Abstract
Objective
The aim of the present study was to identify variables associated with treatment failure in women with menorrhagia who were treated with thermal balloon ablation (TBA) or levonorgestrel releasing intrauterine system (LNG-IUS), and to determine if there are subgroups where one treatment type is more effective than the other.
Methods
The study included 106 women with menorrhagia who were treated with TBA or LNG-IUS at the study institute between January 2003 and December 2007, with a follow-up period greater than 12 months. Data were collected by retrospective review of medical records. Treatment failure was defined as persistent or recurrent menorrhagia within one year after treatment or hysterectomy at any time during follow-up. The relationships between variables and treatment outcome were analyzed using the chi-square or Fisher's exact test. The treatment outcome of TBA was compared with LNG-IUS.
Results
Sixty-seven women were treated with TBA and 39 women were managed with LNG-IUS. Fifty-two women had a myoma ≥2.5 cm. Treatment failure was observed in 24 women (2 recurrent or persistent menorrhagia and 22 hysterectomies) and myoma size (≥2.5 cm vs. <2.5 cm) was associated with treatment outcome. TBA and LNG-IUS showed similar treatment outcomes.
Conclusion
A large myoma is a risk factor for treatment failure in women with menorrhagia treated with TBA or LNG-IUS.
Keywords: Menorrhagia, Thermal balloon ablation, Levonorgestrel-releasing intrauterine system, Myoma
Introduction
Menorrhagia is a common symptom, accounting for 20% of all gynecological visits to general practitioners, and is a major clinical problem with significant effects on quality of life [1]. Various types of treatments have been used for treatment of menorrhagia including medical therapy, surgical endometrial ablation and even hysterectomy. However, medical therapy has limited efficacy because of the high incidence of recurrence, the need for prolonged treatment and the presence of adverse side effects [2,3]. For example, a study showed that about 25% of women initially subjected to conservative treatment underwent a hysterectomy within the first year [4].
Recently, women with menorrhagia who prefer less invasive surgical techniques are being treated with thermal balloon endometrial ablation (TBA) or levonorgestrel releasing intrauterine system (LNG-IUS). TBA is a new ablative tool providing a simple and safe alternative to conventional hysteroscopic endometrial ablation and requiring less advanced surgical skills [5,6]. LNG-IUS was originally developed as a contraceptive, and is reported to be effective for the treatment of menorrhagia [7,8]. However, 10% to 30% of women who are managed with TBA or LNG-IUS need additional treatments including hysterectomy. Furthermore, the variables associated with treatment failure have not yet been determined [7,9-13].
Several prospective randomized trials have reported that TBA and LNG-IUS were equally effective in the treatment of menorrhagia [14]. However, the authors hypothesize that there may be subgroups where either TBA or LNG-IUS is more effective than the other treatment type.
The objectives of the present study were to identify variables associated with treatment failure in women with menorrhagia who were treated with TBA or LNG-IUS, and to determine if there are subgroups where one treatment type is more effective than the other.
Materials and Methods
This study identified 170 women with menorrhagia who were treated with TBA or LNG-IUS at the study institute between January 2003 and December 2007. Women with a follow-up period less than 12 months were excluded. The remaining 106 women, all of whom had intramural or submucosal myoma, were included in the study. Menorrhagia was defined as symptomatic excessive menstruation: 1) heavy (more than five fully wet pads) or painful menstrual bleeding for more than seven days, or 2) unable to leave house on heaviest days, or 3) sleep disturbed more than one night. All patients had no history of breast cancer, abnormal cervical cytology, or an ongoing pregnancy.
The data collected by retrospective review of medical records included age, parity, results of transvaginal ultrasonography, and treatment type (TBA vs. LNG-IUS). Every woman had a transvaginal ultrasonographic examination before treatment and the presence, size and location of a uterine myoma were evaluated. Treatment failure was defined as persistent or recurrent menorrhagia within the first year after treatment or a hysterectomy due to intractable recurrent bleeding or pain during the follow-up period.
