Abstract
Pneumomediastinum (PM) is defined as the presence of free air in the mediastinal cavity. It is often regarded as a revealing sign of a more serious medical condition. PM is broken down into two categories, one, with an instigating event, referred to as secondary PM. The other is when free air is discovered in the mediastinal cavity without a clear etiology, referred to as spontaneous pneumomediastinum (SPM). Often misdiagnosed due to the vague nature of presenting symptoms, SPM must be part of the differential diagnosis of a chest pain patient to expedite discovery and if necessary, management. A MedLine/PubMED search was performed identifying all relevant articles with “SPM” in the title. Six case series were reviewed to determine what clinical scenario constitutes a possible case of SPM. Results showed that almost all patients with SPM exhibited some chest pain, but Hamman’s crunch was present in only one-fifth of patients. Patients with certain pre-existing pulmonary diseases showed a greater propensity for the presence of free air in the mediastinal cavity. SPM must be diagnosed and managed promptly due to rare, but serious complications and any chest pain with an unknown etiology should contain SPM in the differential diagnosis.
Keywords: Chest pain, Mediastinal emphysema, Spontaneous pneumomediastinum, Subcutaneous emphysema
Introduction
The mediastinal cavity is defined as the area demarcated by the pleural cavities laterally, the thoracic inlet superiorly and the diaphragm inferiorly.[1] Pneumomediastinum (PM) also referred to as mediastinal emphysema was originally described in 1819 by Laλnnec and[2,3] is defined as the presence of free air in the mediastinal cavity. The discovery of free air in the mediastinal cavity is often thought of as a phenomenon secondary to a more serious medical condition. PM is broken down into two categories [Figure 1], one is as a result of trauma or caused iatrogenically due to endoscopic or other therapeutic procedures. Such cases are referred to as secondary PM, with a clear and causative factor. The second is the presence of free air in the mediastinal cavity without a clear etiology. In this review, we explore instances where PM is discovered without an identifiable source, which is referred to as spontaneous pneumomediastinum (SPM). The diagnosis of SPM is often obscured due to the fact that chest pain and dyspnea, two of the most common presenting symptoms, are a sign of a multitude of cardio-pulmonary pathologies. A consensus needs to be formed regarding presenting symptoms, clinical signs and medical conditions pre-disposing to the formation of SPM. Our results are presented along with a review of the literature outlining the clinical presentation, diagnostic algorithm as well as the therapeutic process in the setting of SPM.
Figure 1.
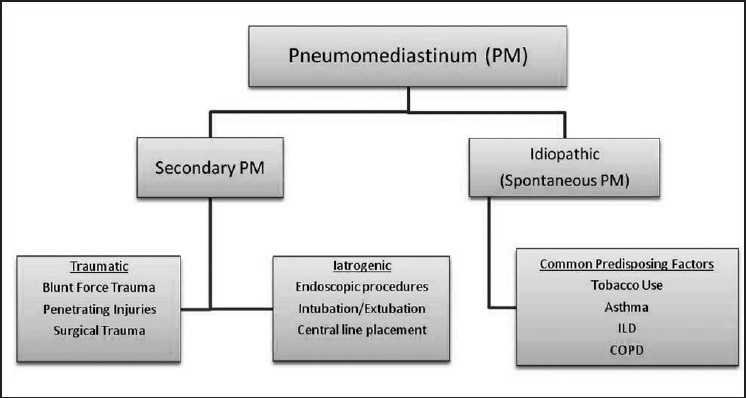
Classification scheme of pneumomediastinum. Pneumomediastinum can be broken down into two main categories, secondary and idiopathic. Both categories have multiple causes
The aim of this review is to outline the clinical scenario of a case of SPM. A MEDLINE/PubMed search was performed with the objective of identifying all articles published in the English language between January 1950 and February 2013 with “SPM” in the title. Combinations of medical subject heading terms including “SPM,” “causes of SPM” and “symptoms of PM” were used. We largely selected publications from the last 10 years, but did not exclude any older publications that were widely referenced and highly regarded. We also searched the reference lists of articles identified by this search strategy and selected those we judged to be relevant. All pertinent reports were retrieved and the relative reference lists were systematically searched in order to identify any potential additional studies that could be included. All data was accessed between March and April 2013.
