Abstract
Background
The incidence of proximal humeral fractures lies between 105 and 342 per 100 000 persons per year. Around the world, this type of fracture remains a major challenge for treating surgeons. While non-displaced fractures can be managed conservatively, displaced ones are often treated surgically.
Methods
Selective literature review
Results
There are still no evidence-based schemes or guidelines for the treatment of proximal humeral fractures, and very few prospective randomized trials are available. The few that have been published recently show a trend in favor of conservative treatment, but they were carried out on small groups of patients and their findings are not directly generalizable. For younger patients, the goal of treatment is generally anatomical repositioning and osteosynthetic stabilization; for older patients, primary treatment with a prosthesis is a further option. Depending on the mode of treatment, complications can arise such as shoulder stiffness, necrosis of the humeral head, pain, infection, loss of reposition, and “cutting out.”
Conclusion
Current evidence supports the individualized treatment of proximal humeral fractures. Treatment decisions must always be made jointly with the patient in consideration of his or her individual needs and characteristics. Particularly for elderly patients, the possibility of conservative treatment should be carefully considered. If conservative treatment is not possible, then the type of operation performed should also be a function of the surgeon’s individual skills and experience with particular types of implant.
Proximal humeral fractures (Figure 1) are common, particularly in the elderly. Along with proximal femoral, distal radial, and vertebral-body fractures, they are a common type of osteoporotic fracture. Women are affected two to three times as often as men (1). An analysis of the Finnish trauma registry revealed that the incidence of proximal humeral fracture rose from 32 to 105 per 100 000 persons per year between 1970 and 2002, along with a rise in the average age of affected women, from 73 to 78 (2). In Hungary, health insurance data from 1999–2003 reveal an incidence of 342 per 100 000 persons per year; in emergency rooms in the USA, there were 61 consultations for proximal humeral fracture per 100 000 persons in the year 2008 (3, 4).
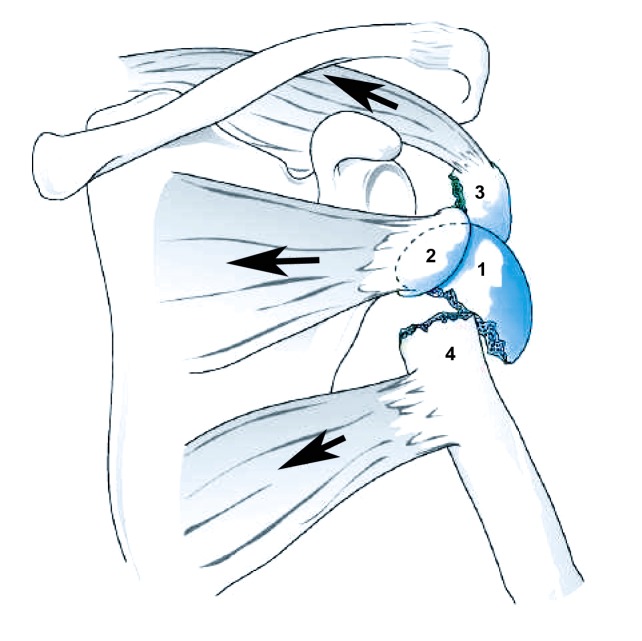
Figure 1.
Fragment displacement caused by the pull of attached rotator-cuff tendons. 1: dome of humeral head, 2: lesser tubercle; 3: greater tubercle, 4: shaft. Reprinted with the kind permssion of Georg Thieme Verlag, Stuttgart
Non-displaced proximal humeral fractures can be treated conservatively; displaced ones are often treated surgically. Osteoporosis is common in the elderly and makes surgery much harder. Because the population as a whole is aging, proximal humeral fracture is becoming an ever more prominent topic in trauma surgery. The proper choice of treatment depends on the specific characteristics of the fracture and of the patient. In this article, we selectively review the pertinent literature to survey the current treatment options for proximal humeral fracture.
History and mechanism of injury
In younger patients, proximal humeral fractures are usually caused by high-energy trauma, such as traffic accidents or sporting accidents. In older patients, the most common cause is a fall onto the outstretched arm from a standing position, which is a type of low-energy trauma (2, 5).
Clinical examination and diagnostic evaluation
Typically, the patient holds the injured arm in a protective posture close to the chest. Pain, swelling, hematoma, and tenderness of the proximal portion of the humerus may indicate the presence of a fracture. The perfusion and sensorimotor function of the limb should be tested in the periphery. The functioning of the axillary nerve should be tested as well.
