Osteoporosis is a major health problem, particularly in the elderly because of the fractures that arise as a consequence of the decreasing bone mineral density (BMD) with age. Common sites of fragility fracture are at the hip, spine, and wrist. The incidence of these and other fragility fractures rises markedly with age. The most serious fracture in terms of morbidity, mortality, and health-care costs is hip fracture. As populations expand and life expectancy improves, the number of fractures is set to increase. The demographics of world populations are set to change with more elderly living in developing countries. In India, the number of postmenopausal women will rise by 81% in the next 20 years from 27.1 million in 2010 to 43.0 million in 2030.[1] The number of women aged 65 years or more will more than double. It has been estimated that by 2050 half of hip fractures will occur in Asia.[2]
A significant advance over the past 15 years has been the development of medical interventions that have been shown to decrease the risk of fragility fractures in high quality randomized controlled trials. Unfortunately, a minority of men and women receive treatment even after sustaining a fragility fracture.[3] The reason for a large treatment gap (the difference between the number of individuals at high-risk and the proportion of the population that receives treatment) is complex and multifactorial. One of the reasons is, however, limitations in the assessment of fracture risk.
The aim of guidelines is to provide an information platform for the assessment and treatment of osteoporosis hence that appropriate treatment is directed to individuals at high fracture risk. Ideally, guidelines should be based on systematic literature reviews and any recommendations supported by an adequate level of evidence. The Indian Menopause Society is to be congratulated in achieving this objective for postmenopausal women.
Although the diagnosis of the disease relies on the quantitative assessment of BMD, which is a major determinant of bone strength, the clinical significance of osteoporosis lies in the fractures that arise. The causation of fractures is however multifactorial. In this respect, there are some analogies with other multifactorial chronic diseases. For example, hypertension is diagnosed on the basis of blood pressure, whereas an important clinical consequence of hypertension is stroke.
Assessment of the BMD provides a crucial determinant of fracture risk and many guidelines have used BMD thresholds to determine whether treatments should be recommended. However, the multifactorial nature of fracture risk means that BMD does not capture non-skeletal determinants of fracture risk such as a liability to fall. A number of risk factors for fracture has been identified that contribute significantly to fracture risk over and above that provided by BMD.[4] A good example is age. The same BMD has a different significance at different ages, such that fracture risk is much higher in the elderly than in the young.[5] This is because age contributes to risk independently of BMD. Over the past few years, a series of meta-analyses has been undertaken to identify additional clinical risk factors that could be used in case finding strategies, with or without the use of BMD. This gave rise to the development of Fracture risk assessment tool (FRAX), a tool that integrates the information derived from the clinical risk factors and the BMD.[6]
The Indian guidance notes the value of BMD, independent clinical risk factors and FRAX in the assessment of fracture risk. In common with many guidelines, treatment is recommended in women with a prior fragility fracture. Treatment is also recommended in women with significant clinical risk factors in whom osteoporosis is diagnosed by densitometry. The guideline steers clear of specific advice on intervention thresholds based on FRAX.
FRAX calculates fracture probability in individuals from age, body mass index and dichotomized risk factors comprising prior fragility fracture, parental history of hip fracture, current tobacco smoking, ever use of long-term oral glucocorticoids, rheumatoid arthritis, other causes of secondary osteoporosis, and alcohol consumption.[6] Femoral neck BMD can be optionally input to enhance fracture risk prediction. Fracture probability is computed taking both the risk of fracture and the risk of death into account. The use of clinical risk factors in conjunction with BMD and age improves sensitivity of fracture prediction without adverse effects on specificity.[7] Even if the performance of FRAX is enhanced by the use of BMD tests, it should be recognized that FRAX without BMD has a predictive value for fractures that is comparable to the use of BMD alone.[8] Thus, a major advantage of FRAX is the ability to assess fracture risk where the BMD is unavailable. The availability and access to densitometry in India is very low,[9] but an Indian-specific FRAX model is available.
The use of FRAX in the clinical practice demands a consideration of the fracture probability at which to recommend treatment. Many different approaches have been used to set intervention thresholds with FRAX. The thresholds used have varied since they depend critically on local factors such as reimbursement issues, health economic assessment, and willingness to pay for health care in osteoporosis, and access to DXA. For this reason, it is not possible or desirable to recommend a unified intervention strategy. The strategy given below draws on that most commonly applied in Europe in the context of postmenopausal osteoporosis.
