Abstract
OBJECTIVE:
The current study evaluates a treatment intervention developed with the goal of reducing symptoms of posttraumatic stress, depression, and anxiety in parents of premature infants.
METHODS:
A total of 105 mothers of preterm infants (25–34 weeks’ gestational age; >600 g) were randomized to receive a 6-session intervention developed to target parental trauma as well as facilitate infant redefinition (n = 62) or to an active comparison group (n = 43). Mothers in the intervention group received a combination of trauma-focused treatments, including psychoeducation, cognitive restructuring, progressive muscle relaxation, and development of their trauma narrative. The intervention also incorporated material targeting infant redefinition, defined as the process of changing the mother’s negative perceptions of her infant and the parenting experience.
RESULTS:
Mothers in the intervention group reported a greater reduction in both trauma symptoms (Cohen’s d = 0.41, P = .023) and depression (Cohen’s d = 0.59, P < .001) compared with the comparison group. Patients under both conditions improved significantly in terms of anxiety, with no differences between groups. Results of the moderator analysis showed that mothers with higher ratings of baseline NICU stress benefited more from the intervention compared with mothers who had lower ratings (P = .036).
CONCLUSIONS:
This short, highly manualized intervention for mothers of preterm infants statistically significantly reduced symptoms of trauma and depression. The intervention is feasible, can be delivered with fidelity, and has high ratings of maternal satisfaction. Given that improvements in mothers’ distress may lead to improved infant outcomes, this intervention has the potential for a high public health impact.
Keywords: intervention, neonatal intensive care, premature infants, posttraumatic stress disorder
What’s Known on This Subject:
Parents of premature infants are susceptible to developing trauma symptoms related to their NICU experience. There are no current well-established interventions that simultaneously address both parental trauma as well as redefinition of the parenting experience.
What This Study Adds:
A brief, cost-effective, and feasible manualized intervention for NICU parents was effective in reducing both parental trauma and depression. Implementation of this intervention in the NICU setting has the potential to improve maternal well-being and infant outcomes.
It has long been documented that parents react negatively to the NICU experience.1,2 The complex reactions of these parents include feelings of guilt, sadness over the loss of the “perfect” child, depression, and posttraumatic stress disorder (PTSD).1,3–5 Vanderbilt et al6 found that 23% of NICU mothers met criteria for acute stress disorder (ASD) while Pierrehumbert et al7 documented the presence of symptoms of PTSD in 41% of NICU parents up to 14 months after their infant’s birth. Data also suggest that up to 83% of mothers who experience significant trauma also endorse distorted views of their infants.8–10 Parents of preterm infants are more likely to show rigid, intrusive, and, later, overprotective parenting styles.11 In addition, many preterm infants seem to be less resilient and more dependent on optimal parenting to achieve their full developmental potential compared with term infants.12
Early interventions for parents with preterm infants have included supportive therapy and self-help techniques to address psychological distress.12–15 More recently, a small number of studies have evaluated intervention programs focused on reducing parent anxiety and trauma symptoms.16,17 However, studies in this population have not included the well-documented treatment components effective in treating PTSD or focused both on the trauma associated with a medically fragile infant and the loss of the expected parental role.2
Interventions have also been developed to help parental engagement with their premature infants.18 These interventions recognize that parents’ perceptions of their infants and parent–infant interactions are influenced by parental characteristics, including trauma.17,19–22 Meyer et al,23 for example, advocate a family-based psychosocial intervention focusing on infant redefinition and re-education of the parents. Meta-analyses of interventions to improve maternal sensitivity conclude that interventions are effective, particularly in mother–child dyads with high clinical need such as prematurity and that short, focused interventions are more effective than longer ones.24 However, to our knowledge, no current interventions combine treatment directed both at parental trauma as well as parent education/infant redefinition.
In our own research, we identified ASD in 44% of mothers of NICU infants as well as a strong relationship with PTSD symptoms 4 months after delivery.25,26 We have also tested a brief 3-session cognitive behavior therapy (CBT)-based intervention developed with the goal of reducing trauma symptoms in NICU parents.27 Given the promise of this short intervention, we expanded the intervention to include: (1) evidence-based treatments to target maternal trauma symptoms; (2) strategies to facilitate the process of infant redefinition by addressing negative perceptions of the infant and alterations in the expected parental role; and (3) guidance around evidence-based parenting approaches for the premature infant. Our hypothesis was that women receiving the intervention would have statistically significantly different self-ratings of trauma, depression, and anxiety symptoms compared with women in a comparison group immediately postintervention.