Ideally, the standard x-ray assessment includes a so-called trauma series with a true anteroposterior view, a scapular Y view, and an axial view. In the acute situation, however, the axial view is often unobtainable because of pain. Particularly for complex fracture types, computed tomography (CT) may yield important additional information about the size and position of the individual fragments and about potentially accompanying bony injuries, e.g., of the glenoid or coracoid process.
Fracture classification
The Neer classification is the one most frequently used in routine clinical situations. Neer modified the Codman four-fragment theory by taking account of the degree of displacement and by adding luxation and head-split fractures. He classified non-displaced fractures as “one-part fractures,” because they can be considered a stable unit and can thus be treated conservatively. Neer defined the threshold values distinguishing mildly displaced from displaced fractures as 1 cm of displacement and/or 45% of angulation. Displaced fractures are classified as two-fragment, three-fragment, or four-fragment fractures. Anterior and posterior luxation fractures and head-split fractures are classified as separate entities (6). The Neer classification has two main disadvantages: It does not account for all possible fracture morphologies, nor does it enable prognosis of necrosis of the humeral head.
Treatment
There are still no evidence-based schemes or guidelines for the treatment of proximal humeral fractures. Although proximal humeral fracture is among the more common types of fracture, very few randomized trials of its treatment have been published. The wide variety of fracture morphologies and treatment options, ranging from conservative treatment to various osteosynthetic methods to the implantation of an endoprosthesis, makes such trials difficult to initiate. There are no standardized and generally accepted threshold values, and the trials that have been performed at various centers are poorly comparable with one another because of the different criteria that they employed. The conclusion of a recent Cochrane review was that no evidence-based recommendations on the treatment of proximal humerus fracture can be derived from the currently available data (7).
In younger patients, non-displaced or mildly displaced fractures are treated conservatively, while the treatment of choice for displaced proximal humerus fractures is anatomical reconstruction and osteosynthesis. In the elderly, the implantation of a prosthesis may need to be considered in order to restore painless, robust function of the humerus, and thus personal independence, as rapidly as possible.
It is problematic for the recommendation of any specific treatment that the threshold values posited by Neer to distinguish displaced from non-displaced fractures are not based on clinical or biomechanical data; rather, they are theoretical constructs (8). Although Neer’s values were long used as the standard for clinical decision-making, recent improvements in osteosynthetic techniques—above all, the development of fixed angle implants—have encouraged a trend toward operative treatment. Mildly displaced fractures are now considered an indication for surgery more commonly than before. Although it is often stated in the literature that 60% to 80% of non-displaced or mildly displaced fractures can be treated conservatively (9), certainly most such fractures are now treated surgically, and the threshold values for a surgical indication are now being set lower than in the past (10). Lill, for example, defines as displaced any fracture with a fragment displacement of 5 mm, an axial deviation of 20°, or a tubercle displacement of 2 mm (11). There is, however, still no consensus on these values. The particular treatment to be used should, therefore, be chosen individually with consideration of the patient’s biological age and bone quality, accompanying illnesses, compliance, and personal wishes.
Conservative treatment
It is universally recognized that non-displaced fractures can be treated conservatively. In these fractures, the surrounding soft tissues are generally intact, and the periosteum, rotator cuff, and joint capsule serve to stabilize the fracture. Valgus impacted fractures are also a good indication for conservative treatment. For mildly displaced fractures, the treatment decision must be made jointly with the patient in view of the accompanying circumstances. The threshold values of Neer (<1 cm, <45°) are generally used for clinical decision-making in elderly patients, and those of Lill (<0.5 cm, <20°, <0.2 cm tubercle displacement) for younger patients (Figure 2) (Table).
Figure 1.

a) A 61-year-old man with a mildly displaced four-fragment fracture
b) Conservative treatment resulted in successful consolidation in an acceptable position
Table. Conservative treatment of proximal humeral fractures.
| Week | Treatment |
|---|---|
| 1st | Gilchrist arm sling, elbow and hand exercises |
| 2nd – 3rd | Pendulum exercises |
| 4th – 6th | Active assisted physiotherapy to 90º abduction and anteversion |
| 7th onward | Free mobilization |
The conservative treatment of non-displaced or mildly displaced fractures generally yields good results. With adequate pain relief, shoulder mobility will generally reach about 85% of that on the opposite side.
The main complications are restriction of movement, necrosis of the head of the humerus, pain, subacromial impingement by a displaced greater tubercle, and the formation of a pseudarthrosis.