A total of six case series were selected and reviewed, which included a total of 201 patients that were admitted to their respected hospitals where an eventual diagnosis of SPM was established.[4,5,6,7,8,9] The range of ages was 3-84 with an average age of 27.25 years (aggregate). Majority of patients, 74% (149 of 201) were male and 26% (52 of 201) were female.[4,5,6,7,8,9]
Features of Presentation
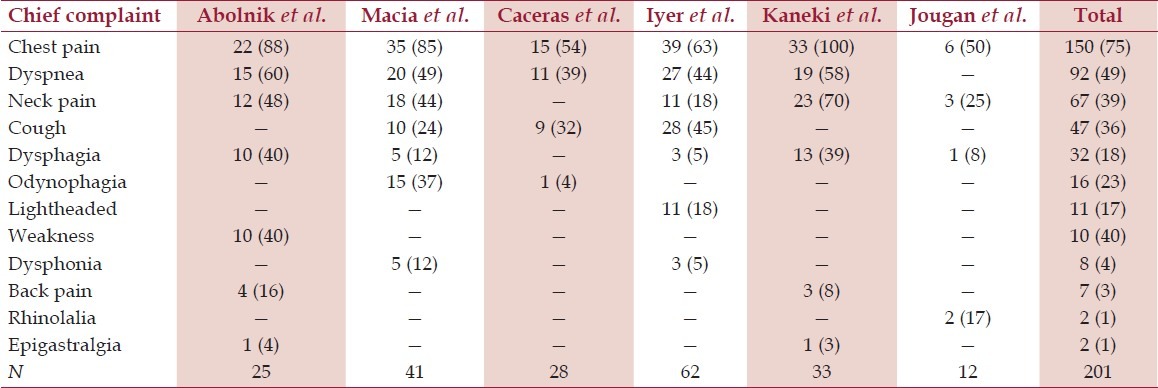
Of the six case series reviewed, the most common presenting symptom was chest pain occurring in 75% of patients (150 of 201) [Table 1]. Other less common symptoms included dyspnea in 49%,[4,5,6,7,8] cough in 36%,[5,6,7] neck pain in 36%[4,5,7,8,9] and dysphagia in 18%.[4,5,7,8,9] There were also sporadic complaints of odynophagia, lightheadedness, weakness, dysphonia, back pain, nasally sounding voice (rhinolalia) and central abdominal pain (epigastralgia)[4,5,6,7,8,9][Table 1].
Table 1.
Chief complaints prior to diagnosis of spontaneous pneumomediastinum
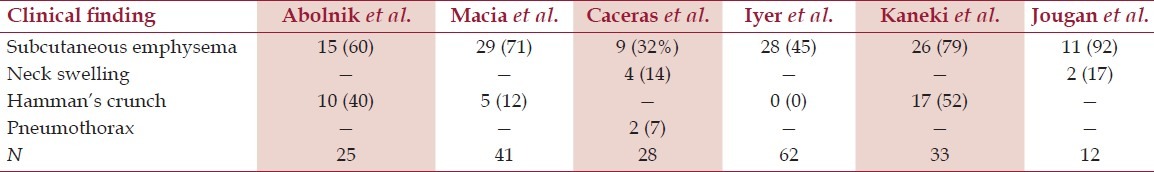
Clinical examination of these patients revealed the presence of subcutaneous emphysema in 58% patients[4,5,6,7,8,9] [Table 2]. However, the presence of Hamman’s crunch, a crunching or bubbling sound over the mediastinum synchronous with the heart beat (Hamman’s sign)[1,2,3] was only observed in 18%[4,5,7,8,9] of SPM patients. There were sporadic findings of neck swelling as well as associated pneumothorax.[6]
Table 2.