Methods
Subjects
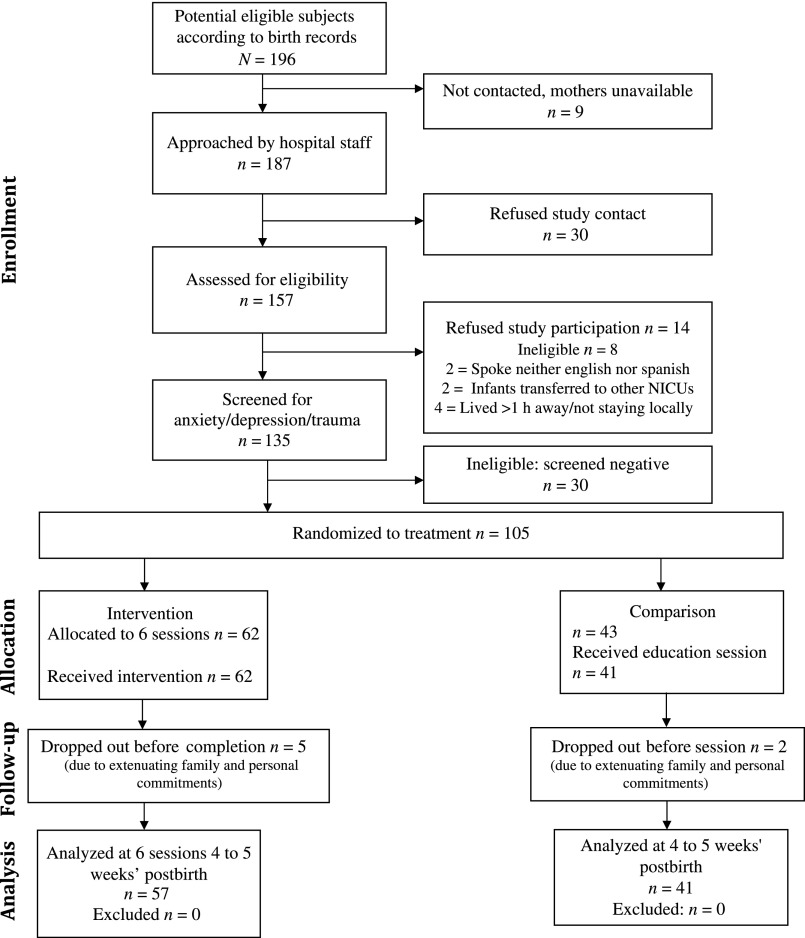
Subjects were 105 English- and Spanish-speaking mothers aged >18 years of infants 25 to 34 weeks’ gestational age and weighing >600 g born at or transferred to 1 of our 4 participating NICUs within the first week of delivery. Our population of interest was that of mothers who had potentially developed symptoms of trauma, anxiety, or depression as a result of having the traumatic experience of a premature birth and NICU hospitalization. Mothers of children with developmental abnormalities or awaiting cardiac surgery and those who were assessed as being unlikely to survive were excluded. Potential participants were informed about the study purpose, eligibility, and requirements. After completing the informed consent document, subjects were administered 3 screening instruments: the Beck Anxiety Inventory (BAI), the Beck Depression Inventory–Second Edition (BDI-II), and the Stanford Acute Stress Reaction Questionnaire (SASRQ). Individuals who reported a score of ≥3 on 2 or more of the questions in each ASD symptom category were considered to have screened positive for ASD. Women who scored above the clinical cutoff on any instrument (BDI-II score ≥20; BAI score ≥16; SASRQ score ≥3 for the required number of questions in 2 or more of the symptom categories) were invited into the intervention phase. Details of the recruitment process are shown in Fig 1.
FIGURE 1.
CONSORT diagram.
Study Design
The study was approved by the Stanford University institutional review board. Recruitment and delivery of the intervention took place between July 2011 and December 2012. A random number generator created by the statistician was used to assign eligible participants, unblinded, to receive either: (1) the manual-driven, CBT-based, trauma-focused plus mother redefinition/education intervention; or (2) an active comparison group. The project coordinator assigned subjects to the groups and allocated subjects to the interventionists. The intervention lasted 3 to 4 weeks with one or two 45- to 55-minute sessions administered weekly. Participants in both conditions were assessed at baseline (1–2 weeks after the birth of the infant) and 1 week after the completion of the intervention or 4 to 5 weeks’ postbirth for the comparison group.
Treatment Manual
The development and content of the 6-session treatment manual, which includes ratings of treatment fidelity and maternal satisfaction, has been previously described.28 Principles of trauma-focused CBT29 were incorporated with the expectation that reducing trauma-related symptoms would help mothers enhance their coping ability, feel more bonded to their infants, and improve their parenting ability. Sessions included: (1) psychoeducation to educate mothers about PTSD and common feelings and thoughts of NICU parents; (2) cognitive restructuring to help mothers recognize and challenge erroneous and maladaptive cognitions; (3) progressive muscle relaxation to reduce anxiety; and (4) development and processing of the mother’s trauma narrative. Two additional sessions, adapted with permission from the Creating Opportunities for Parent Empowerment program,30 were developed to enhance the mother–infant relationship by changing the mother’s negative perceptions of her infant and the parenting experience. This process, described as infant redefinition, is based on the assumption that if parents no longer view their child as abnormal and difficult, they will engage in more normative caregiving interactions.
Comparison Group
Participants in the information/usual care comparison group received one 45-minute information session on the policy, procedures, and environment of the NICU with education about parenting the premature infant. Mothers were referred to the existing parent mentor program for support and coping strategies to help ensure that the contact was similar to the intervention group and would approximate an attention-matched comparison condition. Mothers also received usual NICU care, including contacts with social workers, chaplaincy, and developmental psychologists.
Training and Supervision
Therapists were students from a clinical psychology graduate program and a NICU social worker. Therapists attended an 8-hour training during which they were educated about the specific goals of each session and role-played treatment sessions. Treatment fidelity to all components of the intervention, as measured by the therapists’ adherence to the written manual, was high both across sessions and across therapists.28 The intraclass correlation between raters varied between 0.78 and 0.80 (P < .001), which is considered a high level of reliability.31
Measures
Sociodemographic Characteristics
Sociodemographic data, including age, race, ethnicity, primary language, country of birth, education, income, number of children, previous premature births, and marital status, were assessed at baseline.
Traumatic Events Questionnaire
The Traumatic Events Questionnaire is an 11-item questionnaire that is administered at baseline and used to assess specific trauma experiences capable of eliciting posttraumatic stress symptoms.32 The 2-week test–retest reliability for number of events is 0.91, and for specific events, it ranges from 0.72 to 1.0.