Endometrial curettage was performed prior to treatment to rule out endometrial hyperplasia or any hidden malignancy. The choice of treatment type was decided at the discretion of physicians. The TBA procedure was performed at post-menstrual day 2 or 3 using the Gynecare Thermachoice (Ethicon, Somerville, NJ, USA) under intravenous or spinal anesthesia in an operation theatre. The balloon was inserted into the endometrial cavity and filled with 5% dextrose solution. Balloon pressure was adjusted to 180 mm Hg and fluid temperature was maintained at 87℃ for 8 minutes. LNG-IUS (Mirena, Bayer HealthCare Pharmaceuticals Inc., Wayne, NJ, USA) was inserted into the uterine cavity during the first 7 days of the menstrual cycle according to the manufacturer's instructions.
The analysis involved an intent-to-treat population. In addition, women whose LNG-IUS disappeared, or who received other treatments after TBA or LNG-IUS were also included in the analysis. The relationships between variables and treatment outcome were analyzed using the chi-square or Fisher's exact test. Two-sided P-values <0.05 were considered statistically significant. SPSS for Windows ver. 12.0 (SPSS Inc., Chicago, IL, USA) was used for all data analyses.
Results
The median age was 43 years (range, 26 to 52 years) and most of the subjects were primiparous or multiparous. No endometrial abnormalities were detected at endometrial curettage. Sixty-seven women were treated with TBA and 39 women were managed with LNG-IUS. The median follow-up duration was 36 months (range, 12 to 77 months). During follow-up, treatment failure was observed in 24 women (2 recurrent or persistent menorrhagia and 22 hysterectomies) and the LNG-IUS disappeared or was removed in 8 women (Table 1). Women treated with TBA were of similar age to those treated with LNG-IUS (mean age of 43 years for TBA vs. 42 years for LNG-IUS; P=0.272) and had a similar parity distribution compared to patients who were treated with LNG-IUS (P=0.439) (Table 2). However, in terms of complications, the incidence of postoperative irregular spotting was higher in the TBA group than in the LNG-IUS group.
Table 1.
Baseline characteristics and the relationship between treatment outcome and age, parity, myoma size and treatment type in women with menorrhagia
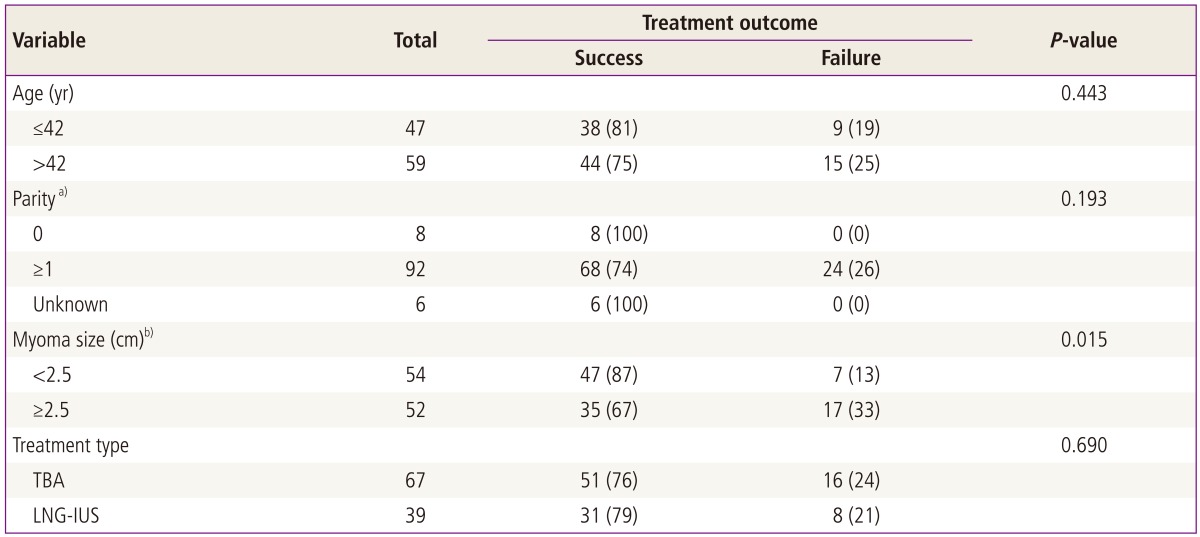
Values are presented as number (%).
