Abstract
Background and Purpose
Early risk of recurrence and mortality after stroke differ by subtype, but less is known about long-term recurrence and hospital readmissions. These differences have economic implications and will affect long-term disability and stroke survivor quality of life. We examined recurrent stroke, all-cause hospital readmission, and mortality by index etiologic subtype.
Methods
We identified 987 Atherosclerosis Risk in Communities Study cohort participants with first-ever stroke and followed them for a median 5.3 years after first stroke. Outcomes were compared across index subtypes (infarction: thrombotic, cardioembolic [CE], and lacunar; hemorrhagic: subarachnoid [SAH] and intracerebral [ICH]) using Kaplan-Meier analysis and Cox proportional hazards regression adjusting for age, sex, and race.
Results
There were 183 recurrent strokes among 147 participants, 3234 hospitalizations among 746 participants, and 529 deaths; only 14% of participants were event free over follow-up. The majority of recurrent events were of the same subtype, except for lacunar infarcts which were followed nearly three-quarters of the time by non-lacunar events. Adjusted mortality was higher for ICH (HR=2.3, 95% CI: 1.7–3.0) compared with thrombotic stroke and lower for lacunar infarcts. Lacunar infarcts had somewhat higher recurrence compared with thrombotic infarcts (1.3, 0.9–1.9), but lower all-cause readmission (0.8, 0.7–1.0). Readmission was 40% higher for CE relative to thrombotic stroke (1.4, 1.1–1.7).
Conclusions
While the highest mortality was observed for ICH, there was significant burden of recurrent stroke and hospital readmissions for lacunar and cardioembolic strokes, respectively. There may be opportunities to reduce the relatively high rate of post-stroke readmissions.
Keywords: stroke subtype, readmission, outcomes
Introduction
Stroke represents an important public health concern in the U.S. It is the 4th leading cause of mortality, the leading cause of severe disability, and a top contributor to healthcare expenditures for the elderly.1, 2 Recurrent events and hospital readmissions, which may be preventable, contribute to morbidity and costs.
While early risk of mortality and recurrence differ by index subtype, less is known about long-term recurrence and hospital readmission.3–5 These differences impact quality of life and may have economic implications. The study aim was to characterize mortality, recurrence, and hospital readmissions after stroke according to etiologic subtype in order to better understand differential post-stroke health outcomes in a population-based sample of U.S. adults.
Methods
The study included all first-ever definite/probable strokes among ARIC study cohort participants; methods reported elsewhere.6 Briefly, 15,792 residents of 4 communities aged 45–64 were recruited from 1987–1989. Information on clinical events and hospitalizations was collected at baseline, 3 subsequent clinic visits at 3-year intervals, during annual telephone calls, and upon review of local hospital discharge lists. All stroke diagnoses (first-ever and recurrent) were based on computer-derived diagnosis and physician medical record review, with differences adjudicated by a second physician reviewer. Classification required evidence of sudden or rapid onset of neurological symptoms lasting >24 hours or leading to death, in the absence of evidence for a nonstroke cause. Strokes were further classified according to etiologic subtype as thrombotic brain infarction, lacunar infarction, cardioembolic stroke (CE), intracerebral hemorrhage (ICH), or subarachnoid hemorrhage (SAH) according to criteria adopted from the National Survey of Stroke (S1: subtype classification).6
We identified 987 first-ever stroke events during a median 19-year follow-up (S2: participant flow diagram). These cases were followed from the index event for recurrent stroke, all-cause hospital readmission, and mortality until the earliest of death, date of last contact if lost-to-follow up, or end of follow-up on 12/31/2008. Outcomes were compared across subtypes using Kaplan-Meier analysis and Cox proportional-hazards regression that estimated hazard ratios (HR) and 95% confidence intervals (CI) adjusting for age, sex, race, and in secondary analysis, Charlson comorbidity index. Recurrence after hemorrhagic subtypes is not reported due to small numbers of events.
Results
The distribution of index stroke subtypes was: 48.7% thrombotic, 20.0% CE, 18.5% lacunar, 8.6% ICH, and 4.2% SAH (S3: participant characteristics). Hemorrhagic stroke patients were slightly younger and more often women than individuals with ischemic strokes. During a median 5.3 years of follow-up after the index event, there were 183 recurrent strokes among 147 participants, 3234 hospital readmissions among 746 participants, and 529 deaths. Only 139 participants (14.1%) were event-free during follow up.
