Abstract
Background
Few published data are available on the benefits of aspirin use in patients with unstable angina (UA).
Hypothesis
Aspirin use carries a mortality benefit in a population‐based cohort of patients presenting with UA.
Methods
All residents of Olmsted County, Minnesota presenting to local emergency departments with acute chest pain from January 1985 through December 1992 having symptoms consistent with UA were identified through medical records. A total of 1628 patients were identified with UA and were stratified by aspirin use in‐hospital and at discharge. Cardiovascular mortality and nonfatal myocardial infarction and stroke were assessed over a median of 7.5 years follow‐up and all‐cause mortality data over a median of 16.7 years. The mean age of patients with UA was 65 years, and 60% were men.
Results
After a median of 7.5 years follow‐up, all‐cause and cardiovascular‐mortality rates were lower among patients prescribed versus not prescribed aspirin on discharge. There were 949 postdischarge deaths over the median follow‐up of 16.7 years. After multivariable adjustment, aspirin use at discharge was associated with a lower long‐term mortality (hazard ratio 0.78; 95% confidence interval, 0.65–0.93).
Conclusions
Aspirin use at hospital discharge following UA is associated with a reduction in long‐term mortality. This long‐term study extends prior trial results from select populations to a population‐based cohort. Copyright © 2010 Wiley Periodicals, Inc.
This study was made possible by the Rochester Epidemiology Project (grant no. R01‐AR30582 from the National Institute of Arthritis and Musculoskeletal and Skin Diseases). The authors have no other funding, financial relationships, or conflicts of interest to disclose.
Introduction
Cardiovascular disease is the leading cause of death worldwide, accounting for more than 900 000 deaths annually in the United States alone. Platelets, platelet products, and clotting factors play a crucial role in the occurrence of the majority of occlusive vascular events including myocardial infarction (MI) and ischemic stroke. Aspirin irreversibly inhibits cyclooxygenase, which in turn blocks thromboxane production, a potent vasoconstrictor and promoter of platelet aggregation.1,2 Following a number of pivotal trials that established the benefits of aspirin in acute coronary syndromes (ACS),3 successive American Heart Association/American College of Cardiology guidelines on non‐ST elevation (NSTE) ACS have recommended the use of aspirin in‐hospital and following discharge in the management of patients presenting with unstable angina (UA).4
Little is known as to whether aspirin being prescribed to unselected patients presenting with chest pain has long‐term benefits in reducing cardiovascular events and mortality. Although randomized controlled trials are the gold standard for quantifying the benefit of treatment, they often include a select subset of patients.5,6 Therefore, it is often useful to confirm results of randomized trials in unselected patients who represent a real‐life scenario. Few published data are available on the benefits of aspirin use in patients with UA. Therefore, the current study was conducted to examine postdischarge follow‐up of a large unselected cohort of patients presenting to the emergency room with chest pain during a period when the routine use of aspirin therapy was instituted. Consequently, based on different practices for prescribing aspirin during that era, the efficacy of aspirin use in patients with UA in reducing mortality could be studied.
Methods
Patient Population
Using written screening logs, we retrospectively identified all residents of Olmsted County, Minnesota presenting to one of the county's 3 emergency rooms with acute chest pain during the period January 1, 1985 through December 31, 1992. The complete medical records of the screened population were reviewed by an experienced nurse abstractor, who identified residents presenting with their first episode of acute chest pain, consistent with an unstable coronary syndrome. Patients were excluded if they had ST segment elevation on their qualifying electrocardiogram (elevation ≥ 1 mm in 2 or more leads), or a definitive alternate etiology for their chest pain, including pulmonary embolism, pneumonia, musculoskeletal pain, pericarditis, and dissecting aortic aneurysm. A total of 1665 patients presenting with acute chest pain with UA were identified. Thirty‐seven patients were excluded at this time for refusal to allow use of their records for research purposes, resulting in a sample size of 1628 patients for analysis.
Data Collection
For all eligible patients, the medical record was abstracted through the resources of the Rochester Epidemiology Project, which allowed capture of the healthcare experience, including outpatient care, of all residents of Olmsted County, Minnesota. The Olmsted County Health Care Utilization and Expenditures Database, which is linked to the Rochester Epidemiology Project, contains detailed line‐item information on all health services utilized and expenditures incurred by every member of the population for as long as they remain a resident in the county. The qualifying electrocardiogram (ECG) was interpreted by a staff cardiologist and verified by 1 of the study physicians.
