Abstract
BACKGROUND AND OBJECTIVE:
Advanced understanding of modifiable predictors of health care use in pediatric chronic illness is critical to reducing health care costs. We examined the relationship between medication non-adherence and health care use in children and adolescents who have a chronic medical condition.
METHODS:
A systematic review of articles by using PubMed, PsycINFO, and CINAHL was conducted. Additional studies were identified by searching reference sections of relevant manuscripts. Studies that tested the relationship between medication non-adherence and health care use (ie, hospitalizations, emergency department visits, outpatient visits) or cost in children and adolescents (mean age ≤18 years) who have a chronic medical condition were included. Extraction of articles was completed by using predefined data fields.
RESULTS:
Ten studies met our inclusion criteria. Nine of the 10 studies reviewed (90%) demonstrated a relationship between medication non-adherence and increased health care use. The directionality of this relationship varied depending on the outcome variable of interest.
CONCLUSIONS:
Medication non-adherence is related to increased health care use in children and adolescents who have a chronic medical condition and should be addressed in clinical care. Future studies should include randomized controlled trials examining the impact of adherence promotion efforts on health care use and costs.
Keywords: medication adherence; health care costs; health care quality, access, and evaluation; chronic disease
In 2010, the United States spent $2.6 trillion on health care, an increase of 3.9% from 2009, and 17.9% of its gross domestic product.1 Hospital care and physician and clinical services (ie, emergency department [ED] visits, hospitalizations, and office visits, hereafter defined as “health care use”) are the 2 largest components of health care spending,2,3 and accounted for over 50% of the growth in health care spending from 2009 to 2010.1 Continued rising health care costs despite the recession, the increasing US national deficit, and the increasing percentage of US health spending financed by the government ($1.2 trillion, 45% of all US health spending) have prompted investigation of modifiable factors to reduce health care use and associated costs.4 Although there is no single strategy for effectively controlling costs, researchers have begun to focus on the 83% of health care resources consumed by individuals who have a chronic medical condition.4,5
The number of children and adolescents diagnosed with a chronic medical condition has been steadily increasing over the past 20 years,6 driven in part by increases in the prevalence of obesity7 and asthma8 as well as advances in medical care that increase survival (eg, cystic fibrosis, kidney transplant).9,10 Increases in the prevalence of chronic medical conditions have only increased the already disproportionate health care expenses accounted for by children and adolescents who have a chronic illness.5,11,12 In 2000, children and adolescents with a special health care need made up 16% of youth but accounted for 53% of hospital days.13 Consequently, targeting factors that influence health care use in this population may provide 1 of the greatest opportunities to reduce pediatric health care spending.
Non-adherence refers to a lack of correspondence between patient self-management behavior and medical or health advice14 and significantly contributes to health care use in adults who have a chronic illness,15–18 accounting for an estimated 33% to 69% of adult hospital admissions and $100 to $300 billion in annual health care costs.19,20 Because much of the health care use attributable to non-adherence includes excess use of urgent care and hospitalizations for preventable complications,16 it represents avoidable costs, an ideal target outcome for interventions aimed at reducing health care spending. As non-adherence is modifiable with intervention,21 adult adherence promotion efforts have begun to focus on both improving health status and reducing health care use, resulting in programs that effectively decrease health care costs.15
Efforts to contain pediatric health care costs could prove to be equally as effective as adult-focused interventions, but have not yet been examined despite the widespread nature of non-adherence in pediatrics. Approximately 63% of children and adolescents who have a chronic illness are prescribed medication,22 but 50% to 88% of children and adolescents are non-adherent to their prescribed regimens.23–25 As in adult samples, pediatric non-adherence may be a modifiable predictor of health care use and resulting health care costs. For example, an adolescent who has asthma may require hospitalization after failing to take his controller medication for several days and suffering an exacerbation. If his medical care included regular assessments of his adherence and adherence promotion efforts as necessary, this hospitalization and its associated costs may have been avoided.16,26
Understanding the impact of adherence promotion interventions on health care costs specific to pediatric populations is necessary given the numerous developmental factors that make pediatric adherence unique (ie, influence of adult caregivers and systems on adherence, evolution of illness burden with age, increasing autonomy for disease management) and the variations in health care systems and outcomes across the lifespan. For example, health care financing for over one-third of children and adolescents is provided by Medicaid and Children’s Health Insurance Programs.27 With inconsistencies in benefits and reimbursement rates between states, it is difficult to compare health care costs across pediatric and adult samples. Furthermore, given the more advanced disease course and higher likelihood of complications experienced by adults who have a chronic illness, the benefits in quality of life and cost savings resulting from pediatric prevention efforts are likely to be less visible in short-term evaluations typically used with these populations.28
An increased understanding of the relationship between non-adherence and health care use in pediatric populations presents an opportunity to examine a highly prevalent and modifiable (amenable to behavioral intervention) potential contributor to pediatric health care costs. Unlike other stable predictors of health care use (ie, gender, socioeconomic status), non-adherence can be modified with behavioral intervention, and thus is of clinical significance. If non-adherence contributes to pediatric health care use, there is the potential to have even greater impact on health care use than adult efforts, because long-term self-management behaviors are often developed in childhood and adolescence.23 Specifically, promoting adherence in pediatric populations may have the potential to reduce short-term health care use as well as long-term health care use that may result from the increased morbidity associated with non-adherence.23
Despite the potential significance, to our knowledge no studies have reviewed the extant literature with a targeted examination of the relationship between medication non-adherence and health care use in children and adolescents who have a chronic illness. This issue is timely as health care reform efforts and discussions regarding covered services and service delivery models (ie, fee for service versus per-member, per month) move forward. We need to better understand how modifiable factors contribute to health care costs and value to identify relevant and significant priorities of health care reform. Application of findings with adult populations would exclude many of the unique modifiable variables that impact pediatric adherence (ie, family functioning, caregiver involvement).14 The purpose of this systematic review is to provide a comprehensive summary of the empirical studies examining the relationship between non-adherence and health care use in children and adolescents who have a chronic medical condition. Recommendations for advancing research in this field and policy implications are also discussed.
