Abstract
Background
The development of premature osteoarthritis after ACL reconstruction is significant cause of morbidity in young, active individuals. Meniscal injuries are frequently noted at the time of reconstruction and the critical role of an intact meniscus in the prevention of osteoarthritis has been well documented. The purpose of this review is to evaluate the impact of meniscal status at the time of ACL reconstruction on the subsequent development of osteoarthritis as determined radiographically.
Methods
A systematic review of the literature was performed to identify studies publishing outcomes of ACL reconstructions with at least two years follow-up that included radiographs. These studies were narrowed, focusing on those which compared radiographic outcomes of at least two groups of patients based of meniscus status at the time of ACL reconstruction.
Results
Eleven studies met our inclusion and exclusion criteria. Patients who underwent partial meniscectomy at the time of ACL reconstruction were significantly more likely to develop radiographic evidence of osteoarthritis than those with normal menisci at 5–10 year follow-up. Comparison of patients who underwent meniscal repair with other groups revealed inconsistent findings. Virtually all patients who underwent complete meniscectomy at the time of ACL reconstruction exhibited radiographic evidence of osteoarthritis at follow-up.
Conclusions
The presence of meniscal injury requiring partial meniscectomy at the time of ACL reconstruction significantly increases osteoarthritis risk.
Level of Evidence
2 - Systematic review of retrospective prognostic studies and lesser quality prospective prognostic studies with consistent results
INTRODUCTION
ACL reconstruction utilizing modern techniques allows clinically stable ligament reconstruction while minimizing scarring and potential trauma to the knee joint.13, 40 Aggressive modern rehabilitation techniques reliably restore knee range of motion and quadriceps strength necessary for normal knee function.29, 46, 47 However, the development of premature arthritis following ACL reconstruction persists and continues to be the focus of significant basic science and clinical research.3, 16, 25, 39, 47
The critical biomechanical role of the meniscus in the knee has long been known and the development of osteoarthritis has been associated with meniscectomy.6, 23 Several authors have documented the influence meniscal injuries can have on outcome after ACL reconstruction.4, 27, 31, 32, 47, 50 The purpose of this manuscript is to perform a systematic review to address the following clinical question: What is the impact of meniscal status at the time of ACL reconstruction on the subsequent development of radiographic signs of osteoarthritis?
MATERIALS AND METHODS
Inclusions and Exclusion Criteria
Inclusion and exclusion criteria for this review are summarized in Table 1. Papers were included if they included descriptions of meniscal status at the time of primary ACL reconstruction with hamstring or patellar tendon autograft using arthroscopic or arthroscopic-assisted techniques. Follow-up was required to be at least two years consisting of radiographic quantification of the development of osteoarthritis broken down by meniscal status. Studies were excluded if they included skeletally immature patients, revision ACL reconstruction, allograft, concurrent non-meniscal procedures, reconstruction with grafts other than patellar tendon or hamstring, open procedures, or multi-ligament knee injuries.
Table 1.
Inclusion and Exclusion Criteria
| Inclusion Criteria | Exclusion Criteria |
|---|---|
| Primary ACL reconstruction | Revision ACL reconstruction |
| Contains description of meniscal status at the time of ACL reconstruction with at least two meniscal groups | Skeletally immature patients |
| Follow-up of at least 2 years | Performance of concurrent non-meniscal procedures |
| Radiographic evaluation of development of osteoarthritis at follow-up | Use of artificial ligaments or ligament augmentation devices |
| Breakdown of development of radiographic findings by meniscal status | Multi-ligament knee injuries |
| Arthroscopic, arthroscopic-assisted, or mini-open ligament reconstruction | Open procedures |
| Reconstruction using patellar tendon or hamstring autograft | Primary ligament repair or reconstruction with graft other than patellar tendon or hamstring |
| Reconstruction using allograft |
Literature Review
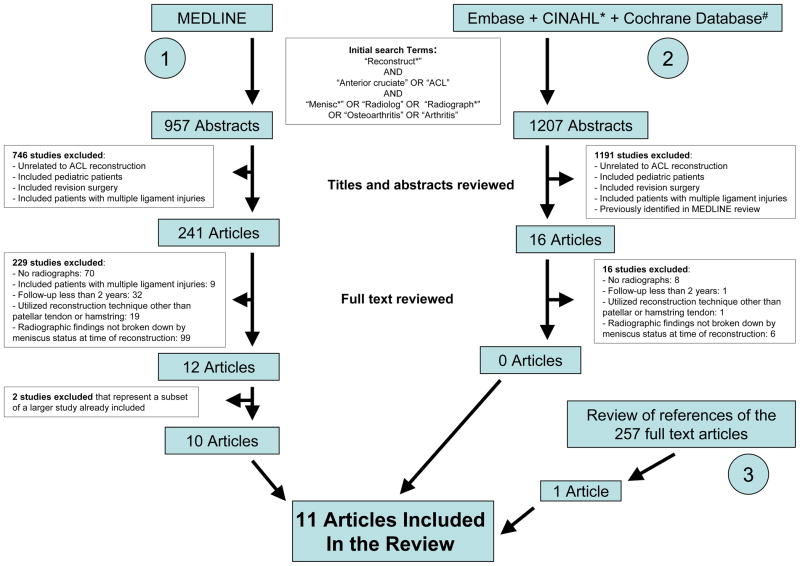
The literature search is summarized in Figure 1. A MEDLINE literature search was preformed to identify all English language publications from January 1, 1966 through January 1, 2007 addressing the influence of meniscal status on the development of osteoarthritis in humans undergoing ACL reconstruction. A search for articles containing the term “reconstruct*” as well as either “anterior cruciate” or “ACL” yielded 2805 results.# These results were further focused by requiring that the citation also contain one of the follow terms: “menisc*,” “radiolog*,” “radiograph*, “osteoarthritis,” or “arthritis,” resulting in 957 publications. The title and abstract of these publications were reviewed and studies not related to ACL reconstruction were excluded. Additionally, studies in which the title and abstract indicated a reason for exclusion using the above criteria were excluded. Full text of the remaining 241 publications was obtained. These articles were reviewed and excluded for absence of radiographs (70 studies), inclusion of patients with multiple ligament injuries (9 studies), use of reconstruction methods other than arthroscopic or arthroscopic-assisted patellar tendon or hamstring tendon reconstruction (19 studies), follow-up of less than 2 years (32 studies), or absence of radiographic findings broken down by meniscal status at the time of repair (99 studies). Twelve studies met the inclusion and exclusion criteria.2, 4, 14, 17, 20, 40, 42–44, 47, 49, 50 Two of these studies43, 44 were excluded because they represented a subset of data from a larger study that was included in the analysis.47
Figure 1.