Study Outcomes
The primary outcomes for the current study were all‐cause and cardiovascular mortality (defined as death secondary to MI, cardiogenic shock, ventricular arrhythmias, or death from any other cardiac etiology) and MI and stroke. Events were identified through review of the medical records, and MI (fatal and nonfatal) was defined by either serologic or ECG criteria, and in cases where an old infarct was noted on ECG, this was not considered an MI unless the patient had 2 or more of the following criteria: (1) symptoms, (2) ECG changes, and (3) cardiac enzymes rise. Stroke (fatal and nonfatal) or cerebrovascular accident was defined as a loss of neurological function caused by an ischemic event persisting > 24 hours or leaving residual signs. MI and stroke were assessed through December 1998 for the 1589 patients who survived their initial hospitalization for UA. Death dates were obtained through the Minnesota electronic death certificates, Minnesota death tapes, Olmsted County electronic death certificates, and medical records. The last known alive date was obtained from patient records.
Statistical Analysis
Baseline characteristics of the study population were calculated as means and standard deviations for continuous variables and compared between the 4 aspirin groups (no aspirin in‐hospital or at discharge, aspirin in‐hospital only, aspirin at discharge only, and aspirin in‐hospital and at discharge) using analysis of variance. Categorical data were summarized as frequencies (percentages) and compared with Pearson's χ2 test. Mortality rates at 30‐day follow‐up were calculated by in‐hospital use of aspirin. Cumulative survival was calculated for patients discharged on aspirin and not on aspirin using the Kaplan‐Meier method and compared with the log‐rank test. For all time‐to‐event analyses, follow‐up began at hospital discharge and included only those patients who survived to discharge, because in‐hospital death precludes discharge aspirin use. Cox proportional hazard models were used to calculate the adjusted hazard ratios (HR) associated with discharge aspirin use. Initial models included adjustment for age and gender. A subsequent model included additional adjustment for diabetes, hypertension, systolic blood pressure, total cholesterol, family history, prior aspirin use, prior revascularization, prior MI or coronary artery disease, ST‐segment depression ≥ 1 mm, extra‐cardiac vascular disease, pulmonary edema related to ischemia, and a history of smoking. All data analyses were conducted using SAS 9.1 (SAS Inc., Cary, NC).
Results
Baseline Characteristics
The mean age of the cohort presenting with acute chest pain and identified with UA was 65 years; 60% were men, whereas 16% had diabetes mellitus and 50% had hypertension (Table 1). Aspirin was given both in the hospital and at discharge for 41% of patients, in‐hospital only for 12% of patients, at discharge only for 5%, and not at all for 42% of patients. Aspirin was more likely to be prescribed in‐hospital, at discharge, or both, in men and patients with diabetes, family history of heart disease, a history of prior revascularization, a history of prior MI or coronary artery disease, ST‐segment depression on ECG, and a higher Agency for Health Care Policy and Research (AHCPR) risk score. The patients who were discharged on aspirin (whether or not they received aspirin in‐hospital) had higher systolic blood pressure and total cholesterol levels.
Table 1.