Methods
The systematic review was conducted in accordance with the published guidelines presented in the Preferred Reporting Items for Systematic Reviews and Meta-Analyses Statement.29
Data Search
PubMed, PsycINFO, and CINAHL were searched in April 2013 for peer-reviewed original research articles published in English before April 2013. The search strategy included a combination of Medical Subject Headings terms (eg, chronic disease, patient compliance, medication adherence, health care costs, hospitalization, emergency service, ambulatory care) and key words (eg, adherence, non-adherence, self-management, compliance, treatment concordance, health care utilization, outpatient visit, emergency department, hospitalization, health care cost, service utilization, service use, health care use, cost, chronic illness, chronic care, chronic) (see Supplemental Information). To ensure all relevant articles were captured, an additional search was done replacing terms describing “chronic disease” with “diabetes,” “asthma,” or “HIV,” effectively searching some of the most developed adherence literature bases in pediatrics (see Supplemental Information). The search did not include restrictions on publication date or study design.
Study Selection and Screening
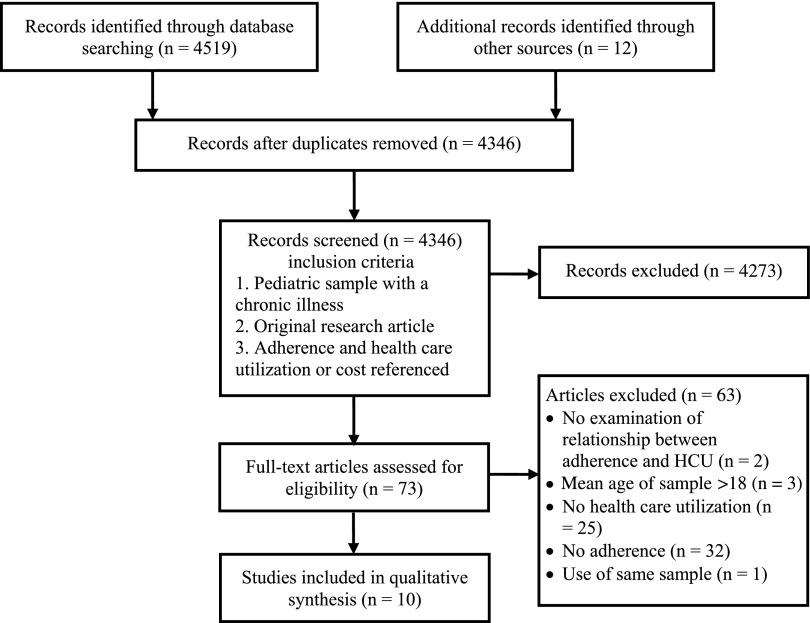
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses 4-phase flow diagram detailing study selection is depicted in Fig 1.29 The initial search resulted in 4519 records. After the removal of duplicates, we screened the abstracts of 4346 manuscripts. Of these, 73 manuscripts met the following inclusion criteria: (1) pediatric sample with a chronic illness; (2) original research article; and (3) mention of adherence and health care use or cost. We then reviewed full-text versions of these 73 manuscripts. We excluded studies that did not assess non-adherence and health care use, did not examine the relationship between these variables, or included participants with a mean age >18 years.
FIGURE 1.
Study selection flow diagram.
Data Extraction
One reviewer (Dr McGrady) completed data extraction from included articles by using a standardized data collection form. A second reviewer (Dr Hommel) checked the abstracted data for accuracy. Data retrieved from articles included: (1) identification of the manuscript (authors, year); (2) characteristics of participants (child age, child chronic illness, caregiver participating); (3) study design in accordance with published guidelines30 (cohort, cross-sectional, case-control, or randomized clinical trial); (4) measure of non-adherence; (5) measure of health care use; and (6) relationship between non-adherence and health care use. In cases in which multiple measures of non-adherence or outcomes were used, all variables were included. Questions regarding inclusion or relevant data were resolved via discussion between authors.
