Abstract
Periapical cemento-osseous dysplasia (PCOD) is a subtype of cemento-osseous dysplasia that usually occurs in middle-aged black women. This report described a case of a 45-year-old Iranian woman who was diagnosed with PCOD on the basis of cone beam computed tomographic (CBCT) findings. CBCT enabled detailed visualization of the bone changes. This report described the special radiographic characteristics of PCOD, including discontinuity of the lingual cortex on the CBCT sectional and three-dimensional images.
Keywords: Cementoma, Jaw Neoplasms, Mandible, Cone-Beam Computed Tomography
Cemento-osseous dysplasia (COD) is the most common fibro-osseous lesion faced in clinical practice and affects the tooth-bearing areas of the jaws.1,2 COD is represented as a benign lesion arising from undifferentiated cells of the periodontal ligament tissues.3 This lesion is classified into three subtypes according to its clinical and radiographic features: periapical, focal, and florid.4
Periapical cemento-osseous dysplasia (PCOD) occurs most commonly in the anterior mandible of patients older than 30 years of age. There is a significant tendency toward female patients and approximately 70% of cases affect blacks.5 PCOD is asymptomatic and the involved teeth are vital.4,5
This lesion appears occasionally in radiographs taken for other reasons. Most cases of the PCOD lesions have a well-defined periphery. Often a radiolucent border of varying width is present.6 It shows three different features according to its stage. In the first stage or osteolytic stage, circular or elliptical resorption areas are seen in the lesion. In the second stage or cementoblastic stage, which is also called the mixed radiolucent-radiopaque stage, small calcifications are seen within the lesion. The final or mature stage is a completely radiopaque lesion.5 It is unusual for a PCOD to become large enough to produce a detectable expansion of the cortical plate.3
The diagnosis of PCOD can be made on the basis of the appropriate radiological and clinical characteristics. Commonly, no treatment is required and only regular follow-up examinations are advised.7
This report described a case of PCOD according to its cone beam computed tomographic (CBCT) findings. CBCT enabled detailed visualization of different aspects of the lesion in multiple planes.
Case Report
A 45-year-old Iranian woman was referred to the private clinic in the city of Hamadan for implant consultation. Her past medical history was not notable, and there was no evidence of systemic disease. She had no history of trauma to the mandible. In the extra-oral examination, no abnormal symptoms were observed. Intra-oral examination revealed normal oral mucosa, the absence of soft tissue expansion, and teeth of a normal color. Periodontal tissues were normal. All of the teeth were asymptomatic, with no pain or tenderness on percussion or palpation. The involved teeth were vital in an electric stimulation test.
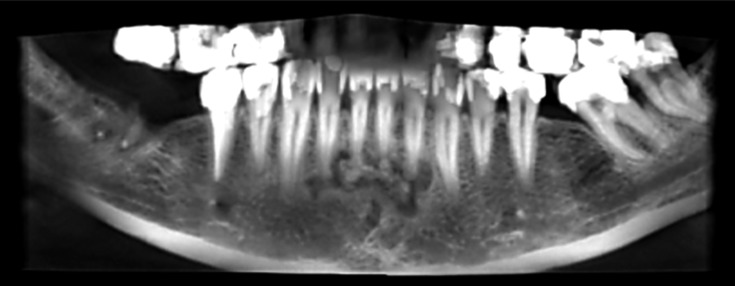
For assessment before implant insertion, CBCT had been ordered. During evaluation of the implant insertion areas on Promax3D CBCT (Planmeca OY, Helsinki, Finland), a radiolucent-radiopaque mixed lesion located on the apices of the lower incisors was observed. On the axial, sagittal, and coronal CBCT images, the extension of the lesion was observed from the mesial side of the right mandibular lateral incisor to the distal side of the left mandibular lateral incisor. It was a multifocal lesion in which solitary lesions were reached together and made a larger lesion. The total dimension of the lesion was about 16.6 mm in the mesiodistal direction and 6.9 mm in the longest superior-inferior direction. On the panoramic reconstructed CBCT image, the lesion associated with the left mandibular lateral incisor was radiolucent, whereas the lesion on the apex of the left central incisor was mixed radiolucent-radiopaque and the lesion associated with the right central incisor was radiopaque with a radiolucent rim around the lesion of this tooth (Fig. 1).
