Abstract
In general, social support from family members affects chronic illness outcomes, but evidence on which specific family behaviors are most important to adult patient outcomes has not been summarized. We systematically reviewed studies examining the effect of specific family member behaviors and communication patterns on adult chronic illness self-management and clinical outcomes. Thirty studies meeting inclusion criteria were identified, representing 22 participant cohorts, and including adults with arthritis, chronic cardiovascular disease, diabetes, and/or end stage renal disease. Family emphasis on self-reliance and personal achievement, family cohesion, and attentive responses to symptoms were associated with better patient outcomes. Critical, overprotective, controlling, and distracting family responses to illness management were associated with negative patient outcomes. Study limitations included cross-sectional designs (11 cohorts), however results from longitudinal studies were similar. Findings suggest that future interventions aiming to improve chronic illness outcomes should emphasize increased family use of attentive coping techniques and family support for the patient’s autonomous motivation.
Keywords: Family Relations, Social Support, Chronic Disease, Self-Care, Outcomes
Introduction
Social support can significantly affect adults’ health and health outcomes (House et al. 1988; Tomaka et al. 2006; Uchino 2004). For adults actively managing chronic illnesses like diabetes, heart disease, and lung disease, social support is particularly critical (Fisher et al. 1998; Krol et al. 1993; Lett et al. 2005; Marino et al. 2008; Patel et al. 2005; Westlake et al. 2002). In chronic illness, higher social support, most commonly measured as the amount of practical and emotional support that patients perceive, has been linked with improved self-management behavior (DiMatteo 2004; Gallant 2003), improved disease control (Griffith et al. 1990), and lower mortality risk (Friedmann et al. 2006; Holder 1997; Murberg and Bru, 2001; Rutledge et al. 2004; Zhang et al. 2007). However, for practitioners advising patients with chronic illness and their families, the patient’s perception of support from family is only one piece of the puzzle. A patient’s perception of social support reflects specific behaviors of family members, behaviors that can have positive or negative effects on the perception of support and on the success of chronic illness management (Franks et al. 1992). Knowing which specific family behaviors are linked with better or worse chronic illness management could help practitioners better understand specific ways families can increase their effective support.
Family behaviors are particularly important in chronic illnesses that require ongoing, active self-management. The management of chronic illnesses often involves changes in daily routines that occur in family settings, such as changes in eating patterns, physical activity, and regular self-testing (i.e. of blood glucose, blood pressure, or respiratory peak flows). The ongoing (often for life) and frequent (often daily) nature of these disease-related routines requires family adaptation, and patients’ success at maintaining these routines could greatly benefit from effective family encouragement. Moreover, family members often take an active role in helping adults with chronic illness execute complex self-management tasks, make disease-related decisions, and cope with disease-related stress (Connell 1991; Friedman 1993; Gleeson-Kreig et al. 2002; Silliman et al. 1996). These behavioral patterns evolve over time and can last many decades.
Behavioral theory points to several specific family behaviors that could be particularly influential in chronic illness management. Family systems theory (Lutz et al. 2009) describes the complex and emotional interconnectedness of family members, emphasizing the general importance of marital satisfaction and positive family function to individual function. Family systems theory also emphasizes ways that a family’s level of interconnectedness might influence their approach to illness management, such as framing talk about illness management as an individual issue versus a group issue. Social interdependence theory (Rusbult and Van Lange, 2003) describes how individual achievement is affected by the actions of family members, such that family cohesion and family orientation towards shared goals could influence the patient’s success at illness management. Self-determination theory (Ryan and Deci, 2000) addresses ways in which family behaviors increase a patient’s autonomous motivation and sense of competence (Williams et al. 1998), which in turn can affect self-management success. Such family behaviors include encouraging patient autonomy in illness-related decisions, avoiding direct criticism of the patient’s illness management, and family use of social control to affect patient health behaviors (Umberson 1987). Coping theory (Lazarus and Folkman, 1984) highlights ways that family members might help or hinder patient coping with disease-related symptoms or stress, including efforts to distract the patient, or conversely, directly confronting and discussing illness management issues with the patient. Finally, family behaviors originally observed among patients with chronic mental illness could also affect patients with other chronic illnesses. One prominent example is expressed emotion (Wearden et al. 2000), which measures family members’ hostility towards, criticism of, and “emotional over involvement” in the patient’s management of illness, and has been linked to worse schizophrenia control and relapse (Leff and Vaughn, 1985).
Our goals in this review were to: describe which specific family behaviors have been studied in the context of adult chronic illness self-management and outcomes, examine which family behaviors are associated with better or worse chronic illness self-management and outcomes, and appraise whether the pattern of linkages found between family behaviors and chronic illness outcomes is consistent with relevant behavioral theories. Past reviews of the impacts of specific family behaviors on chronic illness have shed some light on these questions, but have focused on different populations or outcomes. For example, Fisher and colleagues, in two narrative reviews of family relationships in chronic illness (Fisher et al. 1998; Fisher and Weihs, 2000), included studies with chronically ill adolescents, whose interactions with family members can differ markedly from those of middle-aged or older adults. In addition, Fisher’s reviews were published before 18 of the articles included in this current review were available. A meta-analysis of family-oriented psychosocial interventions in chronic illness by Martire and colleagues (2004) included studies that did not focus on specific family behaviors, and many studies with patients with dementia or frailty (two conditions for which family support tends to focus more on direct instrumental help with tasks than encouragement of self-management). Furthermore, many of the studies in Martire’s review did not have illness management or control outcomes, but rather relationship outcomes such as marital satisfaction. Finally, a recent review of the effects of couples’ coping strategies (Berg and Upchurch, 2007) on adult health conditions included some studies with participants who did not have chronic illness, and included studies with non-patient specific outcomes such as relationship quality and spouse quality of life.
In this review, we summarize the literature on the associations between family behaviors and patient outcomes of mortality, illness control or symptoms, disease-related self-management behavior, and disease-related quality of life. Because we were interested in patterns of family behaviors among adults who can actively self-manage chronic illness, we focused on adults who do not have memory impairment or need assistance with activities of daily living (ADLs). To achieve this goal, we systematically searched health, psychology, and sociology databases for studies examining associations between family behaviors and patient outcomes among patients with diabetes, chronic heart disease, chronic lung disease, chronic kidney disease, and arthritis. We then grouped studies by the type of family behaviors investigated and examined the patterns of associations between these family behaviors and patient outcomes.
Methods
Data Sources and Searches
We conducted this systematic review in consultation with a university-based medical research librarian with expertise in systematic reviews and evidence-based medicine. MEDLINE was searched from 1970 to April 2009 using the following keywords: [chronic disease, self-management, self-care (exploded), diabetes mellitus, hypertension, chronic obstructive pulmonary disease, heart failure, or arthritis] AND [Caregivers (exploded), Family (exploded includes family characteristics, marital status), Friends, Marriage, Family Relations (exploded includes intergenerational relations, sibling relations, parent-child relations), Nuclear Family (exploded includes spouses, siblings, parents), Interpersonal Relations (exploded includes dissent and disputes, professional-family relations, trust), or Role]. CINAHL, PsychInfo, Sociofile, Web of Science, and ISI Proceedings were then searched using database-appropriate terms corresponding as closely as possible to the MEDLINE search terms (exact search strategy available upon request). All searches were limited to studies of adults 18 years and older. We manually searched references of retrieved articles to identify additional pertinent articles.
Definitions of Key Concepts
We defined specific family behaviors as particular ways that family members can relate to the person with illness, for example, by using control or by encouraging self-reliance. The definition of “family” varied by study, but in most cases was limited to persons who lived in the same household as the patient. We labeled a family behavior as “general” when the behavior, as defined and examined in the study, occurred throughout all family interactions, for example general family emphasis on structure and rules. We labeled a family behavior as “disease-specific” when the study examined the behavior solely as it related to illness management, for example overprotective or critical family reactions when discussing illness-related issues.
Study Selection
Eligible studies included original reports of empirical observational research published in peer-reviewed journals. We included studies of adults 18 years or older who had one of the following chronic illnesses that require active self-management on an ongoing basis: diabetes, heart disease, arthritis, chronic lung disease, and end-stage renal disease. We excluded studies that examined the immediate period following an acute event, such as the period immediately following a heart attack, stroke, or surgery. However we included studies with coronary artery disease (CAD) patients that addressed long term issues such as healthy eating, physical activity, medication adherence, or symptom management. We excluded studies focusing on care of adults with dementia or disability requiring assistance with basic ADLs, as family behaviors likely impact patients who need direct care differently than those more capable of self-management. We also excluded studies of cancer patients, whose level of self-management can fluctuate widely over the course of illness, and whose self-management often focuses on symptom and treatment side-effect management. Studies were included if independent variables included the quality of family or marital function or a specific family behavior. Because our goal was to identify specific behaviors that could be encouraged among families of adults with chronic illness, studies solely examining the impact of the patient’s perceived level of social support or the patient’s social network structure were excluded. Eligible studies examined outcomes for the person with chronic illness, including mortality, morbidity, disease control, self-management behavior, and/or disease-related quality of life. Studies solely examining outcomes of patients’ mental health or relationship quality were excluded. English translations of non-English abstracts were reviewed. Any studies that were not clearly excluded by these criteria were reviewed for inclusion by a second author, and disputes were resolved by consensus.