Definitions of Variables
Measures of Medication Non-Adherence
Medication non-adherence was assessed using measures of varying validity and reliability,31 including self-report questionnaires, self-report structured interviews, electronic monitoring devices, prescription refill histories, and biochemical assays (see Table 1). The time period during which non-adherence was assessed ranged from 24 hours to 365 days. Of note, some measures included non-adherence threshold measurements with cut-points. As these cut-points differed across studies, definitions of “good,” “high,” or “optimal” adherence presented in this manuscript are those provided by the authors of reviewed studies.
TABLE 1.
Studies Examining the Relationship Between Adherence and Health Care Use in Pediatric Populations
| Author (Year) | Study Design | Sample Size and Study Population | Measure of Adherence | Controlled For | Relationship Between Adherence and Health Care Use | |||
|---|---|---|---|---|---|---|---|---|
| ED Visits | Outpatient Visits | Hospitalizations | Other Measures of Health Care Use | |||||
| Adams et al (2001)34 | Cohort | 11 195 children (ages 3–15 yr) with asthmaa | Number of canisters or containers of drug dispenseda | Age, gender, site, reliever medication dispensing | Any dispensing of an anti-inflammatory medication was associated with a decreased risk for ED visits. Adjusted RR = 0.4 (95% CI: 0.3–0.5), P < .01 | X | Any dispensing of an anti-inflammatory medication was associated with a decreased risk for hospitalization. Adjusted RR = 0.4 (95% CI: 0.3–0.6), P < .01 | |
| Ashkenazi et al (1993)38 | Cross-sectional | 100 children (ages 2–14 y) with asthma referred to a pediatric ED; 50 children with asthma attending an HAC | Self-report measure including 2 dichotomous items assessing whether medications were taken in the dose and frequency prescribed | Compliance to prescribed dose (P < .001) and frequency (P < .001) was higher in participants in the HAC group than in the ED group | X | X | ||
| STLa | STL were higher in participants in the HAC group than in the ED group, P < .001 | X | X | |||||
| Bartlett et al (2004)40 | Cohort | 158 children with asthma | “How often does your child forget to take his/her asthma medication?” | Child age, family income, asthma morbidity, maternal depressive symptoms | NS, values not reported | X | X | |
| “In the past 2 weeks, how many days would you guess that your child has forgotten to take his or her medicine?” | Child age, family income, asthma morbidity, maternal depressive symptoms | NS, values not reported | ||||||
| Bauman et al (2002)41 | Cohort | 1199 children (ages 4–9 y) with asthmaa | Admitted non-adherence: number of times that caregivers admitted noncompliance with a physician recommendation for asthma management | X | X | Adherence was not associated with whether the child was hospitalized in the past 9 months, P = .059 | Increased adherence was associated with fewer unscheduled asthma visits (provider and ED visits), P < .001 | |
| Boylston Herndon et al (2012)36 | Cohort | 18 456 children (ages 2–18 y) with asthmaa | MPR for ICS: the percentage of days within a 365-d period that an ICS was supplied; Grouped into: 0% to 19% MPR; 20% to 49% MPR, and ≥50% MPRa | Demographics, health characteristics | ≥50% MPR was associated with lower odds of an ED visit than 0% to 19% MPR, OR = 0.56 (95% CI: 0.43–0.73), P < .001 | Greater medication adherence was associated with more frequent asthma-related office visits, P < .01 | 20% to 49% MPR was associated with increased odds of a hospital admission than 0% to 19% MPR, OR = 1.27 (95% CI: 1.04–1.55), P < .01 | Higher adherence was associated with higher per-member per-month payments |
| MPR for LI: the percentage of days within a 365-d period that an LI was supplied; Grouped into: 0% to 19% MPR; 20% to 49% MPR, and ≥50% MPRa | Demographics, health characteristics | ≥50% MPR was associated with lower odds of an ED visit than 0% to 19% MPR, OR = 0.68 (95% CI: 0.53–0.86), P = .002 | Greater medication adherence was associated with more frequent asthma-related office visits, P < .01 | NS, P = .52 | Higher adherence was associated with higher per-member per-month payments | |||
| McNally et al (2009)43 | Randomized controlled trial | 63 children (ages 5–17 y) with persistent moderate or severe asthma | Percent of prescribed oral montelukast doses received each day as recorded by an electronic monitoring device; Grouped into: low and high adherence groups based on the upper and lower quartiles of adherencea | Demographic and clinical covariates examined but not included in model owing to NS | X | X | X | Low adherence group demonstrated an increase in health care use (number of ED visits, hospitalizations, and clinic visits attributable to asthma) over the course of the study, P < .05; High adherence group demonstrated no significant change in health care use, P < .05 |
