Abstract
Background
While communicable diseases are the leading causes of morbidity and mortality in Malawi, the contribution of nosocomial or hospital-acquired infections (HAIs) is unknown but could be substantial. The single most important method of preventing nosocomial infections is hand hygiene. We report a study which was conducted in 2011 to investigate adherence to hand hygiene protocols by clinicians and medical students working at Queen Elizabeth Central Hospital in Blantyre, Malawi.
Methods
There were two parts to the study: a single blinded arm in which participants were observed without their knowledge by trained nurses; and a second arm which included self-completion of questionnaire after participant consent was obtained. The 2009 World Health Organization hand hygiene technique and recommendations which were adopted by Queen Elizabeth Central Hospital were used to define an opportunity for hand washing and effectiveness of hand washing. Hand hygiene effectiveness was defined as adherence to at least 6 out of 7 steps (80%) of the hand hygiene technique when using alcohol-based formulation or at least 8 out of 10 steps (80%) of the hand hygiene technique when using water and soap formulation before and after having direct contact with patients or their immediate surroundings.
Results
Clinicians were found to have disinfected their hands more than medical students (p<0.05) but effectiveness was similar and very low between the two groups (p=0.2). No association was also found between having a personal hand sanitizer and hand hygiene practice (p=0.3). Adherence to hand hygiene was found to be 23%. Most of the participants mentioned infection transmission prevention as a reason for disinfecting their hands. Other reasons mentioned included: a routine personal hand hygiene behaviour and discomfort if not washing hands. The top three reasons why they did not disinfect hands were forgetfulness, unavailability of sanitizers and negligence.
Conclusion
Adherence to hand hygiene practice was found to be low, with forgetfulness and negligence being the major contributing factors. A hospital-wide multifaceted program aiming at clinicians and students education, adoption of alcohol based hand rubs as a primary formulation, production of colored poster reminders and encouraging role modeling of junior practitioners by senior practitioners can help improve compliance to hand hygiene.
Introduction
Nosocomial or hospital acquired infections account for an important burden to patients, carers and health facilities1–2. Melaku et al2 have reported that of 1383 obstetrics and gynecologic patients assessed at a referral hospital in North West Ethiopia, 246 (17.8%) developed hospital acquired infections. Hand hygiene is the single most important method of preventing spread of health care associated nosocomial infection3–5. Failure to comply with hand hygiene is considered the leading cause of health care-associated infections, contributes to the spread of multi-resistant organisms, and is recognized as a significant contributor to outbreaks of infection.
The concept of cleaning hands with an antiseptic agent probably emerged in the early 19th century5 and the first evidence of its superiority over plain soap and water in reducing transmission of health care-associated infection was provided by Ignaz Semmelweis in 18465,6. Formal written guidelines on hand washing practices in hospitals have been developed by the Centers for Disease Control and Prevention (CDC) and Association for Professionals in Infection Control7–10.
In Malawi, where infectious diseases are a great burden, the compliance rate of clinicians and medical students to hand hygiene is unknown. A study was conducted to investigate the adherence to hand hygiene protocols by clinicians and medical students working at Queen Elizabeth Central Hospital in 2011.
Methods
Study design
This was a single blinded observational study with a questionnaire administered cross sectional arm.
Study population
The study population included all clinicians (consultants, registrars and interns) and medical students (3rd, 4th and 5th year Bachelor of Medicine and Bachelor of Surgery students) working in the four departments at Queen Elizabeth Central Hospital in 2011.
Sample size
The study population was stratified into four departments (Medicine, Surgery, Pediatrics and Obstetrics and Gynecology) and then stratified within these departments into clinicians and students. Names of eligible participants were randomly selected from the departments. Sample size was 116 but 58 participants were observed because during the study period, some clinicians were on strike, two refused to be observed and others were on holiday.
Ethical considerations
Considering the ethical bearing that observing participants without their personal consent has, the proposal for the study firstly went through the College of Medicine Research Ethics Committee (COMREC) who approved it. Written consents were obtained from the Hospital Director and the respective Heads of the departments at the hospital. Participant's consent was obtained when filling the questionnaire not when they were being observed. This was done to avoid the Hawthorne effect where participants change behavior because they know they are being observed.