TBA, thermal balloon ablation; LNG-IUS, levonorgestrel-releasing intrauterine system.
a)Women with unknown parity were excluded from the analysis when calculating P-values; b)Women without myoma were determined when myoma size was <2.5 cm.
Table 2.
Comparison of patients in the TBA and LNG-IUS groups
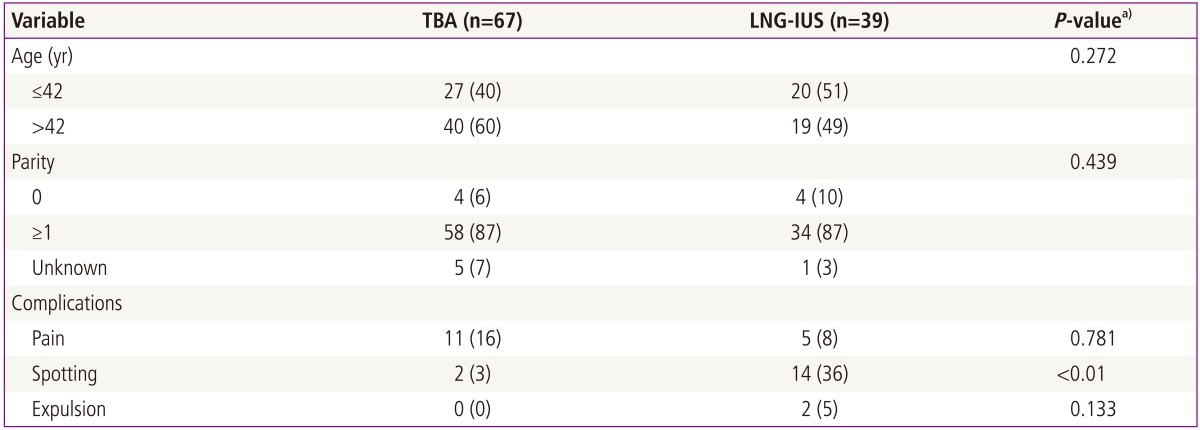
Values are presented as number (%).
TBA, thermal balloon ablation; LNG-IUS, levonorgestrel-releasing intrauterine system.
a)Chi-square test or Fisher's exact test.
Among the variables evaluated in this study, myoma size was significantly associated with treatment outcome in a univariate analysis. On the other hand, age, parity, and treatment type did not affect treatment outcome. Women who were treated with TBA and LNG-IUS had a 76% and 79% treatment success rate, respectively (Table 1).
Because treatment outcome differed according to myoma size, the study population was divided into three subgroups according to myoma size and treatment outcome of TBA and LNG-IUS was analyzed for each subgroup. TBA and LNG-IUS had statistically similar treatment outcomes in all groups. However, in women with a myoma larger than or equal to 5.0 cm, TBA had a higher failure rate than LNG-IUS, although it was not statistically significant (56% for TBA, 25% for LNG-IUS) (Table 3).
Table 3.
Treatment outcome of TBA and LNG-IUS according to myoma size
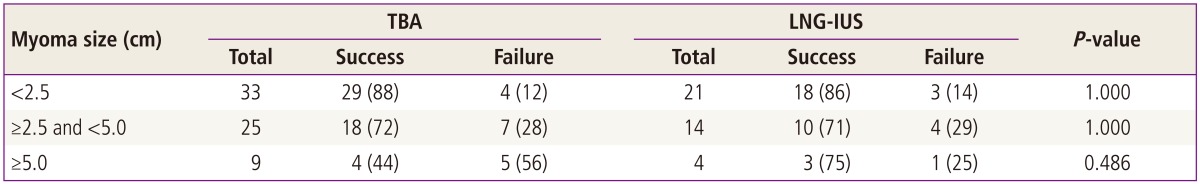
Values are presented as number (%).