Baseline Characteristics of Patients by Aspirin In‐hospital and Discharge Status
| Variable | No Aspirin at Discharge | Aspirin at Discharge | Overall P Value | Discharge Aspirin P Value | In‐Hospital ASA P Value | ||
|---|---|---|---|---|---|---|---|
| No Aspirin in Hospital (n =679) | Aspirin in Hospital (n =197) | No Aspirin in Hospital (n =83) | Aspirin in Hospital (n =669) | ||||
| Age, y | 65.0 (15.8) | 64.4 (15.4) | 63.9 (12.8) | 65.6 (13.1) | 0.61 | 0.44 | 0.51 |
| Male gender | 360 (53%) | 113 (57%) | 57 (69%) | 441 (66%) | <0.001 | <0.001 | <0.001 |
| Diabetes | 85 (13%) | 39 (20%) | 11 (13%) | 133 (20%) | 0.01 | 0.01 | <0.001 |
| Hypertension | 315 (46%) | 103 (52%) | 36 (43%) | 355 (53%) | 0.05 | 0.09 | 0.01 |
| SBP, mm Hg | 150.5 (29.6) | 151.9 (27.8) | 157.5 (30.7) | 155.3 (26.2) | 0.01 | <0.001 | 0.02 |
| Cholesterol (highest prior to admission), mg/dL | 261.2 (63.4) | 255.3 (57.0) | 267.5 (49.8) | 272.3 (63.5) | <0.001 | <0.001 | 0.04 |
| Family history | 160 (24%) | 51 (26%) | 25 (30%) | 206 (31%) | 0.02 | 0.01 | 0.01 |
| Prior aspirin | 34 (5%) | 47 (24%) | 27 (33%) | 217 (32%) | <0.001 | <0.001 | <0.001 |
| Prior revascularization | 47 (7%) | 25 (13%) | 19 (23%) | 130 (19%) | <0.001 | <0.001 | <0.001 |
| History of prior MI or CAD | 314 (46%) | 89 (45%) | 49 (59%) | 358 (54%) | 0.01 | 0.01 | 0.11 |
| ST‐segment depression ≥ 1 mm | 41 (6%) | 27 (14%) | 4 (5%) | 67 (10%) | 0.01 | 0.23 | <0.001 |
| Extracardiac vascular disease | 30 (4%) | 10 (5%) | 3 (4%) | 37 (6%) | 0.75 | 0.48 | 0.31 |
| Pulmonary edema, related to ischemia | 45 (7%) | 16 (8%) | 4 (5%) | 45 (7%) | 0.78 | 0.72 | 0.62 |
| Ever smoked | 382 (56%) | 115 (59%) | 52 (63%) | 411 (61%) | 0.25 | 0.05 | 0.12 |
| AHCPR risk category | 0.04 | 0.05 | 0.01 | ||||
| High risk | 148 (22%) | 53 (27%) | 18 (22%) | 143 (21%) | |||
| Inter risk | 447 (66%) | 126 (64%) | 58 (70%) | 504 (75%) | |||
| Low risk | 84 (12%) | 18 (9%) | 7 (8%) | 22 (3%) | |||
Abbreviations: AHCPR, Agency for Health Care Policy and Research; ASA, aspirin; CAD, coronary artery disease; MI, myocardial infarction; SBP, systolic blood pressure. Numbers in table represent mean (standard deviation) or no (%)
Short‐Term Follow‐up
A trend toward lower 30‐day all‐cause and cardiovascular mortality was present for patients who received aspirin compared to those who did not receive aspirin in‐hospital (Table 2). The differences in MI or stroke rates between the 2 groups was small and not statistically significant.
Table 2.
Cardiovascular Events at 30 Days in Patients With and Without In‐Hospital Aspirin Treatment Who Survived to Hospital Discharge
| Variable | Total (n =1589) | No In‐Hospital Aspirin (n =738) | In‐Hospital Aspirin (n =851) | P Value |
|---|---|---|---|---|
| All‐cause mortality | 18 (1.1) | 12 (1.6) | 6 (0.7) | 0.15 |
| Cardiovascular mortality | 16 (1.0) | 11 (1.4) | 5 (0.6) | 0.15 |
| Myocardial infarction | 22 (1.4) | 9 (1.2) | 13 (1.5) | 0.57 |
| Stroke | 6 (0.4) | 3 (0.4) | 3 (0.4) | 0.75 |
| Death/ myocardial infarction/ stroke | 39 (2.5) | 20 (2.7) | 19 (2.2) | 0.15 |
Numbers in table represent no. (%)
Aspirin Use and Post‐discharge Mortality at Long‐Term Follow‐Up
Over a median follow‐up of 7.5 years, all‐cause and cardiovascular‐mortality rates were lower among patients discharged versus not discharged on aspirin (Table 3). These associations remained present after age, race, sex, and multivariable adjustment. Although MI and stroke rates were not significantly different for individuals discharged on and not on aspirin, the composite outcome of death, MI, and stroke was lower among patients receiving aspirin on discharge (Figure 1).
Table 3.