Data collection process
Every ward at the hospital had at least 4 sinks with soap on them and at least two alcohol hand rubs hanged on the wall along the corridors near patient beds. Data collection occurred in two parts. Firstly, study participants were observed without their knowledge on two ward rounds by trained Nurses who filled their hand hygiene practice on an observer's form. Secondly, each participant was then asked to fill out a participant's questionnaire after consent was obtained.
The 2009 World Health Organization hand hygiene technique and recommendations which were adopted by the hospital were used to define hand washing opportunities and measure the effectiveness of hand hygiene practice. These recommendations define effective hand sanitization as adherence to at least 6 out of 7 steps (80%) of hand hygiene technique with alcohol-based formulation or at least 8 out of 10 steps (80%) of hand hygiene technique with water and soap formulation before and after having direct contact with patients.
Data management and analysis
Quantitative data was analyzed using Microsoft excel and Epi-info 6.0. Parameters assessed include frequencies and Odds of hand disinfection. Qualitative data was coded based on their similarity and difference and then summarized into prevalence of the codes.
Results
Out of 58 participants, 17 (29.3%) were females and 41(70.7%) were males. 14 were consultants, 12 registrars, 6 interns, 12 fifth years and 14 third year students.
The clinicians group had total disinfection opportunity of 479, disinfected their hands 147 (30.7%), with only 41(27.9%) effective disinfections compared to 243, 23(9.5%) and 10 (43.5%) respectively amongst medical students. The adherence rate was found to be 23.5% with only 30% of all disinfections being effective.
An association was found to exist between the qualification of participants and hand disinfection practice (p=0.01). No association was found between qualification and effective hand hygiene (p=0.2); between having a hand sanitizer in the ward and disinfection tendency (p=0.48); between having a personal hand sanitizer and disinfection tendency (p=0.26); or between gender and hand hygiene (p=0.44). The odds for disinfecting hands were similar between male and female participants (OR=0.93).
Reasons given for practicing hand hygiene included prevention of infection transmission (15 participants), routine personal hand hygiene practice (8 participants), feel uncomfortable if they do not disinfect hands (3 participants), and motivated by the presence of a disinfectant (3 participants) to disinfect their hands.
Reasons given for not have disinfected hands included forgetfulness (9 participants), no hand sanitizer or soap (9 participants), many patients in the ward to be seen on ward rounds (8 participants), negligence (3 participants) and that the sinks and sanitizers are placed on far ends of the wards (2 participants).
Discussion
In a study of qualified clinicians and medical students in Blantyre, Malawi, clinicians were more likely to disinfect hands than medical students. This agrees with findings in previous studies elsewhere and the main reasons include more hospital experience and direct contact with patients during ward rounds on the clinicians' part than students11. Evidence suggests that role modeling by experienced physicians can greatly improve compliance to hand hygiene amongst inexperienced physicians12,13. In this regard, participant clinicians in this study may not have been role modeling students in hand hygiene behaviour since compliance in both groups was still low.
The low effectiveness levels in both groups suggest lack of knowledge of the recommended technique could be a contributing factor. Other possible factors include that there are no reminders of the actual steps of the technique in the wards, the hospital is understaffed hence those available are overwhelmed with a lot of work and easily forget to wash hands despite hand sanitizers being accessible.
Conclusion
This study demonstrates that adherence to hand hygiene practice by clinicians and medical students at Queen Elizabeth Central Hospital is low. Clinicians' disinfection tendency is more than students although effectiveness of the technique itself is similar between these groups. Forgetfulness and negligence are the major contributing factors and the problem is worsened by lack of knowledge of the recommended hand hygiene technique and understaffing at the hospital.
Recommendations
A hospital-wide multidisciplinary campaign is needed to significantly improve the compliance rate to hand hygiene practices by clinicians and medical students at Queen Elizabeth Central Hospital. This should include training practitioners, promoting alcohol based hand rubs as a primary formulation to be used at point of care, producing colored poster reminders whose messages are to be designed by the practitioners themselves to make them feel they own the campaign, surveying compliance and giving feedback to practitioners on their hand hygiene performance. Senior practitioners should also be sensitized to act as role models of excellent hand hygiene practice to junior practitioners.
Limitations
The major limitation in this study was that half the required sample size was not observed.
Figure 1.