TBA, thermal balloon ablation; LNG-IUS, levonorgestrel-releasing intrauterine system.
Discussion
Several variables were suggested as risk factors for TBA failure in women with menorrhagia. For example, age, multiple myoma, adenomyosis, dysmenorrheal and large uterine size have been suggested as risk factors for treatment failure in women with menorrhagia [15-17]. However, data regarding factors associated with treatment failure in women with menorrhagia are not consistent [17].
The present study showed that a large myoma was associated with treatment failure in women with menorrhagia who were treated with TBA or LNG-IUS and this is in accordance with other studies [3,18-21]. A large myoma could severely distort the endometrial cavity, thus interfering with contact between the balloon and the endometrium during the TBA procedure. Moreover, a myoma may continue to grow, resulting in increased blood flow to the uterus and an interruption of myometrial contractions during menstruation. This could cause a gradual increase in menstrual blood loss [15,18,19,22]. Results from this study suggest that an endometrium that does not fit into the balloon because of the presence of a large myoma might be free from thermal ablation, resulting in persistent or recurrent menorrhagia in women treated with TBA. However, even if the conformation of the endometrial cavity prevents full contact between the balloon and the entire endometrial wall, TBA could be still effective in menorrhagia with small myomas. Therefore, a thorough evaluation of the severity of endometrial cavity distortion using ultrasonography and/or saline infusion hysterosonography may be helpful in treatment decision-making.
The TBA procedure actually destroys the endometrium and the effect may be long-lasting or even permanent. LNG-IUS, by contrast, does not destroy the endometrium. The effect on menorrhagia is mediated by slow-releasing levonorgestrel. TBA could have an immediate effect on menorrhagia in a subject without uterine structural abnormalities. On the other hand, many LNG-IUS patients experience a slow and gradual decrease in menstrual blood loss over 6 to 12 months and irregular spotting disappears with time. The difference in outcome kinetics between the two types of endometrial destruction may influence both the patient's and physician's choice of treatment.
Although the effects of TBA are dramatic in the early phases, delayed treatment failure was reported in several studies, which was probably caused by endometrial regeneration [22-24]. Ultimately, approximately 10% to 20% of the patients in the cited studies were not cured, and both thick endometrium and young age were risk factors for treatment failure. When young women were treated with TBA, about 20% of the patients required additional treatment after 1 to 2 years. Endometrial thinning in the early proliferative phase of the menstrual cycle and administration of gonadotropin-releasing hormone analogs or danazol prior to use of TBA improved both the operating conditions and treatment outcomes [13]. Considering these types of risk factors, physicians tend to favor TBA for the treatment of perimenopausal women with severe anemia.
A slow and gradual decrease of menorrhagia is frequently observed in women with menorrhagia treated with LNG-IUS. A literature review of reports on LNG-IUS showed that a considerable number of women had withdrawn from treatment primarily because they felt it was ineffective or they experienced irregular vaginal bleeding [11,21,23]. However, in these studies, most of the patients who used the LNG-IUS for 6 to 24 months were satisfied with the treatment effects and their irregular spotting eventually disappeared. Therefore, prior to insertion of LNG-IUS, the physician should explain the possibility of a delayed effect on menorrhagia and the possibility of irregular vaginal bleeding. Furthermore, additional medication during the several months following insertion could increase the success rate of LNG-IUS by encouraging patients not to withdraw from treatment. Such medication can later be discontinued while treatment with LNG-IUS continues [21].