The search strategy of the systemic review is shown, including MEDLINE, Embase, CINAHL, and the Cochrane Central Registry of Controlled Trials, as well as a search of the references of all full-text articles. Eleven studies were identified for nclusion.
A search of the Embase database was then performed utilizing the same search strategy. The title and abstracts of the resulting 950 studies were reviewed and excluded if they were previously identified in the MEDLINE search, were unrelated to ACL reconstruction, or met one of the above exclusion criteria. Full text of the remaining 16 articles was obtained. All were then excluded from the study based on lack of radiographs (8 studies), use of reconstruction methods other than arthroscopic or arthroscopic-assisted patellar tendon or hamstring tendon reconstruction (1 study), follow-up of less than 2 years (1 study), or absence of radiographic findings broken down by meniscal status at the time of repair (6 studies).
Searches of the Cochrane Central Register of Controlled Trials and the Cumulative Index to Nursing and Allied Health Literature (CINAHL) utilizing the same search criteria yielded 56 and 201 studies respectively. The search identified several studies already included in this review but no new studies meeting criteria were identified. Exhaustive review of the references of all full text articles was performed to identify additional papers meeting inclusion and exclusion criteria for this study. One additional study not previously identified was obtained and included in the study.37 Data was extracted from these eleven papers by two authors independently to ensure accuracy. Discrepancies were resolved by discussion until a consensus was reached.
Statistics
Data were analyzed by calculating the risk of developing radiographic signs of osteoarthritis for each treatment group in the included studies. A Fisher’s exact test was used to compare the frequency of these changes between patient groups. Risk difference was calculated by subtracting the risk of developing changes in one group from the risk of developing these changes in another. Risk ratios were calculated by dividing the risk of developing changes in one group by the risk of developing these changes in another. Confidence intervals were calculated for both risk differences and risk ratios. All statistical calculations were performed using Stata (Statacorp, College Station, TX).
RESULTS
Demographics
Demographics of each study are shown in Table 2. The majority of the publications are retrospective prognostic studies (Level 2 evidence) designed after treatment was provided to evaluate the impact of meniscus status on the later development of osteoarthritis. The exception is the 2002 study by Wu et al, which was prospectively designed specifically to address this question. However, follow-up of less than 80 % qualifies the Wu study as level 2 evidence. Mean patient age at the time of reconstruction is generally consistent in the studies and ranges from 23–31 years. All studies include a majority of males. Most of the studies include of majority of patients with chronic ACL tears defined by either the time interval from injury to surgery or by the occurrence of episodes of giving way prior to reconstruction. The study by Hart et al included only patients within 6 months of injury. Articular cartilage status at the time of ACL reconstruction is described in eight of the eleven studies. Five studies exclude patients with articular cartilage injury defined as Outerbridge score greater than 2.4, 14, 17, 37, 40
Table 2.
Patient Demographics
| Author | Journal | Year | Level | Patient Age Mean (range) | Percent male | Acute v Chronic | Method of Reconstruction | Initial Cohort | Final Clinical Cohort | Final Radiograph Cohort | Articular Cartilage Status Given |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Salmon | AJSM | 2006 | 2 | 27 | 70 % | 47 % > 3 mos |
Arthroscopic BTB | 67 | 49 (73 %) | 43 (64 %) | Yes |
| Seon | International Orthopedics | 2006 | 2 | 30 (18–58) | 95 % | 72 % > 6 mos |
Arthroscopic BTB | 70* | 58 (83 %) | 58 (83 %) | No |
| Hart | JBJS-Br | 2005 | 2 | 28 (18–47) | 68 % | 0 % > 6 mos |
Arthroscopic BTB | 50† | 31 (62 %) | 31 (62 %) | Yes |
| Hertel | KSSTA | 2005 | 2 | 31 | 59 % | 48 % > 4 wks |
Mini-arthrotomy BTB | 155‡ | 95 (61 %) | 95 (61 %) | No |
| Giron | KSSTA | 2005 | 2 | 29 (17–53) | 79 % | 100 % > 30 days |
Arthroscopic Hamstrings | 46 | 43 (93 %) | 38 (83 %) | Yes |
| Wang | Chang Gung Medical Journal | 2004 | 2 | 31 (19–57) | 73 % | 100 % > 3 mos |
Arthroscopic BTB | 51§ | 43 (84 %) | 43 (84 %) | No |
| Wu | AJSM | 2002 | 2 | 24 (15–45) | 57 % | 73 % > 4 mos |
2 Incision Arthroscopic Assisted/Arthroscopic BTB | 103 | 63 (61 %) | 63 (61 %) | Yes |
| Patel | Arthroscopy | 2000 | 2 | 33 (18–53) | 75 % | 72 % > 6 mos |
Arthroscopic BTB | 44 | 32 (73 %) | 32 (73 %) | Yes |
| Shelbourne | AJSM | 2000 | 2 | 23 (12–53) | 73 % | 59 % Had eipsode of give-way |
Mini-arthrotomy BTB | 1231 | 921 (75%) | 482 (39%) | Yes |
| Aglietti | KSSTA | 1997 | 2 | 23 (15–40) | 81 % | 100 % > 3 mos |
2 Incision Arthroscopic Assisted BTB | 117| | 89 (76 %) | 77 (66 %) | No |
| Aglietti | CORR | 1994 | 1 | NRj | NR | 100 % > 3 mos |
2 Incision Arthroscopic Assisted BTB | 57 | 57 (100 %) | 57 (100 %) | Yes |
AJSM – American Journal of Sports Medicine
JBJS-Br – Journal of Bone and Joint Surgery – British Edition
KSSTA – Knee Surgery, Sports, Traumatology, and Arthroscopy
CORR – Clinical Orthopaedics and Related Research
Initial cohort was 80 patients – 10 patients with multiple ligament injuries were excluded
Initial cohort was 60 patients – 10 patients with articular cartilage damage were excluded
Initial cohort was 159 patients – 4 patients with PCL injury or fracture were excluded
Initial cohort was 52 patients – 1 patient who underwent osteochondral allograft treatment was excluded
Initial cohort was 146 patients – 29 patients with multiple injuries and those treated with older techniques were excluded
Surgical Technique
Only studies including ACL reconstructions using mini-open, arthroscopic-assisted, or endoscopic techniques were examined in this study. In all cases but one, the authors used the same technique for all reconstructions included in the study. Wu et al utilized the arthroscopic-assisted technique early in their study then changed to an all endoscopic technique. The studies all excluded patients that underwent concurrent surgical procedures other than chondroplasty and meniscal procedures.