Data Extraction and Quality Assessment
Key information about study methods and results was abstracted using a structured form. Initially, each pair of investigators abstracted a set of three articles, and discrepancies in abstracting methods were reconciled. The remaining articles were abstracted by one author each, and abstracted data were checked by the primary author for accuracy. Study quality was rated using criteria adapted from checklists used by other systematic reviews of survey studies (Fletcher et al. 2005). These criteria are based on survey study methods recommended by key texts (Fink and Kosecoff, 1998; Fowler 2002) and the STROBE guidelines for reporting of observational studies (von Elm et al. 2008). Four aspects of quality were rated for each study: 1)Response rate for cross-sectional studies was rated satisfactory if >70% (Shih and Fan, 2008); however, studies with less than 70% response rate were included and noted in the tables; 2)Studies with less than 40 participants were excluded from the review; 3)The instrument used to measure the family behavior of interest was rated as: well-validated and widely used, not widely used but psychometric properties reported, or problematic (details on instruments used to measure family behaviors are given in Appendices A and B); 4) Analysis method was rated satisfactory if the association of interest was examined with adjustment for patient sociodemographics or disease severity. Studies that did not account for either type of confounder were excluded from the review. Details on analysis methods and covariates are given in Appendix B for included articles and in Appendix C for articles excluded due to low quality.
Data Synthesis and Analysis
We grouped similar family behaviors into family behavior themes, based on the definition of the behavior found in the articles. We then tallied the results of tests of associations between each combination of family behavior theme and chronic illness outcome category. We did not summarize statistical results quantitatively in a meta-analysis for two main reasons. Most important, our goal was to describe and differentiate which specific family behaviors had positive, negative or no associations with illness outcomes, patterns which would be obscured by averaging results for multiple family behaviors. In addition, the reviewed studies examined a wide variety of family behaviors, with a wide range of heterogeneous outcomes. Meta-analysis would require models for each combination of family behavior and outcome type, which would lead to more analysis models than were logistically feasible.
Results
Description of Studies
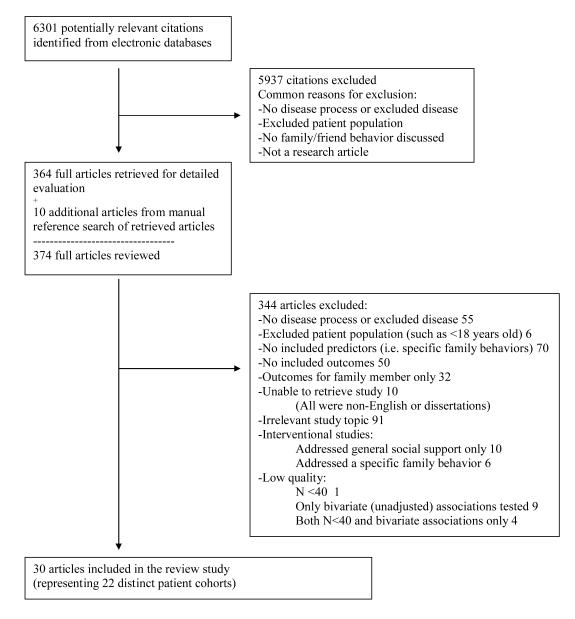
6301 studies were identified based on the keyword search, and 374 full articles meeting initial eligibility criteria were retrieved (Figure 1). 30 articles representing 22 unique participant cohorts met all inclusion criteria for the review.
Figure 1.
Study Selection Process
Table 1 presents characteristics of the included study cohorts (N= 22). Diabetes (N =9) was the most studied condition, followed by arthritis (N = 6, including 5 rheumatoid arthritis [RA] studies and 1 osteoarthritis [OA] study) and cardiovascular disease (CVD, N= 6). One study focused on end stage renal disease (ESRD). Participant gender generally matched expected distributions for each condition; for example RA studies had a majority of female patient participants, coronary artery disease (CAD) and ESRD studies had a majority of male patient participants, and diabetes patient participants were fairly evenly divided by gender. Exceptions were a RA study that focused exclusively on women (Manne and Zautra, 1989, 1990), and CAD (Drory and Florian, 1991) and diabetes (Edelstein and Linn, 1985) studies that focused exclusively on men. Fourteen studies focused on spouse/partner behaviors, while eight focused on family-wide behaviors. A wide range of participant ages were included in the studies, in general representing the expected age distribution of the illnesses studied. Age ranges of all cohorts are not summarized in Table 1, as many studies did not report the full age range of participants. However, nine cohorts clearly included participants less than 45 years old, and only four cohorts clearly excluded participants over 65 years old (Baker et al. 1999; Fisher and Chesla et al. 2000; Trevino et al. 1990; Trief et al. 2001). One OA study (Martire et al. 2006) focused exclusively on older participants (≥ to 50 years old). Seven cohorts contained more than 25% racial or ethnic minority participants; notable were studies focused exclusively on African-Americans with diabetes (Chesla et al. 2004), Chinese-Americans with diabetes (Fisher et al. 2004), and a >90% African-American sample of patients with ESRD (Kimmel et al. 2000). Six of 22 cohorts did not report the race/ethnicity of participants.
Table 1.
Characteristics of Included Studies Total Cohorts = 22*
| Disease Focus | |
| Diabetes | 9 |
| Arthritis | 6 |
| Cardiovascular (Coronary Artery Disease, Hypertension, Heart Failure) |
6 |
| End-Stage Renal Disease | 1 |
| Gender of Cohort Participants | |
| >50% female | 10 |
| Gender not reported | 1 |
| Race/Ethnicity of Cohort Participants | |
| >25% racial/ethnic minority | 7 |
| Race/ethnicity not reported | 6 |
| Relationship(s) Examined | |
| Spouse/partner | 14 |
| Entire family | 8 |
| Examine General or Disease-Specific Family Behaviors | |
| General only | 11 |
| Disease-specific only | 4 |
| Both general and disease-specific | 7 |
| Length of study | |
| Cross-Sectional | 11 |
| Longitudinal (range 3-96 months) | 11 |
Among the 30 individual articles included, we found multiple articles on the same patient cohort. In this table we describe characteristics of distinct patient cohorts (N 22) studied in the included articles.
Study Design and Quality
Table 2 gives details on study design and quality. There were five studies with less than 70 participants (but over 40 participants by inclusion criteria) (Griffin et al. 2001; Hagedoorn et al. 2006; Nicassio and Radojevic, 1993; Rohrbaugh et al. 2008; Williamson et al. 1997). However none of these studies failed to find significant associations between family behaviors and outcomes, alleviating some concerns about study power. Three cross-sectional studies had a response rate <70% (Martire et al. 2006; Garay-Sevilla et al. 1995; Trevino et al. 1990), raising concerns about selection bias, and five did not report response rate. Patient outcomes were measured longitudinally in half (N =11) of the cohorts. Half of the studies measured family behaviors with instruments that were considered to be well-validated and widely used in prior research, many of which focused on general marital satisfaction or family function. Another eight studies (mostly focusing on more specific family behaviors) used relatively new measurement instruments, but also reported instrument psychometric properties in the study. Two studies used family behavior instruments that were not previously tested or validated (Garay-Sevilla et al. 1995; Manne and Zautra, 1990). (See Appendix A for the names of all instruments used to measure family behaviors in the included studies, and references for instrument content and properties.) Two of the four studies measuring self-management behavior as an outcome used unvalidated instruments (Franks et al. 2006; Trevino et al. 1990).
Table 2.
