Abstract
Adrenal infarction is an uncommon cause of adrenal insufficiency. We herein present unique occurrence of bilateral adrenal infarction detected on imaging in a young female with known history of Crohn's disease. The patient responded well to steroids and is on follow up. To our knowledge, this is the first case reported in English literature of adrenal infarct associated with Crohn's disease as extraintestinal manifestation.
Keywords: Adrenal infarction, adrenal insufficiency, Crohn's disease, extraintestinal manifestation
INTRODUCTION
Bilateral primary adrenal infarction is a rare cause of flank pain and adrenal insufficiency. It is usually due to thrombosis of the main adrenal vein or secondary to microvascular thrombosis in the adrenal parenchyma. Adrenal infarction has been best described in the setting of antiphospholipid-antibody syndrome.[1,2] Recently it has also been described in conditions like heparin-induced thrombocytopenia and myelodysplastic syndrome.[3,4] We describe a case of a 25-year-old female patient with history of Crohn's disease who presented with bilateral adrenal infarcts without any computerized tomography (CT) or magnetic resonance imaging (MRI) evidence of hemorrhage. To our knowledge, this is the first case with association between Crohn's disease and bilateral adrenal infarction.
CASE REPORT
A 25-year-old female patient presented with gradual onset right shoulder pain for 1 week, which was constant and achy in nature and radiated to the left shoulder, down to her back and bilateral flanks. The pain was worse on the right side. She also complained of weakness, decreased oral intake and nausea but did not have any fever, vomiting or diarrhea. She was diagnosed with Crohn's disease since the year 1995 with extensive perianal disease complicated by abscess formation and rectovaginal fistula. She had also been put on filgrastim, a granulocyte colony-stimulating factor (G-CSF) analog for chronic leucopenia secondary to azathioprine treatment for Crohn's disease. Physical examination at the time of current admission revealed pallor, mild tachycardia with a heart rate of 115/minute and blood pressure of 96/56 mm Hg. There was epigastric and costovertebral tenderness with mild voluntary guarding. There was no rebound tenderness and her bowel sounds were faint. WBC count was 4.5 × 109/L. Although the patient did not have significant electrolyte abnormalities (sodium: 137 mEq/L, potassium: 4.6 mEq/L), there was postural tachycardia and hypotension.
MRI of the spine and sacroiliac joints did not reveal any evidence of infection/inflammation/disc disease that could be attributed as a cause of the pain. CT scan of abdomen and pelvis with contrast showed some edema in the rectum in keeping with her Crohn's disease as well as some mild terminal ileitis. There was also increased thickening and hypodensities in both the adrenals [Figure 1a]. Further evaluation with MRI [Figure 1b-d] revealed that the adrenals were bulky bilaterally. They showed hypointense signal on T1WI and hyperintense signal intensity on T2WI without any demonstrable hemorrhage. Following administration of gadolinium-based contrast, there was no enhancement of the parenchyma signifying a lack of viable parenchyma, based on which a diagnosis of adrenal infarction without hemorrhage was made.
Figure 1.
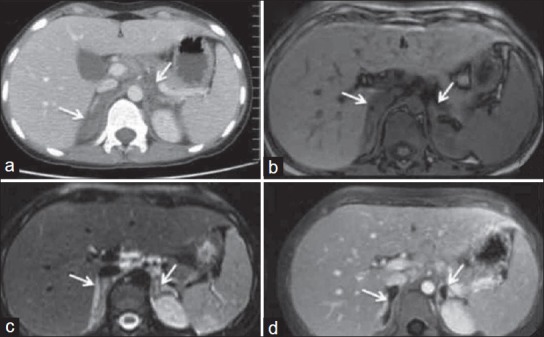
(a) Axial contrast-enhanced CT image at the level of adrenal glands reveals bilateral thickened, hypodense poorly enhancing infarcted adrenal glands. (b) axial T1W, (c) axial T2W MR images show T1 hypointense, T2 hyperintense adrenal gland secondary to edema, (d) postcontrast image shows poor parenchymal enhancement with minimal peripheral capsular enhancement in keeping with adrenal infarction
Biochemical confirmation of adrenal insufficiency was made by low plasma cortisol (21 nmol/l) and ACTH stimulation test that failed to raise the plasma cortisol levels to more than 25 nmol/l. She did not have any altered skin pigmentation or any history of hypotensive episodes in the past making the possibility of a long standing primary adrenal insufficiency unlikely. The PTT and INR were normal. Anticardiolipin antibodies and Lupus-like anticoagulant were negative. She was put on replacement steroids for which she showed a good response. Her appetite improved and she was discharged with complete resolution of pain.
DISCUSSION
Bilateral adrenal infarction is a rare, but a well-recognized cause of adrenal insufficiency. Pathogenesis is likely due to microvascular or main adrenal venous thrombosis. Adrenals are highly vascular with arterial supplies from the inferior phrenic artery, the aorta, and the renal artery. However, there is only a single draining vein. These alterations in flow dynamics in the medullary sinusoids may predispose the gland to microvascular thrombosis in procoagulable states and during episodes of hypotension, and may lead to infarction. Usually this may be complicated by hemorrhage due to ischemic necrosis, reperfusion injury, anticoagulant therapy or a combination of these factors.