Rehabilitation
Rehabilitation protocols are reported in 7 of 11 studies and are detailed in Table 3. Partial weight-bearing was generally allowed within the first 24 hours with Johma et al and Aglietti et al delaying until 3–4 weeks. Full weight-bearing was generally allowed at 4–8 weeks although Wu et al allowed full weight-bearing at 24 hours. Most authors required the use of a hinged knee brace until full weight-bearing. Giron et al did not employ bracing and Wang et al only braced patients who underwent meniscal repair.
Table 3.
Rehabilitation Protocol and Follow-up
| Author | Year | Time to Partial Weight-bearing | Time to Full Weight-bearing | Brace use | Years to follow-up Mean (Range) | Radiographs Obtained | Radiographic Classification System Utilized |
|---|---|---|---|---|---|---|---|
| Salmon | 2006 | 24 Hours | 4 weeks | 30–90 for 4 weeks | 13 | Stand AP Stand 30 PA Lateral Merchant |
IKDC System Grade B,C or D |
| Seon | 2006 | 24 Hours | 8 weeks | 30–90 for 8 weeks | 11.2 (8.6–14) | Stand AP Lateral |
Kellgren and Lawrence Grade ≥ 2 |
| Hart | 2005 | NR | NR | NR | 10 (9–13) | Stand AP Lateral Merchant |
Ahlback Grade ≥1 |
| Hertel | 2005 | NR | NR | NR | 10.7 (9.2–12) | Stand AP | IKDC System Grade B,C, or D |
| Giron | 2005 | Immediate | 3–5 weeks | None | 5 | Stand AP Lateral Merchant Notch |
IKDC System Grade B,C, or D |
| Wang | 2004 | Immediate | 4–6 weeks if meniscus repaired Immediatein others | 0–90 for 4–6 weeks if meniscus repaired None in others |
5.8 (3.8–7.2) | Stand AP Merchant |
Ahlback Grade ≥1 |
| Wu | 2002 | 24 Hours | 24 Hours | 0–90 for 4 weeks if meniscus repaired Hinged brace with full ROM for 4 weeks in others |
10.5 (9–13) | Stand PA Lateral |
Fairbank Grade ≥1 |
| Patel | 2000 | NR | NR | NR | 5.9 (5–8.5) | NR | Fairbank Grade ≥1 |
| Shelbourne | 2000 | NR | NR | NR | 7.6 (5–15) | Stand 45 PA Lateral Merchant |
IKDC System Grade B,C, or D |
| Aglietti | 1997 | 3 weeks | 8 weeks | 10–90 for 4–6 weeks | 7 (5.2–8.7) | Stand AP Lateral Merchant |
IKDC System Grade C or D |
| Aglietti | 1994 | NR | NR | NR | 4.5 (3–7.5) | Stand AP Stand 45 PA Lateral Merchant |
HSS Evaluation Score < 26 |
AP – Antero-posterior
PA – Postero-anterior
NR – Not Reported
Follow-up and Radiographic Evaluation
Mean follow up ranged from 4.5 to 13 years with an average of 8.3 years for all studies. Follow-up radiographs were generally obtained in greater than 60 % of patients from the initial cohorts, although the Patel (55 %) and Shelbourne (39 %) papers had much lower follow-up rates. All studies utilized standing AP or PA views when assessing joints for osteoarthritis. Some authors supplemented this view with lateral,2, 4, 14, 17, 24, 40, 42, 47, 50 notch,14 30 or 45 degree flexion,3, 24, 40, 47 or Merchant views.2, 4, 14, 17, 24, 40, 47, 49
The International Knee Documentation Committee (IKDC) rating system was most frequently used to assess joint degeneration radiographically.19 The Kellgren and Lawrence,28 Fairbank,11 and Hospital for Special Surgery48 rating scales were also utilized. The papers generally defined radiographic evidence of osteoarthritis as an IKDC score of B or worse, Kellgren and Lawrence score of 2 or worse, Ahlback score of I or worse, the presence of Fairbanks changes, or HSS score less than 26. Definitions utilized in each study are shown in Table 3. Joint space loss is a key metric in each of the classification systems. Rough correlation between the joint space losses using each classification systems is shown in Table 4. Because the numeric HSS system is based on joint space narrowing, cyst formation, sclerosis, and coronal plane angulation, a specific score cannot be given based on joint space loss alone.
Table 4.
Correlation of Joint Space Narrowing Across Radiographic Staging Systems
| Joint Space | International Knee Documentation Committee (IKDC) | Kellgren and Lawrence | Ahlback | Fairbank Changes |
|---|---|---|---|---|
| Normal | A | 1* | Absent | |
| Minimal Narrowing | B† | 2‡ | Absent | |
| Moderate Narrowing | C§ | 3| | I¶ | Present |
| Severe Narrowing | D# | 4** | II – V†† | Present |
Defined as doubtful narrowing
Defined as joint space greater than 4 mm
Defined as possible narrowing
Defined as joint space 2 – 4 mm
Defined as definite joint space narrowing
Defined as joint space < 3 mm
Defined as joint space < 2 mm
Defined as marked joint space narrowing
Defined as complete loss of joint space
Meniscus Status and Correlation with Radiographic Evidence of Osteoarthritis
Table 5 describes the articular cartilage status of the patients in each study by Outerbridge grade and correlates meniscal status with radiographic findings. Three studies compare radiographic evidence of osteoarthritis in patients with normal menisci to those with repaired menisci.2, 4, 20 The study by Hertel et al demonstrates a significant difference between the two groups while the two studies by Aglietti et al find no significant difference.