Clinical findings in spontaneous pneumomediastinum patients
Pre-disposing factors
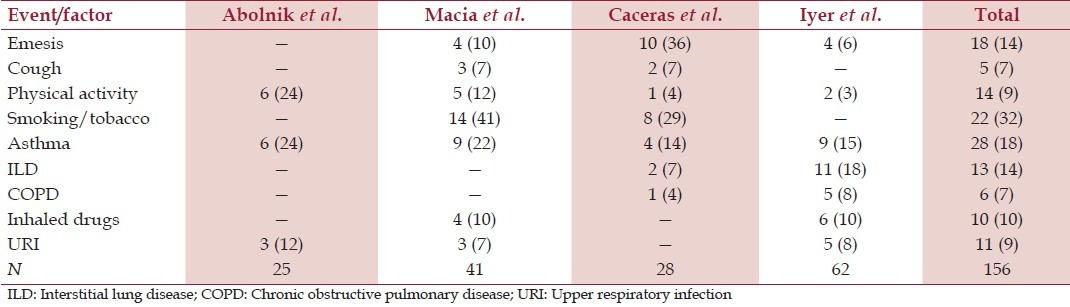
Of the six case series reviewed, four of them, totaling 156 patients, discussed possible triggering events or pre-disposing risk factors of SPM [Table 3]. Of the reporting case series, a positive history of smoking or tobacco use existed in 32%[5,6] of patients. A pre-existing diagnosis of asthma existed in 18%[4,5,6,7] of patients, interstitial lung disease (ILD) existed in 14%[6,7] and a recent history of upper respiratory infection was present in 9%[4,5]. A review of triggering events showed that emesis occurred in 14%[5,6,7] of patients, strenuous physical activity in 9%[4,5,6,7] of patients and bouts of cough in 7%[5,6] of patients.
Table 3.
Triggering event and pre-existing condition/risk factors for spontaneous pneumomediastinum
Presentation
Though, this review focuses on the idiopathic form of PM it is important to mention that clinical presentation of SPM and mild secondary PM may be difficult to differentiate, so every effort must be made to eliminate possible secondary causes. Patients diagnosed to have SPM tend to be young, thin, males who present with arbitrary symptoms of chest pain, cough and dyspnea.[8] Due to the vague nature of these symptoms, the diagnosis requires a high-level of clinical suspicion. It has been estimated that up to 30% or more cases of SPM may go initially undiagnosed.[8]
Spontaneous mediastinum can also occur in a setting of a pre-existing pulmonary condition. A history of asthma and associated coughing bouts has been reported as a possible factor in the development of SPM in up to 25% of cases.[10] Chronic obstructive pulmonary disease (COPD), ILD and recent history of an upper respiratory tract infection have also all been reported. Up to 32% of patients in reporting case series had a history of tobacco use, primarily smoking.[5,6]
SPM has also been linked to certain triggering events such as bouts of emesis, retching, cough and physical sporting activities [Table 3].[5,6,7] Though uncommon, SPM has also been identified in situations such as childbirth,[11] forceful straining during exercise, straining at passing stool, coughing and sneezing.[12]
Diagnosis
Majority of patients with eventual diagnosis of SPM presented with chest pain. The initial differential diagnosis is wide and includes pulmonary, cardiac, musculoskeletal and esophageal etiologies due to the vague nature of presenting symptoms. Eventually, majority causes can be safely diagnosed with a thorough history, detailed physical examination, electrocardiographic as well as radiographic or endoscopic assessment.[13] Though, it was Hamman in 1939 that first reported of his pathognomonic sign for subcutaneous emphysema, it is not always observed in cases of SPM. Review of the case series showed that subcutaneous emphysema is present in majority of patients, but only a small percentage show a positive Hamman’s sign.[4,5,7,8] To make a definitive diagnosis, diagnostic imaging must be part of the work-up [Figure 2]. Chest radiography is almost always the primary imaging technique of choice, which can identify SPM in up to 90% of cases.[8] There are certain radiological signs to look for in suspected cases of PM. If there is sufficient air, the thymus can become elevated to produce the thymic sail sign, which is more common in a pediatric population.[14] Another classical sign indicating free air in the mediastinum is called the “ring sign,” which is caused by air surrounding the pulmonary artery or either of its main branches, especially when the air surrounds the intramediastinal segment of the right pulmonary artery.[15] If a definitive diagnosis can be made with a plain chest film, no further testing is needed and the patient may be observed. However, in cases where chest film is not apparent computed tomography (CT) scanning is always diagnostic.[16]
Figure 2.
