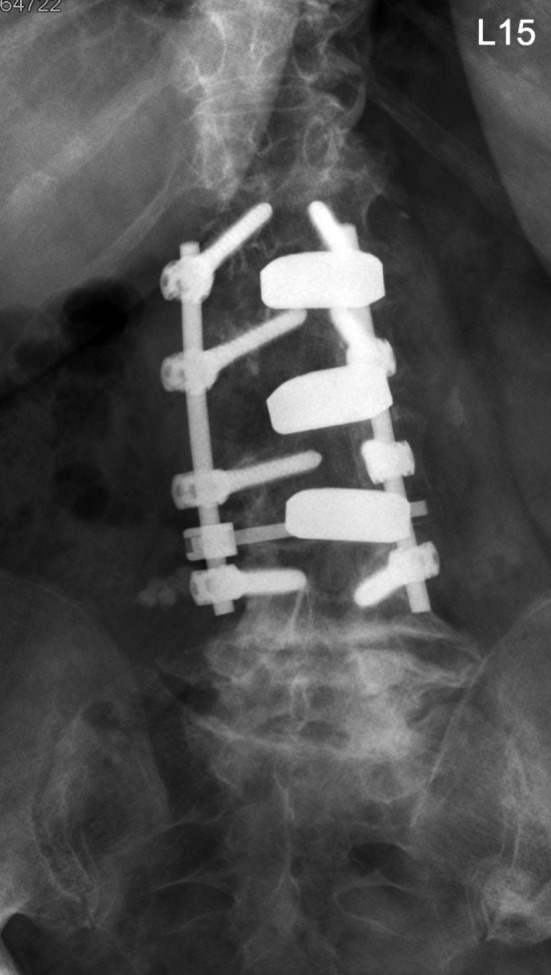
1 1/2 years after unilateral, multisegmental, dorsoventral decompression and fusion, the spinal deformity in the frontal x-ray view has been fully corrected. Laminectomies were performed at the apex of the curvature. There are unaltered signs of degeneration at the levels adjacent to the fusion. More important than the postoperative images is the clinical result: the patient now complains only of mild back pain and takes no medication. For longer walks away from home, she uses a cane to feel secure. She has no radicular symptoms
Further Information on CME.
This article has been certified by the North Rhine Academy for Postgraduate and Continuing Medical Education. Deutsches Ärzteblatt provides certified continuing medical education (CME) in accordance with the requirements of the Medical Associations of the German federal states (Länder). CME points of the Medical Associations can be acquired only through the Internet, not by mail or fax, by the use of the German version of the CME questionnaire. See the following website: cme.aerzteblatt.de.
Participants in the CME program can manage their CME points with their 15-digit “uniform CME number” (einheitliche Fortbildungsnummer, EFN). The EFN must be entered in the appropriate field in the cme.aerzteblatt.de website under “meine Daten” (“my data”), or upon registration. The EFN appears on each participant’s CME certificate.
The CME unit “Growing Up Is Hard—Mental Disorders in Adolescence”
(Issue 25/2013) can be accessed until 22 September 2013.
The CME unit “The Treatment and Natural Course of Peripheral and Central Vertigo” (Issue 29–30 /2013) can be accessed until 20 October 2013.
The CME unit “Shortness of Breath and Cough in Palliative Care”
(Issue 33–34/2013) can be accessed until 17 November 2013.
For Issue 41/2013, we plan to offer the topic “Common causes of poisoning—etiology, diagnosis and treatment.”
Please answer the following questions to participate in our certified Continuing Medical Education program. Only one answer is possible per question. Please select the answer that is most appropriate.