| Percent of prescribed inhaled fluticasone doses received each day as recorded by an electronic monitoring device; Grouped into: low and high adherence groups based on the upper and lower quartiles of adherencea | Demographic and clinical covariates examined but not included in model owing to NS | X | X | X | Low adherence group demonstrated an increase in health care use (number of ED visits, hospitalizations, and clinic visits attributable to asthma) over the course of the study, P < .05; High adherence group demonstrated no significant change in health care use, P < .05 | |||
| Morris et al (1997)42 | Cohort | 89 adolescents and young adults (age <30 y) with type 1 diabetesa | Number of days (out of 365) with maximum possible insulin coverage (as determined by comparing the medically recommended insulin dose with the cumulative volume of insulin prescriptions supplied); Grouped into quartilesa | X | X | Increased adherence was associated with decreased odds of admission for diabetic ketoacidosis (P < .001) Increased adherence was associated with decreased odds of hospital admissions related to complications of diabetes (P = .008) | ||
| Smith et al (2007)35 | Cohort | 1474 children (ages 2–17 y) with persistent asthmaa | Number of filled prescriptions for an inhaled corticosteroida | 1–2 filled prescriptions compared with 0 filled prescriptions decreased odds of an ED visit for asthma, Adj OR = 0.08 (95% CI: 0.05–0.15), P < .001 | X | X | ||
| Number of filled prescriptions for bronchodilatorsa | Age, gender, PCP visits, asthma PCP visits | NS in multivariate model | X | X | ||||
| Dichotomous indicator of whether a prescription for any controller medication was filled within the past 3 moa | Those with a filled prescription were less likely to have an ED visit for asthma (P < .001) than those without a filled prescription | Those with a filled prescription were more likely to have an asthma PCP visit (P < .001) than those without a filled prescription | X | |||||
| Walders et al (2004)37 | Cross-sectional | 75 children (ages 8–16 y) with persistent asthma | Total doses taken per day divided by prescribed doses per daya | Increased adherence was associated with decreased ED visits (r = −0.25, P < .05) | X | X | ||
| Zhao et al (2012)39 | Cross-sectional | 2960 children (age ≤14 y) with asthmaa | Self-reported months (out of 12) patient adhered to prescribed corticosteroid use | Increased adherence was associated with fewer ED visits, P = .00 | X | Increased adherence was associated with fewer hospitalizations, P = .00 | ||
| Self-reported months (out of 12) patient adhered to prescribed leukotriene receptor modulator use | NS, P > .05 | X | NS, P > .05 | |||||
CI, confidence interval; HAC, hospital asthma clinic; ICS, inhaled corticosteroids; LI, leukotriene inhibitors; NS, not significant; OR, odds ratio, PCP, primary care physician; STL, serum theophylline levels.
Representativeness of exposed cohort or assessment of outcome judged to be of high quality per Newcastle-Ottawa Quality Assessment Scale.
Measures of Health Care Use
To facilitate comparison across studies, we classified health care use data as ED visits, outpatient visits, hospitalizations, or “other” measures (eg, combined number of ED visits, outpatient visits, and hospitalizations) of health care use. Measures of health care use were obtained via caregiver self-report, review of the electronic medical record, or review of insurance databases.
Risk of Bias
To ascertain the reliability of the results of the included studies, the risk for bias was assessed by using the items from the Newcastle-Ottawa Quality Assessment Scale.32,33 The Newcastle-Ottawa Quality Assessment Scale is a valid and reliable measure developed to assess the quality of nonrandomized studies included in systematic reviews. High-quality studies are identified using a “star system,” with more stars representing higher quality. Two of the 8 domains of study quality (representativeness of the cohort and outcome assessment method) were relevant to the included studies. We rated each study in accordance with published guidelines on these 2 domains.
Results
Ten studies met all inclusion criteria and were included in this review (see Fig 1). Nine of the studies included children and/or adolescents who had asthma, and 1 study included a sample of adolescents and young adults who had type 1 diabetes. Mean age of study participants ranged from 6.2 to 16 years. Study designs included prospective observational cohort (n = 4), cross-sectional analyses (n = 3), retrospective observational cohort (n = 2), and randomized-controlled trials (n = 1). Three studies used managed care organizations, Medicaid, or Children’s Health Insurance Programs to access population-level data (range of sample sizes, 1474–18 456). The other studies included data from single (n = 4; range of sample sizes, 63–150) or multiple hospitals/clinics (n = 3; range of sample sizes, 158–2960). Measures of adherence varied across studies and included pharmacy refill records (n = 5), self-report measures (n = 3; eg, “In the past 2 weeks, how many days would you guess that your child has forgotten to take his or her medicine?”), and electronic monitors (n = 2).