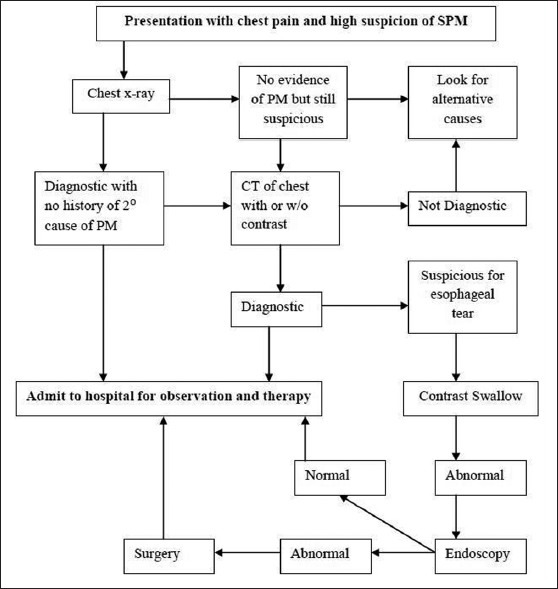
Diagnostic workflow for patients highly suspicious of spontaneous pneumomediastinum. Chest pain suspicious of spontaneous pneumomediastinum can be initially evaluated with a plain chest radiograph. Result depending, further investigations may be ordered
Management
Usually, SPM is not part of the differential diagnosis and it is treated as another causative factor of chest pain, dyspnea and wheezing, i.e., asthma or COPD exacerbation. SPM usually follows a benign course and management is, in most cases conservative. Majority of patients admitted to the hospital are treated with analgesics, rest, oxygen therapy, bronchodilators and occasionally antibiotic treatment.[4] Pure oxygen treatment increases the diffusion pressure of nitrogen in the interstitium and promotes rapid absorption of the free air.[17] If any pre-disposing condition (asthma, infection, airway obstruction, etc.) is responsive to pharmacological management then SPM is self-limiting.[18]
Once released from the hospital SPM patients may be followed on an out-patient basis with serial chest radiographs or CT scans until complete resolution. In addition, bed rest is a vital part of conservative management to help expedite the resolution of SPM to avoid any further complications.
