Abstract
Purpose
The purpose of this study was to compare the efficacy of two imaging modes in a cone beam computed tomography (CBCT) system in detecting root fracture in endodontically-treated teeth with fiber posts or screw posts by selecting two fields of view.
Materials and Methods
In this study, 78 endodontically-treated single canal premolars were included. A post space was created in all of them. Then the teeth were randomly set in one of 6 artificial dental arches. In 39 of the 78 teeth set in the 6 dental arches, a root fracture was intentionally created. Next, a fiber post and a screw post were cemented into 26 teeth having equal the root fractures. High resolution (HiRes) and standard zoom images were provided by a CBCT device. Upon considering the reconstructed images, two observers in agreement with each other confirmed the presence or absence of root fracture. A McNemar test was used for comparing the results of the two modes.
Results
The frequency of making a correct diagnosis using the HiRes zoom imaging mode was 71.8% and in standard zoom was 59%. The overall sensitivity and specificity in diagnosing root fracture in the HiRes mode were 71.79% and 46.15% and in the standard zoom modes were 58.97% and 33.33%, respectively.
Conclusion
There were no significant differences between the diagnostic values of the two imaging modes used in the diagnosis of root fracture or in the presence of root canal restorations. In both modes, the most true-positive results were reported in the post space group.
Keywords: Tooth Fractures, Cone-Beam Computed Tomography, Diagnosis
Introduction
Vertical root fracture (VRF) is defined as a partial or complete longitudinal lucent line on a radiograph that extends through the long axis of the tooth.1 VRFs primarily extend from the inner portion toward the outer side in a buccolingual or a buccopalatal direction and from the cervical to the apical third. In this phase, local inflammation usually stimulates bone resorption and finally induces bone loss. Therefore, in the majority of cases, the radiographic findings resemble periodontal disease.1,2 Combining the usage of radiographic signs and clinical symptoms can be most efficient in the process of root fracture diagnosis.3,4
Root fracture as a longitudinal pattern is common in posterior teeth, particularly in maxillary premolar teeth.5 Endodontic treatment is one of the most common causes of root fracture. VRFs in 3.69% of root-canal treated (RCT) teeth have been reported,6 however, 35.7% of VRFs could detected on dental radiographs.7
The applied force during root canal treatment, the anatomy of the root canal, the degree of canal preparation, or the fitting of the plugger or spreader utilized with the form of the canal might influence the incidence of root fracture. Excessive force during canal obturation is the cause of VRFs in 48-84% of RCT teeth.8
Several studies5,9-13 have confirmed the value and efficacy of cone beam computed tomography (CBCT) in the detection and diagnosis of root fracture. Hassan et al14 found that the variables of the detector character, field of view (FOV), and voxel size affected the ability of different imaging systems in terms of accuracy and sensitivity of diagnosing root fracture in a comparative study of five different CBCT systems. In addition, they determined that root canal filling did not influence the overall accuracy of the systems under investigation.
In the reconstruction of the crown of an RCT tooth, screw posts and, more recently, fiber posts have been used widely, which could present a challenge in making an accurate diagnosis of root fracture.
In some CBCT devices, several imaging modes are available, such as the high resolution (HiRes) and standard zoom modes of the NewTom VG system. These imaging modes have various differences, such as their FOV and voxel sizes as well as the patient exposure dose. Overall, a larger FOV provides lower contrast and spatial resolution than a smaller FOV, which can affect the visibility of details of anatomical structures.15,16
In this study, we selected the high resolution (HiRes) (6-inch FOV, 0.125-0.150 mm voxel size) and standard imaging modes (4-inch FOV, 0.200-0.240 mm voxel size), which have distinct technical specifications, and also identified the several root canal restorations for the reconstruction of the affected tooth. The aims of this study were to compare the diagnostic values of these two different imaging modes in the diagnosis of root fracture and also to determine the influence of employing screw or fiber posts as intracanal restorations on them. We also aimed to identify the preferred mode for the detection of root fracture while limiting the patient-exposure dose while maintaining the same ability to detect root fracture.