Medication Non-Adherence and ED Visits
Six of the 7 studies examining the relationship between medication non-adherence and ED visits in children and adolescents who had asthma found that greater non-adherence using multiple measures was related to more ED visits. Children and adolescents who had asthma who did not fill any prescriptions for anti-inflammatory medications had a higher risk for an ED visit than those who filled at least 1 prescription.34,35 Furthermore, lower percentage of time during which children and adolescents possessed anti-inflammatory medications (medication possession ratio [MPR] = [number of days covered by dispensed medication/365] × 100) was related to higher odds of an ED visit.36 Consistent with these findings, a lower percentage of doses taken, as measured by electronic monitoring devices, was associated with increased ED visits.37
In a study comparing groups of children who had asthma seen in the ED to those seen in asthma clinic, self-reported non-adherence was higher in those seen in the ED.38 Similarly, caregiver report of more non-adherence was associated with more ED visits for children who had asthma.39 In contrast, a third study using a self-report measure of adherence found no relationship between non-adherence and ED visits when included in a multivariate model.40
Medication Non-Adherence and Outpatient Visits
Both of the studies examining medication non-adherence and outpatient visits found that non-adherence was associated with fewer asthma-related office visits. In a sample of children who had asthma, the fewer days a child possessed inhaled corticosteroids or leukotriene inhibitors, the less often asthma-related office visits occurred.36 Similarly, children who had not filled a prescription for a controller medication in the past 3 months were less likely than children who had filled a prescription to have an asthma primary care physician visit.35
Medication Non-Adherence and Hospitalizations
Findings of the 5 studies examining medication non-adherence and hospitalizations were mixed and varied based on method of adherence measurement. Four of these studies included children who had asthma and 1 included adolescents and young adults who had type 1 diabetes. For children who had asthma, failing to fill any prescriptions for anti-inflammatory medication was associated with an increased risk for hospitalization.34 However, when MPRs for inhaled corticosteroids were calculated and grouped, those with 20% to 49% MPR had increased odds of a hospital admission as compared with those with an MPR of 0% to 19%.36 MPRs for leukotriene inhibitors were not associated with hospitalizations.36
Caregiver self-reports of non-adherence to corticosteroids were associated with more hospitalizations in a sample of children who had asthma.39 In another sample, however, a composite score comprised of asking caregivers yes/no questions related to their adherence to filling prescriptions, giving more/less medication than prescribed, and obtaining recommended devices yielded no relation to whether the child was hospitalized in the past 9 months.41 In a sample of adolescents and young adults who had type 1 diabetes, non-adherence was associated with increased odds for admission for diabetic ketoacidosis and other diabetes-related complications.42
Medication Non-Adherence and Other Measures of Health Care Use
Similar to the aforementioned results linking non-adherence with more frequent ED visits, caregivers of children with higher levels of self-reported non-adherence also reported more frequent unscheduled asthma visits (defined as provider and ED visits).41 Results of growth curve modeling analyses suggest that medication non-adherence may be associated not only with rates of health care use, but also changes in health care use patterns.43 In a sample of African American children who had asthma, non-adherence was associated with greater increases in health care use over time than those demonstrated by groups of participants with better adherence.43
The only study to directly examine costs related to non-adherence indicated that non-adherence was associated with lower per-member, per-month public insurance payments in a sample of children who had asthma.36 As adherence to medication requires payment for prescriptions, Boylston Herndon et al found that non-adherent children had lower drug-related costs than children with higher adherence levels. In this study, the costs saved by not filling prescriptions were more than the increased costs of visiting the ED or being hospitalized incurred by these participants.
Risk for Bias
Risk for bias as identified by the items from the Newcastle-Ottawa Quality Assessment Scale and the inclusion of confounding variables is presented in Table 1. Three of the 10 studies (33%) included a cohort likely representative of the relevant pediatric population. Over three-quarters of studies (n = 8, 80%) used objective outcome measures.
Discussion
Nine of the 10 studies reviewed (90%) demonstrated a relationship between medication non-adherence and increases in at least 1 health care use variable. Of note, the directionality of the relationship between medication non-adherence and health care use depended on the outcome of interest. The majority of studies examined reported that medication non-adherence was associated with more ED visits and hospitalizations.
The relationship between medication non-adherence and ED visits and hospitalizations is consistent with findings in adult samples18,44,45 and suggests that there is potential to reduce the $1800 per child spent on hospital care in 2010.46 Children and adolescents who were non-adherent suffered from more exacerbations and complications requiring medication attention and thus required more ED visits or hospitalizations.
Although non-adherence was linked with more ED visits and hospitalizations, it was also related to fewer outpatient visits.35,36 These studies did not differentiate between recommended outpatient visits (eg, regularly scheduled planned clinic visits) and excessive outpatient visits (eg, sick visits that may have been prevented with optimal adherence), and are likely illustrating the relationship between multiple aspects of treatment adherence. Specifically, patients who are non-adherent to 1 aspect of their medical regimen (taking medication) are also more likely to be non-adherent to other parts of their medical regimen (attending regular clinic appointments). Thus, this relationship may represent non-adherence to recommended necessary treatment (both medications and clinic attendance) as opposed to less excessive health care use.