The patient presented with biochemical evidence of adrenal adrenal insuffieciency, pain in back, flanks and right shoulder. The shoulder pain was presumably due to diaphragmatic irritation. Though the flank pain has traditionally been ascribed to hemorrhage in the gland, a recent study[5] suggests that it is more likely due to ischemic necrosis and inflammatory swelling. The findings in our patient would support the latter view. T1WI in our patient did not show hyperintense areas to suggest any hemorrhage and T2WI showed no blooming. T2-weighted images however, showed hyperintense signal which denoted edematous change related to the inflammatory swelling of the adrenal gland. Demonstration of hemorrhage is important as it may alter the treatment, especially the need for anticoagulation.[6]
Bilateral adrenal infarctions have previously been described in a setting of antiphospholipid-antibody syndrome. Antiphospholipid antibodies target the late endosomal and lysosomal lysobisphosphatidic acid (LBPA) in the cholesterol-rich cells of the adrenal cortex leading to secretion of lysosomal proteinases like cathepsin D which leads to a local procoagulant state.[7] Upregulation of vascular cell adhesion molecule-1 (VCAM-1) and E-selectin by antiphospholipid antibodies leading to endothelial damage as well as displacement of Annexin V, an anticoagulant protein by antiphospholipid antibodies can further lead to microthrombosis.[7] Other targets like beta-2-GPI have also been implicated.
Crohn's disease is recognized to be a hypercoagulable state which can be attributed to a variety of factors including thrombocytosis as well as increased levels of clotting factors V and VIII, fibrinogen, accelerated thromboplastin generation, acquired antithrombin III deficiency, and decreased protein C and protein S. However, no single consistent coagulation abnormality has been identified.[8] A wide range of infectious agents (mycobacterial, bacterial, fungal and viral agents) can also lead to adrenal insufficiency. Though our patient had chronic leucopenia and was on filgrastim, the normal WBC count at presentation as well as absence of fever or any other sign of sepsis makes infectious etiology unlikely in our case.
Bilateral adrenal infarcts have not been described in Crohn's disease previously. The absence of antiphospholipid antibodies in our patient might suggest that pathways other than those elucidated previously may be involved in local microthrombosis and resulting adrenal infarctions.
CONCLUSION
Thus, we herein report an unusual extraintestinal complication occurring as a bilateral adrenal infarction with resultant adrenal insufficiency in Crohn's disease. CT and MRI serve as useful aids in diagnosis as well as identifying hemorrhage which could alter the management.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Vlot AJ, van der Molen AJ, Muis MJ, Fijnheer R. Antibodies that stop the adrenals in their tracks. Lancet. 2001;358:382. doi: 10.1016/S0140-6736(01)05559-3. [DOI] [PubMed] [Google Scholar]
- 2.Marie I, Levesque H, Heron F, Cailleux N, Borg JY, Courtois H. Acute adrenal failure secondary to bilateral infarction of the adrenal glands as the first manifestation of primary antiphospholipid antibody syndrome. Ann Rheum Dis. 1997;56:567–8. doi: 10.1136/ard.56.9.567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bakaeen FG, Walkes JC, Reardon MJ. Heparin-induced thrombocytopenia associated with bilateral adrenal hemorrhage after coronary artery bypass surgery. Ann Thorac Surg. 2005;79:1388–90. doi: 10.1016/j.athoracsur.2003.09.108. [DOI] [PubMed] [Google Scholar]
- 4.Lockett HA, Hamilton-Wood C, Vaidya B. Addison's disease due to bilateral adrenal infarction in a patient with myelodysplastic syndrome. Eur J Gen Med. 2011;8:72–4. [Google Scholar]
- 5.Michiels JJ, Berneman Z, Schroyens W, Krestin GP. Bilateral adrenal swelling as a cause of chest, back, and upper abdominal pain in essential thrombocythemia and polycythemia vera is due to microvascular ischemic thrombosis rather than to hemorrhage. Ann Hematol. 2002;81:691–4. doi: 10.1007/s00277-002-0500-5. [DOI] [PubMed] [Google Scholar]
- 6.Riddell AM, Khalili K. Sequential adrenal infarction without MRI-detectable hemorrhage in primary antiphospholipid-antibody syndrome. AJR Am J Roentgenol. 2004;183:220–2. doi: 10.2214/ajr.183.1.1830220. [DOI] [PubMed] [Google Scholar]
- 7.Berneis K, Buitrago-Tellez C, Muller B, Keller U, Tsakiris DA. Antiphospholipid syndrome and endocrine damage: Why bilateral adrenal thrombosis? Eur J Haematol. 2003;71:299–302. doi: 10.1034/j.1600-0609.2003.00145.x. [DOI] [PubMed] [Google Scholar]
- 8.Hatoum OA, Miura H, Binion DG. The vascular contribution in the pathogenesis of inflammatory bowel disease. Am J Physiol Heart Circ Physiol. 2003;285:H1791–6. doi: 10.1152/ajpheart.00552.2003. [DOI] [PubMed] [Google Scholar]