Cardiovascular Events at 7.5 Years Median Follow‐up With and Without Aspirin Treatment at Discharge
| Event | Incidence (95% CI) Per 1000 Person‐Years | Adjusted Hazard Ratioa | Adjusted Hazard Ratiob | |||
|---|---|---|---|---|---|---|
| No Discharge Aspirin | Discharge Aspirin | HR (95% CI) | P Value | HR (95%CI) | P Value | |
| All‐cause mortality | 67 (60, 75) | 42 (37, 49) | 0.65 (0.55, 0.78) | <0.001 | 0.61 (0.48, 0.78) | <0.001 |
| Cardiovascular mortality | 36 (31, 42) | 19 (15, 24) | 0.55 (0.39, 0.78) | <0.001 | 0.46 (0.33, 0.65) | <0.001 |
| Myocardial infarction | 31 (27, 37) | 28 (23, 33) | 0.89 (0.70, 1.13) | 0.33 | 0.73 (0.52, 1.02) | 0.07 |
| Stroke | 16 (13, 20) | 16 (12, 20) | 1.01 (0.73, 1.40) | 0.95 | 0.80 (0.51, 1.27) | 0.35 |
| Death/myocardial infarction/stroke | 92 (83, 101) | 70 (63, 79) | 0.78 (0.67, 0.91) | 0.01 | 0.66 (0.53, 0.81) | <0.001 |
Abbreviations: CI, confidence interval; HR, hazard ratio.
Numbers in table represent no. (95% CI).
Discharge aspirin vs. no discharge aspirin, includes adjustment for age and gender.
Discharge aspirin vs nondischarge aspirin, includes adjustment for age, gender, diabetes, hypertension, elevated systolic blood pressure, hypercholesterolemia, family history of heart disease, prior aspirin use, prior revascularization, prior myocardial infarction or history of coronary artery disease, ST‐segment depression ≥ 1 mm on electrocardiogram, extracardiac vascular disease, pulmonary edema related to ischemia, and ever smoked.
Figure 1.
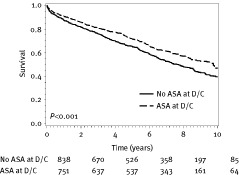
Post‐discharge survival free of the composite outcome of death, myocardial infarction, or stroke by aspirin discharge status. ASA, aspirin; D/C, discharge.
Overall, there were 949 postdischarge deaths over a median of 16.7 years of follow‐up. Cumulative survival is shown by whether patients were discharged on aspirin or not in Figure 2A. Overall, survival was not significantly different for patients who were and were not discharged on aspirin (P = 0.16). However, after age, race, and sex as well as multivariable adjustment, aspirin use at discharge was associated with a lower mortality rate over a median follow‐up of 16.7 years (HR 0.78; 95% confidence interval, 0.65–0.93). Although a beneficial effect of aspirin on survival was present for patients in the high‐risk AHCPR group (P = 0.004), differences were not significant for patients in the low and medium risk AHCPR groups (Figure 2B).
Figure 2.

(A) Post‐discharge mortality‐free survival by aspirin discharge status. (B) Post‐discharge mortality‐free survival by Agency for Health Care Policy and Research risk group depending and aspirin discharge status. ASA, aspirin; D/C, discharge.
Discussion
Aspirin is currently indicated for the inpatient management of acute cardiovascular thrombotic events, and is the standard of care in secondary cardiovascular protection as long‐term therapy. The current analysis evaluated consecutive patients who presented to the 3 emergency departments in Olmsted County, Minnesota with UA and found that discharge aspirin use was associated with a long‐term reduction in all‐cause mortality in patients presenting with UA.
Early clinical trials provided conflicting results regarding the benefits of aspirin in reducing coronary deaths in patients with an ACS.7 The Aspirin Myocardial Infarction Study evaluated the antiplatelet properties of aspirin in patients who survived an acute myocardial infarction (AMI) in a randomized, double‐blind, placebo‐controlled study and showed no mortality benefit for aspirin at 1 year.8 However, around the same time the Persantine and Aspirin Reinfarction Study randomized 2026 patients recovering from AMI into placebo, aspirin, and Persantine plus aspirin.9 Over the 41‐month observation period, aspirin significantly reduced mortality, and when administered within 6 months of the acute event it provided greater cardiovascular protection. Subsequent smaller randomized controlled trials reinforced the efficacy of aspirin in reducing overall cardiovascular death in patients with a history of cerebrovascular disease, MI, and UA.10
In 2002, the Antithrombotic Trialists' Collaboration (ATC) reviewed the effect of antiplatelet therapy, mostly aspirin, in 12 trials of over 18 000 patients with a NSTE ACS.11 Antiplatelet therapy reduced the combined outcome of any serious vascular event by one quarter, nonfatal MI outcomes by one third, nonfatal stroke by one quarter, and vascular mortality by one sixth. The degree to which aspirin reduced the risk of MI over 7.6 years of follow‐up in our study was similar to the findings of ATC. ATC did not show, however, any difference for aspirin in all‐cause mortality. Interestingly, prior aspirin use was found to be a risk factor for a worse outcome in the TIMI risk score analysis in NSTE ACS12 and in other nonrandomized comparisons.13,14 The association likely reflects higher rates of aspirin use among patients with more severe underlying vascular disease, and thus a worse prognosis, rather than a harmful effect of aspirin.