Fig. 1.
A reformatted panoramic CBCT image shows a multifocal lesion extending from the mesial side of the right mandibular lateral incisor to the distal side of the left mandibular lateral incisor.
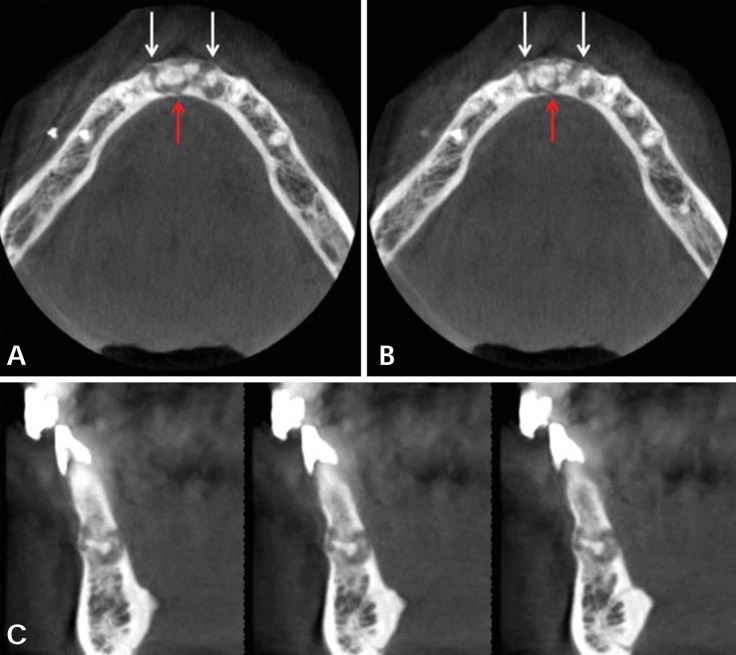
By using the CBCT, the state of the lesion relative to the buccal and lingual cortical plates could be assessed, which might not be possible on the conventional radiographs. On the axial image, two expansion and thinning areas of the buccal cortex were revealed. One of them was located at the mesial side of the right canine and the other between the left central and lateral incisors (Fig. 2A and B). On the axial and cross-sectional images, the discontinuity of the lingual cortex was found at the area between the two central incisors on several consecutive sectional images (Fig. 2A-C). This cortical discontinuity was more obvious on the three-dimensional (3D) CBCT images (Fig. 3). However, it should be considered that the cortical bone could be seen to have destruction on 3D images, even though it would have been thin without discontinuity on the cross-sectional images.
Fig. 2.
A. An axial CBCT image shows the expansion of the buccal cortex (white arrows) and discontinuity of the lingual cortex (red arrow). B. Another axial CBCT image shows the same features as A. C. Cross-sectional CBCT images show the discontinuity of the lingual cortical plate.
Fig. 3.
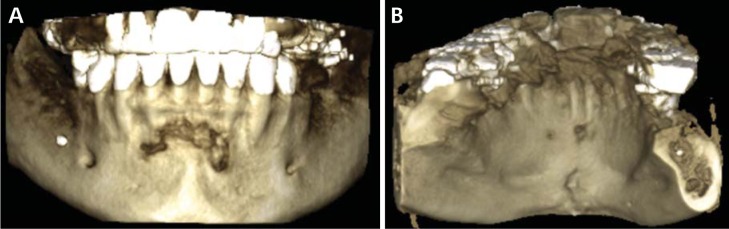
Three-dimensional reconstructed CBCT images of the mandible. A. The frontal view shows erosion of the buccal cortex of the lesion. B. The lingual view shows that the lesion erodes the lingual cortex.