In all, the findings of this review suggest that medication non-adherence is likely an important contributor to health care use in pediatric chronic illness populations. Clinically, these results suggest that intervention efforts to improve adherence may result in reduced health care use and ultimately reduced health care costs. Currently available pediatric adherence interventions can effectively improve adherence and health outcomes.21,47 To our knowledge, no studies have examined the cost-effectiveness of adherence interventions with pediatric populations. Emerging adult literature, however, suggests that the reduced health care and indirect (eg, productivity loss, absenteeism) costs significantly outweigh the costs of implementing behavioral adherence-promoting interventions.48–51
Several limitations and resulting implications for future research exist. First, the relatively small number of studies that met inclusion criteria and the varied risk for bias across studies indicate that this is a nascent area of research that requires further investigation. To broaden the literature base in this important field, future research examining adherence should include health care use and cost analyses and be conducted with additional illness populations. Including additional illness populations is of particular importance, as it will allow for an improved understanding of how adherence relates to health care costs across a variety of illnesses with varying medical regimens and health care use patterns. Second, the observational study design of the reviewed manuscripts negates the possibilities of determining the implications of improving adherence on health care use and costs. Future research should examine this question in the context of randomized controlled trials using longitudinal data. Third, as the method of assessing adherence varied significantly between studies, it is not possible to directly compare results. Given the significant implications of this research, future efforts should use evidence-based methods of adherence assessment.31 Fourth, currently available methods can result in misleading findings, such as cost-savings associated with lower drug-related costs attributable to non-adherence. Researchers using relatively brief follow-up periods capture only the short-term drug cost savings realized from non-adherence and not the long-term, more costly consequences (eg, more frequent hospitalizations) of non-adherence. Thus, future research should address this methodologic issue by longitudinal designs that account for expected costs (eg, medication refills) versus unexpected costs (eg, ED visits) and follow participants for periods of time that allow for long-term consequences of non-adherence to be realized. Fifth, the generalizability of our findings to non-Western populations may be limited by our exclusion of non-English manuscripts. As the prevalence of non-adherence is a global concern,15 more inclusive reviews should be considered.
Resources allocated to improving adherence are often fairly limited. In the current economic and political climate, however, increasing attention has been paid to novel approaches to improving health outcomes while reducing spending. Results of this review suggest that targeting non-adherence in children and adolescents who have a chronic illness may provide a unique opportunity to reduce health care use in a continually growing population. Consistent with the call for action proposed by the World Health Organization,15 multidisciplinary efforts to promote adherence should be a priority for all medical providers and policy makers.
Supplementary Material
Glossary
- ED
emergency department
- MPR
medication possession ratio
Footnotes
Dr McGrady contributed to the manuscript by aiding in conception and design, acquisition of data, analysis and interpretation of data, drafting of manuscript, and statistical analysis; Dr Hommel contributed to the manuscript by aiding in conception and design, analysis and interpretation of data, critical revision of the manuscript for important intellectual content, and supervision; and both authors approved the final manuscript as submitted.
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: The design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation of the manuscript were supported in part by grant T32HD068223 for Dr McGrady. Dr Hommel is funded in part by R01HD067174. Funded by the National Institutes of Health (NIH).
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
References
- 1.Martin AB, Lassman D, Washington B, Catlin A, National Health Expenditure Accounts Team . Growth in US health spending remained slow in 2010; health share of gross domestic product was unchanged from 2009. Health Aff (Millwood). 2012;31(1):208–219 [DOI] [PubMed] [Google Scholar]
- 2.Schoenman J, Chockley N. Understanding U.S. Health Care Spending. Washington, DC: NIHCM Data Brief; 2011:1–13 [Google Scholar]
- 3.Haber S, McCall N, Cromwell G. Children With High Health Care Utilization and Special Health Care Needs: Draft Manuscript. Washington, DC: RTI International; 2007 [Google Scholar]