Table 5.
Radiographic Signs of Osteoarthritis by Meniscus Status at Reconstruction Documented Meniscal Status at the Time of ACL Reconstruction
| Author | Year | Articular Cartilage Outerbridge Grade at Reconstruction | Normal Menisci | Normal or Repaired Menisci | Repaired Menisci | Partial Meniscectomy | Partial or total Meniscectomy | Total Meniscectomy | Significance |
|---|---|---|---|---|---|---|---|---|---|
| Salmon | 2006 | 0–2 | 50 % | 87 % | p = 0.006 | ||||
| Seon | 2005 | NR | 20 % (5/25) | 60 % (20/33) | p = 0.003 | ||||
| Hart | 2005 | 0–2 | 13 % (2/15) | 44 % (7/16) | p = 0.11 | ||||
| Hertel | 2005 | NR | 5 % (1/20) | 43 % (6/14) | 48 % (14/29) | normal v repaired – p = 0.01 normal v partial -p = 0.01 repaired v partial – p = 0.5 |
|||
| Giron | 2005 | 0–2 | 18 % (3/22) | 31 % (6/16) | p = 0.08 | ||||
| Wang | 2004 | NR | 38 % (6/16) | 74 % (20/27) | p = 0.03 | ||||
| Wu | 2002 | 0–4 | 8 % (2/25) | 100 % (9/9) | p = 0.000001 | ||||
| Patel | 2000 | 0–2 | 9 % (1/11) | 100 % (13/13) | p = 0.00001 | ||||
| Shelbourne | 2000 | 0–4 | 12 % (28/235) | 38 % (78/247) | p = 0.003 | ||||
| Aglietti | 1997 | 0–4 | 9 % (2/23) | 7 % (1/15) | 35 % (7/20) | normal v repair – p = 1.0 normal v partial -p = 0.06 repair v partial - p = 0.1 |
|||
| Aglietti | 1994 | 0–2 | 10 % (2/20) | 28 % (5/18) | 58 % (11/19) | normal v repair – p = 0.2 normal v partial -p = 0.002 repair v partial - p = 0.1 |
NR – Not Reported
Two papers contain a comparison of results of patients who underwent total meniscectomy versus normal or repaired meniscus.40, 50 Both studies found a statistically significant increase in the percentage of patients with radiographic evidence of osteoarthritis in the total meniscectomy groups.
Two authors did not report radiographic data for patients who underwent total meniscectomy separately from those who underwent partial meniscectomy. Both papers did show significantly increased radiographic evidence of osteoarthritis in patients who underwent meniscectomy when compared with patients with normal42 or normal and/or repaired menisci.47
Six studies include comparison of radiographs of patients with normal menisci versus those who underwent partial meniscectomy.2, 4, 14, 17, 20, 37 These findings are outlined in Table 6. Three of the six studies found significantly more radiographic changes in the partial meniscectomy group, while the other three studies showed a trend toward more radiographic evidence of osteoarthritis in the partial meniscectomy group that did not reach statistical significance. The relative risk of developing radiographic changes with a partial meniscetomy (Figure 2) and the risk reduction associated with a normal meniscus (Figure 3) are presented along with 95 % confidence intervals.
Table 6.
Comparison of Radiographic Signs of Degeneration in Patients with Normal Menisci and those with Partial Meniscectomy Meniscus Status at ACL Reconstruction
| Author | Year | Years to follow-up Mean (Range) | Percent Follow-up | Normal menisci | Partial meniscectomy | Significance | Radiographic Classification System Utilized |
|---|---|---|---|---|---|---|---|
| Hart | 2005 | 10 (9–13) | 62 % | 13 % (2/15) | 44 % (7/16) | p = 0.11 | Ahlback Grade ≥ 1 |
| Hertel | 2005 | 10.7 (9.2–12) | 61 % | 5 % (1/20) | 48 % (14/29) | p = 0.001 | IKDC System Grade B,C, or D |
| Giron | 2005 | 5 | 83 % | 18 % (3/22) | 31 % (6/16) | p = 0.09 | IKDC System Grade B,C, or D |
| Patel | 2000 | 5.9 (5–8.5) | 73 % | 9 % (1/11) | 100 % (13/13) | p = 0.00001 | Fairbank Grade ≥ 1 |
| Aglietti | 1997 | 7 (5.2–8.7) | 66 % | 9 % (2/23) | 35 % (7/20) | p = 0.06 | IKDC System Grade C or D |
| Aglietti | 1994 | 4.5 (3–7.5) | 100 % | 10 % (2/20) | 58 % (11/19) | p = 0.02 | HSS Evaluation Score < 26 |
Figure 2.
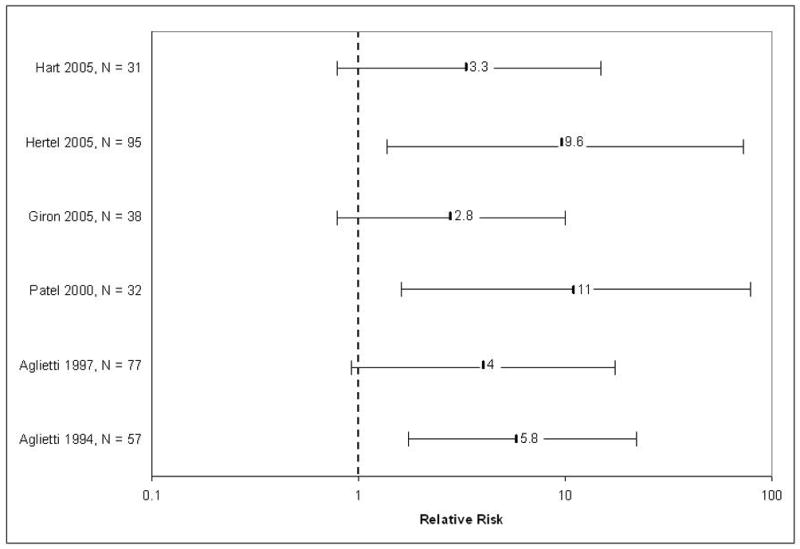
The relative risk of development of radiographic signs of osteoarthritis in patients with partial meniscectomy was calculated by dividing the percentage of patients with a partial meniscectomy at the time of ACL reconstruction who developed signs of osteoarthritis by the percentage of patients with a normal meniscus who developed signs of osteoarthritis.
