Dear Editor,
It is well-reported that persistent left superior vena cava (PLSVC) draining directly into the left atrium (LA), is the most common congenital thoracic venous anomaly.[1]
It results from failure of regression of the left cardinal vein.[2] In 80-90% of the reported cases, PLSVC drains into the right atrium (RA), through a coronary sinus. In remaining 10% of cases, it connects to the LA and can be associated with hemodynamic instability, syncope, systemic emboli and abscesses.[3,4] Patients with PLSVC are usually asymptomatic, but due to its anatomical defect, difficulties for establishing central venous access, pacemaker implantation and cardiothoracic surgery are common.[5] Contrast echocardiography remains the cornerstone diagnostics of PLSVC.[6,7] The risk of adverse effects associated with contrast echocardiogram including transient ischemic attack or stroke remains extremely low.[8] Transthoracic echocardiogram (TTE), in general is safer than transesophageal echocardiogram (TEE) because there is no risk of the sedatives, esophageal perforation and aspiration in the former.[9] To the best of our knowledge, there are very few reported cases, which gives the importance of injecting microbubble contrast specifically into the left arm for establishing the diagnosis of PLSVC by echocardiogram.[10,11] We herein, report another case of PLSVC draining directly into the LA, diagnosed by bubble echocardiogram when the contrast was injected in the left cubital vein and escaped initial detection after injecting into the right cubital vein. Our case taken in conjunction with the reported ones suggests the proper technique of establishing the diagnosis of Persistent Left Superior Vena Cava to identify the rare cause of stroke.
A 23-year-old male patient with a history of a known patent foramen ovale (PFO) and an old left parietal lobe abscess, presented with a syncopal episode that occurred shortly after receiving agitated saline contrast in an out-patient echo lab. The syncopal episode was likely due to cerebral vascular insufficiency due to the massive amount of micro bubbles entering the cerebral circulation. Two years previously, during the evaluation of his brain abscess, TEE was carried out, when microbubble contrast was injected in the right arm, which revealed a left-to-right shunt representing the diagnosis of PFO and a conservative approach was recommended. The precise cause of the brain abscess could not be determined, but it was felt to be possibly related to the PFO. One week before the presentation, he started having complaints of shortness of breath on exertion. A repeat TTE with bubble study was performed to evaluate the status of the PFO and to exclude other cardiac causes of dyspnea. The intravenous contrast for this study was started in the left arm and shortly after the microbubble contrast injection was given; the patient complained of feeling lightheaded, then collapsed to the ground and was unresponsive for a few minutes. He denied any fever, chills, blurred or double vision. His vital signs and physical examination were unremarkable with the cranial nerves intact and no focal motor or sensory changes. Laboratory diagnostics were unremarkable. TTE with agitated saline injected intravenously through his left arm showed a normal coronary sinus with a large bolus of bubbles entering into the LA first and then subsequently the RA [Figure 1a]. These findings were consistent with a venous connection to the LA or left pulmonary veins, most likely showing PSLVC draining into the LA. On his previous echocardiogram, the microbubbles entered into the RA when intravenous agitated saline was injected in the right arm [Figure 1b]. The finding was confirmed by left upper extremity venous angiogram that showed left superior vena cava (LSVC) with direct communication to the LA and collateral branch from the LSVC, which communicates with the normal right superior vena cava [Figure 2].
Figure 1.
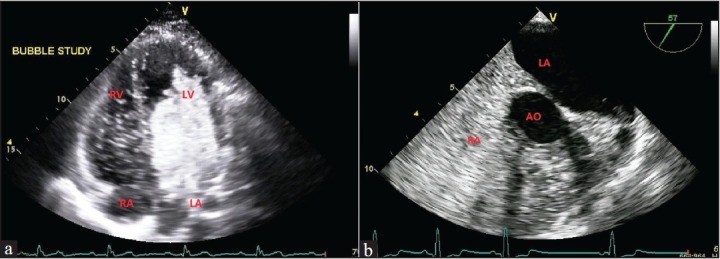
(a) Transthoracic echocardiogram bubble study with agitated saline injected intravenously through the left arm showing a large bolus of bubbles entering into the left atrium (LA). (b) Transesophageal echocardiogram bubble study with agitated saline injected intravenously through the right arm revealed complete opacification of the LA with bubbles in the right atrium. Abbreviations; Right ventricle (RV), Left ventricle (LV), Aorta (AO)
Figure 2.