The present guidelines in India recommend that postmenopausal women with a prior fragility fracture may be considered for interventions without the necessity for a BMD test (other than to monitor treatment). For this reason, the intervention threshold in women without a prior fracture can be set at the age-specific fracture probability equivalent to that in women with a prior fragility fracture.[10] In essence, this represents a “fracture threshold” expressed as a probability. For a major osteoporotic fracture, the threshold rises with age from 2.8% at the age of 50 years to 17% at the age of 75 years or more [Figure 1]. In other words, the intervention threshold is set at the “fracture threshold.” This is the approach to intervention thresholds used in France, Switzerland, Europe, and by the National Osteoporosis Guideline Group for the UK.[10,11,12,13,14,15] The approach used, has been particularly well-validated and the intervention strategy shown to be cost-effective in the UK.
Figure 1.
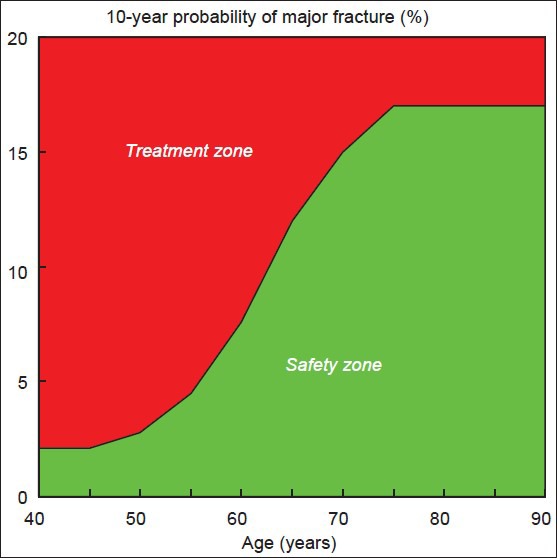
Assessment guidelines based on the 10-year probability of a major fracture (%). The sigmoid curve denotes the “fracture threshold” in postmenopausal women from India, which in turn may be considered as an intervention threshold
Thresholds can also or additionally be based on hip fracture probability [Figure 2].
Figure 2.
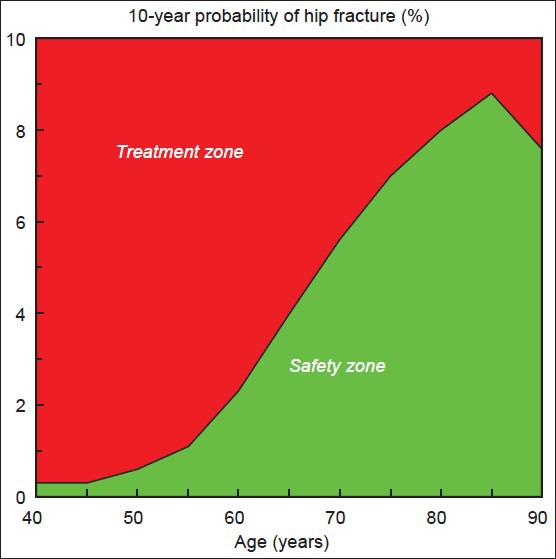
Assessment guidelines based on the 10-year probability of a hip fracture (%). The sigmoid curve denotes the “fracture threshold” in postmenopausal women from India, which in turn may be considered as an intervention threshold
The high societal and personal costs of osteoporosis pose challenges to public health and physicians, particularly since most patients with osteoporosis remain untreated. Indeed, less than 20% of patients with a fragility fracture receive therapy to reduce future fracture within the year following fracture. The aspiration of the guidance is to stimulate a cohesive approach to the management of osteoporosis in India and I wish it well.
REFERENCES
- 1.UN (2010) Population division of the department of economic and social affairs of the united nations secretariat (2010) world population prospects: The 2010 revision. [Last accessed on 2013 Mar 21]. Available from: http://www.esa.un.org/unpd/wpp/index.htm .