Complications
Though complications are rare in SPM, prompt diagnosis and management are imperative to prevent further progression. In laboratory experiments induced by Macklin and Macklin, SPM showed a possibility to convert to tension or malignant PM,[17] which may lead to cardiac or great vessel compression. Cases of persistent mediastinal free air have been reported that suggest air leaking into the pericardial sac can result in pneumopericardium.[18] Similar mechanisms can lead to free air reaching the retropharyngeal and the retroperitoneal spaces.[18] Air can also easily pass through the cervical region due to the close proximity between the mediastinum and the upper spine which may result in pneumorrhachis, free air in the spinal canal.[19] Airflow movement through pleural structures can explain the onset of pneumothorax or even tension pneumothorax;[18] however, its occurrence is rare. If such complications arise they should be treated emergently with chest tube placement or surgical decompression.[20]
Discussion
The mediastinal cavity is defined as area demarcated by the pleural cavities laterally, the thoracic inlet superiorly and the diaphragm inferiorly.[1] PM refers to the presence of free air within the mediastinal cavity. SPM, which was initially described by Laennec in 1819, was further characterized in case series by Hamman in 1939.[10] SPM is a rare condition reported with incidence of less than 1:44,000 and often follows a benign course.[5] Though many pre-existing medical conditions have been thought to pre-dispose to the development of SPM, the pathophysiologic process is the same. It is thought that sudden changes in pressure in the thoracic cavity may precede the development of SPM due to the alveolar leakage. The pathogenesis of SPM was first proposed by Macklin in 1939, who thought that alveolar ruptures lead to air dissection along bronchovascular sheaths, which with eventual spreading of this pulmonary interstitial emphysema into the mediastinum.[21,17] The Macklin effect reported in 1944, the PM pathophysiology, is broken down into a three step process, alveolar ruptures, air dissection along bronchovascular sheaths and spreading of this pulmonary interstitial emphysema into the mediastinum.[21,17]
The Macklin effect is also involved in secondary PM such as in blunt traumatic PM, but also in PM arising in various conditions, such as respiratory distress syndromes, barotraumas, asthma crises, mechanical ventilation and valsalva maneuvers (parturition, intense vomiting and epileptic seizures).[6,7,8,11,12]
Conclusion
SPM is a rare condition that often follows a benign course and is often under diagnosed due to a clinical presentation similar to many respiratory pathologies. Due to rare but serious complications, diagnosis and expectant management are necessary. Development of SPM is often seen in young males who are smokers or patients that have a pre-existing pulmonary condition. In SPM patients, chest pain and dyspnea are the predominant symptoms often clouding the differential diagnosis. The pathognomonic sign of Hamman’s crunch is only be present in a small percentage of SPM patients, but it does not rule out the need for further investigations. In any patient, especially actively smoking young males, pulmonary patients or in patients that have a recent medical history with a high clinical suspicion, a full comprehensive radiological assessment must be performed to rule out presence of SPM due to its possible complications.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Fraser RS, Pare JA, Fraser RG, Pare PD. Synopsis of Diseases of the Chest. 2nd ed. Philadelphia, PA: WB Saunders; 1994. The normal chest; pp. 1–116. [Google Scholar]
- 2.Laënnec RT. De L’auscultation Médiate ou Traité du Diagnostic des Maladies des Poumon et du Coeur. 1st ed. Paris: Brosson & Chaudé; 1819. [Google Scholar]