Figure 3.
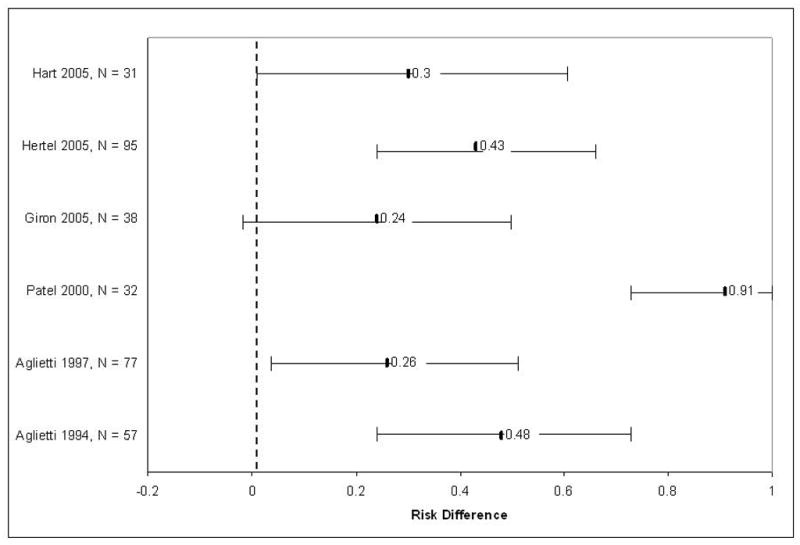
The absolute risk reduction of the development of osteoarthritis associated with a normal meniscus was calculated by subtracting the percentage of patients with a normal meniscus at the time of ACL reconstruction who developed signs of osteoarthritis from the percentage of patients with a partial meniscectomy who developed signs of osteoarthritis.
Comparison of patients with normal or repaired menisci showed higher rates of radiographic degeneration than the partial meniscectomy group in one paper.49 Repaired menisci were compared with partial meniscectomy in three studies. Significantly more degenerative change in the partial meniscectomy group was noted in two studies2, 4 while one author noted no difference.20
Analysis of Heterogeneity
An anaylsis of heterogeneity was performed on the six studies noted above to compare radiographic signs of osteoarthritis in patients with normal menisci with those that underwent partial meniscectomy.2, 4, 14, 17, 20, 37 Qualitatively, the studies used different outcome measures of radiographic systems to grade degenerative joint disease including HSS score, Faribank grade, IKDC grade, and Ahlback grade. Even studies which used the same system defined different cutoffs between cases of radiographic DJD and non-cases, with one study defining changes as an IKDC grade worse than A while others defined changes as an IKDC grade worse than B. Quantitatively, we evaluated the null hypothesis that the findings of the individual trials are the same. In the most extreme example, comparing number of cases of radiographic changes in the partial meniscectomy groups of the Patel37 and Aglietti2 studies [100% (13 out of 13) versus 35% (7 out of 20), respectively] yields a risk difference of 65% with a P value of 0.0002 (2-sided Fisher’s Exact test). Since p < 0.10, we assume heterogeneity exists between the studies and thus elected not to combine the data in a meta-analysis.
DISCUSSION
The findings in this systematic review correlate the status of the meniscus at the time of ACL repair with the frequency of the development of radiographic evidence of osteoarthritis. They consistently demonstrate that an intact meniscus and to a lesser extend a repaired meniscus at the time of ACL reconstruction is correlated with a decreased likelihood of developing radiographic evidence of osteoarthritis in the first 5–10 years after reconstruction.
Abundant research on stable knees has shown the consequences of complete meniscectomy in the premature development of osteoarthritis.5, 11, 22, 23, 33 Partial meniscectomy is generally better tolerated, with good clinical outcomes and radiographic degeneration comparable with controls noted at up to 15 years.8, 10, 21, 45 One randomized study did find increased clinical symptoms patients who underwent complete meniscectomy compared with those who underwent partial meniscectomy but radiographic differences were not found.18 The role of the menisci as a secondary stabilizers in the ACL-deficient knee have long been known and clinical results have been poor after complete meniscectomy in these patients.7, 30 The finding in this review of frequent development of radiographic signs of osteoarthritis after ACL reconstruction in patients with complete meniscectomy is consistent with previous findings in both stable and unstable knees and is expected.
Three studies in this review analyze a group of patients who underwent meniscal repair.2, 4, 20 The two studies by Aglietti et al are consistent in their finding that the meniscal repair group and normal meniscus group exhibit similar radiographic findings and are both superior to the partial meniscectomy group. These data are in contrast to the findings by Hertel et al in which the meniscus repair group behaved more similarly to the partial meniscectomy group. These discrepancies may reflect the success of the meniscal repairs in the studies and possibly different repair methods. Aglietti et al use the outside-in method of Morgan and Casscells while Hertel et al do not describe their method of repair.34 The findings of Aglietti et al are not surprising given previous documentation of the success of concurrent ACL and meniscal repair exceeding that of isolated meniscal repair.9, 35, 38
This review also describes those patients with a partial meniscectomy as greater than five times more likely to develop radiographic evidence of osteoarthritis than patients with an intact meniscus at ACL reconstruction. This finding stresses the key role of the meniscus in prevention of radiographic signs of osteoarthritis. The relatively low rate of radiographic changes (10 %) in the group with intact menisci is much lower than documented rates of osteoarthritis in patients with conservatively treated ACL tears (40 %) without meniscal injury at similar follow-up interval.41 This finding supports the position that ACL reconstruction in a knee with intact menisci does not increase risk of osteoarthritis.
