Abstract
Lifestyle modification programs (LMP) for weight loss in adolescents with obesity are effective but not available. Primary care may be a setting for reaching more adolescents. Two models of LMP for use in primary care were examined. Adolescents and caregivers enrolled in a 1-year randomized trial comparing Group LMP with Self-Guided LMP. All participants (N = 169) received the same treatment recommendations and met with a health coach six times in clinic. Group LMP participants had an additional 17 group sessions; those in Self-Guided LMP followed the remainder of the program at home with parental support. The primary outcome was percentage change in initial body mass index. The mean (SE) 1.31% (0.95%) reduction in Group LMP did not differ significantly from the 1.17% (0.99%) decrease in the Self-Guided LMP (p = 0.92). Both treatments were significantly effective in reducing body mass index. Given its brevity, the Self-Guided LMP offers an innovative approach for primary care.
Keywords: adolescents, obesity, primary care, weight management
Introduction
The rate of adolescent obesity has tripled in the past 3 decades (Ogden & Carroll, 2010; Ogden, Carroll, Kit, & Flegal, 2012). Research on the long-term safety and efficacy of treatments for adolescent obesity, compared with those for childhood obesity, is lacking (Butryn et al., 2010). A comprehensive program of lifestyle modification is effective for adolescents with obesity, though no single dietary or physical activity approach has been identified as more effective than others. Programs have included family-based behavior modification, nutrition education, physical activity, and parental support (Oude Luttikhuis et al., 2009). Lifestyle modification programs (LMPs) are often time and staff intensive, and research typically has been conducted at major academic institutions in specialty centers, limiting accessibility. Novel treatment approaches are needed (Oude Luttikhuis, et al., 2009). These novel interventions need to combine approaches in a variety of settings for greater access to care while also offering effective programming that is practical and can reach the many youth requiring services.
An Alternative to Intensive LMP
The effectiveness of self-guided therapy (i.e., bibliotherapy) for adolescent obesity is unclear because the research has been conducted primarily with adults, and results have been mixed (Jeffery et al., 2003). Davis et al. (2012) found that monthly newsletters were as effective as in-person visits in the maintenance of weight loss after a 4-month nutrition and strength training intervention for overweight Latino and African-American adolescents (Davis et al., 2012). Thus, the self-help approach may warrant further investigation. Access to LMP could also be improved with the use of less intensive programs, as compared with those that require weekly treatment sessions for several months. Nguyen et al. (2012) examined the effectiveness of quarterly in-person booster sessions following a seven-session LMP compared with the same program plus adjunctive telephone coaching and electronic contact intervention (Nguyen et al., 2012). At the 1- and 2-year follow ups, there were no significant differences between groups, and both groups achieved similar but modest reductions in body mass index z (BMI z) score. These studies did not examine the efficacy of self-guided therapy for inducing weight loss, which is a critical area of research. Steele et al. (2012) recently compared a 10-session group-based program with a brief 3-session family intervention using the Trim Kids manual (Sothern, Von Almen, & Schumacher, 2002). The two approaches achieved comparable modest improvements in BMI z scores at post-treatment and 1-year follow-up in children. Both interventions, however, were less effective for adolescents (Steele et al., 2012).
Primary care practice may provide an excellent setting in which to engage adolescents and their families in weight management. The American Academy of Pediatrics recommends that primary care providers offer nutrition, physical activity, and behavior modification counseling to children who are overweight (Krebs & Jacobson, 2003). Studies examining the treatment of adolescents who are overweight in primary care settings have reported promising results (DeBar et al., 2012; Dolinsky, Armstrong, Walter, & Kemper, 2012; Kwapiszewski & Lee Wallace, 2011). A 4-month trial found that a brief provider visit, followed by a phone and mail intervention, resulted in 40% of participants achieving a reduction in BMI z scores, compared with only 10% who received usual care (Saelens et al., 2002). Another study has reported positive trends in a small sample of adolescents (Lane-Tillerson, Davis, Killion, & Baker, 2005).
The present study examined two family-based LMPs developed to treat underserved urban and rural youth with obesity. Adolescents and caregivers were enrolled in a 1-year randomized trial that compared an intensive (23-session) Group LMP, developed at an academic medical center, with a brief (6-session) Self-Guided LMP, the latter which could be a model for use in primary care. Prior studies of adults and adolescents have reported that higher intensity lifestyle counseling (i.e., more treatment visits) induces greater weight loss than a low-intensity intervention, which led us to predict that intensive Group LMP would induce a greater percentage reduction in BMI at 1 year (Moyer, 2012). At the same time, we wished to estimate the amount of weight loss that could be achieved with the innovative less intensive self-guided approach.