Summary of Study Design, Behaviors Studied, Outcomes, and Quality
| Author Yeara |
Disease | N Follow- Upb |
Populationc | Family Behaviord | Associated Withe | Not Associated With | Study Qualityf | ||
|---|---|---|---|---|---|---|---|---|---|
| Resp Rate |
Measurement | Anal | |||||||
| Martire 2006 | Arthritis- Osteo |
137 C | 70% F 69 yo (7) 95% Cau |
Concordance on pain rating | Pain severity (+) Physical function (+) |
N | R | DZ | |
| Griffin 2001 | Arthritis- Rheumatoid |
42 L | 64% F 55 yo (10) |
Attentive Disease Response | Disease activity (+) | N/A | W | DZ | |
| Punishing Disease Response | Disease activity (−) | ||||||||
| Distracting Disease Response | Disease activity | ||||||||
|
Manne 1989; Manne 1990 |
Arthritis- Rheumatoid |
103 C | 100% F 25-76 yo 96% Cau |
Spousal Criticism (disease related) |
Adjustment to disease (−) Activity limitations (−) Pain (−) |
Arthritis flares frequency / duration |
Y | W/Ng | DZ |
| Nicassio 1993 | Arthritis- Rheumatoid |
44 C | 73% F 55 yo (NR) NR% Cau |
Family Control | Pain (−) | Y | W | B | |
| Family Activity | Disability (+) | ||||||||
| Waltz 1998 | Arthritis- Rheumatoid |
234 L 1 yr |
68-73% F 56 yo (12) & 5N8R y%o (C1a3u) |
Negative Spouse Behavior | Pain (−) | N/A | R | B | |
| Williamson 1997 | Arthritis- Rheumatoid |
52 C | NR% F NR% Cau |
Spouse response: punishing, solicitous, & distracting combined |
Pain behavior (−) | Y | W | DZ | |
| Marital Satisfaction | Pain behavior | ||||||||
| Drory 1991 | CAD | 128 C | 0% F 56 yo (8) 83% Cau |
Family Cohesion - balance | Disease-related QOL | NR | W | B | |
| Family Adaptability | Disease-related QOL | ||||||||
| Franks 2006 | CAD | 94 L 6 mos |
19% F 65 yo (10) 67% Cau |
Social Control | Self-management behavior (−) | N/A | R/W | D | |
| Marital Satisfaction | Self-management behavior (+) | ||||||||
| Chesla 2004 | Diabetes All Type 2 Insulin 25% |
159 C | 60% F 54 yo (9) 0% Cau 100% Af Am |
Family Structure / Organization | Disease-related QOL (+) | Glycemic control Physical activity Eating behavior |
Y | R | B |
| Family World View | Physical activity (+) Disease-related QOL (+/n) |
Glycemic control Eating behavior |
|||||||
| Family Emotion Management (unresolved disease conflict) |
Disease-related QOL (−) | Glycemic control Physical activity Eating behavior |
|||||||
| Edelstein 1985 | Diabetes Type NR Insulin 100% |
97 L 6 mos |
0% F 55 yo (8) 80% Cau |
Family Achievement Orientation |
Metabolic control (+) (Combination of HbA1c, fasting glucose, triglycerides, total cholesterol) |
N/A | W | B | |
| Family Organization | Metabolic control (−) | ||||||||
| Family Conflict | Metabolic control (−) | ||||||||
| Fisher 2004 | Diabetes All Type 2 Insulin 9% |
158 C | 41% F 57 yo (8) 0% Cau 100% Ch Am |
Spouse Respect (disease related) |
Health QOL (+) | Disease-related QOL | Y | R | B |
| Couple Expressiveness | Health QOL | ||||||||
| Spouse Conflict Resolution | Disease-related QOL (−) | Health QOL | |||||||
| Garay-Sevilla 1995 | Diabetes All Type 2 Insulin 0% |
200 C | 66% F 19-85 yo NR% Cau |
Family Functioning | Eating behavior Medication adherence |
N | Nh | B | |
|
Fisher & Chesla 2000; Chesla 2003 |
Diabetes All Type 2 Insulin NR |
187 C161 L 1 yr |
39.8% F 25-62 yo 65% Cau 35% Lat |
Family Structure / Organization C&L |
Physical activity (+) (Lat) C Eating behavior (−) (Lat) C |
HbA1c BMI Disease-related QOL Physical activity (Cau, Lat L) Eating behavior (Cau, Lat L) |
Y | R | B |
| Family Sex Role Traditionalism C |
Health QOL (+) (Cau) Disease-related QOL (−) (Lat) |
HbA1c BMI Physical activity Eating behavior |
|||||||
| Family World View C&L | Health QOL (+) (Cau) C/L Eating behavior (−) (Lat) L |
HbA1c BMI Health QOL (Lat) Physical activity Eating behavior (Cau) |
|||||||
| Family Emotion Management (unresolved disease conflict) C&L |
Eating behavior (−) (Cau) L Health QOL (−) (Lat) C |
HbA1c BMI Health QOL (Cau, Lat L) Physical Activity Eating behavior (Lat) |
|||||||
| Hagedoorn 2006 | Diabetes 67% Type 1 Insulin 100% |
67 L 3 mos |
53% F 45 yo (11) NR% Cau |
Partner Overprotection (disease-related) |
Diabetes-related distress (−) | Glycemic control | N/A | R | D |
| Konen 1993 | Diabetes Type NR Insulin 20% |
409 C | 54% F 53 yo (16) 60% Cau |
Family Cohesion - balanced | Glycemic control | NR | W | B | |
| Trief 1998 | Diabetes 54% Type 1 Insulin 100% |
150C | 44%F 20-79 yo 97%Cau |
Family Cohesion | Physical function (+) | HbA1c Diabetes QOL |
NR | W | B |
| Family Conflict | HbA1c Diabetes QOL |
||||||||
|
Trief 2001; Trief 2002; Trief 2004 |
Diabetes 57% Type 1 Insulin 100% |
78C 60L 2yrs |
42% F 46 yo (11) NR% Cau |
Marital Intimacy | Physical activity C (+) Eating behavior C (+) Follow doctor Diabetes distress C (+) Diabetes |
HbA1c C/L Glucose testing C/L Physical activity L Eating behavior L recommendations L Diabetes distress L Health QOL C/L |
NR | W | B |
| Marital Adjustment | Physical activity C (+) Eating behavior C (+/n) Follow doctor Diabetes QOL C/L (+) Diabetes distress C/L (+) |
HbA1c C/L Glucose testing C/L Physical activity L Eating behavior L Follow doctor recommendations L Health QOL C/L |
|||||||
| Kimmel 2000 | ESRD | 174 L 5 yrs |
23% F 21-80 yo NR% Cau 91% Af Am |
Marital Satisfaction Negative Dyadic Adjustment |
Mortality (+) Mortality (−) |
N/A | W | B | |
| Negative Dyadic Adjustment | Mortality (−) | ||||||||
| Rohrbaugh 2008 | Heart Failure | 57 L 6 mos |
28% F 67 yo (12) 85% Cau |
Spouse “we” talk | Heart failure Combined mental / physical health QOL score (+) |
N/A | R | DZ | |
|
Coyne 2001; Benazon 2006; Rohrbaugh 2006 |
Heart Failure | 184 L | 21-27% F 26-78 yo |
Marital Quality | Mortality | Y | R | B | |
| Useful Illness Discussion | Mortality (+) L 8 yrs |
||||||||
| Positive/Negative Interaction Ratio |
Mortality (+) L 8 yrs |
||||||||
| Spouse Expressed Emotion | Mortality L 4 yrs | ||||||||
|
Baker 1999; Baker 2000; Baker 2003 |
HTN | 205 C 72 Li 103 L 3yrs |
38% F 20-65 yo 75% Cau |
Marital Adjustment / Satisfaction |
Ambulatory blood pressure (+) L Left ventricular mass (+) L |
NR | W | B | |
| Marital Cohesion | Ambulatory | ||||||||
| Trevino 1990 | HTN | 109 C | 58% F 27-63 yo 65% Cau 35% Af Am |
Marital Adjustment | Medication adherence (+) BMI (+) |
Diastolic blood pressure Physical activity Smoking cessation Alcohol consumption |
N | W | D |
If multiple articles studied the same cohort, they are grouped in the same row
If multiple articles per cohort, number of participants in cross-sectional analyses is listed next to C, and number of participants in longitudinal studies is listed next to L. If multiple longitudinal articles per cohort, time to first follow up is given.
Age range listed if given, otherwise mean age of cohort (SD) is listed
Name for family behavior used by the study
(+) = association with patient benefit, (−) = association with patient harm, (n) = no association with patient outcome. Associations are those found at first longitudinal follow-up point unless marked C or L
Resp Rate: Y=response rate >70% (noted for cross-sectional studies only) Measurement: W=well validated instrument used to measure family behavior, R=not well validated but reliability and validity of measurement instruments referenced or tested, N=poor ameasurement techniques (explanations in footnotes)
Instrument measuring patient report of spouse criticism created for this study and psychometric properties not reported
Created own instrument for study, psychometric properties not referenced or reported
N=72 for echocardiogram follow-up, N=103 for ambulatory blood pressure follow-up
Abbreviations: NR=not reported, F=female, yo=years old, yrs=years, mos=months, Cau=Caucasian, Ch Am=Chinese-American, Lat=Latino, Af Am=African-American, C=cross-sectional, L=longitudinal, BMI=body mass index, CAD=coronary artery disease, ESRD=end stage renal disease, HbA1c=hemoglobin A1c, HTN=hypertension, QOL=QOL, SMB=self-management behavior
In analyses of the associations between family behaviors and patient outcome a majority of studies (N =14) adjusted for disease severity and patient sociodemographics, five adjusted only for disease severity, and three adjusted only for patient sociodemographics. Of the four diabetes studies that included patients using either insulin or oral diabetes medications, only two adjusted for medication regimen in analyses (Chesla et al. 2004; Fisher et al. 2004). Only a few studies adjusted for potentially confounding psychosocial factors such as participants’ general social support, overall marital function, or depressive symptoms (Drory and Florian, 1991; Manne and Zautra, 1990; Martire et al. 2006).
Relationships Between Family Behaviors and Patient Chronic Illness Outcomes
General family behaviors were examined in 18 cohorts, and disease-specific family behaviors were examined in 11 cohorts (some studies examined both, see Table 1). The names and definitions of all general and disease-specific family behaviors examined are summarized in Tables 3.1 and 3.2. Forty-one statistically significant associations between family behaviors and patient illness outcomes were identified and are summarized in Table 4. Individual study design, result, and quality information is shown in Table 2, with more detailed information available in Appendix B.
Table 3.1.