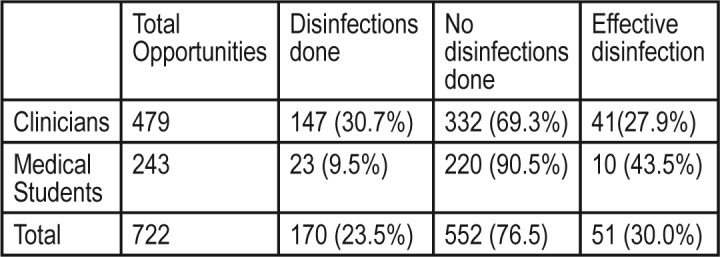
Health practitioners, number of disinfections and number of effective disinfections.
References
- 1.Pourakbari B, Rezaizadeh G, Mahmoudi S, Mamishi S. Epidemiology of nosocomial infections in pediatric patients in an Iranian referral hospital. J Prev Med Hyg. 2012;53(4):204–206. [PubMed] [Google Scholar]
- 2.Melaku S, Gebre-Selassie S, Damtie M, Alamrew K. Hospital acquired infections among surgical, gynaecology and obstetrics patients in Felege-Hiwot referral hospital, Bahir Dar, northwest Ethiopia. Ethiop Med J. 2012;50(2):135–144. [PubMed] [Google Scholar]
- 3.Camins BC, Fraser VJ. Reducing the risk of health care-associated infections by complying with CDC hand hygiene guidelines. Joint Comm J Qual Patient Saf. 2005;31(3):173–179. doi: 10.1016/s1553-7250(05)31023-3. [DOI] [PubMed] [Google Scholar]
- 4.Garner JS, Favero MS. CDC guidelines for the prevention and control of nosocomial infections. Guideline for handwashing and hospital environmental control, 1985. Supersedes guideline for hospital environmental control published in 1981. Am J Infect Control. 1986;14(3):110–129. doi: 10.1016/0196-6553(86)90019-2. [DOI] [PubMed] [Google Scholar]
- 5.Biddle C. Semmelweis revisited: hand hygiene and nosocomial disease transmission in the anesthesia workstation. Journal of the American Association of Nurse Anesthetists A. 2009;77(3):229–237. [PubMed] [Google Scholar]
- 6.Stewardson A, Allegranzi B, Sax H, Kilpatrick C, Pittet D. Back to the future: rising to the Semmelweis challenge in hand hygiene. Future Microbiol. 2011;6(8):855–876. doi: 10.2217/FMB.11.66. [DOI] [PubMed] [Google Scholar]
- 7.Guideline for hand hygiene in healthcare settings. Healthcare Infection Control Practices Advisory Committee and Hand-Hygiene Task Force; Society for Healthcare Epidemiology of America; Association for Professionals in Infection Control and Epidemiology; Infection Diseases Society of America. J Am Coll Surg. 2004;198(1):121–127. doi: 10.1016/j.jamcollsurg.2003.08.016. [DOI] [PubMed] [Google Scholar]
- 8.Guideline for Hand Hygiene in Health-Care Settings: recommendations of the Healthcare Infection Control Practices Advisory Committee and the HICPAC/SHEA/APIC/IDSA Hand Hygiene Task Force. 2002. [PubMed] [Google Scholar]
- 9.Boyce JM, Pittet D. Healthcare Infection Control Practices Advisory Committee. Society for Healthcare Epidemiology of America. Association for Professionals in Infection Control. Infectious Diseases Society of America. Hand Hygiene Task Force. Infect Control Hosp Epidemiol. 2002;23(12 Suppl):S3–S40. doi: 10.1086/503164. [DOI] [PubMed] [Google Scholar]
- 10.Boyce JM, Pittet D. Healthcare Infection Control Practices Advisory Committee; HICPAC/SHEA/APIC/IDSA Hand Hygiene Task Force. MMWR Recomm Rep. 2002;51(RR-16):1–45. [PubMed] [Google Scholar]
- 11.Joint Comm Perspect. 2. Vol. 28. CDC; WHO; 2008. CDC/WHO Hand Hygiene Guidelines crosswalk; pp. 4–7. [PubMed] [Google Scholar]
- 12.Suchitra J, Lakshmidevi N. ‘Handwashing compliance: is it a reality?’. Online Journal of Health and Allied Sciences. 2007;5:20. [Google Scholar]
- 13.Whitby M, McLaws ML, Ross MW. Why healthcare workers don't wash their hands: a behavioral explanation. Infect Control Hosp Epidemiol. 2006;27(5):484–492. doi: 10.1086/503335. Epub 2006 Apr 26. [DOI] [PubMed] [Google Scholar]


