The innate nonadaptive immune system plays a crucial role in the acute response to infectious agents. Within hours of exposure to an invading microorganism, well before adaptive cellular or humoral immune responses are engaged, the bulk of most infections is cleared by cells and molecules that bind with broad specificity to structures common to various pathogens. Only when infectious organisms break through these barriers do antigen receptor–bearing effector cells of the adaptive immune system come into play, ensuring that these organisms are cleared.
Blurring the distinction between the innate and the cognate aspects of the immune system are subsets of lymphocytes that recognize pathogenic determinants and are expressed even in immunologically naive animals (1). The significance of these lymphocytes is shown by the strong protection, elicited by T-independent natural IgM antibody, against certain viral and bacterial infections (2). The B- or T-cell receptors of these lymphocytes often contain highly conserved sequences, arise reproducibly in all mice, and do not depend on exogenous antigen for their generation. In this respect, they constitute an “evolutionary memory” and form a bridge between pattern recognition molecules — mannose receptors, macrophage scavenger receptors, and other similar molecules (3) — and the classic adaptive responses, which generally require T-cell help both to hone the specificity of the molecular interaction and to maintain immunological memory. These evolutionarily conserved responses to ubiquitously expressed microbial components are not confined to B cells, as there are numerous examples of αβ and γδ T cells that express canonical receptors to microbial components (4, 5).
In this issue of the JCI, Shaw et al. (6) show that these structurally distinct receptors functioning in different branches of the immune system nonetheless share patterns of ligand specificity. This provocative finding not only suggests mechanisms that may influence the progression of the disease, but also identifies a hitherto unknown function of an antibody response to a pathogenic bacterium.
Natural antibodies to phosphorylcholine
One manifestation of the chronic inflammatory process in ApoE–/– mice, which provide a commonly studied animal model for atherosclerosis, is the vigorous induction of autoantibodies to oxidized LDL (OxLDL). Working with this disease model, Shaw et al. (6) show that these antibodies belong to a class of highly conserved natural antibodies with the so-called T15 idiotype. These antibodies are known to participate in the immune response to phosphorylcholine (PC) and to confer protection from organisms such as Streptococcus pneumoniae.
PC is a component of multiple prokaryotic and eukaryotic organisms. In S. pneumoniae, it is associated with the cell wall component teichoic acid via N-acetylgalactosamine, and in a variety of other Gram-positive organisms, including other Streptococcus, Clostridium, and Bacillus species, PC is associated with different sugar residues. This lipid is also found in a variety of disease-inducing protozoa, fungi, nematodes, and other intestinal parasites (1). The immune response to PC in mice and its role in inducing protective antibodies against virulent S. pneumoniae infection are well described. When administered in the form of a heat-killed S. pneumoniae vaccine, the antibody response to PC is largely T-independent (IgM and IgG3) and oligoclonal, being dominated by antibodies containing a canonical VHDJH-Vκ22Jκ5 H+L Ig chain combination.
This combination of H+L chains was first identified in the induced plasmacytoma line T(EPC)15, which was shown to secrete antibodies specific to PC. This canonical combination of H+L chains defines the T15 idiotype (Id), which can be identified by anti-Id antibodies, either polyclonal or monoclonal (7, 8). Such probes have been used to show that normal mouse serum contains low levels of T15Id+ natural antibody with anti-PC activity but that these levels can be dramatically boosted by a primary immunization with the bacterial vaccine (9). There is strong evidence that the B cell precursors with this specificity develop during a critical window of development in fetal and early neonatal life (10). This developmental program can be ablated either by anti-Id–mediated deletion of T15Id+ B cells in perinatal life (11) or by molecular intervention to prevent formation of the germline-encoded canonical T15 H+L Ig chains (12). Both of these approaches cause a permanent loss of T15+ B cells and hence of the protective antibody. The anti-PC antibodies are among the best studied of so-called natural antibodies and represent a significant fraction of normal serum IgM found in germ-free mice (13).