General Family Behaviors and Communication Techniques Examined in Included Studies
| Family Behavior Theme | Other Studied Behaviors Included in Theme* |
Explanation of Family Behavior Theme** |
|---|---|---|
| Positive Effects Expected | ||
| Good Marital/Family Function |
Marital Satisfaction Marital Adjustment Marital Quality Positive-Negative Interaction Ratio Family Function |
General composite of satisfaction including: happiness with relationship handling practical issues emotional and physical intimacy communication accommodation respect support |
| Family Cohesion | Marital Cohesion Marital Intimacy Family Cohesion-amount Family Cohesion-balance |
common interests sharing ideas sharing emotional experiences closeness commitment |
| Family Expression | Couple Expressiveness | demonstrating affection expressing emotional state |
| Family Autonomy Encouragement |
Family World View | encourage reliance on self believe world is comprehensible and manageable |
| Negative Effects Expected | ||
| Negative Interactions | Negative Spouse Behavior Negative Dyadic Adjustment |
General composite of negative interactions including: frequent conflicts excessive demands critical interactions lack of common interests |
| Family Criticism | Spouse Criticism Family Conflict |
expressing disapproval, resentment, irritation, impatience |
| Mixed Effects Expected | ||
| Family Achievement Orientation |
casting activities into an achievement-oriented or competitive framework |
|
| Family Activity | participating in social and recreational activities | |
| Family Control | setting rules and procedures to run family life | |
| Family Structure/Organization |
Family Organization | emphasizing orderliness, structure, and similarity to one another |
| Family Sex-Role Traditionalism |
supporting traditional sex roles, such as women working inside the home |
Names for family behaviors used by included studies
Adapted from psychometric instruments used to measure the family behavior theme
Table 4.
Associations Between Family Behavior Themes and Chronic Illness Outcomes in Included Studies
| Chronic Illness Outcome Category * | ||||
|---|---|---|---|---|
| Mortality | Physiologic Control / Symptom Control |
Self-Management Behavior |
Disease-Related Quality of Life |
|
| General Behaviors | ||||
| Positive: | ||||
| Marital/Family Function | ++ | + + + +/n n n | + +/n n n | + |
| Family Cohesion | + n n n | + | + n n | |
| Family Affectional Expression | n | |||
| Family Autonomy Encouragement | n n | + −/n n | + +/n | |
| Negative: | ||||
| Negative Interactions | − | − | n | |
| Family Criticism | − n | n | ||
|
| ||||
| Other: | ||||
| Family Achievement Orientation | + | |||
| Family Activity | + | |||
| Family Control | − | |||
| Family Structure/Organization | − n n | n n | + n | |
| Family Sex-Role traditionalism | n | n | +/− | |
|
| ||||
| Disease-Specific Behaviors | ||||
| Positive: | ||||
| Disease Respect | n | n | +/n | |
| Useful Illness Discussion | + | + | ||
| Attentive Disease Response | + | |||
| “We” Talk | + | |||
|
| ||||
| Negative: | ||||
| Disease Criticism | − | |||
| Disease Overprotection | n − | − | ||
| Punishing Disease Response | − − | |||
| Distracting Disease Response | − n | |||
| Expressed Emotion | n | |||
| Disease Conflicts Unresolved | n n | −/n n | − − −/n | |
|
| ||||
| Other: | ||||
| Social Control | − | |||
Notations are made for each test of association between predictors and outcomes of interest in included studies: + positive association found − negative association found n no association found +/−, +/n, −/n different associations found in same category in same study
Chronic Illness Outcome Types: Physiologic or Symptom Control = glycemic control, blood pressure control, left ventricular size, pain levels, joint inflammation, etc. Self-Management Behavior = adherence to treatment regimens, healthy eating, physical activity Disease-Related Quality of Life = disease-specific quality of life, or physical health subscales of general health QOL instruments
General family behaviors
Several general family behaviors were linked to positive patient outcomes. (Family behaviors are referred to by their family behavior theme names, listed in Tables 3.1 and 3.2.) Family autonomy encouragement, i.e., family encouragement of self-reliance and the ability to manage the surrounding environment, was associated with increased physical activity (Chesla et al. 2004) and better disease-related quality of life among people with diabetes (Chesla et al. 2004; Chesla et al. 2003; Fisher and Chesla et al. 2000). Family achievement orientation, i.e. family casting events into a competitive achievement framework, was positively associated with diabetes metabolic control (Edelstein and Linn, 1985). Family cohesion, i.e., a pattern of common interests and shared emotions within the family, predicted better blood pressure control at 3 years among hypertensive patients (Baker et al. 2000). Among diabetes patients, family cohesion was associated with better self-management behavior (Trief et al. 2001). However in three diabetes studies family cohesion was not associated with glycemic control (Konen et al. 1993; Trief et al. 1998; Trief et al. 2004).
Other general family behaviors were found to be associated with poor patient outcomes. Family control, i.e. an emphasis on rules and procedures in family life, was associated with more pain among adults with rheumatoid arthritis (Nicassio and Radojevic, 1993). Similarly, family structure-organization (i.e. having highly structured relationships, with a strong emphasis on orderliness and routine), was associated with worse metabolic control among men with diabetes (Edelstein and Linn, 1985). Chesla and colleagues (2004) did find that family structure-organization was associated with higher diabetes-related quality of life, but their definition of this behavior included family emphasis on closeness as well as on roles and rules. Family criticism, i.e., a general pattern of conflict in family relationships, was associated with increased pain among rheumatoid arthritis patients (Manne and Zautra, 1990). In addition, family criticism predicted worse glycemic and lipid control at 6 months among people with diabetes in one study (Edelstein and Linn, 1985), but was not associated with glycemic control in another (Trief et al. 1998).
Disease-specific family behaviors
In studies of disease-specific family behaviors, several disease-related communication techniques were associated with physiologic illness control and self-management adherence. Among people with heart failure, useful illness discussion with family members, i.e., discussion about illness that was perceived to be open and useful by the person with heart failure, was associated with an adjusted 8-year survival relative risk (RR) of 1.70 (95% CI 1.27-2.88) per 1 standard deviation (SD) increase in a validated discussion measure (Rohrbaugh et al. 2006). Spouse use of “we” statements more than “I” or “you” statements (reflecting framing of illness management as a group vs. an individual issue) when discussing heart failure management predicted improvement in patients’ heart failure symptoms over six months (Rohrbaugh et al. 2008). In contrast, unresolved disease conflicts were associated with worse eating behavior and worse disease-related quality of life among people with diabetes (Chesla et al. 2004; Chesla et al. 2003; Fisher et al. 2004).
Other studies examined spouse responses to patients’ symptoms or illness management problems. Attentive spouse responses to arthritis symptoms predicted improved rheumatoid arthritis disease activity at 9 months, while punishing (i.e. angry) responses predicted worse disease activity ratings (Griffin et al. 2001). Also among rheumatoid arthritis patients, spouse criticism of patients’ approach to illness management (Manne and Zautra, 1990), and punishing, overprotective, and distracting spouse responses to patient symptoms (Williamson et al. 1997) were associated with increased arthritis pain. In a longitudinal study of coronary artery disease patients, spouse use of social control, defined as rewards, threats, or a sense of obligation to “correct” patient health behaviors, predicted worse patient self-management behavior over 6 months (Franks et al. 2006).
Marital or family function
Generally positive marital or family function was beneficially associated with all categories of illness outcomes, most strikingly with improved mortality and physiologic control of illness. In a study of adults with heart failure, high marital quality predicted significantly lower mortality risk at 8 years (adjusted RR 0.50, 95%CI 0.73-0.34) compared to those with low marital quality (Benazon et al. 2006; Rohrbaugh et al. 2006). The impact of marital quality on survival was similar in magnitude to the independent effect of NYHA classification in the same study (adjusted RR survival 0.57 per increase in level). Positive marital function also predicted improved blood pressure control and left-ventricular mass among patients with hypertension (HTN) (Baker et al. 2003). In this study, those with high marital satisfaction had a subsequent mean 24-hour diastolic blood pressure 3.2 mmHg lower than those with low marital satisfaction, similar to the 2.6 mmHg decrease associated with HTN medication adherence in the same study. Among patients with ESRD, marital satisfaction predicted a significantly lower risk of 3 year mortality (adjusted RR 0.71, 95% CI 0.54-0.93 for each SD increase in marital satisfaction), and negative marital interactions predicted a significantly higher risk of mortality (adjusted RR 1.46, 95% CI 1.14-1.87 for each SD increase in negative interactions), after adjusting for patient age, renal disease severity, serum albumin, and dialyzer type (Benazon et al. 2006; Kimmel et al. 2000). These independent effects on mortality were similar to those found for age (RR 1.80), female gender (RR 0.63), dialysis compliance (RR 0.76), and general social support (RR 0.64). In studies among CAD, HTN, and diabetes patients, positive family functioning was associated with improved eating behavior, physical activity, and medication adherence (Franks et al. 2006; Trevino et al. 1990; Trief et al. 2004). However positive family function was not associated with glycemic control in two diabetes studies (Konen et al. 1993; Trief et al. 2004).
Moderators of Family Behavior Effects
Several potential moderators of family behavior effects were examined. When gender affected the magnitude of the family behavior-outcome association, associations were generally stronger for women than for men. For example, Kimmel et al. (2000) found that positive and negative marital function more strongly affected ESRD mortality risk among women, and Coyne et al. (2001) found that marital quality and useful illness discussions affected heart failure mortality more strongly for women. Among patients with diabetes, partner overprotection predicted significantly higher HbA1c levels among women than in men (Hagedoorn et al. 2006). However in another diabetes study, the effect of family environment on diabetes outcomes did not significantly vary by gender (Fisher and Chesla et al. 2000). And, in contrast to the previously mentioned studies, Fisher et al. (2004) found that unresolved conflict about diabetes management was associated with significantly higher levels of physical activity, but also more fat consumption, in men than in women.