In this study, myoma size was associated with treatment failure of TBA or LNG-IUS in women with menorrhagia. However, this study did not observe a statistically significant difference in treatment outcomes in patients with a large myoma. There should be a thorough physician-patient discussion on the merits and drawbacks of each treatment type prior to the treatment.
References
- 1.Nilsson L, Rybo G. Treatment of menorrhagia. Am J Obstet Gynecol. 1971;110:713–720. doi: 10.1016/0002-9378(71)90259-6. [DOI] [PubMed] [Google Scholar]
- 2.Cooper KG, Parkin DE, Garratt AM, Grant AM. Two-year follow up of women randomised to medical management or transcervical resection of the endometrium for heavy menstrual loss: clinical and quality of life outcomes. Br J Obstet Gynaecol. 1999;106:258–265. doi: 10.1111/j.1471-0528.1999.tb08240.x. [DOI] [PubMed] [Google Scholar]
- 3.Crosignani PG, Vercellini P, Mosconi P, Oldani S, Cortesi I, De Giorgi O. Levonorgestrel-releasing intrauterine device versus hysteroscopic endometrial resection in the treatment of dysfunctional uterine bleeding. Obstet Gynecol. 1997;90:257–263. doi: 10.1016/S0029-7844(97)00226-3. [DOI] [PubMed] [Google Scholar]
- 4.Carlson KJ, Miller BA, Fowler FJ., Jr The Maine Women's Health Study: II. Outcomes of nonsurgical management of leiomyomas, abnormal bleeding, and chronic pelvic pain. Obstet Gynecol. 1994;83:566–572. doi: 10.1097/00006250-199404000-00013. [DOI] [PubMed] [Google Scholar]
- 5.Hart R, Magos A. The alternatives to hysterectomy. Baillieres Best Pract Res Clin Obstet Gynaecol. 1999;13:271–290. doi: 10.1053/beog.1999.0022. [DOI] [PubMed] [Google Scholar]
- 6.Lethaby A, Hickey M. Endometrial destruction techniques for heavy menstrual bleeding: a Cochrane review. Hum Reprod. 2002;17:2795–2806. doi: 10.1093/humrep/17.11.2795. [DOI] [PubMed] [Google Scholar]
- 7.Hurskainen R, Teperi J, Rissanen P, Aalto AM, Grenman S, Kivela A, et al. Quality of life and cost-effectiveness of levonorgestrel-releasing intrauterine system versus hysterectomy for treatment of menorrhagia: a randomised trial. Lancet. 2001;357:273–277. doi: 10.1016/S0140-6736(00)03615-1. [DOI] [PubMed] [Google Scholar]
- 8.Lethaby AE, Cooke I, Rees M. Progesterone or progestogen-releasing intrauterine systems for heavy menstrual bleeding. Cochrane Database Syst Rev. 2005;(4):CD002126. doi: 10.1002/14651858.CD002126.pub2. [DOI] [PubMed] [Google Scholar]
- 9.Apgar BS, Kaufman AH, George-Nwogu U, Kittendorf A. Treatment of menorrhagia. Am Fam Physician. 2007;75:1813–1819. [PubMed] [Google Scholar]
- 10.Iavazzo C, Salakos N, Bakalianou K, Vitoratos N, Vorgias G, Liapis A. Thermal balloon endometrial ablation: a systematic review. Arch Gynecol Obstet. 2008;277:99–108. doi: 10.1007/s00404-007-0449-7. [DOI] [PubMed] [Google Scholar]
- 11.Busfield RA, Farquhar CM, Sowter MC, Lethaby A, Sprecher M, Yu Y, et al. A randomised trial comparing the levonorgestrel intrauterine system and thermal balloon ablation for heavy menstrual bleeding. BJOG. 2006;113:257–263. doi: 10.1111/j.1471-0528.2006.00863.x. [DOI] [PubMed] [Google Scholar]