Surgical treatment
Fractures that do not meet the above criteria for conservative treatment should be treated surgically. Further indications for surgery include metaphyseal comminution, dislocated fractures, open fractures, head-split and anatomical neck fractures, and injuries to the neighboring blood vessels and nerves. In principle, a decision must be made whether to use a head-preserving or a head-replacing technique.
Osteosynthesis—Whatever type of implant is chosen, the goal of surgical reconstruction is always the anatomical reposition and stable fixation of the fracture. Displaced fractures of the greater and lesser tubercles are repositioned and stabilized with two small-fragment traction screws as long as the bone is of good enough quality and the fragments are of adequate size. If the fragment is too small, or when there are multiple fragments, refixation is achieved with cerclage or with suture anchors.
Fractures of the surgical neck of the humerus include the typical subcapital humeral fracture (a two-fragment fracture) as well as most three-fragment and all four-fragment fractures. Many different options for osteosynthesis have been described. The most common ones are percutaneous K-wire osteosynthesis, plate osteosynthesis, and nail osteosynthesis.
Percutaneous K-wire osteosynthesis is mainly suitable for fractures without metaphyseal comminution. This method is technically demanding and can be performed only if closed reduction is possible. Because the approach is minimally invasive, the perfusion of the humeral head is not compromised. The disadvantages of percutaneous K-wire osteosynthesis include lesser stability and wire-related complications such as migration, infection, and joint perforation. Good clinical results can be obtained in experienced hands with strict patient selection (12).
Open reduction enables better manipulation of the fracture fragments and is therefore suitable for the treatment of any type of fracture with plate osteosynthesis. The manipulation of the fragments does, however, worsen their perfusion. Early functional therapy should be enabled in order to prevent shoulder stiffness. The introduction of fixed angle implants has led to a marked improvement of surgical treatment and to a clear trend away from conservative treatment and toward osteosynthesis. Osteosynthesis with a fixed angle implant is now the most commonly performed procedure (Figure 3). This method has markedly improved the stability of osteosynthesis (13). Although the approach works very well in younger patients, the care of osteoporotic fractures remains problematic. Even fixed angle implants are often not well anchored in osteoporotic bone, so that the goal of adequate stability to enable early physiotherapy may not be met. Indeed, in osteoporotic fractures, a fixed angle plate osteosynthesis is often too stable: The osteoporotic humeral head collapses while the fixed angle screws remain in place. The result is called “cutting out,” a situation in which the screws perforate the joint. Early in the history of fixed angle plate osteosynthesis, its complication rate was found to be ca. 25%; this figure was confirmed in the prospective multicenter trial of Südkamp et al. (14). 62 complications were registered in 52 (34%) of 155 patients. 40% of the complications were attributable to problems of surgical technique, most commonly intraoperative perforation of the humeral head by a screw. Further complications included plate fracture (1.9%), impingement (2.6%), pseudarthrosis (2.6%), wound infection (3.9%), loss of reposition (7.1%), and necrosis of the humeral head (3.9%) (14).
Figure 3.

a) This 52-year-old man fell and sustained a three-fragment proximal humeral fracture with valgus impaction.
b) Treatment with open reposition and a fixed angle plate
Nail osteosynthesis is performed to combine the high stability of rigid implants with the soft-tissue preservation of minimally invasive techniques. Nailing is indicated in cases with marked metaphyseal comminution or spiral fractures extending into the humeral shaft. Recent trials comparing various types of modern fixed angle plate or nail with each other, or fixed angle plates with nails, did not reveal any clinical differences (15, 16).
The often mediocre functional results and high complication rates of surgery for proximal humeral fractures in the elderly have fueled a debate in the current literature as to whether osteosynthesis offers elderly patients any advantage over conservative treatment. The first comparative trials in this area were published recently, including some small-scale randomized controlled trials. None of them showed surgery to be better than conservative treatment. Sanders et al. carried out a matched pairs analysis of 18 patients treated with fixed angle plate osteosynthesis and 18 conservatively treated patients: The latter group had better clinical results and fewer complications (17). Similar findings were obtained by Fjalestad et al. in a matched pairs analysis in 2005 and then in a prospective randomized trial in 2012 (18, 19). In another randomized trial, Olerud et al. found a trend toward better functional results in the patients who had been treated surgically with a fixed angle plate (20), but at the cost of a higher complication rate: 30% of the patients in the surgical group had a complication requiring operative revision, compared to none in the conservatively treated group.