Only one study examined patient age as a modifier, and found that younger participants (age 27-50 years old) with positive marital adjustment had more improvement in HTN medication adherence than older participants (Trevino et al. 1990). Fisher and Chesla et al. (2000) were the only investigators to compare effects of family behaviors across racial/ethnic groups. In this cohort, increased family autonomy encouragement predicted improved disease-related quality of life among Caucasians with diabetes, but predicted worse dietary intake and glycemic control among Latinos. In the same study, family sex-role traditionalism (i.e. support of traditional gender roles in the family), was associated with increased disease-related quality of life among Caucasians but with decreased quality of life among Latinos. In addition, unresolved disease conflicts led to worse eating behavior among Caucasians with no impact on Latinos, and family structure impacted Latinos’ physical activity and eating behavior but not Caucasians’.
Finally, Baker et al. found that the effect of marital adjustment on HTN control varied by the amount of time partners spent together (Baker et al. 2003). Patients with good marital adjustment and high amount of spouse contact, and those with poor marital adjustment and lower spouse contact, had lower blood pressures at follow-up than other participants.
Discussion
In this review, we summarize evidence that family function and certain specific family behaviors are associated with self-management behavior and outcomes for adults with chronic illness. The outcomes associated with family behaviors included clinical outcomes of mortality, blood pressure control, cardiac ventricular hypertrophy, glycemic control, and joint inflammation. Positive marital and family function was the most studied factor, and evidence suggests that it predicts better physiologic control of illness and improved chronic illness patient survival.
Among specific family behaviors, grouping behaviors by theme allowed us to assess whether results were consistent with behavioral theories that address influences on successful chronic illness management. The results of many of the reviewed studies are consistent with self-determination theory (Ryan and Deci, 2000), which states that support of an individual’s autonomy and competence, and relating motivation for behavior change to the person’s concept of self, leads to higher patient engagement in health behaviors. Reviewed studies found that family encouragement of self-reliance, autonomy, and personal achievement for the person with illness, as well as family cohesion, were associated with improved illness outcomes in rheumatoid arthritis, CAD, HTN, and diabetes. Also consistent with self-determination theory, family behaviors that emphasized control, criticism, and overprotection were associated with negative illness outcomes. Among illness management coping strategies described by coping theory (Lazarus and Folkman, 1984), evidence in this review supported family use of active, problem-focused coping strategies over avoidant strategies. For example, attentive responses and open illness discussion predicted improved illness outcomes, while unresolved disease-related conflicts and angry responses were associated with worse illness outcomes, across rheumatoid arthritis, diabetes, and heart failure.
Prior studies of the health impacts of family behaviors have found results that are complementary to those of this review. Several qualitative studies of adults with chronic illness and their family members have identified family autonomy support, overprotectiveness, and poor communication as influential to patient illness management (Bailey and Kahn, 1993; Gallant 2007; Sandberg et al. 2006; Trief et al. 2003). A 2008 review of communication styles between adolescents with type 1 diabetes and their parents found that family conflict and control were linked to worse adolescent diabetes outcomes (Dashiff et al. 2008). Di Matteo’s meta-analysis (2004) of social support effects on treatment adherence included studies of children with a wide range of chronic illnesses, but also found that family cohesiveness and family conflict significantly affected self-management adherence.
In this review, patient gender and race/ethnicity moderated specific family behavior effects in ways that mirror the influences of gender and race/ethnicity on perceived general social support found in other literature. In particular, previous studies have found that general social support effects are stronger for women than men (Gallant and Dorn, 2001; Jackson 2006; Kaplan and Hartwell, 1987; Rosland et al. 2010; Wing et al. 1991) and vary by race/ethnicity (Bailey and Lherisson-Cedeno, 1997; Fitzgerald et al. 1997; Ford et al. 1998). Most studies in this review examining gender differences found that both positive and negative family behaviors had stronger effects for women than men. This finding could be related to relationship context, such as expected family roles for women, or individual factors such as gender related differences in coping mechanisms. Differences in the cultural context of relationships, such as expected family member roles and family health beliefs, could have led to the different effects of family behaviors observed among Caucasians and Latinos. Family race/ethnicity and cultural beliefs are potentially potent modifiers of family behavior effects that deserve more attention in future studies.
Future research on family behaviors in chronic illness management could address several important topics that received little or no attention in these reviewed studies. While older patients may be more likely to have family involvement in illness management, only one study focused on older patients (Martire et al. 2006). One prevalent chronic illness, chronic lung disease, was not addressed in the included studies, although studies on family environment in asthma (Geden et al. 2002) and on marital adjustment in chronic obstructive pulmonary disease (Ashmore et al. 2005) were excluded due to quality problems (see Appendix C for a list of studies otherwise meeting inclusion criteria that were excluded due to quality problems). The role of family behaviors in chronic advanced renal disease, which requires significant ongoing self-management, also deserves further study.
Among family behaviors, more studies on disease-specific family behaviors are warranted, since there is growing evidence that disease-specific social support has more impact on health outcomes than general social support (Aalto et al. 1997; Bediako and Friend, 2004; Gallant 2003). In addition, many of the studies excluded for quality reasons addressed family-wide behaviors, as opposed to focusing on spouses only (see Appendix C). Future high-quality studies on family-wide behaviors in chronic illness would be valuable.
Among patient outcomes, there were few studies of the impact of family behavior on self-management adherence, despite strong evidence that general social support affects self-management behavior (Gallant 2003). Future studies of family behaviors in chronic illness should study self-management behavior as an outcome, using available validated measures of self-management behavior. Furthermore, there is evidence that social support affects some self-management behaviors differently than others (Hogan et al. 2002; Nicklett and Liang, 2010; Rosland et al. 2008), so future studies should examine the effect of family behavior on individual self-management behaviors whenever possible.
Few studies evaluated the relationship between specific family member behaviors and perceived social support, making it difficult to examine whether family member behaviors impact outcomes through increased perceived support (Franks et al. 1992). In the reviewed study by Kimmel and colleagues (2000), good marital function predicted mortality among people with ESRD even when adjusted for perceived social support, suggesting that marital function may be working through mechanisms beyond increasing perceived support. In the study by Garay-Sevilla and colleagues (1995), general perceived social support was associated with increased patient dietary and medication adherence, while controlling behavior among family members was associated with less patient medication adherence only, suggesting that behaviors or influences outside of family member control were more important for dietary adherence. Future studies that explore the relationship between specific family behaviors and patients’ perceived social support could provide important information about the mechanisms of family behavior effects and the relative importance of non-family sources of social support.
Several methodological weaknesses were found among the studies in this review. Addressing these issues could greatly improve the quality of evidence regarding the health impacts of family member behavior. The cross-sectional design of half of the studies presented challenges for study interpretation, since it was difficult to determine whether family behaviors led to differences in health status, or whether variations in health status caused differences in family behaviors. However, half of the included cohorts examined longitudinal outcomes, including all studies of mortality outcomes, and several studies of marital function effects. Specific family behaviors with significant longitudinal effects included family cohesion, family encouragement of self-reliance and achievement, and useful illness discussion (positive effects); and family criticism, family emphasis on structure, disease overprotection, and punishing disease response (negative effects). If taken alone, these longitudinal results still support conclusions that family support of autonomous motivation and active coping styles positively impact illness outcomes. Nevertheless, more longitudinal studies are needed to confirm these patterns, and we recommend that future studies of family behavior influences on chronic illness outcomes use longitudinal designs whenever possible.
To further improve methodologic quality, future studies should adjust analyses for factors known to affect illness outcomes, such as disease severity, and use validated instruments for measuring family behaviors. Among patients with diabetes, there is evidence that family behaviors affect patients using insulin differently than those using oral medications only. It is notable that, among the eight studies in this review examining glycemic control or diabetes self-management behavior as outcomes, only the two studies with 100% insulin-using patients found significant effects of family behavior (Edelstein and Linn, 1985; Hagedoorn et al. 2006). Future studies of family behaviors among diabetes patients should adjust for medication regimen and consider evaluating differences among those who use insulin versus those who do not. Finally, all studies of family behaviors should account for the confounding effects of mental health. Family behavior affects symptoms of depression and anxiety among patients, and poor mental health can also lead to an erosion of social support (Bisschop et al. 2004; Connell et al. 1994; Sherman 2003; Uchino 2004). Future studies of family behavior should at minimum control for mental health symptoms, and could also consider examining mental health as a determinant of family behavior or as a moderator of family behavior effects.
Our review itself has limitations. Due to our study goals and the wide heterogeneity among family behaviors and outcomes, a meta-analysis with a quantitative averaged outcome was neither desirable nor feasible. Therefore the current review should be interpreted as a first step in describing the state of the literature, and future meta-analyses of the magnitude of the effects of certain family behaviors may be warranted when more high-quality evidence is available. Second, we included results from studies that examined associations between multiple family behaviors and outcomes, which could have led to false positive findings from chance alone. Third, despite the use of quality criteria based on accepted standards (von Elm et al. 2008), our choice of quality criteria was by necessity arbitrary, and quality ratings included some subjective judgments. Finally, our focus on adult, functionally independent patients limits the generalizability of results observed to other patient populations. In particular, family behaviors that focus on autonomous motivation of patient self-management may not be the most beneficial to small children, mentally or cognitively impaired patients, or patients who need assistance with basic ADLs. In addition, valuable family behaviors and coping techniques may vary for patients with acute illnesses, long periods of quiescence between illness episodes, or illnesses such as cancer in which symptom and treatment side-effect management are predominant.