Davidson Trauma Scale
The Davidson Trauma Scale (DTS) is a 17-item scale, administered at baseline and follow-up, that is used to assess Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision (DSM-IV-TR), symptoms of PTSD.33 The scale has solid test–retest reliability (R = 0.86) and internal consistency (r = 0.99). At a score of 4, the DTS achieves an 83% diagnostic accuracy with the Structured Clinical Interview for DSM-IV.
Stanford Acute Stress Reaction Questionnaire
The SASRQ is a 30-item self-report questionnaire used to assess DSM-IV-TR symptoms of ASD34; it was administered at baseline. Psychometric properties of the SASRQ show good internal consistency, test–retest reliability, and predictive validity.
Parental Stressor Scale: Neonatal Care Unit
The Parental Stressor Scale: Neonatal Care Unit (PSS: NICU35) is a 34-item scale administered at baseline. It is use to evaluate parents’ perceptions of the stressors due to the infants’ NICU stay in 3 areas: physical environment of the NICU, infant behavior/appearance, and alterations in parental role. The PSS: NICU is internally consistent (>0.70 for all scales).
Beck Depression Inventory–Second Edition
The BDI-II36 is a 21-item questionnaire that was administered at baseline and follow-up. It is used to assess depressive symptoms and has a reliability of 0.92.
Beck Anxiety Inventory
The BAI37 is a 21-item self-report measure, administered at baseline and follow-up, to assess symptoms of anxiety. The scale has good internal consistency and 1-week test–retest reliability of 0.75.
Mini–International Neuropsychiatric Interview
The Mini–International Neuropsychiatric Interview38 is a structured interview diagnosis, administered at baseline and follow-up. It was used to establish the DSM-IV-TR diagnoses of major depressive episode, any anxiety disorder, and PTSD. A multicenter study that compared the diagnoses by general practitioners obtained according to this structured interview versus the diagnoses obtained by psychiatrists according to nonstructured interviews obtained a κ coefficient between 0.41 and 0.68, sensitivity between 0.41 and 0.86, and specificity between 0.84 and 0.97.
Illness Health Severity Index
The illness health severity index is a probability of death index (range: 0–1) that was calculated by using a multivariable risk adjustment model. The index was designed to capture important factors related to patient risk based on the Vermont Oxford Network model39,40 by using modifications tailored to the California Perinatal Quality Care Collaborative data. The model includes terms for gestational age, gestational age squared, race, gender, location of birth, multiple birth, prenatal care, 5-minute Apgar score, small size for gestational age (lowest 10th percentile), major birth defect, and California Children’s Services NICU level. The NICU level is determined by using modifications tailored to the database according to a regional NICU comparison chart.
Analyses
Means and SDs were used to summarize continuous variables, and counts and proportions were used to summarize categorical measures. Two-sample t tests (for continuous variables) and χ2 tests (for categorical variables) were used to compare baseline measures across the intervention and comparison groups (2-sided, α = .05). A standard linear mixed effects modeling41,42 was used to formally model the change from the preintervention to the postintervention assessment. Specifically, we used a random intercept model assuming a linear trend over time. In line with the intention-to-treat principle, we included all randomized individuals in the analyses for whom data were available from at least 1 of the 2 assessments (preintervention and/or postintervention). Data points that were not available were treated as missing at random conditional on observed information according to a maximum likelihood estimation.43 All 105 individuals randomized either to the intervention (n = 62) or to the comparison condition (n = 43) were included in the mixed effects modeling. The retention rate was high in both groups. At the time of the postintervention assessment, there were 5 dropouts (8%) who were assigned to the intervention and 2 dropouts (5%) who were assigned to the comparison group. We incorporated the MacArthur framework44,45 into this longitudinal modeling framework for our exploratory moderator analysis. In our longitudinal context, the change (slope) from preintervention to postintervention is treated as the outcome in the moderator analysis. The Mplus46 Program version 7 was used to conduct the maximum likelihood estimation for all of the longitudinal mixed effects analyses.
Results
Baseline Characteristics
Baseline demographic and clinical features of mothers and infants are shown in Table 1. There were no statistical differences between the intervention and comparison groups on most baseline variables, including ratings of trauma (SASRQ and DTS), anxiety (BAI) and depression (BDI-II), previous trauma history (Traumatic Events Questionnaire), and current psychiatric diagnoses of major depression, dysthymia, or anxiety. With the exception of maternal age, there were no differences in the sociodemographic variables. Neither group experienced any adverse events during the course of the intervention. Mothers assigned to the intervention group rated their overall NICU experience (PSS: NICU global index) as being more stressful compared with the comparison mothers (P = .02) in addition to having higher ratings on the PSS: NICU subscales of infant behavior/appearance and alteration in parental role.
TABLE 1.