Question 1
What are the main causes of lumbar spinal stenosis in older people?
congenital deformities
malpositions caused by bad posture
degenerative segmental changes
drug-induced osteomalacia
post-menopausal hormone deficiencies
Question 2
Which of the following is a common differential diagnosis of spinal claudication?
thrombosis
lumbar disc herniation
necrosis of the femoral head
multiple sclerosis
myopathy
Question 3
Your history and clinical examination of a 70-year-old man arouse the suspician of lumbar spinal stenosis in need of treatment. What further study is the best one to establish the diagnosis?
electrophysiology (nerve conduction velocity)
lumbar puncture
computed tomography (CT)
routine laboratory testing
MRI of the lumbar spine
Question 4
What diagnostic test is useful for evaluating the condition of bone and the possible presence of osteoporosis?
Doppler ultrasonography
serum calcium level
strength testing
somatosensory evoked potentials
lumbar CT
Question 5
In which of the following situations is surgery indicated for lumbar spinal stenosis?
when MRI shows stenosis at L3/4 in an asymptomatic patient
when MRI shows stenoses at L3/4 and L4/5 in a patient who has had medically well-controlled sciatica for two weeks
when the patient has sciatica on walking and the MRI is normal
when MRI shows stenosis at L4/5 with a progressive foot drop over the last three weeks
when the patient has occasional bladder and bowel disturbances and the MRI is normal
Question 6
A 72-year-old man presents with progressive back and leg pain of three weeks’ duration. Which of the following statements about the differential diagnosis is correct?
If PAOD is found, degenerative spinal stenosis is ruled out as the cause of symptoms.
The underlying cause may be cancer, regardless of the patient’s age.
Physical examination should suffice to establish the diagnosis.
If the patient has pain after walking 500 meters, he probably does not have lumbar spinal stenosis.
A tick-bite three years ago is of no diagnostic relevance.
Question 7
The neurological examination reveals pain on maneuvers that stretch the lumbar and sacral nerve roots, grade M2 gastrocnemius weakness on the right, and pain on percussion of the lower portion of the lumbar spine. What should be the next diagnostic step(s)?
myelography with post-myelographic CT
further observation, follow-up appointment in eight weeks
MRI and blood tests
chest CT, electrophysiological tests
lumbar puncture
Question 8
What is the quality of the currently available evidence pertaining to a treatment approach for symptomatic lumbar spinal stenosis that addresses the specific situation of older patients?
There is no evidence-based therapeutic algorithm.
Systematic reviews of numerous randomized controlled trials provide adequate evidence of efficacy.
There is adequate evidence that long-term treatment with opioids is effective.
Many randomized trials have clearly proven the superiority of fusion surgery over decompression.
Very good evidence favors the use of orthoses.
Question 9
A 68-year-old woman complains of back pain independent of position ever since she did some gardening about a week ago. A thorough physical examination reveals nothing abnormal. An MRI scan shows lumbar spinal stenosis L3/4 as the only abnormality. What next step is indicated?
surgical decompression without fusion
conservative treatment
lumbar myelography
lumbar puncture
surgical decompression and fusion at the next elective opportunity
Question 10
A 70-year-old woman has been suffering from medically intractable, immobilizing, diffuse, bilateral back and leg pain for approximately the last six months. She can walk no further than a few meters, and physical examination reveals weakness of the left quadriceps femoris muscle. MRI reveals high-grade circumferential spinal stenosis at L3/4 and L4/5 with degenerative spondylolisthesis. What treatment is indicated?
remedial gymnastics
steroid injections
epidural local anesthetic injection
operative decompression and instrumented fusion
a supportive orthosis
Acknowledgments
Translated from the original German by Ethan Taub, M.D.
Footnotes
Conflict of interest statement
The authors state that they have no conflicts of interest.