- 4.Emanuel EJ. Where are the health care cost savings? JAMA. 2012;307(1):39–40 [DOI] [PubMed] [Google Scholar]
- 5.Partnership for Solutions. Chronic Conditions: Making the Case for Ongoing Care. Baltimore, MD: The Johns Hopkins University; 2002 [Google Scholar]
- 6.Van Cleave J, Gortmaker SL, Perrin JM. Dynamics of obesity and chronic health conditions among children and youth. JAMA. 2010;303(7):623–630 [DOI] [PubMed] [Google Scholar]
- 7.Wang G, Dietz WH. Economic burden of obesity in youths aged 6 to 17 years: 1979-1999. Pediatrics. 2002;109(5). Available at: www.pediatrics.org/cgi/content/full/109/5/e81 [DOI] [PubMed] [Google Scholar]
- 8.Weiss KB, Sullivan SD, Lyttle CS. Trends in the cost of illness for asthma in the United States, 1985-1994. J Allergy Clin Immunol. 2000;106(3):493–499 [DOI] [PubMed] [Google Scholar]
- 9.Cystic Fibrosis Foundation Cystic Fibrosis Foundation Patient Registry 2010 Annual Data Report. Bethesda, MD: Cystic Fibrosis Foundation; 2010 [Google Scholar]
- 10.Smith JM, Martz K, Blydt-Hansen TD. Pediatric kidney transplant practice patterns and outcome benchmarks, 1987-2010: A report of the North American Pediatric Renal Trials and Collaborative Studies. Pediatr Transplant. 2013;17(2):149–157 [DOI] [PubMed] [Google Scholar]
- 11.Berry JG, Hall M, Hall DE, et al. Inpatient growth and resource use in 28 children’s hospitals: a longitudinal, multi-institutional study. JAMA Pediatr. 2013;167(2):170–177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chevarley FM. Utilization and Expenditures for Children With Special Health Care Needs. Rockville, MD: Agency for Healthcare Research and Quality; 2006 [Google Scholar]
- 13.Newacheck PW, Kim SE. A national profile of health care utilization and expenditures for children with special health care needs. Arch Pediatr Adolesc Med. 2005;159(1):10–17 [DOI] [PubMed] [Google Scholar]
- 14.Modi AC, Pai AL, Hommel KA, et al. Pediatric self-management: A framework for research, practice, and policy. Pediatrics. 2012;129(2). Available at: www.pediatrics.org/cgi/content/full/129/2/e473 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sabate E. Adherence to Long-term Therapies: Evidence for Action. Geneva, Switzerland: World Health Organization; 2003 [Google Scholar]
- 16.Bender BG, Rand C. Medication non-adherence and asthma treatment cost. Curr Opin Allergy Clin Immunol. 2004;4(3):191–195 [DOI] [PubMed] [Google Scholar]
- 17.Muenchberger H, Kendall E. Predictors of preventable hospitalization in chronic disease: priorities for change. J Public Health Policy. 2010;31(2):150–163 [DOI] [PubMed] [Google Scholar]
- 18.Roebuck MC, Liberman JN, Gemmill-Toyama M, Brennan TA. Medication adherence leads to lower health care use and costs despite increased drug spending. Health Aff (Millwood). 2011;30(1):91–99 [DOI] [PubMed] [Google Scholar]
- 19.Berg JS, Dischler J, Wagner DJ, Raia JJ, Palmer-Shevlin N. Medication compliance: a healthcare problem. Ann Pharmacother. 1993;27(9 suppl):S1–S24 [PubMed] [Google Scholar]
- 20.DiMatteo MR. Variations in patients’ adherence to medical recommendations: a quantitative review of 50 years of research. Med Care. 2004;42(3):200–209 [DOI] [PubMed] [Google Scholar]
- 21.Kahana S, Drotar D, Frazier T. Meta-analysis of psychological interventions to promote adherence to treatment in pediatric chronic health conditions. J Pediatr Psychol. 2008;33(6):590–611 [DOI] [PubMed] [Google Scholar]
- 22.Newacheck PW, Taylor WR. Childhood chronic illness: prevalence, severity, and impact. Am J Public Health. 1992;82(3):364–371 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rapoff MA. Adherence to Pediatric Medical Regimens. New York, NY: Springer; 2010 [Google Scholar]
- 24.Logan D, Zelikovsky N, Labay L, Spergel J. The Illness Management Survey: identifying adolescents’ perceptions of barriers to adherence. J Pediatr Psychol. 2003;28(6):383–392 [DOI] [PubMed] [Google Scholar]
- 25.Hommel KA, Davis CM, Baldassano RN. Objective versus subjective assessment of oral medication adherence in pediatric inflammatory bowel disease. Inflamm Bowel Dis. 2009;15(4):589–593 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.de Brantes F, Rosenthal MB, Painter M. Building a bridge from fragmentation to accountability—the Prometheus Payment model. N Engl J Med. 2009;361(11):1033–1036 [DOI] [PubMed] [Google Scholar]
- 27.Federal Interagency Forum on Child and Family Statistics America’s Children in Brief: Key National Indicators of Well-Being, 2012. Washington, DC: U.S. Government Printing Office; 2012 [Google Scholar]
- 28.Stille C, Turchi RM, Antonelli R, et al. Academic Pediatric Association Task Force on Family-Centered Medical Home . The family-centered medical home: specific considerations for child health research and policy. Acad Pediatr. 2010;10(4):211–217 [DOI] [PubMed] [Google Scholar]