Methods
Participants
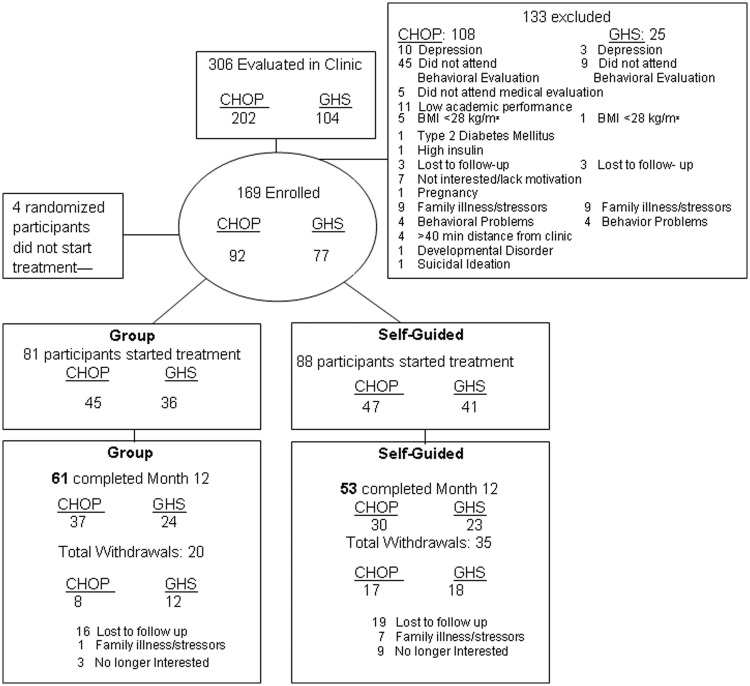
Participants were 12–16-year-old males and postmenarcheal females with a BMI ≥ 28 kg/m2. An urban, primarily African American, sample was recruited at The Children’s Hospital of Philadelphia (CHOP) and a rural Caucasian sample at the Geisinger Health System (GHS) in Danville, PA. Participants were recruited from primary care electronic medical records, physician alerts in the electronic medical record, and public service announcements. Written informed consent was obtained from parents and assent from the adolescents. Adolescents and their parent or guardian completed a behavioral screening conducted by a psychologist to identify significant psychopathology and to determine motivation for participating in the study. Candidates underwent a medical screening to rule out contraindications to treatment. These included cardiovascular disease (including arrhythmias), type 1 or 2 diabetes mellitus, psychiatric disorders (such as major depressive disorder and behavioral disorders), pregnancy, use of a weight-loss medication or a weight loss of ≥5 kg in the prior 6 months, use of medications promoting weight gain (e.g., oral steroids), or cigarette smoking (as described in Figure 1). (Because this was the first assessment of those two interventions in a primary care setting, we selected a participant sample with less severe co-morbid conditions, before undertaking a trial with a typical clinic population.) This study was approved by the institutional review boards at the two sites (ClinicalTrials.Gov Identifier: NCT01073215).
Figure 1.
Consort diagram describing the flow of participants through each stage of the randomized trial.
Procedures
A total of 306 candidates applied for entry to the study, and a total of 173 were found eligible and randomized to Self-Guided LMP or Group LMP in a 1:1 ratio via a permuted block randomization design, stratified by site. The data for the 169 randomized participants who attended at least one treatment session were used in the analyses (see Figure 1).
Interventions
Adolescents in both treatment conditions received the same 12-month comprehensive family-based LMP curriculum. The LMP was delivered following detailed treatment manuals provided to adolescents and parents (or guardians) (Wadden & Berkowitz, 2001), which were written at a fifth-grade reading level. All adolescents were asked to consume a nutritionally balanced diet of 1300–1500 kcal/day, according to the United States Department of Agriculture (USDA) MyPyramid guidelines (USDA, 2009) to increase physical activity to 60 min or 10,000 steps daily, and to decrease sedentary behaviors to fewer than 2 hr daily (Wadden & Berkowtiz, 2001; Wadden et al., 1990). The program included the following: Self-monitoring of food and calorie intake, as well as target goals; physical activity; stress management; stimulus control; problem solving; contingency management; cognitive restructuring; and social (parental) support, as described by Butryn et al. (2010). To facilitate daily recording of food intake and physical activity, adolescents were compensated up to $3 for each weekly record completed.