References
- 1.Allen RT, Rihn JA, Glassman SD, Currier B, Albert TJ, Phillips FM. An evidence-based approach to spine surgery. Am J Med Qual. 2009;24(Suppl 6):15–24. doi: 10.1177/1062860609348743. [DOI] [PubMed] [Google Scholar]
- 2.Watters WC, Baisden J, Gilbert TJ, et al. Degenerative lumbar spinal stenosis: an evidence-based clinical guideline for the diagnosis and treatment of degenerative lumbar spinal stenosis. Spine J. (3rd) 2008;8:305–310. doi: 10.1016/j.spinee.2007.10.033. [DOI] [PubMed] [Google Scholar]
- 3.Statistisches Bundesamt Gesundheit. Fachserie 12 Reihe 6.2.1. Wiesbaden: Statistisches Bundesamt; 2011. Diagnosedaten der Patienten und Patientinnen in Krankenhäusern (einschließlich Sterbe- und Stundenfälle) [Google Scholar]
- 4.Cheung KM, Karppinen J, Chan D, et al. Prevalence and pattern of lumbar magnetic resonance imaging changes in a population study of one thousand forty-three individuals. Spine. 2009;34:934–940. doi: 10.1097/BRS.0b013e3181a01b3f. [DOI] [PubMed] [Google Scholar]
- 5.Jensen MC, Brant-Zawadzki MN, Obuchowski N, Modic MT, Malkasian D, Ross JS. Magnetic resonance imaging of the lumbar spine in people without back pain. N Engl J Med. 1994;331:69–73. doi: 10.1056/NEJM199407143310201. [DOI] [PubMed] [Google Scholar]
- 6.Porter RW. Spinal stenosis and neurogenic claudication. Spine. 1996;21:2046–2052. doi: 10.1097/00007632-199609010-00024. [DOI] [PubMed] [Google Scholar]
- 7.Suri P, Rainville J, Kalichman L, Katz JN. Does this older adult with lower extremity pain have the clinical syndrome of lumbar spinal stenosis? JAMA. 2010;304:2628–2636. doi: 10.1001/jama.2010.1833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Imagama S, Matsuyama Y, Sakai Y, et al. An arterial pulse examination is not sufficient for diagnosis of peripheral arterial disease in lumbar spinal canal stenosis: a prospective multicenter study. Spine. 2011;36:1204–1210. doi: 10.1097/BRS.0b013e3181ebd86f. [DOI] [PubMed] [Google Scholar]
- 9.Saito J, Ohtori S, Kishida S, et al. Difficulty of diagnosing the orgin of lower leg pain in patients with both lumbar spinal stenosis and hip joint osteoarthritis. Spine. 2012;37:2089–2093. doi: 10.1097/BRS.0b013e31825d213d. [DOI] [PubMed] [Google Scholar]
- 10.Lee BH, Moon SH, Kim HJ, Lee HM, Kim TH. Osteoporotic profiles in elderly patients with symptomatic lumbar spinal canal stenosis. Indian J Orthop. 2012;46:279–284. doi: 10.4103/0019-5413.96379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wassenaar M, van Rijn RM, van Tulder MW, et al. Magnetic resonance imaging for diagnosing lumbar spinal pathology in adult patients with low back pain or sciatica: a diagnostic systematic review. Eur Spine J. 2012;21:220–227. doi: 10.1007/s00586-011-2019-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chou R, Baisden J, Carragee EJ, Resnick DK, Shaffer WO, Loeser JD. Surgery for low back pain: a review of the evidence for an American Pain Society Clinical Practice Guideline. Spine. 2009;34:1094–1109. doi: 10.1097/BRS.0b013e3181a105fc. [DOI] [PubMed] [Google Scholar]
- 13.Atlas SJ, Keller RB, Wu YA, Deyo RA, Singer DE. Long term outcomes of surgical and nonsurgical management of lumbar spinal stenosis; 8 to 10 year results from the maine lumbar spine study. Spine. 2005;30:936–943. doi: 10.1097/01.brs.0000158953.57966.c0. [DOI] [PubMed] [Google Scholar]