Demographic and Baseline Clinical Characteristics (N = 105)
| Baseline Characteristic | Intervention (n = 62) | Comparison (n = 43) | Group Difference |
|---|---|---|---|
| DTS | 49.40 ± 25.49 | 42.35 ± 27.05 | t(103) = 1.360 |
| BDI-II | 20.60 ± 9.48 | 17.49 ± 10.68 | t(103) = 1.568 |
| BAI | 21.97 ± 11.83 | 20.30 ± 12.49 | t(103) = 0.693 |
| Infant gestational age, wk | 30.90 ± 3.00) | 31.56 ± 2.60 | t(103) = 1.161 |
| Infant severity score | 0.047 ± 0.05 | 0.034 ± 0.03 | t(103) = 1.438 |
| Mother's age, y | 33.76 ± 6.25 | 30.70 ± 5.50 | t(103) = 2.590 |
| Length of stay, d | 52.60 ± 32.23 | 42.56 ± 33.69 | t(103) = 1.541 |
| Mother's education less than college degree | 19 (30.6) | 19 (44.2) | χ2(1) = 2.016 |
| Mother's race, white (vs non-white) | 42 (67.7) | 22 (51.2) | χ2(1) = 2.932 |
| Mother's ethnicity, Hispanic (vs non-Hispanic) | 16 (25.8) | 14 (32.6) | χ2(1) = 0.567 |
| Mother is US born | 37 (59.7) | 23 (53.5) | χ2(1) = 0.397 |
| Married/partnered (vs single/divorced) | 58 (93.5) | 43 (100) | χ2(1) = 2.884 |
| Household incomea | |||
| <$50 000 | 15 (25.0) | 9 (25.7) | χ2(1) = 0.006 |
| $50 000–$99 000 | 10 (16.7) | 5 (14.3) | χ2(1) = 0.094 |
| ≥$100 000 | 35 (58.3) | 21 (60.0) | χ2(1) = 0.025 |
| Interview in English (vs Spanish) | 55 (88.7) | 37 (86.0) | χ2(1) = 0.166 |
| Trauma Events Questionnaire | 31 (50.0) | 14 (32.6) | χ2(1) = 3.154 |
| SASRQ | 56 (90.3) | 40 (93.0) | χ2(1) = 0.236 |
| PSS: NICU | |||
| Global index | 3.02 ± 0.72 | 2.65 ± 0.86 | t(103) = 2.369 |
| Sights and sounds of the NICU | 2.88 ± 0.84 | 2.66 ± 1.12 | t(103) = 1.150 |
| Infant behavior and appearance | 3.12 ± 0.96 | 2.58 ± 1.00 | t(103) = 2.794 |
| Alteration in parental role | 3.86 ± 0.82 | 3.48 ± 1.11 | t(103) = 2.012 |
| MINI | |||
| Current major depressive episode | 51 (82.3) | 36 (83.7) | χ2(1) = 0.038 |
| Dysthmia | 2 (5.4) | 1 (3.4) | χ2(1) = 0.144 |
| Current anxiety disorder | 7 (11.3) | 2 (4.7) | χ2(1) = 1.428 |
Data are presented as mean ± SD or n (%). MINI, Mini–International Neuropsychiatric Interview.
Ten subjects (8 control, 2 intervention) with missing income information were not included.
Primary Outcomes
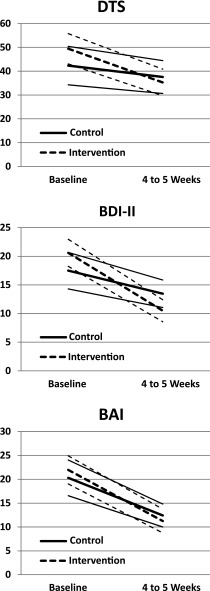
Figure 2 shows longitudinal trajectories of primary (DTS) and secondary (BDI-II, BAI) outcomes. Scores on the DTS and BDI-II declined significantly more over time for mothers in the intervention group compared with those in the comparison group. By contrast, although both groups showed a significant decline in their scores on the BAI, the rate and magnitude of the change were not statistically significantly different between the groups.
FIGURE 2.
Longitudinal trajectories of primary and secondary outcomes (based on observed means by using all available cases at each assessment. At baseline, n = 43 for the comparison group and n = 62 for the intervention group. At 4 to 5 weeks, n = 41 for the comparison group and n = 57 for the intervention group. The thick lines represent means, and the thin lines represent 95% confidence bands.
Table 2 summarizes the results of the longitudinal analyses by using mixed effects modeling. Mothers under both conditions improved significantly on trauma symptoms (DTS). There was a significant moderate effect of the intervention on DTS scores (Cohen’s d = 0.41, P = .023). Mothers’ depression symptoms improved significantly under both conditions. As with trauma, BDI-II scores declined more under the intervention compared with the comparison condition (Cohen’s d = 0.59, P < .001). Patients under both conditions improved significantly in terms of anxiety (BAI). However, unlike for the DTS and BDI-II, the rate of decline was similar across the 2 conditions. To test the sensitivity of our results to the presence or absence of these baseline covariates, we compared the analysis with and without controlling for these baseline covariates. The differences between the 2 analyses were minimal and did not affect our conclusions with respect to the main outcome variables.
TABLE 2.
Estimated Change From Baseline to Postintervention Based on Mixed Effects Longitudinal Analysis
| Variable | Intervention | Comparison | Group Difference |
|---|---|---|---|
| DTS | |||
| Change | –12.886 | –5.509 | –7.378 |
| 95% CI | –17.413 to –8.359 | –10.732 to –0.285 | –13.724 to –1.032 |
| Effect sizea | – | – | –0.412 |
| BDI-II | |||
| Change | –9.343 | –4.991 | –4.352 |
| 95% CI | –11.236 to –7.450 | –7.128 to –2.854 | –6.791 to –1.914 |
| Effect sizea | – | –0.586 | |
| BAI | |||
| Change | –10.237 | –8.562 | –1.675 |
| 95% CI | –12.912 to –7.563 | –11.545 to –5.580 | –4.939 to 1.588 |
| Effect sizea | – | – | –0.160 |
CI, confidence interval.