Both Group and Self-Guided LMP participants had six scheduled clinic visits (∼45 min each) at which the parent and adolescent dyad met with a health coach (e.g., nurses and nurse practitioners, dietitians, masters’ level counselors, or doctoral level psychologists) for an individual family meeting. Participants were taught both by face-to-face meetings and by review of the manual. Counseling during these visits promoted adherence to the study’s diet and physical activity goals. Parents and teens in the Self-Guided LMP condition were instructed to read and complete the lessons in the treatment manual and review them together on a weekly basis at home.
Parents and teens in the Group LMP were provided 17 additional in-clinic group visits at which they reviewed their progress in completing the lessons from the treatment manual, had interactive discussions around eating and physical activity topics, and received peer support. Parents met in separate group sessions, which ran concurrently with their child’s group.
Certification of Interventionists and Treatment Fidelity
Health coaches were trained to deliver both Self-Guided and Group LMP by completing about 20 hours of initial face-to-face training meetings along with review of interventionist and participant manuals. They successfully completed two sessions of the Group LMP and one session of Self-Guided conditions, as observed by senior clinicians. Coaches attended regularly scheduled team meetings, led by senior clinicians, to review their adherence to the protocol.
Outcome Measures
Weight was measured (using a digital scale) at each of the major assessments (i.e., baseline and months 6 and 12). Height and waist circumference were measured following standard techniques (World Health Organization, 1989). The primary efficacy measure was percentage change in BMI (kg/m2) from baseline to month 12. Secondary outcomes included changes in BMI and BMI z-score (Centers for Disease Control and Prevention, 2005) and the proportion of subjects achieving reductions in BMI of ≥5 or ≥10% (i.e., clinically meaningful indicators of weight loss), and waist circumference. Adherence to the LMP was assessed indirectly by tracking attendance at sessions. Psychosocial and physiologic measures that were collected are not examined in this report.
Data Analysis
The primary hypotheses were that participants in Group LMP would achieve a greater percentage reduction in initial BMI at months 6 and 12 than those in Self-Guided LMP. This measure controls for changes in height over time and for differences in baseline BMI. Secondary outcomes included change in BMI and BMI z-score (Epi Info, 2002). For the primary outcome, repeated measures mixed effects models were fitted that included condition as the between subjects factor and time (changes from baseline to months 6 and 12) as the within subjects factor, adjusted for site. Sensitivity analyses were conducted that fit mixed models that used baseline carried forward and last observation carried forward approaches in which missing data were replaced by the participant’s baseline body weight or last body weight obtained, respectively.
A secondary hypothesis was that within both the African American urban adolescents at CHOP and within the rural Caucasians at GHS, Group LMP would result in greater percentage change in BMI compared with Self-Guided LMP. Two mixed model analyses were conducted to assess percentage change in BMI between conditions within urban African-Americans at CHOP and within rural Caucasians at GHS.
In an exploratory analysis, the relationship between attendance and losing ≥5 or ≥10% of initial BMI was examined using Fisher’s exact tests. Attendance was represented as a binary variable based on a median split within condition. For all analyses, the significance level (α) was equal to 0.05. Analyses were conducted using SAS, version 9.2.
Results
Study Sample and Retention
Baseline characteristics of the 169 (92 urban at CHOP, 77 rural at GHS) participants who attended at least one treatment session are presented in Table I. There were no statistically significant differences between treatment conditions or sites on any of the baseline measures. Seventy-seven percent of participants were female. Forty-seven percent self-identified as African American, 47% as Caucasian, and 5% as being of more than one ethnicity (see Table I). Participants had a mean (SD) age of 14.6 (1.4) years and a BMI of 36.7 (5.2) kg/m2. Parental education levels are described in Table I. At month 12, overall retention was 67.5%. There was a significant difference in retention between groups, with 75% for group LMP and 60% for self-guided (p = 0.04, see Figure 1). However, the mixed model analysis was used to take into account attrition related to observed variables (e.g., condition). There were no statistically significant differences in retention between sites at month 12 (CHOP 73%, GHS 61%; p = 0.10).
Table I.