Natural antibodies in atherosclerotic mice
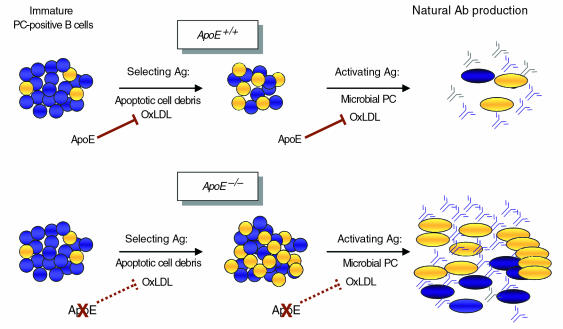
Shaw et al. (6) now report that this particular antibody has clearly defined specificity for modified LDL determinants. In ApoE–/– mice, the development of atherosclerosis is paralleled by increasing titers of antibodies to OxLDL. Using hybridomas and a comprehensive series of antibody specificity tests, these authors show that a major portion of the response can be attributed to the expansion and activation of independently arising T15+ clones, and they confirm this finding with molecular analyses (6). Although the anti-PC response has been studied for more than 30 years, this study appears to provide the first clues to the nature of the ligand that selects for T15+ clones during development. As shown in Figure 1, other B-cell clones also respond to modified lipoprotein determinants, but the T15 response predominates in most mice. Interestingly, the anti-PC responses employ different Vκ regions but the same Jκ5 region. Jκ5 is located at the 3′-most end of the Jκ locus, and its use has been interpreted as an indication that the progenitors of these B cells have revised their receptors during early development to escape from self-reactivity (14). This model suggests a possible mechanism by which multispecific T15+ B-cell clones may have been positively selected. These clones, which react not only with OxLDL and bacterial PC but also with apoptotic cells, may have been selected by interaction with apoptotic debris at sites of B-cell development in fetal liver and bone marrow (15), in a process that could involve receptor editing before or during the proliferation of specific B cells. Although the present authors have previously shown (16, 17) that deliberate immunization of hypercholesterolemic rabbits or mice expressing high levels of OxLDL lessens atherosclerosis, the role of these autoantibodies against OxLDL needs more evaluation.
Figure 1.
Potential role of OxLDL and ApoE in autoantibody production. Top: Under normal circumstances, the newly formed IgM+ B-cell population in the perinatal bone marrow or fetal liver can respond to millions of specific antigenic structures. Included in this population are anti-PC clones, some of which carry the T15 idiotype. In the selection step, PC epitopes on apoptotic material or OxLDL (selecting Ag) may enrich for T15/PC-specific B cells. The degree to which this occurs would be limited by the efficiency of debris-scavenging by macrophages or by the availability of ApoE. Additionally, these T15 clones may be stimulated to differentiate by the normally regulated amounts of PC or OxLDL (activating Ag). Bottom: In the absence of ApoE, accumulated OxLDL may promote a still more profound enrichment for T15 clones or may stimulate existing clones to differentiate into T15-producing (natural antibody–producing) plasma cells. Either possibility would give rise to the high levels of anti-OxLDL antibodies observed in the ApoE–/– mice. Circles represent B cells; ovals represent mature antibody-secreting plasma cells. Blue, αPC; yellow, T15/PC.
The exuberant response of the T15+ clones in ApoE–/– mice is clearly antigen-driven, and the antigens appear to be oxidized phospholipids and/or their protein counterparts. It will be important to determine the fine specificity and the affinity of their binding to each of these species of modified LDL. Additionally, mechanisms involved in the activation of these B cells needs evaluation. Normally, T15+ B cells can be triggered into proliferation and IgM antibody production in a T-independent fashion. The role of T cells in the response is not yet clear, nor is it known whether switching to IgG isotypes occurs. This possibility could be of considerable importance for understanding atherosclerotic plaque formation, since foam cells may use Fc receptors to take up OxLDL complexed with IgG but not IgM antibodies. Conceivably, then, chronic infection with organisms expressing PC may induce synthesis of anti-PC antibodies of IgM or even IgG isotypes, which could influence the disease process. Since the anti-PC B-cell repertoire changes during the life of the organism, the participation of natural IgM anti-PC antibodies in the disease process may vary with age (18).