Despite these limitations, our results have important implications for future research and practice. Researchers could further study family behaviors that are consistent with promising behavioral theories, and expand the evidence-base by studying the influence of family behaviors not yet well examined. Practitioners should be aware of the evidence that family members can increase or decrease the effectiveness of efforts to improve illness control and quality of life for those with chronic illness. Practitioners should consider asking people with chronic illness how their family interacts with them and influences their illness management. Illness management programs should emphasize those family behaviors with the most evidence of positively influencing patient outcomes, for example, by promoting family autonomy encouragement and discouraging family criticism. Most importantly, interventions should be developed and evaluated which aim to increase those family behaviors with the most observational evidence of impact on outcomes.
In summary, this review suggests that family use of patient autonomy-supportive behaviors and active illness management coping strategies positively affect chronic illness outcomes. More research is needed to determine which family behaviors most influence chronic illness management and to determine how to influence those family behaviors in ways that improve illness outcomes.
Supplementary Material
Table 3.2.
Disease-Specific Family Behaviors and Communication Techniques Examined in Included Studies
| Family Behavior Theme | Other Studied Behaviors Included in Theme* |
Explanation of Family Behavior Theme** |
|---|---|---|
| Positive Effects Expected | ||
| Disease Respect | Spouse Respect | In disease-related matters: taking person with illness seriously trying to understand chronically ill person’s point of view respecting independence |
| Useful Illness Discussion | Concordance on Pain Rating | frequent useful discussions about illness |
| Attentive Disease Response | focusing on symptoms asking how to help sufferer |
|
| “We” Talk About Disease | Proportion of first-person plural (“we, us, our”) pronouns of total pronouns when discussing illness management |
|
| Negative Effects Expected | ||
| Disease Criticism | Spouse Criticism | in disease-related matters expressing disapproval, resentment, irritation, impatience |
| Disease Overprotection | Partner Overprotection Solicitous Disease Response |
discounting person’s ability to handle disease and symptoms, taking over self-management tasks |
| Punishing Disease Response | anger in response to symptom | |
| Distracting Disease Response | Spouse Distraction | distracting from symptoms by bringing up other topic or activity |
| Expressed Emotion | Combination of 3 concepts: hostility towards person with illness emotional over-involvement: family blames selves making critical comments |
|
| Disease Conflicts Unresolved | Spouse Conflict Resolution Family Emotion Management |
conflicts about disease remain unresolved discussing disease-related issues avoided |
| Mixed Effects Expected | ||
| Social Control | using behavioral control (rewards, threats, sense of obligation) to “correct” people who are unsuccessful or unwilling to make healthy behavior changes |
Names for family behaviors used by included studies
Adapted from psychometric instruments used to measure the family behavior theme.
Acknowledgements
Funding Sources: This research was supported by the Department of Veterans Affairs, the Robert Wood Johnson Clinical Scholars Program, the Michigan Diabetes Research and Training Center (NIH #UL1RR024986) and the Michigan Institute for Clinical and Health Research (NIH #UL1RR024986). John Piette is a VA Senior Career Scientist.
Reference database searches done by Gurpreet K. Rana, MLIS, University of Michigan Taubman Medical Library. Ms. Rana received compensation for this work from the University of Michigan Robert Wood Johnson Clinical Scholars Program. We would like to thank Sarah Conner, Jessica Forestier, and Meghan Schmansky for assistance with compiling data and editing.
Footnotes
Conflicts of Interest: none to report
References
- Aalto AM, Uutela A, Aro AR. Health related quality of life among insulin-dependent diabetics: disease-related and psychosocial correlates. Patient Education & Counseling. 1997;30(3):215–225. doi: 10.1016/s0738-3991(96)00963-9. [DOI] [PubMed] [Google Scholar]
- Ashmore JA, Emery CF, Hauck ER, MacIntyre NR. Marital adjustment among patients with chronic obstructive pulmonary disease who are participating in pulmonary rehabilitation. Heart & Lung. 2005;34(4):270–278. doi: 10.1016/j.hrtlng.2004.12.005. [DOI] [PubMed] [Google Scholar]
- Bailey BJ, Kahn A. Apportioning illness management authority: how diabetic individuals evaluate and respond to spousal help. Qual Health Res. 1993;3(1):55–73. doi: 10.1177/104973239300300104. [DOI] [PubMed] [Google Scholar]
- Bailey BJ, Lherisson-Cedeno D. Diabetes outcomes and practices: comparison of African Americans and Caucasians. Journal of National Black Nurses Association. 1997;9(1):66–75. [PubMed] [Google Scholar]
- Baker B, Helmers K, O’Kelly B, Sakinofsky I, Abelsohn A, Tobe S. Marital cohesion and ambulatory blood pressure in early hypertension. American Journal of Hypertension. 1999;12(2 Pt 1):227–230. doi: 10.1016/s0895-7061(98)00184-8. [DOI] [PubMed] [Google Scholar]
- Baker B, Paquette M, Szalai JP, Driver H, Perger T, Helmers K, et al. The influence of marital adjustment on 3-year left ventricular mass and ambulatory blood pressure in mild hypertension. Archives of Internal Medicine. 2000;160(22):3453–3458. doi: 10.1001/archinte.160.22.3453. [DOI] [PubMed] [Google Scholar]
- Baker B, Szalai JP, Paquette M, Tobe S. Marital support, spousal contact and the course of mild hypertension. Journal of Psychosomatic Research. 2003;55(3):229–233. doi: 10.1016/s0022-3999(02)00551-2. [DOI] [PubMed] [Google Scholar]
- Bediako SM, Friend R. Illness-Specific and General Perceptions of Social Relationships in Adjustment to Rheumatoid Arthritis: The Role of Interpersonal Expectations. Annals of Behavioral Medicine. 2004;28(3):203–210. doi: 10.1207/s15324796abm2803_9. [DOI] [PubMed] [Google Scholar]
- Benazon NR, Foster MD, Coyne JC. Expressed emotion, adaptation, and patient survival among couples coping with chronic heart failure. Journal of Family Psychology. 2006;20(2):328–334. doi: 10.1037/0893-3200.20.2.328. [DOI] [PubMed] [Google Scholar]
- Berg CA, Upchurch R. A developmental-contextual model of couples coping with chronic illness across the adult life span. Psychological Bulletin. 2007;133(6):920–954. doi: 10.1037/0033-2909.133.6.920. [DOI] [PubMed] [Google Scholar]
- Bisschop MI, Kriegsman DM, Beekman AT, Deeg DJ. Chronic diseases and depression: the modifying role of psychosocial resources. [Research Support, Non-U.S. Gov’t] Social Science & Medicine. 2004;59(4):721–733. doi: 10.1016/j.socscimed.2003.11.038. [DOI] [PubMed] [Google Scholar]
- Chesla CA, Fisher L, Mullan JT, Skaff MM, Gardiner P, Chun K, et al. Family and disease management in African-American patients with type 2 diabetes. Diabetes Care. 2004;27(12):2850–2855. doi: 10.2337/diacare.27.12.2850. [DOI] [PubMed] [Google Scholar]
- Chesla CA, Fisher L, Skaff MM, Mullan JT, Gilliss CL, Kanter R. Family predictors of disease management over one year in Latino and European American patients with type 2 diabetes. Family Process. 2003;42(3):375–390. doi: 10.1111/j.1545-5300.2003.00375.x. [DOI] [PubMed] [Google Scholar]
- Connell CM. Psychosocial contexts of diabetes and older adulthood: reciprocal effects. Diabetes Educator. 1991;17(5):364–371. doi: 10.1177/014572179101700507. [DOI] [PubMed] [Google Scholar]
- Connell CM, Davis WK, Gallant MP, Sharpe PA. Impact of social support, social cognitive variables, and perceived threat on depression among adults with diabetes. Health Psychology. 1994;13(3):263–273. doi: 10.1037//0278-6133.13.3.263. [DOI] [PubMed] [Google Scholar]
- Coyne JC, Rohrbaugh MJ, Shoham V, Sonnega JS, Nicklas JM, Cranford JA, et al. Prognostic importance of marital quality for survival of congestive heart failure. American Journal of Cardiology. 2001;88(5):526–529. doi: 10.1016/s0002-9149(01)01731-3. [DOI] [PubMed] [Google Scholar]
- Dashiff C, Hardeman T, McLain R. Parent-adolescent communication and diabetes: an integrative review. Journal of Advanced Nursing. 2008;62(2):140–162. doi: 10.1111/j.1365-2648.2007.04549.x. [DOI] [PubMed] [Google Scholar]
- DiMatteo MR. Social support and patient adherence to medical treatment: a meta-analysis. Health Psychology. 2004;23(2):207–218. doi: 10.1037/0278-6133.23.2.207. [DOI] [PubMed] [Google Scholar]