Materials and Methods
In this in vitro study, the diagnostic value of the two different modes including HiRes and standard zoom in the evaluation of longitudinal root fracture was assessed. The gold standard was the direct observation of a root fracture line on the root surface. The fracture line was defined as a fracture line having a vertical or an oblique direction along the root surface but with no visible displacement of the fracture fragments. In this study, 78 premolar teeth with a single root canal were selected and periapical parallel radiographs were taken. An experienced endodontist having more than ten years of professional experience confirmed the single straight root canals.
The teeth with less than a 15-cm root length and deformed roots were excluded. Any calculus and/or attached alveolar bone were removed from all of the tooth surfaces. The crowns of the teeth located at the cementoenamel junction (CEJ) were cut by a diamond disc. After filling the root canal with gutta-percha (Diadent, Burnaby, BC, Canada) and an AH26 sealer (Dentsply DeTrey, Konstanz, Germany), the root surfaces of the selected teeth were colorized by methylene blue to rule out root fracture. They were categorized in three experimental and three control groups. During the study, the samples were kept in a wet environment. The post spaces were prepared at the half- or the two-thirds root length by using a Gates-Glidden No. 2 or No. 3 drill (Maillefer, Ballaigues, Switzerland) and a heat carrier.
The root surface was covered by a layer of wax having a 0.5-mm thickness for the ultimate reconstruction of the periodontal ligament space. The tooth samples were arranged in 6 simulated or artificial jaw arches. These arches were made from a mixture of sawdust, bovine bone powder, and acryl.
For simulation of a root fracture in a clinical situation, a root fracture was induced by a No. 5 finger plugger (Maillefer, Ballaigues, Switzerland) and/or a Model D finger spreader (Maillefer, Ballaigues, Switzerland) having 0.04 mm/mm tapering by applying a wedging force or by rotating the screw post in the post space. The aforementioned endodontist with more than 10 years of experience in root fracture diagnosis was involved in the process of root fracture induction. Overall, all of the induced fracture lines originated from the intracanal portion and extended to the periphery of the root.
This endodontist simulated root fracture in 39 teeth that had been randomly selected from 6 arches. Then, these teeth were removed from their sockets to confirm the presence of root fracture. The root surface was observed directly using a magnifier. If the fractured compartments were accompanied by a gross separation of the root structure, the fragments were adjoined to each other by using finger pressure and affixed using glue on the outer surfaces of the roots. Then, parallel radiographs using a phosphor storage plate (PSP) sensor (Digora Optime, Sordex, Helsinki, Finland) and exposure parameters of 70 kVp, 7 mA, and 0.12 seconds were taken of the different teeth to confirm that the simulated fracture lines were not easily detectable. In the 13 teeth with root fracture, screw posts (Dentatus, Spånga, Sweden) and, in another 13, fiber posts (RTD, St. Egreve, France) were cemented with self-adhesive resin cement (Breeze®, Orange County, CA, USA) without applying excessive pressure. The selection of the teeth to put in the experimental or control groups and also in the fiber posts, screw posts, or post spaces in each experimental and control group were random.
Overall in this study, we had 78 premolar teeth in 6 different groups, one set in each of 6 simulated arches. However, we attempted to have at least 4 of the 13 teeth set in each arch match the group descriptions detailed below:
Group A: Teeth with a fiber post and a positive fracture line
Group B: Teeth with a fiber post and a negative fracture line
Group C: Teeth with a screw post and a positive fracture line
Group D: Teeth with a screw post and a negative fracture line
Group E: Teeth with a post space and a positive fracture line
Group F: Teeth with a post space and a negative fracture line
To reconstruct a soft tissue shadow and to avoid differences in the density observed or the detection of an image artifact, a model with a U-shaped water-containing lacuna fixed on a plexy plate was designed. In the center of the model, the artificial mandible was set onto the center of the plate. This complex was then set onto the desk of a NewTom VG CBCT device (QR Srl Company, Verona, Italy). Depending on the voxel resolution and FOV, volumetric images were acquired using both HiRes (6-inch FOV, 0.125-0.150 mm voxel size) and standard (4-inch FOV, 0.200-0.240 mm voxel size) zoom modes.