On the digital periapical radiograph that was taken for further follow-up, a typical feature of PCOD was observed (Fig. 4). There was no root resorption or tooth displacement. The lamina dura surrounding the apical areas of the involved teeth was lost. Periodontal ligament space widening was found, especially around the root of the left lateral incisor.
Fig. 4.
A periapical radiograph shows a mixed radiolucent-radiopaque appearance of the lesion, located on the apices of the lower incisors. The lamina dura surrounding the apical areas of the involved teeth is lost.
Based on the patient clinical and radiographic findings, a diagnosis of multifocal periapical cemento-osseous dysplasia was made. No treatment was considered. The only recommendation was periodic radiographic follow-up.
Discussion
The term cemento-osseous dysplasia is well known and widely used. PCOD is a specific lesion within this group of conditions that usually occurs in middle-aged black women.4 A systematic review of the literature on COD indicated an ethnic distribution of 59%, 37%, and 3% for blacks, Asians (Japanese, Chinese, and Korean), and Caucasians including Indian cases, respectively, in case reports.8 Zegarelli et al reported the incidence of PCOD in the general population to be 2-3/1000.9
Periapical cemento-osseous dysplasia generally does not cause cortical bone expansion or perforation.9-12 Alsufyani and Lam reviewed the clinical and radiographic characteristics of 118 patients with COD.13 They showed that 71.6% of 118 patients had no cortical expansion, 76% had intact lamina dura, and 93% had a normal periodontal ligament space. None of them had mandibular cortical plate destruction.
Modern advances in imaging help the dentist to use the CBCT with the appropriate field of view and spatial resolution; therefore, the internal mineralized structure of the pathologic lesions can be investigated with a low radiation dose.14 Axial CBCT images clearly demonstrate the location and extension of the lesion. The expansion and perforation of the cortical plates can be evaluated on CBCT even if they are slight. This report showed the discontinuity of the lingual cortex on some axial and cross-sectional CBCT images. This characteristic of the lesion was an unusual feature among the cases of PCOD reported up to now that may be due to its large size and needed to be checked in further regular follow-ups. This feature also could be found in an exaggerated fashion on the 3D CBCT images. Although 3D imaging could help the radiologist in diagnosing the lesion for the first look, it should be noted that it is not a reliable viewing modality for assigning the real status of the lesion in relation to its surrounding bone structures.
In many COD cases that have been misdiagnosed and/or mismanaged, the lesions were identified in their early stages as a periapical rarefying osteitis such as periapical abscess, granuloma, or cyst, and unnecessary endodontic treatment was performed. Therefore, vitality tests are especially important for differential diagnosis.
In the radiolucent-radiopaque mixed stage and the radiopaque stage, the differential diagnosis might include chronic sclerosing osteomyelitis, cementoossifying fibroma, odontoma, cementoblastoma, and osteoblastoma.13 Periapical cemento-osseous dysplasia is usually detected on routine radiological examinations. However, the differential diagnosis of our case could be calcifying cystic odontogenic tumor and cemento-ossifying fibroma.
By using CBCT discrimination of PCOD from these lesions that exhibit similar internal calcification on conventional radiography, would be more accurate.
High density mass in PCOD which is centered in low density area is different from findings of calcifying cystic odontogenic tumor in which calcification is observed at or near the cyst wall.15 Also, cemento-ossifying fibroma has more obvious concentric buccolingual expansion on multiplanar CBCT image.
Unless PCOD is symptomatic, treatment is usually not needed because development and maturation of the lesion is self-limiting. Intervention may cause secondary infection of the cementum-like radiopacities, which may in turn induce osteomyelitis in these lesions.13 However, if PCOD demonstrates unusual changes or becomes symptomatic, surgical intervention would then be needed.7 This case was considered as no treatment with only periodic follow-up check.