- 3.Roguin A. Rene theophile hyacinthe laënnec (1781-1826): The man behind the stethoscope. Clin Med Res. 2006;4:230–5. doi: 10.3121/cmr.4.3.230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Abolnik I, Lossos IS, Breuer R. Spontaneous pneumomediastinum. A report of 25 cases. Chest. 1991;100:93–5. doi: 10.1378/chest.100.1.93. [DOI] [PubMed] [Google Scholar]
- 5.Macia I, Moya J, Ramos R, Morera R, Escobar I, Saumench J, et al. Spontaneous pneumomediastinum: 41 cases. Eur J Cardiothorac Surg. 2007;31:1110–4. doi: 10.1016/j.ejcts.2007.03.008. [DOI] [PubMed] [Google Scholar]
- 6.Caceres M, Ali SZ, Braud R, Weiman D, Garrett HE., Jr Spontaneous pneumomediastinum: A comparative study and review of the literature. Ann Thorac Surg. 2008;86:962–6. doi: 10.1016/j.athoracsur.2008.04.067. [DOI] [PubMed] [Google Scholar]
- 7.Iyer VN, Joshi AY, Ryu JH. Spontaneous pneumomediastinum: Analysis of 62 consecutive adult patients. Mayo Clin Proc. 2009;84:417–21. doi: 10.1016/S0025-6196(11)60560-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kaneki T, Kubo K, Kawashima A, Koizumi T, Sekiguchi M, Sone S. Spontaneous pneumomediastinum in 33 patients: Yield of chest computed tomography for the diagnosis of the mild type. Respiration. 2000;67:408–11. doi: 10.1159/000029539. [DOI] [PubMed] [Google Scholar]
- 9.Jougon JB, Ballester M, Delcambre F, Mac Bride T, Dromer CE, Velly JF. Assessment of spontaneous pneumomediastinum: Experience with 12 patients. Ann Thorac Surg. 2003;75:1711–4. doi: 10.1016/s0003-4975(03)00027-4. [DOI] [PubMed] [Google Scholar]
- 10.Hamman L. Spontaneous mediastinal emphysema. Bull Johns Hopkins Hosp. 1939;64:1–21. [Google Scholar]
- 11.Duffy BL. Post partum pneumomediastinum. Anaesth Intensive Care. 2004;32:117–9. doi: 10.1177/0310057X0403200120. [DOI] [PubMed] [Google Scholar]
- 12.Dechambre S, d’Odémont JP, Cornelis JP, Fastrez J. Spontaneous pneumomediastinum after sneezing. Ann Thorac Surg. 1995;60:1457. doi: 10.1016/0003-4975(95)00553-W. [DOI] [PubMed] [Google Scholar]
- 13.Koullias GJ, Korkolis DP, Wang XJ, Hammond GL. Current assessment and management of spontaneous pneumomediastinum: Experience in 24 adult patients. Eur J Cardiothorac Surg. 2004;25:852–5. doi: 10.1016/j.ejcts.2004.01.042. [DOI] [PubMed] [Google Scholar]
- 14.Moseley JE. Loculated pneumomediastinum in the newborn. A thymic “spinnaker sail” sign. Radiology. 1960;75:788–90. doi: 10.1148/75.5.788. [DOI] [PubMed] [Google Scholar]
- 15.Hammond DI. The “ring-around-the-artery” sign in pneumomediastinum. J Can Assoc Radiol. 1984;35:88–9. [PubMed] [Google Scholar]
- 16.Newcomb AE, Clarke CP. Spontaneous pneumomediastinum: A benign curiosity or a significant problem? Chest. 2005;128:3298–302. doi: 10.1378/chest.128.5.3298. [DOI] [PubMed] [Google Scholar]
- 17.Macklin MT, Macklin CC. Malignant interstitial emphysema of the lungs and mediastinum as an important occult complication in many respiratory diseases and other conditions: an interpretation of the clinical literature in the light of laboratory experiment. Medicine. 1944;23:281–358. [Google Scholar]
- 18.Steffey WR, Cohn AM. Spontaneous subcutaneous emphysema of the head, neck, and mediastinum. Arch Otolaryngol. 1974;100:32–5. doi: 10.1001/archotol.1974.00780040036007. [DOI] [PubMed] [Google Scholar]
- 19.Al-Mufarrej F, Gharagozloo F, Tempesta B, Margolis M. Spontaneous cervicothoracolumbar pneumorrhachis, pneumomediastinum and pneumoperitoneum. Clin Respir J. 2009;3:239–43. doi: 10.1111/j.1752-699X.2008.00116.x. [DOI] [PubMed] [Google Scholar]
- 20.Kirsh MM, Orvald TO. Mediastinal and subcutaneous emphysema complicating acute bronchial asthma. Chest. 1970;57:580–1. doi: 10.1378/chest.57.6.580. [DOI] [PubMed] [Google Scholar]
- 21.Macklin CC. Transport of air along sheaths of pulmonic blood vessels from alveoli to mediastinum: Clinical implications. Arch Intern Med. 1939;64:913–26. [Google Scholar]