Exposure parameters for the HiRes zoom mode were 110 kV, 3.07 mA, and 5.4 seconds. At first, two scout images, that is, lateral and posterior-anterior views, taken in accordance with the sample position, were initially prepared and, after this, a 360° scan was performed. The time required for the reconstruction of volumetric images after the patient's complete exposure was 4 minutes. The above-mentioned steps were repeated using a standard zoom with an exposure parameter of 110 kV, 2.05 mA and 3.6 seconds.
Then, to reconstruct the study images taken from the volumetric ones, the plane was selected in such a way as to ensure that it was parallel to the occlusal plane. Axial images with a thickness and an interval of 0.4mm(Fig. 1) and cross-sectional images with a thickness of 0.5 mm and an interval of 0.5 mm perpendicular to the mesiodistal and/or bucco-lingual axes of each root (Fig. 2) were prepared by a maxillofacial radiologist and an endodontist. They were familiar with CBCT and had more than 15 years of professional work experience; they served as observers. These individuals then determined the absence or presence of root fracture and their locations concomitantly and in agreement with each other (i.e., on the root surface and/or in which). The process of observation was repeated on 50 out of the 78 samples after one week for both imaging modes. SPSS 16.0 (SPSS Inc., Chicago, IL, USA) was used for data gathering and analysis. The sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), and likelihood ratio (LR) measurements were then calculated. Significance was established at the P<0.05 level. A McNemar test was used for comparing the correct diagnosis provided by the two different imaging modes and also for determining whether the presence or absence of fiber posts or screw posts affected the ability of the dental practitioner to make an accurate diagnosis.
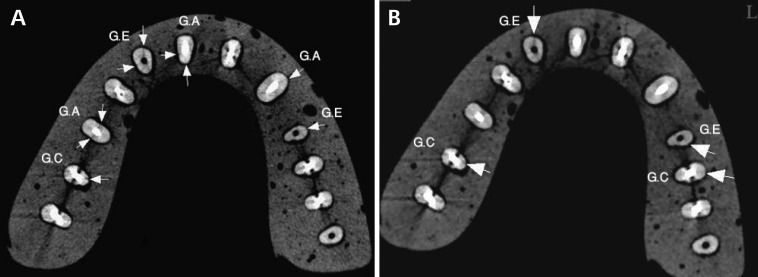
Fig. 1.
The axial images of high resolution (A) and standard (B) zoom modes of CBCT images show several root fractures (arrows). The teeth with a fiber post and root fracture (Group A; G.A), with a screw post and root fracture (Group C; G.C), and with a post space and root fracture (Group E; G.E) are seen in each arch set.
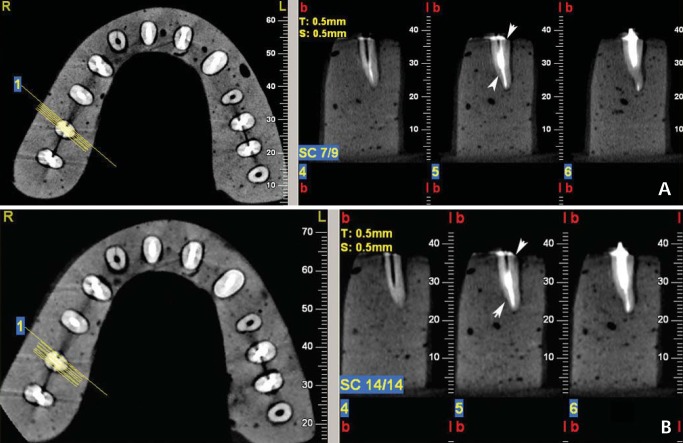
Fig. 2.