Estimated slope difference/estimated SD of the slope, where SD = square root of the estimated variance pooled across the control and intervention conditions.
Moderator Variables
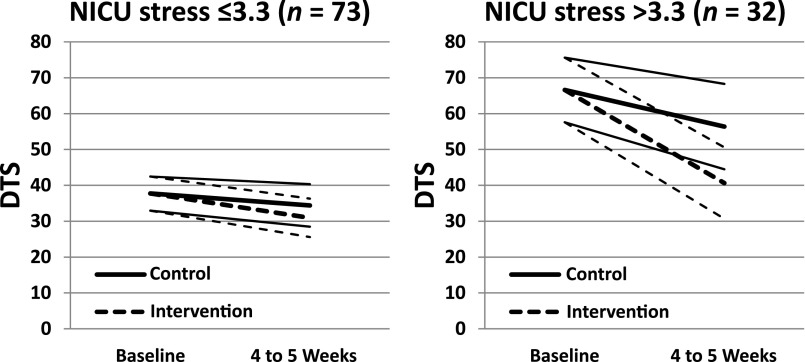
We examined potential moderators of the intervention effect on DTS scores, our primary outcome measure. Eleven baseline variables were considered to be potential moderators (infant illness severity index, length of stay, Traumatic Events Questionnaire, PSS: NICU global index, current major depressive episode, maternal education, maternal age, income, white/non-white race, Hispanic ethnicity, and US born), as described in Table 1. The analytical criteria used for detecting moderators conformed to the MacArthur approach.44,45 According to our mixed effects modeling, in which the key parameter of interest was the effect of the interaction between the intervention status and a potential moderator on the change in DTS, the global rating of NICU stress assessed by using the PSS: NICU was identified as a moderator of treatment effect on the DTS (P = .036). To further explore the differential effect of treatment depending on the ratings of baseline NICU stress, subjects were dichotomized into the top 30% and the bottom 70% based on their responses on the PSS: NICU. Figure 3 shows that mothers with higher ratings of baseline NICU stress benefited more from the intervention compared with mothers with lower ratings of baseline NICU stress.
FIGURE 3.
Baseline NICU stress moderating the effect of intervention on DTS decline; DTS trajectories are based on mixed effects growth model estimates. The thick lines represent means, and the thin lines represent 95% confidence bands. The moderator analysis was conducted by using the continuous NICU stress measure. The score was split into 2 categories in the graphic to help readers visualize the moderating effect of NICU stress.
Among the 11 baseline variables examined as potential moderators, mother’s education and household income were found to be nonspecific predictors of the outcome (ie, they predicted outcome regardless of which intervention they received). Less educated mothers (P ≤ .001) and mothers with lower household income (P = .025) showed a greater decline in DTS irrespective of whether they were in the intervention or comparison group.
Discussion
The primary finding of the current study was that a brief, 6-session intervention based on principles of trauma-focused CBT paired with techniques developed to help enhance parenting confidence and alter negative parental perceptions of their premature infant was successful in reducing maternal symptoms of trauma and depression 4 to 5 weeks after their infant’s birth. Mothers who received the intervention had significantly lower scores on both the DTS (P = .02) and the BDI-II (P < .001) compared with mothers in the comparison group. The study is unique in that it integrates trauma-focused treatment with interventions previously found to be useful in enhancing parenting skills and infant outcomes in premature infants.47
Results also showed a significant decline in maternal ratings of anxiety for both intervention and comparison groups. This finding is consistent with previous research showing a decrease in anxiety and depression in parents of premature infants over time, even without intervention.48 However, it is important to note that the comparison group in our study was an active comparison group and not a passive control. Subjects in the comparison group received a combination of parent education and training in ways to negotiate the NICU environment. However, the failure of the comparison condition to produce comparable changes in trauma symptoms is consistent with findings showing that educational measures alone are insufficient to diminish trauma symptoms.
Results of the moderator analysis indicate that none of the sociodemographic variables had any effect on the response to the intervention, suggesting that the intervention is effective and applicable for individuals of differing ethnic backgrounds and socioeconomic status. The severity of the infant’s medical condition and previous maternal psychiatric or trauma history similarly failed to influence the response to treatment. However, maternal rating of overall NICU stress was found to be a significant moderator of the treatment effect. The analysis found that the intervention was most effective for mothers who had the highest ratings of NICU stress, suggesting that mothers who rate the NICU experience as being particularly stressful were more likely to report benefits from participation. Thus, although the intervention was broadly successful in addressing trauma symptoms in a cross-section of participants, results show that women in the top one-third of the sample with respect to ratings of parental stress are most likely to show improvements in their trauma symptoms. This finding suggests that the intervention may be more applicable for highly stressed mothers, which is consistent with principles of stepped-care intervention programs for PTSD as proposed by Zatzick et al.49 Finally, with respect to the moderator analysis, less educated mothers and mothers with lower household income reported a greater decline in DTS scores irrespective of whether they were in the intervention or comparison group. This finding is consistent with work from our group showing that more highly educated women are at greater risk of PTSD in the NICU setting.50
The efficacy of our brief intervention has several potentially important clinical implications for NICU care. The findings that >90% of mothers completed all 6 sessions and were satisfied with the treatment suggest that this intervention can be successfully implemented in the NICU. The entire intervention is manualized; it can be easily taught to individuals without specialized training in psychological treatments; and treatment fidelity, as measured by the therapists’ adherence to the written manual, was high both across sessions and across therapists.28
Data from other settings have suggested a relationship between disturbances of attachment and traumatic stress reactions in mothers with a history of interpersonal violence. Schechter and Willheim51 found that greater severity of maternal PTSD was associated with lower maternal baseline salivary cortisol levels and greater likelihood of distorted, inflexible, and negative mental representations of the child. Limited research on parents of preterm infants and parental traumatization suggest that up to 83% of mothers who experience significant trauma endorse distorted views of their infants.1,9,10 Negative or traumatic experiences of delivery have also been associated with eating and sleeping problems in preterm infants,8 and maternal psychological distress of the mother has been associated with subsequent emotional and behavioral problems of the child.52,53 Thus, successful intervention to reduce parental trauma in the NICU setting may have important implications for subsequent child development.