Baseline Characteristics for Participants Assigned to Group LMP and Self-Guided LMP
| Group LMP | Self-guided LMP | ||||
|---|---|---|---|---|---|
|
N = 81 |
N = 88 |
||||
| Characteristics, mean (SD) | Total sample | CHOP N = 45 | GHS N = 36 | CHOP N = 47 | GHS N = 41 |
| Age, (year) | 14.6 (1.4) | 14.5 (1.5) | 14.7 (1.3) | 14.3 (1.5) | 14.9 (1.4) |
| Weight, (kg) | 100.5 (18.8) | 100.4 (20.1) | 98.7 (17) | 101.1 (17.4) | 101.7 (21) |
| Height, (cm) | 165.2 (7.6) | 165 (8) | 165.8 (7) | 163.8 (7.6) | 166.2 (7.5) |
| BMI (kg/m2) | 36.7 (5.2) | 36.6 (5) | 35.8 (5.2) | 37.5 (5) | 36.6 (5.8) |
| BMI Z-score | 2.3 (0.3) | 2.4 (0.3) | 2.3 (0.3) | 2.4 (0.3) | 2.3 (0.3) |
| Waist circumference, cm | 111 (13.3) | 108.5 (13.5) | 113.2 (12.9) | 109.9 (11) | 113.2 (15.7) |
| Maternal BMI | 36.6 (7.6) | 37.8 (7.5) | 34.5 (7.8) | 35.6 (7.2) | 38.3 (7.5) |
| Characteristics, N (%) | |||||
| Sex, female | 130 (76.9%) | 34 (75.6%) | 28 (77.8%) | 38 (80.9%) | 30 (73.2%) |
| Race N (%) | |||||
| Caucasian | 79 (46.7%) | 4 (8.9%) | 34 (94.4%) | 1 (2.1%) | 40 (97.6%) |
| African American | 79 (46.7%) | 35 (77.8%) | 0 (0%) | 43 (91.5%) | 1 (2.4%) |
| Native American | 1 (0.6%) | 1 (2.2%) | 0 (0%) | 0 (0%) | 0 (0%) |
| Unknown | 2 (1.2%) | 2 (4.4%) | 0 (0%) | 0 (0%) | 0 (0%) |
| More than one race | 8 (4.7%) | 3 (6.7%) | 2 (5.6%) | 3 (6.4%) | 0 (0%) |
| Ethnicity, Hispanic | 4 (2.4%) | 3 (6.7%) | 0 (0%) | 1 (2.1%) | 0 (0%) |
| Parental education N (%) | |||||
| High School or less | 55 (32.5%) | 14 (31.1%) | 17 (47.2%) | 13 (27.7%) | 11 (26.8%) |
| Some College | 98 (58%) | 26 (57.8%) | 18 (50%) | 30 (63.8%) | 24 (58.5%) |
| College or more | 16 (9.5%) | 5 (11.1%) | 1 (2.8%) | 4 (8.5%) | 6 (14.6%) |
Percentage Reduction in BMI
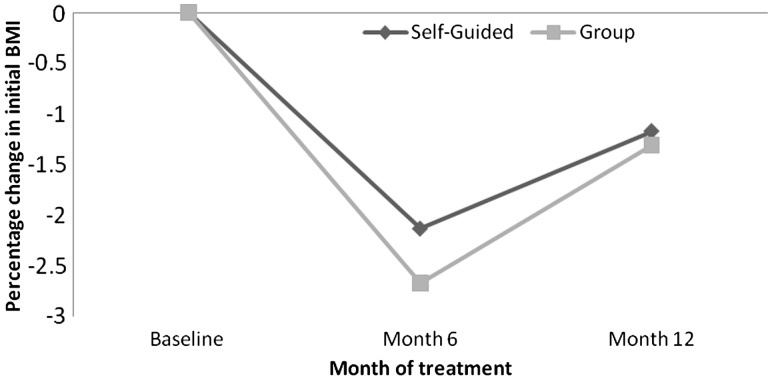
At month 12, participants in Group LMP achieved a mean (SE) reduction in initial BMI of 1.31% (0.95) compared with 1.17% (0.99) for those in Self-Guided LMP. The difference between groups was not statistically significant (condition p = 0.75, time p = 0.01, time*condition p = 0.67) (see Table II and Figure 2). Collapsed across the two conditions, mean reduction in initial BMI at month 12, for the entire sample was 1.2% (0.69%) (p = 0.01). As shown in Table I, there also were no statistically significant differences between conditions in changes in BMI (kg/m2), BMI z-score, weight (kg), height (cm), or waist circumference at months 6 or 12 (ps > 0.71).