The axial and cross-sectional images of high resolution (A) and standard (B) zoom modes show the direction of root fracture in a tooth with a screw post and root fracture (arrows).
Results
In this experimental study, the respective proportions of correct diagnoses of root fracture were 71.8% overall and, in the post space, screw post, and fiber post groups, were 84.6%, 61.5%, and 69.2%, respectively in the HiRes mode. The general frequency of making a correct diagnosis was reported to be 59%, and in the above-mentioned groups was specifically 69.2%, 61.5%, and 46.2% for the standard zoom. However, in the post-space group, we found the highest incidence of a true-positive finding (Table 1). The reproducibility after a one-week time interval was 91% for the HiRes zoom and 85% for the standard zoom mode. The frequencies of making a correct identification of the presence or absence of root fracture in both HiRes and standard zoom imaging modes appear in Table 2.
Table 1.
The frequency of correct diagnosis of the presence of root fracture in high resolution (HiRes) and standard zoom imaging modes
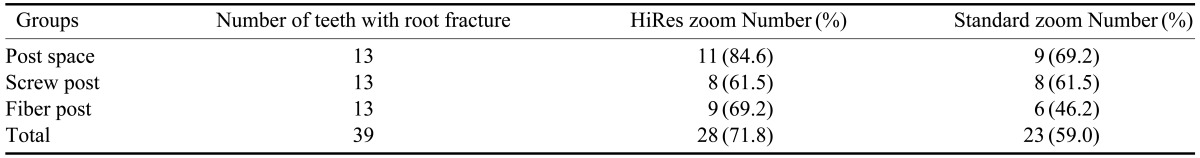
Table 2.
Frequency of correct diagnosis of root fracture in high resolution (HiRes) and standard zoom imaging modes
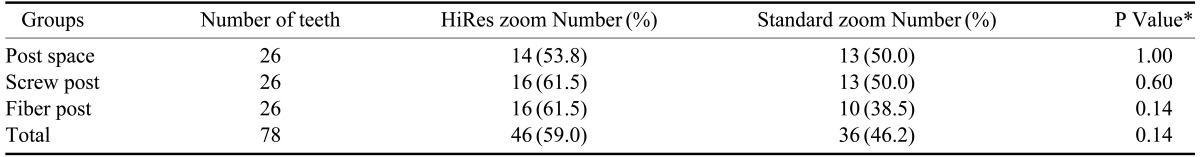
*McNemar test
No significant differences were observed between these imaging modes in each group in the identification of root fracture. As seen in Tables 1 and 2, in the screw post and fiber post groups, true-negative findings in both modes of CBCT were found more frequently in the screw post group.
Sensitivity and specificity levels as well as PPVs and NPVs, respectively, in addition to their LRs are presented in Table 3 for the three groups in each of the different modes. Overall, the sensitivity of the HiRes and standard zoom modes in making the diagnosis of root fracture was 71.79% and 58.97%, and the specificity was 46.15% and 33.33%, respectively. Thus, using the HiRes zoom mode to make an accurate diagnosis of positive and negative root fracture was better. Low sensitivity of both CBCT modes and high specificity of the HiRes mode were observed in the fiber and screw post groups. In the post space group, we found high sensitivity and low specificity of both modes in the diagnosis of root fracture. The highest number of teeth with root fracture detected at the cervical level on the lingual surface were reported.
Table 3.