There are several limitations to the study. The sample size was relatively small and although representative of the population in our hospital catchment area, African-American mothers were underrepresented. As a result, it is unknown whether the findings of the study would be generalizable to other ethnic groups. However, although our sample was skewed toward mothers of high socioeconomic status, the moderator analysis did not show any effect of maternal age, education, income, or ethnicity on the response to the intervention. Additional limitations include that, similar to many previous NICU interventions, fathers were not included in the sample; outcome data were based on self-report; and the data were short-term in nature. Finally, although the results are encouraging, they can only be generalized to the population of highly stressed NICU mothers who screened positive for inclusion in the study.
Conclusions
Our data found that a short, highly manualized intervention for mothers of preterm infants statistically significantly reduced symptoms of trauma and depression. The intervention is feasible in busy NICUs and had high ratings of maternal satisfaction. Given that improvements in mothers’ distress may lead to improved infant outcomes, this intervention has the potential for high public health impact.
Acknowledgments
We acknowledge the contributions of Drs Kimberly Yonkers and Patricia Chamberlain from our Scientific Advisory Group and Dr Nancy Feinstein.
Glossary
- ASD
acute stress disorder
- BAI
Beck Anxiety Inventory
- BDI-II
Beck Depression Inventory–Second Edition
- CBT
cognitive behavioral therapy
- DSM-IV-TR
Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision
- DTS
Davidson Trauma Scale
- PSS: NICU
Parental Stressor Scale: Neonatal Care Unit
- PTSD
posttraumatic stress disorder
- SASRQ
Stanford Acute Stress Reaction Questionnaire
Footnotes
Dr Shaw conceptualized and designed the study and drafted the initial manuscript; Dr St John contributed to the manual development, supervised the infant sessions, and reviewed and revised the manuscript; Ms Lilo contributed to the manual development, coordinated and supervised the data collection, and reviewed and revised the manuscript; Dr Jo participated in writing the proposal, carried out and drafted the data analysis, and reviewed and revised the manuscript; Dr Benitz facilitated the implementation of the study and reviewed and revised the manuscript; Dr Stevenson participated in the planning of the study, facilitated the implementation of the study, and reviewed and revised the manuscript; Dr Horwitz conceptualized and designed the study, collaborated on the data analysis, and reviewed and revised the manuscript; and all authors approved the final manuscript as submitted.
This trial has been registered at www.clinicaltrials.gov (identifier NCT01307293).
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: Supported by National Institutes of Mental Health grant R34-MH086579A to Drs Shaw and Horwitz and National Center for Research Resources and the National Center for Advancing Translational Sciences, National Institutes of Health, through grant UL1 RR025744. Funded by the National Institutes of Health (NIH).
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
References
- 1.Miles MS. Parents of critically ill premature infants: sources of stress. Crit Care Nurs Q. 1989;12(3):69–74 [DOI] [PubMed] [Google Scholar]
- 2.Tarkan L. For parents on NICU, trauma may last. New York Times Available at: www.nytimes.com/2009/08/25/health/25trau.html?pagewanted=all&_r=0. Accessed August 7, 2013
- 3.Kersting A, Dorsch M, Wesselmann U, et al. Maternal posttraumatic stress response after the birth of a very low-birth-weight infant. J Psychosom Res. 2004;57(5):473–476 [DOI] [PubMed] [Google Scholar]
- 4.Holditch-Davis D, Bartlett TR, Blickman AL, Miles MS. Posttraumatic stress symptoms in mothers of premature infants. J Obstet Gynecol Neonatal Nurs. 2003;32(2):161–171 [DOI] [PubMed] [Google Scholar]
- 5.Peebles-Kleiger MJ. Pediatric and neonatal intensive care hospitalization as traumatic stressor: implications for intervention. Bull Menninger Clin. 2000;64(2):257–280 [PubMed] [Google Scholar]
- 6.Vanderbilt D, Bushley T, Young R, Frank DA. Acute posttraumatic stress symptoms among urban mothers with newborns in the neonatal intensive care unit: a preliminary study. J Dev Behav Pediatr. 2009;30(1):50–56 [DOI] [PubMed] [Google Scholar]
- 7.Pierrehumbert B, Nicole A, Muller-Nix C, Forcada-Guex M, Ansermet F. Parental post-traumatic reactions after premature birth: implications for sleeping and eating problems in the infant. Arch Dis Child Fet Neonatal Ed. 2003;88(5):F400–F404 [DOI] [PMC free article] [PubMed]