- 29.Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group . Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Vandenbroucke JP, von Elm E, Altman DG, et al. STROBE Initiative . Strengthening the reporting of observational studies in epidemiology (STROBE): explanation and elaboration. PLoS Med. 2007;4(10):e297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Quittner AL, Modi AC, Lemanek KL, Ievers-Landis CE, Rapoff MA. Evidence-based assessment of adherence to medical treatments in pediatric psychology. J Pediatr Psychol. 2008;33(9):916–936, discussion 937–938 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wells G, Shea B, O’connell D, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Paper presented at 3rd Symposium on Systematic Reviews: Beyond the Basics; 2000 [Google Scholar]
- 33.Higgins JPT, Altman DG. Assessing Risk of Bias in Included Studies. Cochrane Handbook for Systematic Reviews of Interventions. West Sussex, England: John Wiley & Sons, Ltd; 2008:187–241 [Google Scholar]
- 34.Adams RJ, Fuhlbrigge A, Finkelstein JA, et al. Impact of inhaled antiinflammatory therapy on hospitalization and emergency department visits for children with asthma. Pediatrics. 2001;107(4):706–711 [DOI] [PubMed] [Google Scholar]
- 35.Smith SR, Wakefield DB, Cloutier MM. Relationship between pediatric primary provider visits and acute asthma ED visits. Pediatr Pulmonol. 2007;42(11):1041–1047 [DOI] [PubMed] [Google Scholar]
- 36.Herndon JB, Mattke S, Evans Cuellar A, Hong SY, Shenkman EA. Anti-inflammatory medication adherence, healthcare utilization and expenditures among Medicaid and children’s health insurance program enrollees with asthma. Pharmacoeconomics. 2012;30(5):397–412 [DOI] [PubMed] [Google Scholar]
- 37.Walders N, Kopel SJ, Koinis-Mitchell D, McQuaid EL. Patterns of quick-relief and long-term controller medication use in pediatric asthma. J Pediatr. 2005;146(2):177–182 [DOI] [PubMed] [Google Scholar]
- 38.Ashkenazi S, Amir J, Volovitz B, Varsano I. Why do asthmatic children need referral to an emergency room? Pediatr Allergy Immunol. 1993;4(2):93–96 [DOI] [PubMed] [Google Scholar]
- 39.Zhao J, He Q, Zhang G, et al. Status of asthma control in children and the effect of parents’ knowledge, attitude, and practice (KAP) in China: a multicenter study. Ann Allergy Asthma Immunol. 2012;109(3):190–194 [DOI] [PubMed] [Google Scholar]
- 40.Bartlett SJ, Krishnan JA, Riekert KA, Butz AM, Malveaux FJ, Rand CS. Maternal depressive symptoms and adherence to therapy in inner-city children with asthma. Pediatrics. 2004;113(2):229–237 [DOI] [PubMed] [Google Scholar]
- 41.Bauman LJ, Wright E, Leickly FE, et al. Relationship of adherence to pediatric asthma morbidity among inner-city children. Pediatrics. 2002;110(1 pt 1). Available at: www.pediatrics.org/cgi/content/full/110/1/e6 [DOI] [PubMed] [Google Scholar]
- 42.Morris AD, Boyle DI, McMahon AD, Greene SA, MacDonald TM, Newton RW. Adherence to insulin treatment, glycaemic control, and ketoacidosis in insulin-dependent diabetes mellitus. The DARTS/MEMO Collaboration. Diabetes Audit and Research in Tayside Scotland. Medicines Monitoring Unit. Lancet. 1997;350(9090):1505–1510 [DOI] [PubMed] [Google Scholar]
- 43.McNally KA, Rohan J, Schluchter M, et al. Adherence to combined montelukast and fluticasone treatment in economically disadvantaged African American youth with asthma. J Asthma. 2009;46(9):921–927 [DOI] [PubMed] [Google Scholar]
- 44.Encinosa WE, Bernard D, Dor A. Does prescription drug adherence reduce hospitalizations and costs? The case of diabetes. Adv Health Econ Health Serv Res. 2010;22:151–173 [DOI] [PubMed] [Google Scholar]
- 45.Valenti WM. Treatment adherence improves outcomes and manages costs. AIDS Read. 2001;11(2):77–80 [PubMed] [Google Scholar]
- 46.Agency for Healthcare Research and Quality. Total health services—mean and median expenses per person with expense and distribution of expenses by source of payment: United States, 2010. Medical Expenditure Panel Survey Household Component Data. Available at: http://meps.ahrq.gov/mepsweb/. Accessed July 8, 2013
- 47.Graves MM, Roberts MC, Rapoff M, Boyer A. The efficacy of adherence interventions for chronically ill children: a meta-analytic review. J Pediatr Psychol. 2010;35(4):368–382 [DOI] [PubMed] [Google Scholar]
- 48.Chapman RH, Ferrufino CP, Kowal SL, Classi P, Roberts CS. The cost and effectiveness of adherence-improving interventions for antihypertensive and lipid-lowering drugs. Int J Clin Pract. 2010;64(2):169–181 [DOI] [PubMed] [Google Scholar]
- 49.Chapman RH, Kowal SL, Cherry SB, Ferrufino CP, Roberts CS, Chen L. The modeled lifetime cost-effectiveness of published adherence-improving interventions for antihypertensive and lipid-lowering medications. Value Health. 2010;13(6):685–694 [DOI] [PubMed] [Google Scholar]
- 50.Desborough JA, Sach T, Bhattacharya D, Holland RC, Wright DJ. A cost-consequences analysis of an adherence focused pharmacist-led medication review service. Int J Pharm Pract. 2012;20(1):41–49 [DOI] [PubMed] [Google Scholar]
- 51.Patrick AR, Schousboe JT, Losina E, Solomon DH. The economics of improving medication adherence in osteoporosis: validation and application of a simulation model. J Clin Endocrinol Metab. 2011;96(9):2762–2770 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.