The effect of root canal restoration on diagnostic values of high resolution (HiRes) and standard CBCT imaging modes in the diagnosis of root fracture
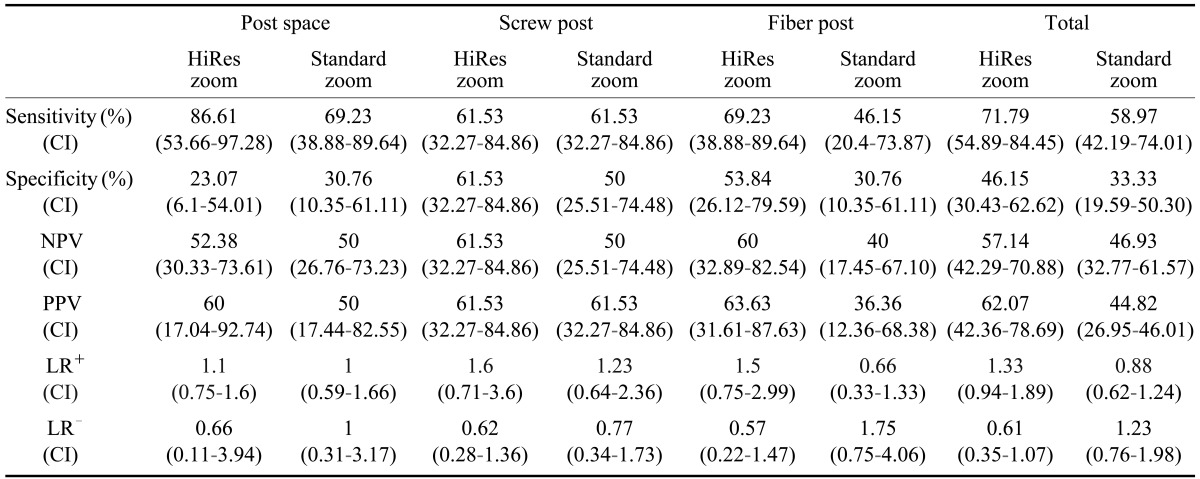
CI: confidence interval, NPV: negative predictive value, PPV: positive predictive value, LR+: positive likelihood ratio, LR-: negative likelihood ratio
Discussion
In this study, using different reconstructed images such as axial and cross-sectional images and considering the different directions of metal artifacts and root fracture were found to be useful in the diagnosis of root fracture. Sometimes root fracture could be masked by an induced artifact. Overall, the artifacts of fiber posts were not significant different compared with those of screw posts. The sensitivity of CBCT in the presence of root canal restorations was lower than their absence; however, it did not influence the specificity. The reasons for lower sensitivity of CBCT modes in the presence of screw and fiber posts included the following: the presence of streak artifacts secondary to the reconstruction of the crown and the treatment of the root canal, an undiagnosable root fracture that was limited to the root apex, and restricted spatial resolution (0.25 mm).9,10,17 No significant differences were observed in any group between these imaging modes in the identification of root fracture.
In our study, the diagnostic values of the HiRes and standard CBCT zoom modes in the diagnosis of root fracture were compared. The results of this study showed that in both zoom modes, the post space group showed the highest true-positive results. This result might have resulted from the lack of the negative effect of the streak artifacts originating from screw or fiber posts. There were no significant differences in the diagnosis of root fracture among the three different groups, even though the HiRes zoom showed a higher frequency of correct diagnosis of root fracture. The improvement in the diagnosis of root fracture could have been due to the smaller voxel size of the HiRes zoom mode (0.125-0.15) in comparison with the standard zoom (0.2-0.24 mm) in our study. The effect of voxel size in the diagnosis of root fracture in other studies14,18 and in detection of other root pathologies such as root resorption19 was confirmed. Dalili et al has reported that the HiRes zoom mode was more sensitive than the standard zoom mode in the detection of small cavities.19 Liedke et al has also found that the images with different voxel resolution (0.2, 0.3, and 0.4 mm) showed a similar sensitivity and specificity in the investigation of external root resorption, but a 0.3-mm voxel resolution allowed for the correct detection of the root resorption cavity with greater probability.20 It should be taken into consideration that observable fracture lines would be more delicate than root resorption; therefore, the images with a smaller voxel size would be recommended in the diagnosis of root fracture.