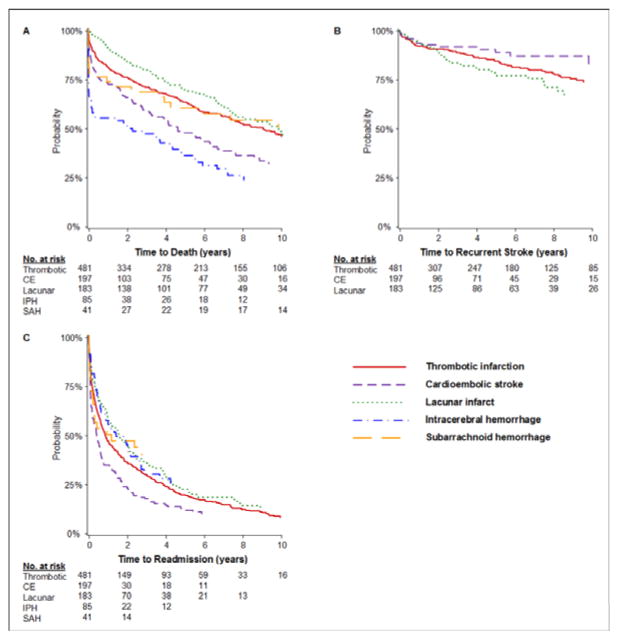
Roughly 70% of recurrent strokes were of the same subtype; however, only 28% were the same when the index stroke was lacunar (S4: recurrent stroke distribution). Post-stroke survival was lowest for ICH (45.4% at 1 year) and highest for lacunar infarcts (9.6%; Figure 1, Table 1). Cardioembolic strokes had the highest all-cause readmission, 65.5% at 1 year, while lacunar infarcts had the lowest at 41.2%. CVD-related readmissions showed the same patterns across ischemic subtypes (23.4% for CE and 5.9% for lacunar). After adjustment for age, sex, and race, mortality was higher for CE (HR=1.3, 95% CI: 1.0–1.6) and ICH (2.3, 1.7–3.0) compared with thrombotic strokes and lower for lacunar (0.8, 0.6–1.0; Figure 2). All-cause readmission was 40% higher for CE compared with thrombotic strokes (1.4, 1.1–1.7). Additional adjustment for comorbidity did not appreciably change the results for recurrence or readmission. All-cause mortality estimates were attenuated for CE (1.14, 0.91–1.44) and increased for SAH (1.22, 0.78–1.92).
Figure 1.
Kaplan-Meier analysis of mortality, recurrence, and readmission by subtype. Survival curves are for all-cause mortality (A), first recurrent stroke event (B), and first hospital readmission for any cause (C) in the 10 years after index stroke event. Numbers of patients at risk at 2-year intervals are shown below the curves. Log-rank p-values for differences in survival by stroke subtype were 0.05 for mortality, 0.05 for recurrent stroke, and <0.0001 for hospital readmission. Recurrent stroke outcomes are not shown for hemorrhagic stroke subtypes due to small numbers of events.
Table 1.
Incidence (95% CI) of mortality, recurrence, and hospital readmission by index subtype
| Characteristic | Etiologic Stroke Subtype | ||||
|---|---|---|---|---|---|
| Thrombotic (N=481) | Cardioembolic (N=197) | Lacunar (N=183) | Intracerebral Hemorrhage (N=85) | Subarachnoid Hemorrhage (N=41) | |
| Mortality | |||||
| 30-day | 7.5 (5.5–10.3) | 12.8 (8.8–18.3) | 1.1 (0.3–4.4) | 36.5 (27.3–47.7) | 24.4 (13.9–40.6) |
| 1-year | 19.6 (16.3–23.4) | 27.6 (21.9–34.6) | 9.6 (6.1–15.0) | 45.4 (35.4–56.6) | 26.9 (15.9–43.3) |
| Recurrent stroke | |||||
| 30-day | 1.6 (0.7–3.2) | 2.3 (0.9–6.0) | 1.1 (0.3–4.4) | - | - |
| 1-year | 7.9 (5.7–11.0) | 6.5 (3.6–11.9) | 6.5 (3.6–11.4) | - | - |
| Hospital readmission | |||||
| All-cause readmission | |||||
| 30-day | 14.4 (11.5–18.0) | 22.0 (16.5–29.1) | 12.9 (8.8–18.8) | 9.3 (4.0–21.0) | 18.8 (8.9–37.1) |
| 1-year | 53.2 (48.6–57.9) | 65.6 (58.2–72.8) | 41.2 (34.3–48.8) | 42.8 (30.6–57.4) | 50.0 (34.3–68.1) |
| CVD-related readmission* | |||||
| 30-day | 1.8 (0.9–3.6) | 6.6 (3.7–11.6) | 0.6 (0.1–3.9) | 0 | 0 |
| 1-year | 13.3 (10.4–17.0) | 23.4 (17.5–31.0) | 5.9 (3.2–23.2) | 9.4 (3.6–23.2) | 6.8 (1.7–24.6) |
Primary ICD-9 discharge diagnosis codes 390-429, 440-459, 745-747
Figure 2.