- 8.Cohen LR, Hien DA, Batchelder S. The impact of cumulative maternal trauma and diagnosis on parenting behavior. Child Maltreat. 2008;13(1):27–38 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ross LE, McLean LM. Anxiety disorders during pregnancy and the postpartum period: a systematic review. J Clin Psychiatry. 2006;67(8):1285–1298 [DOI] [PubMed] [Google Scholar]
- 10.Schechter DS, Coots T, Zeanah CH, et al. Maternal mental representations of the child in an inner-city clinical sample: violence-related posttraumatic stress and reflective functioning. Attach Hum Dev. 2005;7(3):313–331 [DOI] [PubMed] [Google Scholar]
- 11.Wightman A, Schluchter M, Drotar D, et al. Parental protection of extremely low birth weight children at age 8 years. J Dev Behav Pediatr. 2007;28(4):317–326 [DOI] [PubMed] [Google Scholar]
- 12.Minde K. Prematurity and serious medical conditions in infancy: implications for development, behavior, and intervention. In: Zeanah C, ed. Handbook of Infant Mental Health. 2nd ed. New York, NY: Guilford Press; 2000:176–194 [Google Scholar]
- 13.Preyde M, Ardal F. Effectiveness of a parent “buddy” program for mothers of very preterm infants in a neonatal intensive care unit. CMJA. 2003;168(8):969–973 [PMC free article] [PubMed]
- 14.Roman LA, Lindsay JK, Boger RP, et al. Parent-to-parent support initiated in the neonatal intensive care unit. Res Nurs Health. 1995;18(5):385–394 [DOI] [PubMed] [Google Scholar]
- 15.Anderson GC, Chiu SH, Dombrowski MA, Swinth JY, Albert JM, Wada N. Mother-newborn contact in a randomized trial of kangaroo (skin-to-skin) care. J Obstet Gynecol Neonatal Nurs. 2003;32(5):604–611 [DOI] [PubMed] [Google Scholar]
- 16.Jotzo M, Poets CF. Helping parents cope with the trauma of premature birth: an evaluation of a trauma-preventive psychological intervention. Pediatrics. 2005;115(4):915–919 [DOI] [PubMed] [Google Scholar]
- 17.Kaaresen PI, Rønning JA, Tunby J, Nordhov SM, Ulvund SE, Dahl LB. A randomized controlled trial of an early intervention program in low birth weight children: outcome at 2 years. Early Hum Dev. 2008;84(3):201–209 [DOI] [PubMed] [Google Scholar]
- 18.Harrison L, Lotas M, Jorgensen K. Environmental issues. In: Kenner C, McGrath J, eds. Developmental Care of Newborns and Infants. St. Louis, MO: Mosby Inc; 2004:229–262 [Google Scholar]
- 19.Als H, Duffy FH, McAnulty GB, et al. Early experience alters brain function and structure. Pediatrics. 2004;113(4):846–857 [DOI] [PubMed] [Google Scholar]
- 20.Brisch KH, Bechinger D, Betzler S, Heinemann H. Early preventive attachment-oriented psychotherapeutic intervention program with parents of a very low birthweight premature infant: results of attachment and neurological development. Attach Hum Dev. 2003;5(2):120–135 [DOI] [PubMed] [Google Scholar]
- 21.Browne JV, Talmi A. Family-based intervention to enhance infant-parent relationships in the neonatal intensive care unit. J Pediatr Psychol. 2005;30(8):667–677 [DOI] [PubMed] [Google Scholar]
- 22.Melnyk BM, Feinstein NF, Alpert-Gillis L, et al. Reducing premature infants’ length of stay and improving parents’ mental health outcomes with the Creating Opportunities for Parent Empowerment (COPE) neonatal intensive care unit program: a randomized, controlled trial. Pediatrics. 2006;118(5) [DOI] [PubMed] [Google Scholar]
- 23.Meyer EC, Zeanah CH, Boukydis CFZ, Lester BM. A clinical interview for parents of high-risk infants: concept and applications. Infant Ment Health J. 1993;14(3):192–207 [Google Scholar]
- 24.Bakermans-Kranenburg MJ, van IJzendoorn MH, Juffer F. Less is more: meta-analyses of sensitivity and attachment interventions in early childhood. Psychol Bull. 2003;129(2):195–215 [DOI] [PubMed] [Google Scholar]
- 25.Shaw RJ, Deblois T, Ikuta L, Ginzburg K, Fleisher B, Koopman C. Acute stress disorder among parents of infants in the neonatal intensive care nursery. Psychosomatics. 2006;47(3):206–212 [DOI] [PubMed] [Google Scholar]
- 26.Shaw RJ, Bernard RS, Deblois T, Ikuta LM, Ginzburg K, Koopman C. The relationship between acute stress disorder and posttraumatic stress disorder in the neonatal intensive care unit. Psychosomatics. 2009;50(2):131–137 [DOI] [PubMed] [Google Scholar]
- 27.Bernard RS, Williams SE, Storfer-Isser A, et al. Brief cognitive-behavioral intervention for maternal depression and trauma in the neonatal intensive care unit: a pilot study. J Trauma Stress. 2011;24(2):230–234 [DOI] [PubMed] [Google Scholar]
- 28.Shaw RJ, Brecht CJ, St John N, et al. Prevention of postpartum traumatic stress in mothers with preterm infants: manual development and evaluation. Issues Ment Health Nurs. 2013;34(8):578–586 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Nemeroff CB, Bremner JD, Foa EB, Mayberg HS, North CS, Stein MB. Posttraumatic stress disorder: a state-of-the-science review. J Psychiatr Res. 2006;40(1):1–21 [DOI] [PubMed] [Google Scholar]