In addition, the overall sensitivity and specificity in the detection of root fracture were evaluated. The HiRes zoom mode was more accurate in confirming the presence or absence of root fracture compared with the standard mode. In particular, the sensitivity of the HiRes zoom mode was higher than that of the standard zoom mode in the post space group. These findings were similar to the findings of Hassan et al10 and Wang et al11 concerning whether the root canal fillings decreased the sensitivity. A streak artifact from opaque gutta-percha could resemble a root fracture that, in turn, might decrease the sensitivity of CBCT images. In our study, the streak artifacts from the screw and fiber posts also decreased the sensitivity of both CBCT modes. Similarly, in a study of Youssefzadeh et al,21 beam hardening artifacts between gutta-percha and the post restricted the diagnosis of root fracture by CT scan. Hassan et al13 also confirmed the effects of root canal filling as detected by five selected CBCT systems in the diagnosis of root fracture. They found that root canal filling did not influence the sensitivity of CBCT scanners, but it decreased their specificity in the detection of root fracture.
Another critical point is the increased patient exposure to radiation in the HiRes mode in comparison with the standard zoom mode due to the increased FOV and longer exposure time. However, selecting the proper imaging mode should be based on the type of root pathology, root fillings, and restorative materials used, as well as the patient's condition.
The remarks made by the observers in this study proved that the axial images provided more information than the mesiodistal or buccolingual cross-sectional images. This finding concurred with those of Hassan et al14 and Kajan and Taromsari.12
In our study, the diagnoses of root fracture at the cervical third level and on the lingual surface were diagnosed more frequently than in other sites. The thickness of the root in the cervical third could be effective in increasing the contrast resolution to further enhance or achieve a more accurate diagnosis of root fracture.
In conclusion, these two modes of CBCT with their corresponding differences in FOVs and voxel sizes could not be distinguished in making the diagnosis of root fracture in the presence or absence of root restorations.
Acknowledgement
We would like to thank Julie Monti Safari for her dedicated effort in editing the present article. In addition we wish to express our gratitude Oro-Maxillofacial Developmental Diseases Research Center in Rasht, Iran.
Footnotes
This study was financially supported by the Vice Chancellor of Research and Technology of Guilan University of Medical Sciences in Rasht, Iran.
References
- 1.Rivera EM, Walton RE. Longitudinal toot fractures. In: Torabinejad M, Walton RE, editors. Endodontics; principles and practice. 4th ed. St. Louis: Saunders Elsevier; 2009. pp. 108–128. [Google Scholar]
- 2.Meister F, Jr, Lommel TJ, Gerstein H. Diagnosis and possible causes of vertical root fracture. Oral Surg Oral Med Oral Pathol. 1980;49:243–253. doi: 10.1016/0030-4220(80)90056-0. [DOI] [PubMed] [Google Scholar]
- 3.Peciuliene V, Rimkuviene J. Vertical root fractures in endodontically treated teeth: a clinical survey. Stomatologija. 2004;6:77–80. [Google Scholar]
- 4.Hülsmann M, Schäfer E. Problems in endodontics: etiology, diagnosis, and treatment. London: Quintessence; 2009. pp. 353–371. [Google Scholar]
- 5.Mora MA, Mol A, Tyndall DA, Rivera EM. In vitro assessment of local computed tomography for the detection of longitudinal tooth fractures. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;103:825–829. doi: 10.1016/j.tripleo.2006.09.009. [DOI] [PubMed] [Google Scholar]
- 6.Morfis AS. Vertical root fractures. Oral Surg Oral Med Oral Pathol. 1990;69:631–635. doi: 10.1016/0030-4220(90)90248-q. [DOI] [PubMed] [Google Scholar]