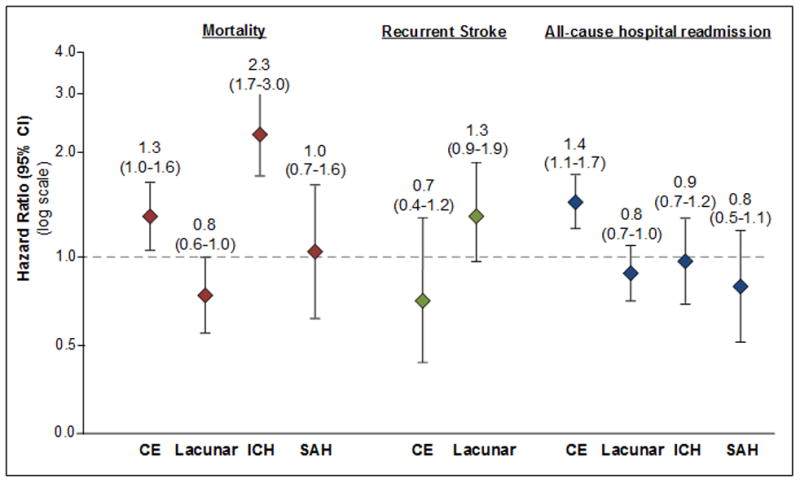
Hazard ratios for mortality, recurrence, and readmission by subtype. Values above each bar indicate hazard ratios (95% confidence intervals) for outcomes by etiologic subtype with thrombotic stroke serving as the referent group for all comparisons. Recurrent stroke results are not shown for hemorrhagic subtypes due to small numbers of events.
Conclusion
Post-stroke mortality was highest for ICH; however, there was significant morbidity for other stroke types, particularly all-cause hospital readmission after cardioembolic stroke. While some studies found no difference between hemorrhagic and ischemic strokes with regard to readmission,7 others reported higher 4-year readmission for ischemic stroke.8 One-year rehospitalization rates in a Canadian study were highest for ischemic strokes (37.9%).9 We extend these results by examining readmission for ischemic subtypes, reporting higher readmission for CE and lower readmission for lacunar infarcts compared with thrombotic events. A hospital-based registry noted that infection was a common reason for rehospitalization, comprising 28% of all events in the year following stroke. This suggests there may be opportunities to reduce potentially preventable post-stroke readmissions such as pneumonia and UTI.7
Mortality in our study was lower than reported elsewhere, possibly reflecting differences in case mix and temporal changes in case fatality.9, 10 As expected, hemorrhagic subtypes had the highest mortality. Consistent with our results, previous studies report that recurrence rates were highest for large-artery thrombosis and CE while being no different or somewhat lower for lacunar infarcts.3–5, 11–14
Strengths of our study were the population-based design, near-complete event ascertainment, validation of events, and long-term follow-up. The majority of studies examining readmissions by subtype used hospital-based cohorts or administrative databases, which often do not validate events and may not be representative of all strokes in a given region. Limitations include the small number of hemorrhagic events, which limited our ability to assess recurrence, and the inability to identify those readmissions that were potentially preventable.
The disease burden experienced by stroke survivors is of increasing concern given the ageing of the population, improvements in case fatality, and growing healthcare costs. The high rate of hospital readmissions highlights the need for prevention not only of recurrent events, but also of all-cause readmissions. Readmissions may result from gaps in secondary prevention and medical care and therefore might be prevented with improved coordination of care and discharge planning. Prevention and management strategies targeted according to stroke subtypes may be warranted.
Supplementary Material
Acknowledgments
The authors thank the ARIC Study staff and participants for their important contributions.
Funding Sources
The ARIC Study is supported by National Heart, Lung, and Blood Institute contracts and SBJ by a National Heart, Lung, and Blood Institute training grant (T32HL7055).
Footnotes
Disclosure Statement
The authors report no disclosures.