One way to test these admittedly speculative ideas would be to compare the effects of T15+ antibody levels in different mouse models of atherosclerosis. In ApoE–/– mice, the disease process begins very early, progresses steadily, and does not require high levels of dietary cholesterol. Conversely, in LDL receptor–deficient (LDLR-deficient) mice, the beginnings of atherosclerosis are not evident unless animals receive a specific diet (19). How might the production of anti-OxLDL antibodies — and the natural history of the disease — be affected by providing this diet to LDLR–/– mice only after the critical perinatal period when T15+ clones become selected? Similarly, since OxLDL has been found in fetal arteries of ApoE–/– animals (20), this ligand may be involved in the positive selection of the emerging T15+ clones (Figure 1). The increased levels of OxLDL in the ApoE–/– mice may amplify the normal selection process, resulting in a greatly expanded pool of these cells in the adult. The current work (6) shows that a highly conserved antibody response to PC can affect the metabolism of modified LDL, but whether it contributes to atherosclerosis, either promoting or ameliorating this condition, remains to be determined.
Patterns of ligand specificity
Shaw et al. (6) also show that T15+ antibodies bind specifically to apoptotic cells, extending their group’s previous observation that antibodies to OxLDL block uptake and disposal of apoptotic cells by macrophages (21). Pattern recognition receptors such as the macrophage scavenger receptors and CD36 likewise recognize determinants on apoptotic cells. Whether T15+ antibodies interfere with these receptors or with the recently described phagocytic receptor for apoptotic cells (22) remains to be explored, but the overlapping biochemical specificity of these pattern recognition receptors and of the natural antibodies is striking in any case. In addition, type 1 macrophage scavenger receptors bind lipoteichoic acid (23), another T15 ligand.
Together, these findings provide several examples of ligands — or classes of ligands — shared by these seemingly dissimilar components of the innate immune system, and they raise intriguing questions about functional interactions between these molecules. Do T15 antibodies modulate the uptake and clearance of apoptotic cells in vivo? Does interference with this important macrophage function provide a potential source of other neoantigens and induce the proliferation of other self-reactive clones?
References
- 1.Harnett W, Harnett MM. Phosphorylcholine: friend or foe of the immune system? Immunol Today. 1999;20:125–129. doi: 10.1016/s0167-5699(98)01419-4. [DOI] [PubMed] [Google Scholar]
- 2.Ochsenbein AF, et al. Control of early viral and bacterial distribution and disease by natural antibodies. Science. 1999;286:2156–2159. doi: 10.1126/science.286.5447.2156. [DOI] [PubMed] [Google Scholar]
- 3.Hoffmann JA, Kafatos FC, Janeway CA, Ezekowitz RA. Phylogenetic perspectives in innate immunity. Science. 1999;284:1313–1318. doi: 10.1126/science.284.5418.1313. [DOI] [PubMed] [Google Scholar]
- 4.Reardon CL, et al. Murine epidermal V gamma 5/V delta 1-T-cell receptor+ T cells respond to B-cell lines and lipopolysaccharides. J Invest Dermatol. 1995;105(Suppl.):58S–61S. doi: 10.1111/1523-1747.ep12316074. [DOI] [PubMed] [Google Scholar]
- 5.Boismenu R, Havran WL. An innate view of gamma delta T cells. Curr Opin Immunol. 1997;9:57–63. doi: 10.1016/s0952-7915(97)80159-8. [DOI] [PubMed] [Google Scholar]
- 6.Shaw PX, et al. Natural antibodies with the T15 idiotype may act in atherosclerosis, apoptotic clearance, and protective immunity. J Clin Invest. 2000;105:1731–1740. doi: 10.1172/JCI8472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Benca R, Quintans J, Kearney JF, Flood PM, Schreiber H. Studies on phosphorylcholine-specific T cell idiotypes and idiotype-specific immunity. Mol Immunol. 1980;17:823–831. doi: 10.1016/0161-5890(80)90031-0. [DOI] [PubMed] [Google Scholar]