- Drory Y, Florian V. Long-term psychosocial adjustment to coronary artery disease. Archives of Physical Medicine & Rehabilitation. 1991;72(5):326–331. [PubMed] [Google Scholar]
- Edelstein J, Linn MW. The influence of the family on control of diabetes. Social Science & Medicine. 1985;21(5):541–544. doi: 10.1016/0277-9536(85)90038-3. [DOI] [PubMed] [Google Scholar]
- Fink A, Kosecoff JB. How to Conduct Surveys: A Step-by-Step Guide. Sage Publications; Thousand Oaks, CA: 1998. [Google Scholar]
- Fisher L, Chesla CA, Bartz RJ, Gilliss C, Skaff MA, Sabogal F, et al. The family and type 2 diabetes: a framework for intervention. Diabetes Educator. 1998;24(5):599–607. doi: 10.1177/014572179802400504. [DOI] [PubMed] [Google Scholar]
- Fisher L, Chesla CA, Chun KM, Skaff MM, Mullan JT, Kanter RA, et al. Patient-appraised couple emotion management and disease management among Chinese American patients with type 2 diabetes. Journal of Family Psychology. 2004;18(2):302–310. doi: 10.1037/0893-3200.18.2.302. [DOI] [PubMed] [Google Scholar]
- Fisher L, Chesla CA, Skaff MM, Gilliss C, Mullan JT, Bartz RJ, et al. The family and disease management in Hispanic and European-American patients with type 2 diabetes. Diabetes Care. 2000;23(3):267–272. doi: 10.2337/diacare.23.3.267. [DOI] [PubMed] [Google Scholar]
- Fisher L, Weihs KL. Can addressing family relationships improve outcomes in chronic disease? Report of the National Working Group on Family-Based Interventions in Chronic Disease. Journal of Family Practice. 2000;49(6):561–566. [PubMed] [Google Scholar]
- Fitzgerald JT, Anderson RM, Funnell MM, Arnold MS, Davis WK, Aman LC, et al. Differences in the impact of dietary restrictions on African Americans and Caucasians with NIDDM. Diabetes Educator. 1997;23(1):41–47. doi: 10.1177/014572179702300104. [DOI] [PubMed] [Google Scholar]
- Fletcher K, Underwood W, III, Davis SQ, Mangrulkar RS, McMahon LF, Jr, Saint S. Effects of work hour reduction on residents’ lives: A systematic review. JAMA. 2005;294(9):1088–1100. doi: 10.1001/jama.294.9.1088. [DOI] [PubMed] [Google Scholar]
- Ford ME, Tilley BC, McDonald PE. Social support among African-American adults with diabetes, Part 2: A review. Journal of the National Medical Association. 1998;90(7):425–432. [PMC free article] [PubMed] [Google Scholar]
- Fowler FJ. Survey Research Methods. 3rd ed Sage Publications; Thousand Oaks, CA: 2002. [Google Scholar]
- Franks MM, Stephens MA, Rook KS, Franklin BA, Keteyian SJ, Artinian NT. Spouses’ provision of health-related support and control to patients participating in cardiac rehabilitation. Journal of Family Psychology. 2006;20(2):311–318. doi: 10.1037/0893-3200.20.2.311. [DOI] [PubMed] [Google Scholar]
- Franks P, Campbell TL, Shields CG. Social relationships and health: the relative roles of family functioning and social support. Social Science & Medicine. 1992;34(7):779–788. doi: 10.1016/0277-9536(92)90365-w. [DOI] [PubMed] [Google Scholar]
- Friedman MM. Social support sources and psychological well-being in older women with heart disease. Research in Nursing & Health. 1993;16(6):405–413. doi: 10.1002/nur.4770160604. [DOI] [PubMed] [Google Scholar]
- Friedmann E, Thomas SA, Liu F, Morton PG, Chapa D, Gottlieb SS. Relationship of depression, anxiety, and social isolation to chronic heart failure outpatient mortality. American Heart Journal. 2006;152(5):940.e941–948. doi: 10.1016/j.ahj.2006.05.009. [DOI] [PubMed] [Google Scholar]
- Gallant M. The influence of social support on chronic illness self-management: a review and directions for research. Health education & behavior. 2003;30(2):170–195. doi: 10.1177/1090198102251030. [DOI] [PubMed] [Google Scholar]
- Gallant M. Help or hindrance? How family and friends influence chronic illness self-management among older adults.(Report) Research on aging. 2007;29(5):375. [Google Scholar]
- Gallant M, Dorn GP. Gender and race differences in the predictors of daily health practices among older adults. Health Education Research. 2001;16(1):21–31. doi: 10.1093/her/16.1.21. [DOI] [PubMed] [Google Scholar]
- Garay-Sevilla ME, Nava LE, Malacara JM, Huerta R, Diaz de Leon J, Mena A, et al. Adherence to treatment and social support in patients with non-insulin dependent diabetes mellitus. Journal of Diabetes & its Complications. 1995;9(2):81–86. doi: 10.1016/1056-8727(94)00021-f. [DOI] [PubMed] [Google Scholar]
- Geden E, Isaramalai S, Taylor S. Influences of partners’ views of asthma self-management and family environment on asthmatic adults’ asthma quality of life. Applied Nursing Research. 2002;15(4):217–226. doi: 10.1053/apnr.2002.35945. [DOI] [PubMed] [Google Scholar]
- Gleeson-Kreig J, Bernal H, Woolley S. The role of social support in the self-management of diabetes mellitus among a Hispanic population. Public Health Nursing. 2002;19(3):215–222. doi: 10.1046/j.0737-1209.2002.19310.x. [DOI] [PubMed] [Google Scholar]
- Griffin KW, Friend R, Kaell AT, Bennett RS. Distress and disease status among patients with rheumatoid arthritis: Roles of coping styles and perceived responses from support providers. Annals of Behavioral Medicine. 2001;23(2):133–138. doi: 10.1207/S15324796ABM2302_8. [DOI] [PubMed] [Google Scholar]
- Griffith LS, Field BJ, Lustman PJ. Life stress and social support in diabetes: association with glycemic control. International Journal of Psychiatry in Medicine. 1990;20(4):365–372. doi: 10.2190/APH4-YMBG-NVRL-VLWD. [DOI] [PubMed] [Google Scholar]
- Hagedoorn M, Keers JC, Links TP, Bouma J, Ter Maaten JC, Sanderman R. Improving self-management in insulin-treated adults participating in diabetes education. The role of overprotection by the partner. Diabetic Medicine. 2006;23(3):271–277. doi: 10.1111/j.1464-5491.2006.01794.x. [DOI] [PubMed] [Google Scholar]
- Hogan BE, Linden W, Najarian B. Social support interventions: Do they work? Clinical Psychology Review. 2002;22(3):381–440. doi: 10.1016/s0272-7358(01)00102-7. [DOI] [PubMed] [Google Scholar]
- Holder B. Family support and survival among African-American end-stage renal disease patients. Advances in Renal Replacement Therapy. 1997;4(1):13–21. doi: 10.1016/s1073-4449(97)70012-8. [DOI] [PubMed] [Google Scholar]
- House JS, Landis KR, Umberson D. Social relationships and health. Science. 1988;241(4865):540–545. doi: 10.1126/science.3399889. [DOI] [PubMed] [Google Scholar]
- Jackson T. Relationships between perceived close social support and health practices within community samples of American women and men. The Journal of Psychology. 2006;140(3):229–246. doi: 10.3200/JRLP.140.3.229-246. [DOI] [PubMed] [Google Scholar]
- Kaplan RM, Hartwell SL. Differential effects of social support and social network on physiological and social outcomes in men and women with type II diabetes mellitus. Health Psychology. 1987;6(5):387–398. doi: 10.1037//0278-6133.6.5.387. [DOI] [PubMed] [Google Scholar]
- Kimmel PL, Peterson RA, Weihs KL, Shidler N, Simmens SJ, Alleyne S, et al. Dyadic relationship conflict, gender, and mortality in urban hemodialysis patients. Journal of the American Society of Nephrology. 2000;11(1518-1525) doi: 10.1681/ASN.V1181518. [DOI] [PubMed] [Google Scholar]
- Konen JC, Summerson JH, Dignan MB, Konen JC, Summerson JH, Dignan MB. Family function, stress, and locus of control. Relationships to glycemia in adults with diabetes mellitus. Archives of Family Medicine. 1993;2(4):393–402. doi: 10.1001/archfami.2.4.393. [DOI] [PubMed] [Google Scholar]
- Krol B, Sanderman R, Suurmeijer TP. Social support, rheumatoid arthritis and quality of life: concepts, measurement and research. Patient Education & Counseling. 1993;20(2-3):101–120. doi: 10.1016/0738-3991(93)90125-g. [DOI] [PubMed] [Google Scholar]
- Lazarus RS, Folkman S. Stress, Appraisal, and Coping. Springer; New York: 1984. [Google Scholar]
- Leff J, Vaughn C. Its significance for mental illness. Guilford Press; New York: 1985. Expressed emotion in families. [Google Scholar]
- Lett HS, Blumenthal JA, Babyak MA, Strauman TJ, Robins C, Sherwood A. Social support and coronary heart disease: epidemiologic evidence and implications for treatment. Psychosomatic Medicine. 2005;67(6):869–878. doi: 10.1097/01.psy.0000188393.73571.0a. [DOI] [PubMed] [Google Scholar]
- Lutz BJ, Chumbler NR, Lyles T, Hoffman N, Kobb R. Testing a home-telehealth programme for US veterans recovering from stroke and their family caregivers. Disabilty & Rehabilitation. 2009;31(5):402–409. doi: 10.1080/09638280802069558. [DOI] [PubMed] [Google Scholar]
- Manne SL, Zautra AJ. Spouse criticism and support: Their association with coping and psychological adjustment among women with rheumatoid arthritis. Journal of Personality and Social Psychology. 1989;56(4):608–617. doi: 10.1037//0022-3514.56.4.608. [DOI] [PubMed] [Google Scholar]