References
- 1.Eversole R, Su L, ElMofty S. Benign fibro-osseous lesions of the craniofacial complex. A review. Head Neck Pathol. 2008;2:177–202. doi: 10.1007/s12105-008-0057-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Thakkar N, Horner K, Sloan P. Familial occurrence of periapical cemental dysplasia. Virchows Arch A Pathol Anat Histopathol. 1993;423:233–236. doi: 10.1007/BF01614776. [DOI] [PubMed] [Google Scholar]
- 3.Kawai T, Hiranuma H, Kishino M, Jikko A, Sakuda M. Cemento-osseous dysplasia of the jaws in 54 Japanese patients: a radiographic study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1999;87:107–114. doi: 10.1016/s1079-2104(99)70303-3. [DOI] [PubMed] [Google Scholar]
- 4.Komabayashi T, Zhu Q. Cemento-osseous dysplasia in an elderly Asian male: a case report. J Oral Sci. 2011;53:117–120. doi: 10.2334/josnusd.53.117. [DOI] [PubMed] [Google Scholar]
- 5.Falace D, Cunningham C. Periapical cemental dysplasia: simultaneous occurrence in multiple maxillary and mandibular teeth. J Endod. 1984;10:455–456. doi: 10.1016/S0099-2399(84)80269-1. [DOI] [PubMed] [Google Scholar]
- 6.Alsufyani NA, Lam EW. Cemento-osseous dysplasia of the jaw bones: key radiographic features. Dentomaxillofac Radiol. 2011;40:141–146. doi: 10.1259/dmfr/58488265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.DiFiore P, Bowen S. Cemento-osseous dysplasia in African-American men: a report of two clinical cases. J Tenn Dent Assoc. 2010;90:26–29. [PubMed] [Google Scholar]
- 8.MacDonald-Jankowski DS. Florid cemento-osseous dysplasia: a systematic review. Dentomaxillofac Radiol. 2003;32:141–149. doi: 10.1259/dmfr/32988764. [DOI] [PubMed] [Google Scholar]
- 9.Zegarelli E, Kutscher A, Napoli N, Iurono F, Hoffman P. The cementoma. A study of 230 patients with 435 cementomas. Oral Surg Oral Med Oral Pathol. 1964;17:219–224. doi: 10.1016/0030-4220(64)90145-8. [DOI] [PubMed] [Google Scholar]
- 10.Scholl RJ, Kellett HM, Neumann DP, Lurie AG. Cysts and cystic lesions of the mandible: clinical and radiologic-histopathologic review. Radiographics. 1999;19:1107–1124. doi: 10.1148/radiographics.19.5.g99se021107. [DOI] [PubMed] [Google Scholar]
- 11.Manganaro AM, Millett GV. Periapical cemental dysplasia. Gen Dent. 1996;44:336–339. [PubMed] [Google Scholar]
- 12.Alawi F. Benign fibro-osseous diseases of the maxillofacial bones. A review and differential diagnosis. Am J Clin Pathol. 2002;118(Suppl):S50–S70. doi: 10.1309/NUXA-JUT9-HA09-WKMV. [DOI] [PubMed] [Google Scholar]
- 13.Alsufyani NA, Lam EW. Osseous (cemento-osseous) dysplasia of the jaws: clinical and radiographic analysis. J Can Dent Assoc. 2011;77:b70. [PubMed] [Google Scholar]
- 14.Macdonald-Jankowski DS. Focal cemento-osseous dysplasia: a systematic review. Dentomaxillofac Radiol. 2008;37:350–360. doi: 10.1259/dmfr/31641295. [DOI] [PubMed] [Google Scholar]
- 15.Ariji Y, Ariji E, Higuchi Y, Kubo S, Nakayama E, Kanda S. Florid cemento-osseous dysplasia. Radiographic study with special emphasis on computed tomography. Oral Surg Oral Med Oral Pathol. 1994;78:391–396. doi: 10.1016/0030-4220(94)90074-4. [DOI] [PubMed] [Google Scholar]