- 2.Cooper C, Campion G, Melton LJ., 3rd Hip fractures in the elderly: A world-wide projection. Osteoporos Int. 1992;2:285–9. doi: 10.1007/BF01623184. [DOI] [PubMed] [Google Scholar]
- 3.Elliot-Gibson V, Bogoch ER, Jamal SA, Beaton DE. Practice patterns in the diagnosis and treatment of osteoporosis after a fragility fracture: A systematic review. Osteoporos Int. 2004;15:767–78. doi: 10.1007/s00198-004-1675-5. [DOI] [PubMed] [Google Scholar]
- 4.Kanis JA. Diagnosis of osteoporosis and assessment of fracture risk. Lancet. 2002;359:1929–36. doi: 10.1016/S0140-6736(02)08761-5. [DOI] [PubMed] [Google Scholar]
- 5.Hui SL, Slemenda CW, Johnston CC., Jr Age and bone mass as predictors of fracture in a prospective study. J Clin Invest. 1988;81:1804–9. doi: 10.1172/JCI113523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kanis JA On behalf of the World Health Organization Scientific Group. Technical Report. University of Sheffield, UK: WHO Collaborating Centre; 2008. [Last accessed on 2013 Mar 14]. Assessment of osteoporosis at the primary health-care level. Available from: http://www.shef.ac.uk/FRAX/pdfs/WHO_Technical_Report.pdf . [Google Scholar]
- 7.Kanis JA, Oden A, Johnell O, Johansson H, De Laet C, Brown J, et al. The use of clinical risk factors enhances the performance of BMD in the prediction of hip and osteoporotic fractures in men and women. Osteoporos Int. 2007;18:1033–46. doi: 10.1007/s00198-007-0343-y. [DOI] [PubMed] [Google Scholar]
- 8.Kanis JA, McCloskey E, Johansson H, Oden A, Leslie WD. FRAX® with and without bone mineral density. Calcif Tissue Int. 2012;90:1–13. doi: 10.1007/s00223-011-9544-7. [DOI] [PubMed] [Google Scholar]
- 9.Kanis JA, Johnell O. Requirements for DXA for the management of osteoporosis in Europe. Osteoporos Int. 2005;16:229–38. doi: 10.1007/s00198-004-1811-2. [DOI] [PubMed] [Google Scholar]
- 10.Kanis JA, McCloskey EV, Johansson H, Strom O, Borgstrom F, Oden A, et al. Case finding for the management of osteoporosis with FRAX: Assessment and intervention thresholds for the UK. Osteoporos Int. 2008;19:1395–408. doi: 10.1007/s00198-008-0712-1. [DOI] [PubMed] [Google Scholar]
- 11.Ostéoporose: Recommandations. ASCO; 2010. [Last accessed on 2013 Mar 14]. Association Suisse contre l’Ostéoporose. Available from: http://www.svgo.ch/content/documents/SVGO_Empfehlungen2010_V19April2010.pdf . [Google Scholar]
- 12.Compston J, Cooper A, Cooper C, Francis R, Kanis JA, Marsh D, et al. Guidelines for the diagnosis and management of osteoporosis in postmenopausal women and men from the age of 50 years in the UK. Maturitas. 2009;62:105–8. doi: 10.1016/j.maturitas.2008.11.022. [DOI] [PubMed] [Google Scholar]
- 13.Briot K, Cortet B, Thomas T, Audran M, Blain H, Breuil V, et al. 2012 update of French guidelines for the pharmacological treatment of postmenopausal osteoporosis. Joint Bone Spine. 2012;79:304–13. doi: 10.1016/j.jbspin.2012.02.014. [DOI] [PubMed] [Google Scholar]
- 14.Kanis JA, McCloskey EV, Johansson H, Cooper C, Rizzoli R, Reginster JY, et al. European guidance for the diagnosis and management of osteoporosis in postmenopausal women. Osteoporos Int. 2013;24:23–57. doi: 10.1007/s00198-012-2074-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lekamwasam S, Adachi JD, Agnusdei D, Bilezikian J, Boonen S, Borgström F, et al. A framework for the development of guidelines for the management of glucocorticoid-induced osteoporosis. Osteoporos Int. 2012;23:2257–76. doi: 10.1007/s00198-012-1958-1. [DOI] [PubMed] [Google Scholar]