- 14.Chang Y, Singer DE, WuYa, Keller RB, Atlas SJ. The effect of surgical and nonsurgical treatment on longitudinal outcomes of lumbar spinal stenosis over 10 years. J Am Geriatr Soc. 2005;53:785–792. doi: 10.1111/j.1532-5415.2005.53254.x. [DOI] [PubMed] [Google Scholar]
- 15.Pearson A, Lurie J, Tosteson T, Zhao W, Abdu W, Weinstein JN. Who should have surgery for spinal stenosis? Treatment effect predictors in SPORT. Spine. 2012;37:1791–1802. doi: 10.1097/BRS.0b013e3182634b04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Atlas SJ, Elitto A. Spinal stenosis: surgical versus nonsurgical treatment. Clin Orthopad Relat Res. 2006;443:198–207. doi: 10.1097/01.blo.0000198722.70138.96. [DOI] [PubMed] [Google Scholar]
- 17.van Tulder MW, Koes B, Malmivaara A. Outcome of non-invasive treatment modalities on back pain: an evidence-based review. Eur Spine J. 2006;15(Suppl 1):64–81. doi: 10.1007/s00586-005-1048-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Brown LL. A double-blind, randomized, prospective study of epidural steroid injection vs. the mild(®) procedure in patients with symptomatic lumbar spinal stenosis. Pain Pract. 2012;12:333–341. doi: 10.1111/j.1533-2500.2011.00518.x. [DOI] [PubMed] [Google Scholar]
- 19.Cohen SP, Bicket MC, Jamison D, Wilkinson I, Rathmell JP. Epidural steroids: a comprehensive, evidence-based review. Reg Anesth Pain Med. 2013;38:175–200. doi: 10.1097/AAP.0b013e31828ea086. [DOI] [PubMed] [Google Scholar]
- 20.Thomé C, Börm W, Meyer F. Degenerative lumbar spinal stenosis: current strategies in diagnosis and treatment. Dtsch Arztebl Int. 2008;105(20):373–379. doi: 10.3238/arztebl.2008.0373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Thomé C, Zevgaridis D, Leheta O, et al. Outcome after less-invasive decompression of lumbar spinal stenosis: a randomized comparison of unilateral laminotomy, bilateral laminotomy, and laminectomy. J Neurosurg Spine. 2005;3:129–141. doi: 10.3171/spi.2005.3.2.0129. [DOI] [PubMed] [Google Scholar]
- 22.Jakola AS, Sørlie A, Gulati S, Nygaard OP, Lydersen S, Solberg T. Clinical outcomes and safety assessment in elderly patients undergoing decompressive laminectomy for lumbar spinal stenosis: a prospective study. BMC Surg. 2010;10 doi: 10.1186/1471-2482-10-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jansson KG, Nemeth G, Granath F, Blomqvist P. Spinal stenosis reoperation rate in Sweden is 11% at 10 years—a national analysis of 9,664 operations. Eur Spine J. 2005;14:659–663. doi: 10.1007/s00586-004-0851-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Resnick DK, Choudhri TF, Dailey AT, et al. Guidelines for the performance of fusion procedures for degenerative disease of the lumbar spine. Part 9: fusion in patients with stenosis and spondylolisthesis. J Neurosurg Spine. 2005;2:679–685. doi: 10.3171/spi.2005.2.6.0679. [DOI] [PubMed] [Google Scholar]
- 25.Schulte TL, Bullmann V, Lerner T, et al. Lumbar spinal stenosis. Orthopade. 2006;35:675–692. doi: 10.1007/s00132-006-0971-5. [DOI] [PubMed] [Google Scholar]
- 26.Gibson JN, Waddell G. Surgery for degenerative lumbar spondylosis: updated Cochrane Review. Spine. 2005;30:2312–2320. doi: 10.1097/01.brs.0000182315.88558.9c. [DOI] [PubMed] [Google Scholar]