The current study demonstrates the long‐term benefits of aspirin use for patients presenting with UA in a community‐based setting. The current analysis was designed to evaluate a geographically defined cohort free of selection bias presenting with UA, and determine long‐term mortality effects associated with aspirin use. The inclusion period spanned an era when aspirin was not considered the standard of care in the treatment of UA or in secondary prophylaxis. All‐cause mortality was significantly decreased over a median follow‐up of 16.7 years in patients receiving aspirin on discharge, which was not found to be different in the ATC meta‐analysis. This beneficial effect of aspirin at long‐term follow‐up was driven by the high‐risk AHCPR group, likely due to the largest effect size in this high‐risk group. This discrepancy with the ATC meta‐analysis might be explained by the longer median follow‐up provided in our study, as there was a trend toward improved mortality in ATC. The study has several important historical and clinical implications. Today, aspirin is universally accepted as providing mortality benefit in the management of patients presenting with UA; consequently, long‐term placebo‐controlled studies are not ethically possible. The current study was able to compare populations receiving aspirin to no antiplatelet treatment, and assess long‐term all‐cause mortality. As such, the current study extends findings from previous research such as the ATC meta‐analysis, but with a longer follow‐up.
The Olmsted County chest pain study is unique in that it was able to assess mortality benefits over a long period of follow‐up for patients with UA. The benefit of aspirin therapy that emerged at 30 days persisted out to > 15 years. This is concordant with the findings of the International Study of Infarct Survival 2, a randomized placebo‐controlled trial in which patients with suspected acute MI were treated with aspirin for 35 days. The survival benefit was realized by 1 month and persisted for 10 years.15
Large population‐based studies such as one from Scotland including over 100 000 patients presenting to the emergency department with stable and unstable angina have suggested that the long‐term prognosis for patients presenting with angina is almost as poor as for patients presenting with an MI.16 This would argue for a strict implementation of prescribing aspirin on discharge for patients with any form of ACS, but it is concerning that even in the current era, not all patients presenting with ACS are discharged on aspirin.17 The Maximal Individual Therapy in Acute Myocardial Infarction registry18 provided evidence that 10% of patients presenting with acute MI did not receive aspirin, which resulted in a 10% increase in mortality. Krumholz et alalso noted that 24% of elderly patients were discharged without aspirin after ACS, and this group had a higher 6‐month mortality than those treated with aspirin.19
There are several limitations to the current study. First, there might be unmeasured characteristics in patients who were discharged on aspirin that might have influenced clinical decisions about whether they received aspirin or not. Second, without interim data we are unable to determine if patients who were initially not discharged on aspirin ever received aspirin afterward or if patients discharged on aspirin continued therapy. If patients not discharged on aspirin subsequently initiated therapy the true benefits of aspirin would be larger than we report. Also, if patients discharged on aspirin were noncompliant, there would likely be an underestimation of the true benefits of aspirin. The major strengths of this study include the enrollment of consecutive and unselected patients and follow‐up over a long period of time with strict events assessment.
Conclusion
Data from the current study provide evidence on the beneficial effect of aspirin use in reducing in‐hospital and long‐term mortality in unselected patients with UA. Specifically, the benefits of aspirin at hospital discharge extended through a median 16.7 years of follow‐up. The current study is unique in that it followed a large cohort for an extended duration including a period of time where aspirin was not the standard of care.