We chose to focus this review on patients reconstructed arthroscopically or with mini-open techniques utilizing hamstring or patellar autografts. These techniques represent the most common ACL reconstruction methods in use today and the rates of osteoarthritis development described above are applicable to most patients with isolated ACL tears treated with these methods. Authors using open reconstruction techniques have been reported similar findings, with partial or complete meniscectomy at the time of reconstruction predicting greater risk of development of osteoarthritis in 4–7 year follow-up.1, 12, 26, 31
The data presented above highlight the correlation of meniscus status at the time of ACL repair with development of radiographic evidence of osteoarthritis in patients with isolated ACL injuries. Several authors reporting 3–5 year follow-up ACL reconstruction cohorts that include patient with concomitant collateral ligament injury have also noted the correlation of meniscectomy at the time of repair with subsequent development of radiographic evidence of osteoarthritis.15, 24, 32, 36
This review provides strong evidence of the correlation between meniscus status at ACL reconstruction and the subsequent development of radiographic evidence of osteoarthritis. The major weakness of the study; however, is its inability to demonstrate causality. The correlation between meniscus status and radiographic changes does not necessarily indicate that the meniscus status is related to the development of these changes. It is possible that in those patients with a concomitant meniscal injury we are dealing with higher energy injuries or more chronic ACL injuries. More damage to the articular cartilage at the time of injury or recurrent episodes of instability in chronic cases could lead to the development of later osteoarthritis regardless of meniscal status. Similarly, because the medial meniscus is a secondary restraint of anterior tibial subluxation in the absence of an ACL, patients with meniscal pathology likely experience greater instability and hence greater cartilaginous injury prior to reconstruction. Finally, meniscal pathology may be associated with other patient characteristics not identified in this review that could explain an increased incidence of radiographic signs of osteoarthritis in this patient population.
Assessment of the impact of medial versus lateral meniscal pathology on outcome after reconstruction was not possible as the majority of studies did not distinguish between them when reporting radiographic findings.
The conclusions of this review are subject to the limitations and possible biases of the source studies. Selection bias was minimal as all studies enrolled a consecutive series of patients with well-defined selection criteria, although differences in patient selection criteria between studies such as the inclusion or exclusion of patient with articular cartilage lesions and the chronicity of injury do result in a somewhat heterogeneous overall patient population. Care must thus be taken when comparing results from study to study. Similarly, performance bias was also minimized as all studies utilized that same reconstruction technique and same surgeon for all patients, regardless of meniscal pathology. Transfer bias is a concern in this review as several of the studies had rather poor follow-up. It is possible that patients with post-operative symptoms are more likely to follow-up than those who are without symptoms. It is unclear what impact, if any, this bias may have as both patients with and without meniscal pathology would be affected. Detection bias appears minimal as both groups were evaluated using the same radiographic techniques within each study. It should be noted; however, that the outcome measure utilized in each study, radiographic evidence of osteoarthritis, does not necessarily indicate the presence of osteoarthritis as it is a clinical diagnosis.
The ideal method for establishing causality in the link between meniscal pathology and osteoarthritis would be the utilization of a prospective study design. Patients should be carefully selected, excluding those patients with internal derangement of the knee other than ACL and meniscal pathology. Careful examination of all patient and injury characteristics must be undertaken to identify any possible confounding variables. Finally, an attempt should be made to determine the degree of injury suffered by the articular cartilage at the time of injury – possibly through MRI evaluation of the extent of the bone bruise present. Outcome measures should include radiographic assessment as well as a validated patient-oriented clinical outcome measure such as the Knee Injury and Osteoarthritis Outcome Score (KOOS) or the Western Ontario and MacMaster University Osteoarthritis Index (WOMAC).
Footnotes
The use of the asterisk (*) symbol in a MEDLINE search denotes truncation of a word. All possible endings of the root word are searched.
References
- 1.Aglietti P, Buzzi R, D’Andria S, Zaccherotti G. Long-term study of anterior cruciate ligament reconstruction for chronic instability using the central one-third patellar tendon and a lateral extraarticular tenodesis. Am J Sports Med. 1992;20:38–45. doi: 10.1177/036354659202000111. [DOI] [PubMed] [Google Scholar]
- 2.Aglietti P, Buzzi R, Giron F, Simeone AJV, Zaccherotti G. Arthroscopic-assisted anterior cruciate ligament reconstruction with the central third patellar tendon: a 5–8-year follow-up. Knee Surg, Sports, Traumatol, Arthrosc. 1997;5:138–44. doi: 10.1007/s001670050041. [DOI] [PubMed] [Google Scholar]