- 30.Melnyk BM, Alpert-Gillis L, Feinstein NF, et al. Improving cognitive development of low-birth-weight premature infants with the COPE program: a pilot study of the benefit of early NICU intervention with mothers. Res Nurs Health. 2001;24(5):373–389 [DOI] [PubMed] [Google Scholar]
- 31.Kraemer HC, Lowe Kraemer K, Kupfer DJ. To Your Health: How to Understand What Research Tells Us About Risk. New York, NY: Oxford University Press; 2003 [Google Scholar]
- 32.Vrana S, Lauterbach D. Prevalence of traumatic events and post-traumatic psychological symptoms in a nonclinical sample of college students. J Trauma Stress. 1994;7(2):289–302 [DOI] [PubMed] [Google Scholar]
- 33.Davidson JR, Book SW, Colket JT, et al. Assessment of a new self-rating scale for post-traumatic stress disorder. Psychol Med. 1997;27(1):153–160 [DOI] [PubMed] [Google Scholar]
- 34.Cardeña E, Koopman C, Classen C, Waelde LC, Spiegel D. Psychometric properties of the Stanford Acute Stress Reaction Questionnaire (SASRQ): a valid and reliable measure of acute stress. J Trauma Stress. 2000;13(4):719–734 [DOI] [PubMed] [Google Scholar]
- 35.Miles MS, Funk SG, Carlson J. Parental Stressor Scale: neonatal intensive care unit. Nurs Res. 1993;42(3):148–152 [PubMed] [Google Scholar]
- 36.Beck AT, Steer RA, Brown GK. Beck Depression Inventory-II (BDI-II). San Antonio, TX: Psychological Corporation; 1996 [Google Scholar]
- 37.Beck AT, Epstein N, Brown G, Steer RA. An inventory for measuring clinical anxiety: psychometric properties. J Consult Clin Psychol. 1988;56(6):893–897 [DOI] [PubMed] [Google Scholar]
- 38.Sheehan DV, Lecrubier Y, Sheehan KH, et al. The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. 1998;59(20 suppl 20):22–33, quiz 34–57 [PubMed] [Google Scholar]
- 39.Horbar JD. The Vermont Oxford Network: evidence-based quality improvement for neonatology. Pediatrics. 1999;103(1 suppl E):350–359 [PubMed] [Google Scholar]
- 40.Zupancic JA, Richardson DK, Horbar JD, Carpenter JH, Lee SK, Escobar GJ. Vermont Oxford Network SNAP Pilot Project Participants. Revalidation of the score for neonatal acute physiology in the Vermont Oxford Network. Pediatrics. 2007;119(1) [DOI] [PubMed] [Google Scholar]
- 41.Raudenbush S, Bryk A. Hierarchical Linear Models: Applications and Data Analysis Methods. Thousand Oaks, CA: Sage; 2002 [Google Scholar]
- 42.Singer JD, Willett JB. Applied Longitudinal Data Analysis: Modeling Change and Event Occurrence. New York, NY: Oxford University Press; 2003 [Google Scholar]
- 43.Little RJA, Rubin DB. Statistical Analysis With Missing Data. New York, NY: J Wiley & Sons; 2002 [Google Scholar]
- 44.Kraemer HC, Wilson GT, Fairburn CG, Agras WS. Mediators and moderators of treatment effects in randomized clinical trials. Arch Gen Psychiatry. 2002;59(10):877–883 [DOI] [PubMed] [Google Scholar]
- 45.Kraemer HC, Kiernan M, Essex M, Kupfer DJ. How and why criteria defining moderators and mediators differ between the Baron & Kenny and MacArthur approaches. Health Psychol. 2008;27(2 suppl):S101–S108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Muthén LK, Muthén BO. MPlus User's Guide, Seventh Edition [computer program]. Los Angeles, CA: Muthén & Muthén 1998–2012. Available at: www.statmodel.com/download/usersguide/Mplus%20user%20guide%20Ver_7_r6_web.pdf. Accessed August 7, 2013
- 47.Als H, Gilkerson L, Duffy FH, et al. A three-center, randomized, controlled trial of individualized developmental care for very low birth weight preterm infants: medical, neurodevelopmental, parenting, and caregiving effects. J Dev Behav Pediatr. 2003;24(6):399–408 [DOI] [PubMed] [Google Scholar]
- 48.Carter JD, Mulder RT, Frampton CM, Darlow BA. Infants admitted to a neonatal intensive care unit: parental psychological status at 9 months. Acta Paediatr. 2007;96(9):1286–1289 [DOI] [PubMed] [Google Scholar]
- 49.Zatzick D, Roy-Byrne P, Russo J, et al. A randomized effectiveness trial of stepped collaborative care for acutely injured trauma survivors. Arch Gen Psychiatry. 2004;61(5):498–506 [DOI] [PubMed] [Google Scholar]
- 50.Shaw RJ, Bernard RS, Storfer-Isser A, Rhine W, Horwitz SM. Parental coping in the neonatal intensive care unit. J Clin Psychol Med Settings. 2013;20(2):135–142 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Schechter DS, Willheim E. When parenting becomes unthinkable: intervening with traumatized parents and their toddlers. J Am Acad Child Adolesc Psychiatry. 2009;48(3):249–253 [DOI] [PubMed] [Google Scholar]
- 52.McCormick MC, Workman-Daniels K, Brooks-Gunn J. The behavioral and emotional well-being of school-age children with different birth weights. Pediatrics. 1996;97(1):18–25 [PubMed] [Google Scholar]
- 53.Miceli PJ, Goeke-Morey MC, Whitman TL, Kolberg KS, Miller-Loncar C, White RD. Brief report: birth status, medical complications, and social environment: individual differences in development of preterm, very low birth weight infants. J Pediatr Psychol. 2000;25(5):353–358 [DOI] [PubMed] [Google Scholar]