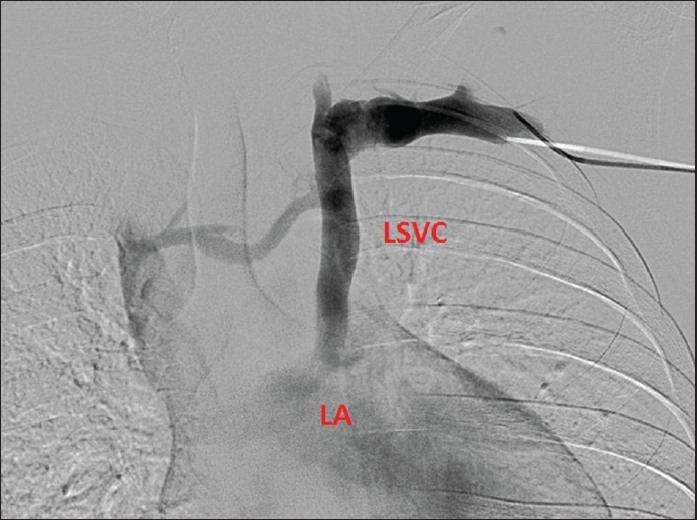
Left upper extremity venous angiogram showing left superior vena cava (LSVC) with direct communication to the left atrium and a collateral branch (bridging innominate vein) from the LSVC, which communicates with the normal right superior vena cava
PLSVC was treated with percutaneous transcatheter closure with an 18 mm Amplatzer vascular plug, near to the junction of PLSVC and LA. Subsequently, PFO was closed with a 25 mm cribriform device. The purpose of closure of PLSVC and PFO is prevention of further embolism. Hence, we suggest that echocardiogram with agitated saline injected intravenously through the left arm is important in the diagnosis of a case of PLSVC draining directly into the LA.
References
- 1.Povoski SP, Khabiri H. Persistent left superior vena cava: Review of the literature, clinical implications, and relevance of alterations in thoracic central venous anatomy as pertaining to the general principles of central venous access device placement and venography in cancer patients. World J Surg Oncol. 2011;9:173. doi: 10.1186/1477-7819-9-173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Erdoğan M, Karakaş P, Uygur F, Meşe B, Yamak B, Bozkir MG. Persistent left superior vena cava: The anatomical and surgical importance. West Indian Med J. 2007;56:72–6. doi: 10.1590/s0043-31442007000100013. [DOI] [PubMed] [Google Scholar]
- 3.Ansari RS, Domfu FM. Brain abscess with persistent left superior vena cava. Neurosciences (Riyadh) 2009;14:379–81. [PubMed] [Google Scholar]
- 4.Goyal SK, Punnam SR, Verma G, Ruberg FL. Persistent left superior vena cava: A case report and review of literature. Cardiovasc Ultrasound. 2008;6:50. doi: 10.1186/1476-7120-6-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Duymus M, Yesilkaya Y, Orman G, Bozkurt A, Yilmaz O. Persistent left superior vena cava draining to the left atrium: A case report and review of the literature. Pol J Radiol. 2012;77:65–6. doi: 10.12659/pjr.883632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Vercruysse J, François K, De Wolf A, Herregods S, Bouchez S. Persistent left superior vena cava (PLSVC) connected to the left atrium. Acta Anaesthesiol Belg. 2010;61:39–41. [PubMed] [Google Scholar]
- 7.Lentini S, Recupero A. Recognition of persistent left superior vena cava in non-congenital patients undergoing cardiac surgery. Perfusion. 2011;26:347–50. doi: 10.1177/0267659111408378. [DOI] [PubMed] [Google Scholar]
- 8.Bommer WJ, Shah PM, Allen H, Meltzer R, Kisslo J. The safety of contrast echocardiography: Report of the committee on contrast echocardiography for the American society of echocardiography. J Am Coll Cardiol. 1984;3:6–13. doi: 10.1016/s0735-1097(84)80423-4. [DOI] [PubMed] [Google Scholar]
- 9.Ramadan AS, Stefanidis C, Ngatchou W, LeMoine O, De Canniere D, Jansens JL. Esophageal stents for iatrogenic esophageal perforations during cardiac surgery. Ann Thorac Surg. 2007;84:1034–6. doi: 10.1016/j.athoracsur.2007.04.047. [DOI] [PubMed] [Google Scholar]
- 10.Thaiyananthan NN, Jacono FJ, 3rd, Patel SR, Kern JA, Stoller JK. Right-to-left anatomic shunt associated with a persistent left superior vena cava: The importance of injection site in demonstrating the shunt. Chest. 2009;136:617–20. doi: 10.1378/chest.08-2641. [DOI] [PubMed] [Google Scholar]
- 11.Hutyra M, Skala T, Sanak D, Novotny J, Köcher M, Taborsky M. Persistent left superior vena cava connected through the left upper pulmonary vein to the left atrium: An unusual pathway for paradoxical embolization and a rare cause of recurrent transient ischaemic attack. Eur J Echocardiogr. 2010;11:E35. doi: 10.1093/ejechocard/jeq079. [DOI] [PubMed] [Google Scholar]