- 3.Aglietti P, Buzzi R, Zaccherotti G. Patellar tendon versus doubled semitendinosis and gracilis tendons for anterior cruciate ligament reconstruction. Am J Sports Med. 1994;22:211–7. doi: 10.1177/036354659402200210. [DOI] [PubMed] [Google Scholar]
- 4.Aglietti P, Zaccherotti G, Biase P, Taddei I. A comparison between medial meniscus repair, partial meniscectomy, and normal meniscus in anterior cruciate ligament reconstructed knees. Clin Orthop Relat Res. 1994;307:165–73. [PubMed] [Google Scholar]
- 5.Allen PR, Denham RA, Swan AV. Late degenerative changes after meniscectomy. J Bone Joint Surg Br. 1984;66:666–71. doi: 10.1302/0301-620X.66B5.6548755. [DOI] [PubMed] [Google Scholar]
- 6.Appel H. Late results after meniscectomy in the knee joint. Acta Orthop Scand. 1970;133 (Suppl):1–111. doi: 10.3109/ort.1970.41.suppl-133.01. [DOI] [PubMed] [Google Scholar]
- 7.Barrack RL, Bruckner JD, Kneisl J, Inman WS, Alexander JH. The outcome of nonoperatively treated complete tears of the anterior cruciate ligament in active young adults. Clin Orthop Relat Res. 1990;259:192–9. [PubMed] [Google Scholar]
- 8.Burks RT, Metcalf MH, Metcalf RW. Fifteen-year follow-up of arthroscopic partial meniscectomy. Arthroscopy. 1997;13:673–9. doi: 10.1016/s0749-8063(97)90000-1. [DOI] [PubMed] [Google Scholar]
- 9.Cannon WD, Vittori JM. The incidence of healing in arthroscopic meniscus repairs in anterior cruciate reconstructed knees versus stable knees. Am J Sports Med. 1992;20:176–81. doi: 10.1177/036354659202000214. [DOI] [PubMed] [Google Scholar]
- 10.Chatain F, Adeleine P, Chambat P, Nevret P. A comparative study of medial versus lateral arthroscopic partial meniscectomy on stable knees: 10-year minimum follow-up. Arthroscopy. 2003;19:842–9. doi: 10.1016/s0749-8063(03)00735-7. [DOI] [PubMed] [Google Scholar]
- 11.Fairbank TJ. Knee joint changes after meniscectomy. J Bone Joint Surg Br. 1948;30:664–70. [PubMed] [Google Scholar]
- 12.Ferretti A, Conteduca F, De Carli A, Fontana M, Mariani PP. Osteoarthritis of the knee after ACL reconstruction. Int Orthop. 1991;15:367–71. doi: 10.1007/BF00186881. [DOI] [PubMed] [Google Scholar]
- 13.Fu FH, Bennett CH, Ma CB, Menetrey J, Latterman C. Current trends in anterior cruciate ligament reconstruction, part II: operative procedures and clinical correlations. Am J Sports Med. 2000;28:124–9. doi: 10.1177/03635465000280010801. [DOI] [PubMed] [Google Scholar]
- 14.Giron F, Aglietti P, Cuomo P, Mondanelli N, Ciardullo A. Anterior cruciate ligament reconstruction with double-looped semitendinosus and gracilis graft directly fixed to cortical bone: 5-year results. Knee Surg, Sports, Traumatol, Arthrosc. 2005;13:81–91. doi: 10.1007/s00167-004-0553-1. [DOI] [PubMed] [Google Scholar]
- 15.Harilainen A, Linko E, Sandelin J. Randomized prospective study of ACL reconstruction with interference screw fixation in patellar tendon autografts versus femoral metal plate suspension and tibial post fixation in hamstring tendon autografts: 5-year clinical and radiological follow-up results. Knee Surg Sports Traumatol Arthrosc. 2006;14:517–28. doi: 10.1007/s00167-006-0059-0. [DOI] [PubMed] [Google Scholar]
- 16.Harner CD, Olson E, Irrgang JJ. Allograft versus autograft anterior cruciate ligament reconstruction: 3- to 5-year outcome. Clin Orthop Relat Res. 1996;324:131–44. doi: 10.1097/00003086-199603000-00016. [DOI] [PubMed] [Google Scholar]
- 17.Hart AJ, Buscombe J, Malone A, Dowd GSE. Assessment of osteoarthritis after reconstruction of the anterior cruciate ligament. J Bone Joint Surg Br. 2005;87-B:1483–7. doi: 10.1302/0301-620X.87B11.16138. [DOI] [PubMed] [Google Scholar]
- 18.Hede A, Larsen E, Sandberg H. Partial versus total meniscectomy. A prospective, randomized study with long-term follow-up. J Bone Joint Surg Br. 1992;74:118–21. doi: 10.1302/0301-620X.74B1.1732238. [DOI] [PubMed] [Google Scholar]
- 19.Hefti F, Muller W, Jakob RP, Staubli HU. Evaluation of knee ligament injuries with IKDC form. Knee Surg Sports Traumatol Arthrosc. 1993;1:226–34. doi: 10.1007/BF01560215. [DOI] [PubMed] [Google Scholar]
- 20.Hertel P, Behrend H, Cierpinski T, Musahl V, Widjaja G. ACL reconstruction usinig bone-patellar tendon-bone press-fit fixation: 10-year clinical results. Knee Surg, Sports, Traumatol, Arthrosc. 2005;13:248–55. doi: 10.1007/s00167-004-0606-5. [DOI] [PubMed] [Google Scholar]
- 21.Hulet CH, Locker BG, Schiltz D, Texier A, Tallier E, Vielpeau CH. Arthroscopic medial meniscectomy on stable knees. J Bone Joint Surg Br. 2001;83:29–32. doi: 10.1302/0301-620x.83b1.11115. [DOI] [PubMed] [Google Scholar]
- 22.Jergensen U, Sonne-Holm S, Lauridsen F, Rosenlint A. A long-term follow-up of meniscectomy in athletes. A prospective longitudinal study. J Bone Joint Surg Br. 1987;69:480–3. doi: 10.1302/0301-620X.69B1.3818740. [DOI] [PubMed] [Google Scholar]
- 23.Johnson RJ, Kettelkamp DB, Clark W, Leaverton P. Factors affecting late results of meniscectomy. J Bone Joint Surg Am. 1974;56:719–29. [PubMed] [Google Scholar]
- 24.Jomha NM, Borton DC, Clingeleffer AJ, Pinczewski LA. Long term osteoarthritic changes in anterior cruciate ligament reconstructed knees. Clin Orthop Relat Res. 1999;358:188–93. [PubMed] [Google Scholar]
- 25.Jomha NM, Pinczewski LA, Clingeleffer AJ, Otto DD. Arthroscopic reconstruction of the anterior cruciate ligament with patellar tendon autograft and interference screw fixation: results at seven years. J Bone Joint Surg Br. 1999;81:775–9. doi: 10.1302/0301-620x.81b5.8644. [DOI] [PubMed] [Google Scholar]
- 26.Jonsson H, Riklund-Ahlstrom K, Lind J. Positive pivot shift after ACL reconstruction predicts later osteoarthritis: 63 patients followed 5–9 years after surgery. Acta Orthop Scand. 2004;75:594–9. doi: 10.1080/00016470410001484. [DOI] [PubMed] [Google Scholar]