These recent prospective trials included only small numbers of patients, and their findings therefore do not have a direct, unlimited application in clinical practice. These trials reveal possible trends and offer food for thought, but they should not be misconstrued as being more definitive than they are.
The removal of fixed angle implants must be regarded critically because of the high likelihood of complications, ranging to secondary necrosis of the humeral head. Elderly patients, in particular, should be advised not to have their implants removed unless they suffer from implant-specific symptoms or an arthrolysis needs to be performed.
Endoprostheses—Despite the availability of modern fixed angle plate and nail systems, many proximal humeral fractures cannot be adequately reconstructed. Current evidence implies that three- and four-fragment fractures of the proximal humerus should be treated with a prosthesis if the dome fragment is itself fragmented or hollow because of a loss of spongiosa, if the patient has advanced osteoporosis, or if prior osteosynthesis has failed and there is no prospect of operative revision with preservation of the humeral head (Figure 4).
Figure 4.

After implantation of a fracture prosthesis, the tubercles were resorbed, with resulting proximalization of the prosthesis. The necessary conversion to an inverse prosthesis was performed with a modular prosthesis system so that the shaft did not have to be replaced
When a proximal humeral fracture is treated with a fracture prosthesis, the decisive factors for a good result are healing and correct positioning of the tubercles, restoration of the correct height of the humeral head, and correct reconstruction of both lateral offset and retroversion. Successive developments in the design of fracture prostheses have enabled these requirements to be ever more closely met.
Yet, despite these developments, a consideration of our own results together with those published in the literature reveals that the function of the shoulder joint after the endoprosthetic treatment of a fracture is often disappointingly poor, far worse than is generally seen after prosthesis implantation for omarthrosis. Patients whose fractures are treated with prostheses generally do not have much pain (21, 22).
Many elderly patients already have a rotator-cuff lesion before they sustain a proximal humeral fracture. Ultrasonographic studies suggest that 28% of persons at age 60, 50% of persons at age 70, and 80% of persons at age 80 have a rotator-cuff tear (23). Such patients often have worse results after treatment with a fracture prosthesis. Inverse prostheses, because of their special design, are particularly suitable for patients with a clinically relevant lesion of the rotator cuff.
Intact deltoid function is required for an inverse prosthesis to achieve a good clinical result, and therefore the functionality of the axillary nerve must be checked preoperatively. The literature still contains little data on this mode of fracture treatment. It has been reported that the treatment of proximal humerus fractures with an inverse prosthesis tends to result in a limited range of motion (24), comparable to that seen with conventional fracture prostheses. The current state of the evidence suggests that inverse fracture prostheses are an option for the treatment of non-reconstructible proximal humeral fractures in patients over age 65 with non-reconstructible defects of the rotator cuff. A critical point, however, is that options for surgical reversal are very limited after unsuccessful treatment with an inverse prosthesis, and reports of long-term results are lacking. In view of the high potential for complications and the lack of opportunity for reversal, inverse endoprostheses should only be implanted by surgeons with specific experience in this technique.
Overview
The currently available evidence cannot be used to derive any standardized, evidence-based treatment scheme for proximal humeral fractures. The introduction of fixed angle osteosynthesis has led to an extension of the indications for osteosynthesis. With the aid of these modern implants, proximal humeral fractures in younger patients can generally be treated in such a way as to make them stable for early physiotherapy; for older patients, however, the treatment remains problematic. Alternative methods such as conservative treatment or the implantation of endoprostheses are now under discussion. Even though initial randomized trials showed conservative treatment to be superior to osteosynthesis for elderly patients, one must bear in mind that these trials were carried out on small, heterogeneous groups of patients with short follow-up intervals, and they did not include all treatment options. Thus, their findings cannot be generalized, but they do show that conservative therapy is, at least, a treatment option that deserves consideration. It would be incorrect to conclude that every elderly person with a proximal humeral fracture should be treated conservatively, but the trials clearly show that not every fracture needs to be operated on. Especially in elderly patients—including those with three- and four-fragment fractures—the Neer threshold values for displacements should be respected, if possible: If the patient’s fracture is stable, in the sense of being a “one-part fracture” as defined by Neer, it may be treated conservatively, at least as an initial attempt.