- 27.van Tulder MW, Koes B, Seitsolo S, Malmivaara A. Outcome of invasive treatment modalities on back pain and sciatica: an evidence-based review. Euro Spine J. 2006;15(Suppl 1):82–92. doi: 10.1007/s00586-005-1049-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hanley EN, Phillips ED, Kostuik JP. Frymoyer JW, editor. Who should be fused? The adult spine. Principles and practice. 1991:1873–1917. [Google Scholar]
- 29.Christie SD, Song JK, Fessler RG. Dynamic interspinous process technology. Spine. 2005;30:73–78. doi: 10.1097/01.brs.0000174532.58468.6c. [DOI] [PubMed] [Google Scholar]
- 30.Richards JC, Majumdar S, Lindsey DP, Beaupré GS, Yerby SA. The treatment mechanism of an interspinous process implant for lumbar neurogenic intermittent claudication. Spine. 2005;30:744–749. doi: 10.1097/01.brs.0000157483.28505.e3. [DOI] [PubMed] [Google Scholar]
- 31.Zucherman JF, Hsu KY, Hartjen CA, et al. A multicenter, prospective, randomized trial evaluating the X-Stop interspinous process decompression system for the treatment of neurogenic intermittens claudication: two year follow-up results. Spine. 2005;30:1351–1358. doi: 10.1097/01.brs.0000166618.42749.d1. [DOI] [PubMed] [Google Scholar]
- 32.Grob D, Benini A, Junge A, Mannion AF. Clinical experience with the Dynesys semirigid fixation system for the lumbar spine: surgical and patient-oriented outcome in 50 cases after an average of 2 years. Spine. 2005;30:324–331. doi: 10.1097/01.brs.0000152584.46266.25. [DOI] [PubMed] [Google Scholar]
- 33.Sapkas G, Mavrogenis AF, Starantzis KA, Soultanis K, Kokkalis ZT, Papagelopoulos PJ. Outcome of a dynamic neutralization system for the spine. Orthopedics. 2012;35:e1497–e1502. doi: 10.3928/01477447-20120919-19. [DOI] [PubMed] [Google Scholar]
- 34.Schnake KJ, Schaeren S, Jeanneret B. Dynamic stabilization in addition to decompression for lumbar spinal stenosis with degenerative spondylolisthesis. Spine. 2006;31:442–449. doi: 10.1097/01.brs.0000200092.49001.6e. [DOI] [PubMed] [Google Scholar]
- 35.Garfin SR, Herkowitz HN, Mirkovic S. Spinal stenosis. Instr Course Lect. 2000;49:361–374. [PubMed] [Google Scholar]
- 36.Weinstein JN, Lurie JD, Tosteson TD, et al. Surgical compared with nonoperative treatment for lumbar degenerative spondylolisthesis. four-year results in the Spine Patient Outcomes Research Trial (SPORT) randomized and observational cohorts. J Bone Joint Surg Am. 2009;9:1295–1304. doi: 10.2106/JBJS.H.00913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lee CK. Accelerated degeneration of the segment adjacent to a lumbar fusion. Spine. 1988;13:375–377. doi: 10.1097/00007632-198803000-00029. [DOI] [PubMed] [Google Scholar]
- 38.Min JH, Jang JS, Jung B, et al. The clinical characteristics and risk factors for the adjacent segment degeneration in instrumented lumbar fusion. J Spinal Disord Tech. 2008;21:305–309. doi: 10.1097/BSD.0b013e318142b960. [DOI] [PubMed] [Google Scholar]
- 39.Scheufler KM, Dohmen H, Vougioukas VI. Percutaneous transforaminal lumbar interbody fusion for the treatment of degenerative lumbar instability. Neurosurgery. 2007;60(Suppl 2):203–212. doi: 10.1227/01.NEU.0000255388.03088.B7. [DOI] [PubMed] [Google Scholar]
- 40.Gepstein R, Shabat S, Reichel M, Pikarsky I, Folman Y. Treatment of postdiscectomy low back pain by percutaneous posterior lumbar interbody fusion versus open posterior lumbar fusion with pedicle screws. Spine J. 2008;8:741–746. doi: 10.1016/j.spinee.2007.07.393. [DOI] [PubMed] [Google Scholar]