- 27.Kartus JT, Russell VJ, Salmon LJ, et al. Concomitant partial meniscectomy worsens outcome after arthroscopic anterior cruciate ligament reconstruction. Acta Orthop Scand. 2002;73:179–85. doi: 10.1080/000164702753671777. [DOI] [PubMed] [Google Scholar]
- 28.Kellgren JK, Lawrence JS. Radiologic assessment of osteoarthritis. Ann Rheum Dis. 1957;16:494–501. doi: 10.1136/ard.16.4.494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lephart SM, Kocher MS, Harner CD. Quadriceps strength and functional capacity after anterior cruciate ligament reconstruction: patellar tendon autograft versus allograft. Am J Sports Med. 1993;21:738–43. doi: 10.1177/036354659302100519. [DOI] [PubMed] [Google Scholar]
- 30.Losse G, Daniel D, Malcolm L. The effect of meniscus surgery on anterior-posterior motion of the knee. Orthop Trans. 1983;7:280–1. [Google Scholar]
- 31.Lynch MA, Henning CE, Glick KR. Knee joint surface changes: long-term follow-up meniscus tear treatment in stable anterior cruciate ligament reconstruction. Clin Orthop Relat Res. 1983;172:148–53. [PubMed] [Google Scholar]
- 32.McConville OR, Kipnis JM, Richmond JC, Rockett SE, Michaud MJ. The effect of meniscal status on knee stability and function after anterior cruciate ligament reconstruction. Arthroscopy. 1993;9:431–9. doi: 10.1016/s0749-8063(05)80318-4. [DOI] [PubMed] [Google Scholar]
- 33.McGinty JB, Lawrence FG, Marvinr RAM. Partial or total meniscectomy. A comparative analysis. J Bone Joint Surg Am. 1977;59:763–6. [PubMed] [Google Scholar]
- 34.Morgan CD, Casscells SW. Arthroscopic meniscus repair: a safe approach to the posterior horns. Arthroscopy. 1986;2:3–12. doi: 10.1016/s0749-8063(86)80003-2. [DOI] [PubMed] [Google Scholar]
- 35.Morgan CD, Wojtys EM, Casscells CD, Casscells SW. Arthroscopic meniscal repair evaluated by second-look arthroscopy. Am J Sports Med. 1991;19:632–8. doi: 10.1177/036354659101900614. [DOI] [PubMed] [Google Scholar]
- 36.Otto D, Pinczewski LA, Clingeleffer A, Odell R. Five-year results of single-incision arthroscopic anterior cruciate ligament reconstruction with patellar tendon autograft. Am J Sports Med. 1998;26:181–8. doi: 10.1177/03635465980260020601. [DOI] [PubMed] [Google Scholar]
- 37.Patel JV, Church JS, Hall AJ. Central third bone-patellar tendon-bone anterior cruciate ligament reconstruction: a 5-year follow-up. Arthroscopy. 2000;16:67–70. doi: 10.1016/s0749-8063(00)90130-0. [DOI] [PubMed] [Google Scholar]
- 38.Rosenberg TD, Scott SM, Coward DB, et al. Arthroscopic meniscal repair evaluated with repeat arthroscopy. Arthroscopy. 1986;2:14–20. doi: 10.1016/s0749-8063(86)80005-6. [DOI] [PubMed] [Google Scholar]
- 39.Ruiz AL, Kelly M, Nutton RW. Arthroscopic ACL reconstruction: a 5–9 year follow-up. Knee. 2002;9:197–200. doi: 10.1016/s0968-0160(02)00019-4. [DOI] [PubMed] [Google Scholar]
- 40.Salmon LJ, Russell VJ, Refshauge K, et al. Long-term ooutcome of endoscopic anterior cruciate ligament reconstruction with patellar tendon autograft: minimum 13 year review. Am J Sports Med. 2006;34:721–32. doi: 10.1177/0363546505282626. [DOI] [PubMed] [Google Scholar]
- 41.Segawa H, Omori G, Koga Y. Long-term results of non-operative treatment of anterior cruciate ligament injury. Knee. 2001;8:5–11. doi: 10.1016/s0968-0160(00)00062-4. [DOI] [PubMed] [Google Scholar]
- 42.Seon JK, Song EK, Park SJ. Osteoarthritis after anterior cruciate ligament reconstruction using a patellar tendon autograft. Int Orthop. 2006;30:94–8. doi: 10.1007/s00264-005-0036-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Shelbourne KD, Carr DR. Meniscal repair compared with meniscectomy for bucket-handle medial meniscus tears in anterior cruciate ligament-reconstructed knees. Am J Sports Med. 2003;31:718–23. doi: 10.1177/03635465030310051401. [DOI] [PubMed] [Google Scholar]
- 44.Shelbourne KD, Dersam MD. Comparison of partial meniscectomy versus meniscus repair for bucket-handle lateral meniscus tears in anterior cruciate ligament reconstructed knees. Arthroscopy. 2004;20:581–5. doi: 10.1016/j.arthro.2004.03.009. [DOI] [PubMed] [Google Scholar]
- 45.Shelbourne KD, Dickens JF. Digital radiographic evaluation of medial joint space narrowing after partial meniscectomy of bucket-handle medial meniscus tears in anterior cruciate ligament-intact knees. Am J Sports Med. 2006;34:1648–55. doi: 10.1177/0363546506288019. [DOI] [PubMed] [Google Scholar]
- 46.Shelbourne KD, Gray T. Anterior cruciate ligament reconstruction with autogenous patellar tendon graft followed by accelerated rehabilitation: a two- to nine-year followup. Am J Sports Med. 1997;25:786–95. doi: 10.1177/036354659702500610. [DOI] [PubMed] [Google Scholar]
- 47.Shelbourne KD, Gray T. Results of anterior cruciate ligament reconstruction based on meniscus and articular cartilage status at the time of surgery. Am J Sports Med. 2000;28:446–52. doi: 10.1177/03635465000280040201. [DOI] [PubMed] [Google Scholar]
- 48.Sherman MF, Warren RF, Marshall JL, Savatsky GJ. A clinical and radiographic analysis of 127 anterior cruciate insufficient knees. Clin Orthop Relat Res. 1988;227:229–39. [PubMed] [Google Scholar]
- 49.Wang CJ, Huang TW, Jih S. Radiographic assessment of the knee after patellar tendon reconstruction for chronic anterior cruciate ligament deficiency. Chang Gung Med J. 2004;27:85–90. [PubMed] [Google Scholar]
- 50.Wu WH, Hackett T, Richmond JC. Effect of meniscal and articular surface status on knee stability, function, and symptoms after anterior cruciate ligament reconostruction: a long-term prospective study. Am J Sports Med. 2002;30:845–50. doi: 10.1177/03635465020300061501. [DOI] [PubMed] [Google Scholar]