The decision how to treat a proximal humeral fracture must always be made by an experienced trauma surgeon jointly with the patient, and should take account of the patient’s individual needs and characteristics, such as his or her biological age, accompanying illnesses, bone quality, and fracture morphology. In particular, the decision whether to operate on a fracture or treat it conservatively requires a detailed assessment of fracture morphology and stability as well as extensive experience in the treatment of proximal humeral fractures, so that the patient can be adequately informed of the advantages and disadvantages of the various treatment options and the prognosis associated with each.
Key Messages.
Although humeral fracture is one of the more common types of fracture, there have been very few randomized controlled trials (RCTs) of its treatment.
The few RCTs performed to date have shown a trend in favor of conservative treatment, but the patient groups were small and heterogeneous, and the findings of these trials cannot be directly applied in clinical practice.
Non-displaced or mildly displaced fractures can be treated conservatively.
In younger patients, the goals of treatment are anatomical reposition and the osteosynthetic stabilization of displaced fractures. In elderly patients, primary treatment with a prosthesis may also be reasonable, depending on the severity of injury.
Depending on the type of treatment, potential complications include shoulder stiffness, necrosis of the humeral head, pain, infection, loss of reposition, and “cutting out.”
Acknowledgments
Translated from the original German by Ethan Taub, M.D.
Footnotes
Conflict of interest statement
PD Dr. Burkhart has received reimbursement of travel expenses and congress participation fees from Tornier and Stryker. He and Prof. Müller led a workshop on shoulder endoprostheses that was sponsored by Tornier. PD Dr. Dietz has received lecture honoraria and reimbursement of travel expenses from Axomed, payment for carrying out clinical trials on behalf of Synthes and Tantum AG, and research funding from Synthes, Mathys AG, and Tantum AG. Prof. Bastian has received reimbursement of travel expenses from Medartis and lecture honoraria and congress participation fees from the AO Foundation, Germany. Prof. Müller has received reimbursement of travel expenses from Tornier, Stryker, Synthes, and Medartis and lecture honoraria from Synthes. Prof. Hoffmann and Dr. Thelen state that they have no conflict of interest.
References
- 1.Court-Brown CM, Garg A, McQueen MM. The epidemiology of proximal humeral fractures. Acta Orthop Scand. 2001;72:365–371. doi: 10.1080/000164701753542023. [DOI] [PubMed] [Google Scholar]
- 2.Palvanen M, Kannus P, Niemi S, Parkkari J. Update in the epidemiology of proximal humeral fractures. Clin Orthop Relat Res. 2006;442:87–92. doi: 10.1097/01.blo.0000194672.79634.78. [DOI] [PubMed] [Google Scholar]
- 3.Kim SH, Szabo RM, Marder RA. Epidemiology of humerus fractures in the United States: nationwide emergency department sample, 2008. Arthritis Care Res. 2012;64:407–414. doi: 10.1002/acr.21563. [DOI] [PubMed] [Google Scholar]
- 4.Pentek M, et al. Epidemiology of osteoporosis related fractures in Hungary from the nationwide health insurance database, 1999-2003. Osteoporos Int. 2008;19:243–249. doi: 10.1007/s00198-007-0453-6. [DOI] [PubMed] [Google Scholar]
- 5.Lind T, Kroner K, Jensen J. The epidemiology of fractures of the proximal humerus. Arch Orthop Trauma Surg. 1989;108:285–287. doi: 10.1007/BF00932316. [DOI] [PubMed] [Google Scholar]
- 6.Neer CS., 2nd Displaced proximal humeral fractures. I. Classification and evaluation. J Bone Joint Surg Am. 1970;52:1077–1089. [PubMed] [Google Scholar]
- 7.Handoll HH, Ollivere BJ. Interventions for treating proximal humeral fractures in adults. Cochrane Database Syst Rev. 2010 doi: 10.1002/14651858.CD000434.pub2. CD000434. [DOI] [PubMed] [Google Scholar]
- 8.Hertel R. Fractures of the proximal humerus in osteoporotic bone. Osteoporos Int. 2005;16(Suppl 2):65–72. doi: 10.1007/s00198-004-1714-2. [DOI] [PubMed] [Google Scholar]