- 8.Kearney JF, Barletta R, Quan ZS, Quintans J. Monoclonal vs. heterogeneous anti-H-8 antibodies in the analysis of the anti-phosphorylcholine response in BALB/c mice. Eur J Immunol. 1981;11:877–883. doi: 10.1002/eji.1830111106. [DOI] [PubMed] [Google Scholar]
- 9.McDaniel LS, Benjamin WH, Forman C, Briles DE. Blood clearance by anti-phosphocholine antibodies as a mechanism of protection in experimental pneumococcal bacteremia. J Immunol. 1984;133:3308–3312. [PubMed] [Google Scholar]
- 10.Masmoudi H, Mota-Santos T, Huetz F, Coutinho A, Cazenave PA. All T15 Id-positive antibodies (but not the majority of VHT15+ antibodies) are produced by peritoneal CD5+ B lymphocytes. Int Immunol. 1990;2:515–520. doi: 10.1093/intimm/2.6.515. [DOI] [PubMed] [Google Scholar]
- 11.Elliott M, Kearney JF. Idiotypic regulation of development of the B cell repertoire. Ann NY Acad Sci. 1992;651:336–345. doi: 10.1111/j.1749-6632.1992.tb24633.x. [DOI] [PubMed] [Google Scholar]
- 12.Benedict CL, Kearney JF. Increased junctional diversity in fetal B cells results in a loss of protective anti-phosphorylcholine antibodies in adult mice. Immunity. 1999;10:607–617. doi: 10.1016/s1074-7613(00)80060-6. [DOI] [PubMed] [Google Scholar]
- 13.Grandien A, et al. On the origin of natural IgM in immunoglobulin transgenic mice. Int Immunol. 1992;4:1153–1160. doi: 10.1093/intimm/4.10.1153. [DOI] [PubMed] [Google Scholar]
- 14.Gay D, Saunders T, Camper S, Weigert M. Receptor editing: an approach by autoreactive B cells to escape tolerance. J Exp Med. 1993;177:999–1008. doi: 10.1084/jem.177.4.999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Vakil M, Briles D, Kearney J. Antigen-independent selection of T15 idiotype during B-cell ontogeny in mice. Dev Immunol. 1991;1:203–212. doi: 10.1155/1991/45352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Palinski W, Miller E, Witztum JL. Immunization of low density lipoprotein (LDL) receptor-deficient rabbits with homologous malondialdehyde-modified LDL reduces atherogenesis. Proc Natl Acad Sci USA. 1995;92:821–825. doi: 10.1073/pnas.92.3.821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Freigang S, Horkko S, Miller E, Witztum JL, Palinski W. Immunization of LDL receptor-deficient mice with homologous malondialdehyde-modified and native LDL reduces progression of atherosclerosis by mechanisms other than induction of high titers of antibodies to oxidative neoepitopes. Arterioscler Thromb Vasc Biol. 1998;18:1972–1982. doi: 10.1161/01.atv.18.12.1972. [DOI] [PubMed] [Google Scholar]
- 18.Nicoletti C, Yang X, Cerny J. Repertoire diversity of antibody response to bacterial antigens in aged mice. J Immunol. 1993;150:543–549. [PubMed] [Google Scholar]
- 19.Huszar D, et al. Increased LDL cholesterol and atherosclerosis in LDL receptor-deficient mice with attenuated expression of scavenger receptor B1. Arterioscler Thromb Vasc Biol. 2000;20:1068–1073. doi: 10.1161/01.atv.20.4.1068. [DOI] [PubMed] [Google Scholar]
- 20.Napoli C, et al. Fatty streak formation occurs in human fetal aortas and is greatly enhanced by maternal hypercholesterolemia. Intimal accumulation of low density lipoprotein and its oxidation precede monocyte recruitment into early atherosclerotic lesions. J Clin Invest. 1997;100:2680–2690. doi: 10.1172/JCI119813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chang MK, et al. Monoclonal antibodies against oxidized low-density lipoprotein bind to apoptotic cells and inhibit their phagocytosis by elicited macrophages: evidence that oxidation-specific epitopes mediate macrophage recognition. Proc Natl Acad Sci USA. 1999;96:6353–6358. doi: 10.1073/pnas.96.11.6353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Fadok VA, et al. A receptor for phosphatidylserine-specific clearance of apoptotic cells. Nature. 2000;405:85–90. doi: 10.1038/35011084. [DOI] [PubMed] [Google Scholar]
- 23.Dunne DW, Resnick D, Greenberg J, Krieger M, Joiner KA. The type I macrophage scavenger receptor binds to gram-positive bacteria and recognizes lipoteichoic acid. Proc Natl Acad Sci USA. 1994;91:1863–1867. doi: 10.1073/pnas.91.5.1863. [DOI] [PMC free article] [PubMed] [Google Scholar]