References
- 1.Andrews R, Elixhauser A. Healthcare Cost and Utilization Project–Statistical Brief #42. 2007. The National Hospital Bill: Growth trends and 2005 update on the most expensive conditions by payer. [PubMed] [Google Scholar]
- 2.Writing Group M. Roger VL, Go AS, Lloyd-Jones DM, Benjamin EJ, Berry JD, et al. Heart Disease and Stroke Statistics--2012 Update: A Report From the American Heart Association. Circulation. 2012;125:e2–e220. doi: 10.1161/CIR.0b013e31823ac046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Grau AJ, Weimar C, Buggle F, Heinrich A, Goertler M, Neumaier S, et al. Risk factors, outcome, and treatment in subtypes of ischemic stroke: the German stroke data bank. Stroke. 2001;32:2559–2566. doi: 10.1161/hs1101.098524. [DOI] [PubMed] [Google Scholar]
- 4.Lovett JK, Coull AJ, Rothwell PM. Early risk of recurrence by subtype of ischemic stroke in population-based incidence studies. Neurology. 2004;62:569–573. doi: 10.1212/01.wnl.0000110311.09970.83. [DOI] [PubMed] [Google Scholar]
- 5.Petty GW, Brown RD, Jr, Whisnant JP, Sicks JD, O’Fallon WM, Wiebers DO. Ischemic stroke subtypes: a population-based study of functional outcome, survival, and recurrence. Stroke. 2000;31:1062–1068. doi: 10.1161/01.str.31.5.1062. [DOI] [PubMed] [Google Scholar]
- 6.Rosamond WD, Folsom AR, Chambless LE, Wang CH, McGovern PG, Howard G, et al. Stroke incidence and survival among middle-aged adults: 9-year follow-up of the Atherosclerosis Risk in Communities (ARIC) cohort. Stroke. 1999;30:736–743. doi: 10.1161/01.str.30.4.736. [DOI] [PubMed] [Google Scholar]
- 7.Lin HJ, Chang WL, Tseng MC. Readmission after stroke in a hospital-based registry: risk, etiologies, and risk factors. Neurology. 2011;76:438–443. doi: 10.1212/WNL.0b013e31820a0cd8. [DOI] [PubMed] [Google Scholar]
- 8.Lee WC, Joshi AV, Wang Q, Pashos CL, Christensen MC. Morbidity and mortality among elderly Americans with different stroke subtypes. Advances in Therapy. 2007;24:258–268. doi: 10.1007/BF02849893. [DOI] [PubMed] [Google Scholar]
- 9.Feigin VL, Lawes CM, Bennett DA, Anderson CS. Stroke epidemiology: a review of population-based studies of incidence, prevalence, and case-fatality in the late 20th century. Lancet Neurol. 2003;2:43–53. doi: 10.1016/s1474-4422(03)00266-7. [DOI] [PubMed] [Google Scholar]
- 10.Thrift AG, Dewey HM, Macdonell RA, McNeil JJ, Donnan GA. Incidence of the major stroke subtypes: initial findings from the North East Melbourne stroke incidence study (NEMESIS) Stroke. 2001;32:1732–1738. doi: 10.1161/01.str.32.8.1732. [DOI] [PubMed] [Google Scholar]
- 11.Jackson CA, Hutchison A, Dennis MS, Wardlaw JM, Lewis SC, Sudlow CL. Differences between ischemic stroke subtypes in vascular outcomes support a distinct lacunar ischemic stroke arteriopathy: a prospective, hospital-based study. Stroke. 2009;40:3679–3684. doi: 10.1161/STROKEAHA.109.558221. [DOI] [PubMed] [Google Scholar]
- 12.Sacco RL, Foulkes MA, Mohr JP, Wolf PA, Hier DB, Price TR. Determinants of early recurrence of cerebral infarction. The Stroke Data Bank. Stroke. 1989;20:983–989. doi: 10.1161/01.str.20.8.983. [DOI] [PubMed] [Google Scholar]
- 13.Yokota C, Minematsu K, Hasegawa Y, Yamaguchi T. Long-term prognosis, by stroke subtypes, after a first-ever stroke: a hospital-based study over a 20-year period. Cerebrovasc Dis. 2004;18:111–116. doi: 10.1159/000079258. [DOI] [PubMed] [Google Scholar]
- 14.Rundek R, Sacco R. Prognosis after stroke. In: Mohr JP, Wolf PA, Grotta JC, Moskowitz MA, Mayberg MR, von Kummer R, editors. Stroke pathophysiology, diagnosis, and management. 5. Philadelphia, PA: Elsevier/Saunders; 2011. pp. 219–241. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.