- 12.Gupta B, Mittal S, Misra R, Deka D, Dadhwal V. Levonorgestrel-releasing intrauterine system vs. transcervical endometrial resection for dysfunctional uterine bleeding. Int J Gynaecol Obstet. 2006;95:261–266. doi: 10.1016/j.ijgo.2006.07.004. [DOI] [PubMed] [Google Scholar]
- 13.Sowter MC, Lethaby A, Singla AA. Pre-operative endometrial thinning agents before endometrial destruction for heavy menstrual bleeding. Cochrane Database Syst Rev. 2002;(3):CD001124. doi: 10.1002/14651858.CD001124. [DOI] [PubMed] [Google Scholar]
- 14.Kaunitz AM. Progestin-releasing intrauterine systems and leiomyoma. Contraception. 2007;75:S130–S133. doi: 10.1016/j.contraception.2007.01.012. [DOI] [PubMed] [Google Scholar]
- 15.O'Connor H, Broadbent JA, Magos AL, McPherson K. Medical Research Council randomised trial of endometrial resection versus hysterectomy in management of menorrhagia. Lancet. 1997;349:897–901. doi: 10.1016/S0140-6736(96)07285-6. [DOI] [PubMed] [Google Scholar]
- 16.Shaamash AH, Sayed EH. Prediction of successful menorrhagia treatment after thermal balloon endometrial ablation. J Obstet Gynaecol Res. 2004;30:210–216. doi: 10.1111/j.1447-0756.2004.00189.x. [DOI] [PubMed] [Google Scholar]
- 17.Gemer O, Kruchkovich J, Huerta M, Kapustian V, Kroll D, Anteby E. Perioperative predictors of successful hysteroscopic endometrial ablation. Gynecol Obstet Invest. 2007;63:205–208. doi: 10.1159/000097847. [DOI] [PubMed] [Google Scholar]
- 18.Istre O, Skajaa K, Schjoensby AP, Forman A. Changes in serum electrolytes after transcervical resection of endometrium and submucous fibroids with use of glycine 1.5% for uterine irrigation. Obstet Gynecol. 1992;80:218–222. [PubMed] [Google Scholar]
- 19.Loffer FD. Endometrial ablation in patients with myomas. Curr Opin Obstet Gynecol. 2006;18:391–393. doi: 10.1097/01.gco.0000233932.06060.aa. [DOI] [PubMed] [Google Scholar]
- 20.Shamonki MI, Ziegler WF, Badger GJ, Sites CK. Prediction of endometrial ablation success according to perioperative findings. Am J Obstet Gynecol. 2000;182:1005–1007. doi: 10.1067/mob.2000.105393. [DOI] [PubMed] [Google Scholar]
- 21.Shaw RW, Symonds IM, Tamizian O, Chaplain J, Mukhopadhyay S. Randomised comparative trial of thermal balloon ablation and levonorgestrel intrauterine system in patients with idiopathic menorrhagia. Aust N Z J Obstet Gynaecol. 2007;47:335–340. doi: 10.1111/j.1479-828X.2007.00747.x. [DOI] [PubMed] [Google Scholar]
- 22.Davis JR, Maynard KK, Brainard CP, Purdon TF, Sibley MA, King DD. Effects of thermal endometrial ablation. Clinicopathologic correlations. Am J Clin Pathol. 1998;109:96–100. doi: 10.1093/ajcp/109.1.96. [DOI] [PubMed] [Google Scholar]
- 23.Istre O, Langebrekke A. Repeat hysteroscopic surgery reduces the hysterectomy rate after endometrial and myoma resection. J Am Assoc Gynecol Laparosc. 2003;10:247–251. doi: 10.1016/s1074-3804(05)60306-4. [DOI] [PubMed] [Google Scholar]
- 24.McCausland AM, McCausland VM. Long-term complications of endometrial ablation: cause, diagnosis, treatment, and prevention. J Minim Invasive Gynecol. 2007;14:399–406. doi: 10.1016/j.jmig.2007.04.004. [DOI] [PubMed] [Google Scholar]