- 9.Gaebler C, McQueen MM, Court-Brown CM. Minimally displaced proximal humeral fractures: epidemiology and outcome in 507 cases. Acta Orthop Scand. 2003;74:580–585. doi: 10.1080/00016470310017992. [DOI] [PubMed] [Google Scholar]
- 10.Bell JE, et al. Trends and variation in incidence, surgical treatment, and repeat surgery of proximal humeral fractures in the elderly. J Bone Joint Surg Am. 2011;93:121–131. doi: 10.2106/JBJS.I.01505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lill H, Voigt C. Proximal humeral fracture. Z Orthop Unfall. 2010;148:353–360. [PubMed] [Google Scholar]
- 12.Bogner R, et al. Minimally-invasive treatment of three- and four-part fractures of the proximal humerus in elderly patients. J Bone Joint Surg Br. 2008;90:1602–1607. doi: 10.1302/0301-620X.90B12.20269. [DOI] [PubMed] [Google Scholar]
- 13.Seide K, et al. Locked vs. unlocked plate osteosynthesis of the proximal humerus - a biomechanical study. Clin Biomech. 2007;22:176–182. doi: 10.1016/j.clinbiomech.2006.08.009. [DOI] [PubMed] [Google Scholar]
- 14.Sudkamp N, et al. Open reduction and internal fixation of proximal humeral fractures with use of the locking proximal humerus plate. Results of a prospective, multicenter, observational study. J Bone Joint Surg Am. 2009;91:1320–1328. doi: 10.2106/JBJS.H.00006. [DOI] [PubMed] [Google Scholar]
- 15.Gradl G, Dietze A, Kaab M, Hopfenmuller W, Mittlmeier T. Is locking nailing of humeral head fractures superior to locking plate fixation? Clin Orthop Relat Res. 2009;467:2986–2993. doi: 10.1007/s11999-009-0916-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kuhlmann T, et al. Operative treatment of proximal humeral four-part fractures in elderly patients: comparison of two angular-stable implant systems. Z Orthop Unfall. 2011 doi: 10.1055/s-0031-1280365. [DOI] [PubMed] [Google Scholar]
- 17.Sanders RJ, Thissen LG, Teepen JC, van Kampen A, Jaarsma RL. Locking plate versus nonsurgical treatment for proximal humeral fractures: better midterm outcome with nonsurgical treatment. J Shoulder Elbow Surg. 2011;20:1118–1124. doi: 10.1016/j.jse.2011.01.025. [DOI] [PubMed] [Google Scholar]
- 18.Fjalestad T, Stromsoe K, Blucher J, Tennoe B. Fractures in the proximal humerus: functional outcome and evaluation of 70 patients treated in hospital. Arch Orthop Trauma Surg. 2005;125:310–316. doi: 10.1007/s00402-005-0803-9. [DOI] [PubMed] [Google Scholar]
- 19.Fjalestad T, Hole MO, Hovden IA, Blucher J, Stromsoe K. Surgical treatment with an angular stable plate for complex displaced proximal humeral fractures in elderly patients: a randomized controlled trial. J Orthop Trauma. 2012;26:98–106. doi: 10.1097/BOT.0b013e31821c2e15. [DOI] [PubMed] [Google Scholar]
- 20.Olerud P, Ahrengart L, Ponzer S, Saving J, Tidermark J. Internal fixation versus nonoperative treatment of displaced 3-part proximal humeral fractures in elderly patients: a randomized controlled trial. J Shoulder Elbow Surg. 2011;20:747–755. doi: 10.1016/j.jse.2010.12.018. [DOI] [PubMed] [Google Scholar]
- 21.Besch L, et al. Hemiarthroplasty of the shoulder after four-part fracture of the humeral head: a long-term analysis of 34 cases. J Trauma. 2009;66:211–214. doi: 10.1097/TA.0b013e31815d9649. [DOI] [PubMed] [Google Scholar]
- 22.Kralinger F, et al. Outcome after primary hemiarthroplasty for fracture of the head of the humerus. A retrospective multicentre study of 167 patients. J Bone Joint Surg Br. 2004;86:217–219. doi: 10.1302/0301-620x.86b2.14553. [DOI] [PubMed] [Google Scholar]
- 23.Milgrom C, Schaffler M, Gilbert S, van Holsbeeck M. Rotator-cuff changes in asymptomatic adults. The effect of age, hand dominance and gender. J Bone Joint Surg Br. 1995;77:296–298. [PubMed] [Google Scholar]
- 24.Bufquin T, Hersan A, Hubert L, Massin P. Reverse shoulder arthroplasty for the treatment of three- and four-part fractures of the proximal humerus in the elderly: a prospective review of 43 cases with a short-term follow-up. J Bone Joint Surg Br. 2007;89:516–520. doi: 10.1302/0301-620X.89B4.18435. [DOI] [PubMed] [Google Scholar]