References
- 1. Vane JR, Botting RM. The mechanism of action of aspirin. Thromb Res 2003; 110: 255–258. [DOI] [PubMed] [Google Scholar]
- 2. Burch JW, Stanford N, Majerus PW. Inhibition of platelet prostaglandin synthetase by oral aspirin. J Clin Invest 1978;61: 314–319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Risk of myocardial infarction and death during treatment with low dose aspirin and intravenous heparin in men with unstable coronary artery disease. The RISC Group. Lancet 1990; 336: 827–830. [PubMed] [Google Scholar]
- 4. Anderson JL, Adams CD, Antman EM, et al. ACC/AHA 2007 guidelines for the management of patients with unstable angina/non ST‐elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 2002 Guidelines for the Management of Patients With Unstable Angina/Non ST‐Elevation Myocardial Infarction): developed in collaboration with the American College of Emergency Physicians, the Society for Cardiovascular Angiography and Interventions, and the Society of Thoracic Surgeons: endorsed by the American Association of Cardiovascular and Pulmonary Rehabilitation and the Society for Academic Emergency Medicine. Circulation 2007; 116: e148–e304. [DOI] [PubMed] [Google Scholar]
- 5. Grapow MT, von Wattenwyl R, Guller U, et al. Randomized controlled trials do not reflect reality: real‐world analyses are critical for treatment guidelines! J Thorac Cardiovasc Surg 2006; 132: 5–7. [DOI] [PubMed] [Google Scholar]
- 6. Willenheimer R. Statistical significance versus clinical relevance in cardiovascular medicine. Prog Cardiovasc Dis 2001; 44: 155–167. [DOI] [PubMed] [Google Scholar]
- 7. Hennekens CH, Karlson LK, Rosner B. A case‐control study of regular aspirin use and coronary deaths. Circulation 1978; 58: 35–38. [DOI] [PubMed] [Google Scholar]
- 8. The aspirin myocardial infarction study: final results. The Aspirin Myocardial Infarction Study research group. Circulation 1980; 62(6 pt 2): V79–V84. [PubMed] [Google Scholar]
- 9. Persantine and aspirin in coronary heart disease. The Persantine‐Aspirin Reinfarction Study Research Group. Circulation 1980; 62: 449–461. [DOI] [PubMed] [Google Scholar]
- 10. Hennekens CH, Buring JE, Sandercock P, et al. Aspirin and other antiplatelet agents in the secondary and primary prevention of cardiovascular disease. Circulation 1989; 80: 749–756. [DOI] [PubMed] [Google Scholar]
- 11. Collaborative meta‐analysis of randomised trials of antiplatelet therapy for prevention of death, myocardial infarction, and stroke in high risk patients. BMJ 2002; 324: 71–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Antman EM, Cohen M, Bernink PJ, et al. The TIMI risk score for unstable angina/non‐ST elevation MI: a method for prognostication and therapeutic decision making. JAMA 2000; 284: 835–842. [DOI] [PubMed] [Google Scholar]
- 13. Borzak S, Cannon CP, Kraft PL, et al. Effects of prior aspirin and anti‐ischemic therapy on outcome of patients with unstable angina. TIMI 7 Investigators. Thrombin Inhibition in Myocardial Ischemia. Am J Cardiol 1998; 81: 678–681. [DOI] [PubMed] [Google Scholar]
- 14. Alexander JH, Harrington RA, Tuttle RH, et al. Prior aspirin use predicts worse outcomes in patients with non‐ST‐elevation acute coronary syndromes. PURSUIT Investigators. Platelet IIb/IIIa in Unstable angina: Receptor Suppression Using Integrilin Therapy. Am J Cardiol 1999; 83: 1147–1151. [DOI] [PubMed] [Google Scholar]
- 15. Baigent C, Collins R, Appleby P, et al. ISIS‐2: 10 year survival among patients with suspected acute myocardial infarction in randomised comparison of intravenous streptokinase, oral aspirin, both, or neither. The ISIS‐2 (Second International Study of Infarct Survival) Collaborative Group. BMJ 1998; 316: 1337–1343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Capewell S, Murphy NF, MacIntyre K, et al. Short‐term and long‐term outcomes in 133,429 emergency patients admitted with angina or myocardial infarction in Scotland, 1990‐2000: population‐based cohort study. Heart 2006; 92: 1563–1570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Simpson E, Beck C, Richard H, et al. Drug prescriptions after acute myocardial infarction: dosage, compliance, and persistence. Am Heart J 2003; 145: 438–444. [DOI] [PubMed] [Google Scholar]
- 18. Frilling B, Schiele R, Gitt AK, et al. Too little aspirin for secondary prevention after acute myocardial infarction in patients at high risk for cardiovascular events: results from the MITRA study. Am Heart J 2004; 148: 306–311. [DOI] [PubMed] [Google Scholar]
- 19. Krumholz HM, Radford MJ, Ellerbeck EF, et al. Aspirin for secondary prevention after acute myocardial infarction in the elderly: prescribed use and outcomes. Ann Intern Med 1996; 124: 292–298. [DOI] [PubMed] [Google Scholar]