- Manne SL, Zautra AJ. Couples coping with chronic illness: women with rheumatoid arthritis and their healthy husbands. Journal of Behavioral Medicine. 1990;13(4):327–342. doi: 10.1007/BF00844882. [DOI] [PubMed] [Google Scholar]
- Marino P, Sirey JA, Raue PJ, Alexopoulos GS. Impact of social support and self-efficacy on functioning in depressed older adults with chronic obstructive pulmonary disease. International Journal of Chronic Obstructive Pulmonary Disease. 2008;3(4):713–718. doi: 10.2147/copd.s2840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martire LM, Lustig AP, Schulz R, Miller GE, Helgeson VS. Is it beneficial to involve a family member? A meta-analysis of psychosocial interventions for chronic illness. Health Psychology. 2004;23(6):599–611. doi: 10.1037/0278-6133.23.6.599. [DOI] [PubMed] [Google Scholar]
- Martire LM, Keefe FJ, Schulz R, Ready R, Beach SR, Rudy TE, et al. Older spouses’ perceptions of partners’ chronic arthritis pain: implications for spousal responses, support provision, and caregiving experiences. Psychology & Aging. 2006;21(2):222–230. doi: 10.1037/0882-7974.21.2.222. [DOI] [PubMed] [Google Scholar]
- Murberg TA, Bru E. Social relationships and mortality in patients with congestive heart failure. Journal of Psychosomatic Research. 2001;51(3):521–527. doi: 10.1016/s0022-3999(01)00226-4. [DOI] [PubMed] [Google Scholar]
- Nicassio PM, Radojevic V. Models of family functioning and their contribution to patient outcomes in chronic pain. Motivation and Emotion. 1993;17(3):295–316. [Google Scholar]
- Nicklett EJ, Liang J. Diabetes-related support, regimen adherence, and health decline among older adults. Journals of Gerontology Series B-Psychological Sciences & Social Sciences. 2010;65B(3):390–399. doi: 10.1093/geronb/gbp050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel SS, Peterson RA, Kimmel PL. The impact of social support on end-stage renal disease. Seminars in Dialysis. 2005;18(2):98–102. doi: 10.1111/j.1525-139X.2005.18203.x. [DOI] [PubMed] [Google Scholar]
- Rohrbaugh MJ, Mehl MR, Shoham V, Reilly ES, Ewy GA. Prognostic significance of spouse we talk in couples coping with heart failure. Journal of Consulting & Clinical Psychology. 2008;76(5):781–789. doi: 10.1037/a0013238. [DOI] [PubMed] [Google Scholar]
- Rohrbaugh MJ, Shoham V, Coyne JC. Effect of marital quality on eight-year survival of patients with heart failure. American Journal of Cardiology. 2006;98(8):1069–1072. doi: 10.1016/j.amjcard.2006.05.034. [DOI] [PubMed] [Google Scholar]
- Rosland AM, Heisler M, Choi H, Silveira M, Piette JD. Family influences on self management among functionally independent adults with diabetes or heart failure: Do family members hinder as much as they help? Chronic Illness. 2010;6(1):22–33. doi: 10.1177/1742395309354608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosland AM, Kieffer E, Israel B, Cofield M, Palmisano G, Sinco B, et al. When is social support important? The association of family support and professional support with specific diabetes self-management behaviors. Journal of General Internal Medicine. 2008;23(12):1992–1999. doi: 10.1007/s11606-008-0814-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rusbult CE, Van Lange PA. Interdependence, interaction, and relationships. Annual Review of Psychology. 2003;54:351–375. doi: 10.1146/annurev.psych.54.101601.145059. [DOI] [PubMed] [Google Scholar]
- Rutledge T, Reis SE, Olson M, Owens J, Kelsey SF, Pepine CJ, et al. Social networks are associated with lower mortality rates among women with suspected coronary disease: the National Heart, Lung, and Blood Institute-Sponsored Women’s Ischemia Syndrome Evaluation study. Psychosomatic Medicine. 2004;66(6):882–888. doi: 10.1097/01.psy.0000145819.94041.52. [DOI] [PubMed] [Google Scholar]
- Ryan RM, Deci EL. Self-determination theory and facilitation of intrinsic motivation, social development, and well-being. American Psychologist. 2000;55(1):68–78. doi: 10.1037//0003-066x.55.1.68. [DOI] [PubMed] [Google Scholar]
- Sandberg J, Trief PM, Greenberg RP, Graff K, Weinstock RS. He said, she said": the impact of gender on spousal support in diabetes management. Journal of Couple & Relationship Therapy. 2006;5(2):23–42. [Google Scholar]
- Sherman AM. Social relations and depressive symptoms in older adults with knee osteoarthritis. [Research Support, U.S. Gov’t, P.H.S.] Social Science & Medicine. 2003;56(2):247–257. doi: 10.1016/s0277-9536(02)00023-0. [DOI] [PubMed] [Google Scholar]
- Shih T, Fan X. Comparing response rates from web and mail surveys: a meta-analysis. Field Methods. 2008;20(3):249–271. [Google Scholar]
- Silliman RA, Bhatti S, Khan A, Dukes KA, Sullivan LM. The care of older persons with diabetes mellitus: families and primary care physicians. Journal of the American Geriatrics Society. 1996;44(11):1314–1321. doi: 10.1111/j.1532-5415.1996.tb01401.x. [DOI] [PubMed] [Google Scholar]
- Tomaka J, Thompson S, Palacios R. The relation of social isolation, loneliness, and social support to disease outcomes among the elderly. Journal of Aging & Health. 2006;18(3):359–384. doi: 10.1177/0898264305280993. [DOI] [PubMed] [Google Scholar]
- Trevino DB, Young EH, Groff J, Jono RT. The association between marital adjustment and compliance with antihypertension regimens. Journal of the American Board of Family Practice. 1990;3(1):17–25. [PubMed] [Google Scholar]
- Trief PM, Grant W, Elbert K, Weinstock RS. Family environment, glycemic control, and the psychosocial adaptation of adults with diabetes. Diabetes Care. 1998;21(2):241–245. doi: 10.2337/diacare.21.2.241. [DOI] [PubMed] [Google Scholar]
- Trief PM, Himes CL, Orendorff R, Weinstock RS. The marital relationship and psychosocial adaptation and glycemic control of individuals with diabetes. Diabetes Care. 2001;24(8):1384–1389. doi: 10.2337/diacare.24.8.1384. [DOI] [PubMed] [Google Scholar]
- Trief PM, Ploutz-Snyder R, Britton KD, Weinstock RS. The relationship between marital quality and adherence to the diabetes care regimen. Annals of Behavioral Medicine. 2004;27(3):148–154. doi: 10.1207/s15324796abm2703_2. [DOI] [PubMed] [Google Scholar]
- Trief PM, Sandberg J, Graff K, Castronova N, Yoon M, Weinstock RS. Describing Support: A Qualitative Study of Couples Living with Diabetes. Families, Systems & Health. 2003;21(1):57–67. [Google Scholar]
- Trief PM, Wade MJ, Britton KD, Weinstock RS. A prospective analysis of marital relationship factors and quality of life in diabetes. Diabetes Care. 2002;25(7):1154–1158. doi: 10.2337/diacare.25.7.1154. [DOI] [PubMed] [Google Scholar]
- Uchino B. Social Support and Physical Health: Understanding the Health Consequences of Relationships. Yale University; New Haven: 2004. [Google Scholar]
- Umberson D. Family status and health behaviors: social control as a dimension of social integration. Journal of Health & Social Behavior. 1987;28(3):306–319. [PubMed] [Google Scholar]
- von Elm E, Altman DG, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke JP. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Journal of Clinical Epidemiology. 2008;61(4):344–349. doi: 10.1016/j.jclinepi.2007.11.008. [DOI] [PubMed] [Google Scholar]
- Waltz M, Kriegel W, van’t pad Bosch P. The social environment and health in rheumatoid arthritis: marital quality predicts individual variability in pain severity. Arthritis Care and Research. 1998;11(5):356–374. doi: 10.1002/art.1790110507. [DOI] [PubMed] [Google Scholar]
- Wearden AJ, Tarrier N, Barrowclough C, Zastowny TR, Rahill AA. A review of expressed emotion research in health care. Clinical Psychology Review. 2000;20(5):633–666. doi: 10.1016/s0272-7358(99)00008-2. [DOI] [PubMed] [Google Scholar]
- Westlake C, Dracup K, Creaser J, Livingston N, Heywood JT, Huiskes BL, et al. Correlates of health-related quality of life in patients with heart failure. Heart & Lung. 2002;31(2):85–93. doi: 10.1067/mhl.2002.122839. [DOI] [PubMed] [Google Scholar]
- Williams GC, Rodin GC, Ryan RM, Grolnick WS, Deci EL. Autonomous regulation and long-term medication adherence in adult outpatients. Health Psychology. 1998;17(3):269–276. doi: 10.1037//0278-6133.17.3.269. [DOI] [PubMed] [Google Scholar]
- Williamson D, Robinson ME, Melamed B. Pain behavior, spouse responsiveness, and marital satisfaction in patients with rheumatoid arthritis. Behavior Modification. 1997;21(1):97–118. doi: 10.1177/01454455970211006. [DOI] [PubMed] [Google Scholar]
- Wing RR, Marcus MD, Epstein LH, Jawad A. A “family-based” approach to the treatment of obese type II diabetic patients. Journal of Consulting & Clinical Psychology. 1991;59(1):156–162. doi: 10.1037//0022-006x.59.1.156. [DOI] [PubMed] [Google Scholar]
- Zhang X, Norris SL, Gregg EW, Beckles G. Social support and mortality among older persons with diabetes. Diabetes Educator. 2007;33(2):273–281. doi: 10.1177/0145721707299265. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.