- 7.Rud J, Omnell KA. Root fractures due to corrosion. Diagnostic aspects. Scand J Dent Res. 1970;78:397–403. doi: 10.1111/j.1600-0722.1970.tb02088.x. [DOI] [PubMed] [Google Scholar]
- 8.Bargholz C. Vertical tooth and root fractures. In: Hülsmann M, Schäfer E, editors. Problems in endodontics; etiology, diagnosis and treatment. London: Quintessence; 2009. pp. 353–359. [Google Scholar]
- 9.Bernardes RA, de Moraes IG, Húngaro Duarte MA, Azevedo BC, de Azevedo JR, Bramante CM. Use of cone-beam volumetric tomography in the diagnosis of root fractures. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;108:270–277. doi: 10.1016/j.tripleo.2009.01.017. [DOI] [PubMed] [Google Scholar]
- 10.Hassan B, Metska ME, Ozok AR, van der Stelt P, Wesselink PR. Detection of vertical root fractures in endodontically treated teeth by a cone beam computed tomography scan. J Endod. 2009;35:719–722. doi: 10.1016/j.joen.2009.01.022. [DOI] [PubMed] [Google Scholar]
- 11.Wang P, Yan XB, Lui DG, Zhang WL, Zhang Y, Ma XC. Detection of dental root fractures by using cone-beam computed tomography. Dentomaxillofac Radiol. 2011;40:290–298. doi: 10.1259/dmfr/84907460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kajan ZD, Taromsari M. Value of cone beam CT in detection of dental root fractures. Dentomaxillofac Radiol. 2012;41:3–10. doi: 10.1259/dmfr/25194588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Metska ME, Aartman IH, Wesselink PR, Özok AR. Detection of vertical root fractures in vivo in endodontically treated teeth by cone-beam computed tomography scans. J Endod. 2012;38:1344–1347. doi: 10.1016/j.joen.2012.05.003. [DOI] [PubMed] [Google Scholar]
- 14.Hassan B, Metska ME, Ozok AR, van der Stelt P, Wesselink PR. Comparison of five cone beam computed tomography systems for the detection of vertical root fractures. J Endod. 2010;36:126–129. doi: 10.1016/j.joen.2009.09.013. [DOI] [PubMed] [Google Scholar]
- 15.Liang X, Jacobs R, Hassan B, Li L, Pauwels R, Corpas L, et al. A comparative evaluation of Cone Beam Computed Tomography (CBCT) and Multi-Slice CT (MSCT) Part I. On subjective image quality. Eur J Radiol. 2010;75:265–269. doi: 10.1016/j.ejrad.2009.03.042. [DOI] [PubMed] [Google Scholar]
- 16.Katsumata A, Hirukawa A, Okumura S, Naitoh M, Fujishita M, Ariji E, et al. Relationship between density variability and imaging volume size in cone-beam computerized tomographic scanning of the maxillofacial region: an in vitro study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;107:420–425. doi: 10.1016/j.tripleo.2008.05.049. [DOI] [PubMed] [Google Scholar]
- 17.Zhang Y, Zhang L, Zhu XR, Lee AK, Chambers M, Dong L. Reducing metal artifacts in cone-beam CT images by preprocessing projection data. Int J Radiat Oncol Biol Phys. 2007;67:924–932. doi: 10.1016/j.ijrobp.2006.09.045. [DOI] [PubMed] [Google Scholar]
- 18.Özer SY. Detection of vertical root fractures by using cone beam computed tomography with variable voxel sizes in an in vitro model. J Endod. 2011;37:75–79. doi: 10.1016/j.joen.2010.04.021. [DOI] [PubMed] [Google Scholar]
- 19.Dalili Z, Taramsari M, Mousavi Mehr SZ, Salamat F. Diagnostic value of two modes of cone-beam computed tomography in evaluation of simulated external root resorption: an in vitro study. Imaging Sci Dent. 2012;42:19–24. doi: 10.5624/isd.2012.42.1.19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Liedke GS, da Silveira HE, Silveira HL, Dutra V, de Figueiredo JA. Influence of voxel size in the diagnostic ability of cone beam tomography to evaluate simulated external root resorption. J Endod. 2009;35:233–235. doi: 10.1016/j.joen.2008.11.005. [DOI] [PubMed] [Google Scholar]
- 21.Youssefzadeh S, Gahleitner A, Dorffner R, Bernhart T, Kainberger FM. Dental vertical root fractures: value of CT in detection. Radiology. 1999;210:545–549. doi: 10.1148/radiology.210.2.r99ja20545. [DOI] [PubMed] [Google Scholar]