Table II.
Changes in Degree of Obesity From Baseline to Months 6 and 12 for Adolescent Treated With Group LMP or Self-Guided LMP
| Variable (change) | Baseline to month 6 |
Baseline to month 12 |
|||||
|---|---|---|---|---|---|---|---|
| Group LMP M (SE) Δ | Self-guided LMP M (SE) Δ | Difference between conditions mean (CI) | Group LMP M (SE) Δ | Self-guided LMP M (SE) Δ | Difference between conditions mean (CI) | Difference between conditions p-value | |
| BMI, Percentage | −2.67 (0.67) | −2.13 (0.69) | 0.54 (−1.35, 2.43) | −1.31 (0.95) | −1.17 (0.99) | 0.14 (−2.58, 2.86) | 0.92 |
| BMI, kg/m2 | −0.94 (0.24) | −0.77 (0.25) | 0.16 (−0.53, 0.85) | −0.45 (0.35) | −0.38 (0.36) | 0.08 (−0.92, 1.07) | 0.88 |
| BMI z-score | −0.11 (0.02) | −0.09 (0.02) | 0.02 (−0.03, 0.07) | −0.12 (0.03) | −0.12 (0.03) | 0.00 (−0.08, 0.07) | 0.91 |
| Weight, kg | −1.81 (0.67) | −1.61 (0.70) | 0.20 (−1.71, 2.11) | 0.61 (0.98) | 0.40 (1.04) | −0.21 (−3.03, 2.61) | 0.89 |
| Height, cm | 0.61 (0.15) | 0.66 (0.15) | 0.05 (−0.37, 0.48) | 1.42 (0.27) | 1.32 (0.28) | −0.10 (−0.86, 0.66) | 0.79 |
| Waist circumference, cm | −3.57 (0.77) | −2.31 (0.78) | 1.26 (−0.91, 3.43) | −2.87 (1.01) | −3.41 (1.05) | −0.54 (−3.42, 2.34) | 0.71 |
Note. M (SE) Δ refers to Mean Change from baseline to time point indicated with corresponding standard error. CI refers to the 95% confidence interval around the between condition mean difference (e.g., Mean Self minus Mean Group).
Figure 2.
Percentage reduction in initial BMI at month 6 and month 12 for participants treated by Self-Guided (diamonds) or Group (squares) family-based LMP. There were no significant differences between the two treatment conditions at month 6 or month 12.
The baseline carried forward analysis revealed similar results as the mixed-effects model. Percentage reductions in initial BMI at month 6 were 2.0% (0.49%) for Group LMP and 1.3% (0.47%) for Self-Guided LMP (p = 0.31), and at month 12, they were 0.88% (0.70%) and 0.53% (±0.67%), respectively (p = 0.72). Similar results were obtained with the last observation carried forward analysis.
Secondary Outcomes
Within-Group Differences at Urban and Rural Sites
Based on the mixed model analyses, there were no significant differences between the Group LMP and Self-Guided LMP conditions in percentage change in BMI at month 12 within urban African-Americans at CHOP or within rural Caucasians at GHS. Similarly, there were no significant differences at month 12 between Group LMP and Self-Guided LMP in BMI (kg/m2), BMI Z-score, weight (kg), height (cm), or waist circumference within urban African-Americans at CHOP or within rural Caucasians at GHS (ps > 0.18) (data not presented).
Categorical Weight Loss
At month 12, 18.5% of participants in the Group LMP and 12.5% of those in the Self-Guided LMP lost ≥5% of their initial BMI (p = 0.29). Corresponding values for losing ≥10% of initial BMI were 8.6 and 5.7%, respectively (p = 0.55). Similar results were found at both sites (data not presented). (These analyses assumed that participants with missing data at month 12 lost no weight.)
Attendance and Percentage Reduction in BMI
A median split analysis for low vs. high attendance in the Self-Guided LMP sessions (i.e., adolescents with low attendance attended four or fewer of six clinic sessions) showed that attendance was significantly associated with achieving a ≥5% reduction in BMI at month 12. None of the low attendees met this criterion compared with 22% of high attendees (p = 0.0021). A similar analysis for Group LMP (i.e., low attendees attended 17 or fewer sessions of a possible 23 sessions) revealed that only 8% of low attendees lost ≥5% of initial BMI at month 12, compared with 27% of high attenders (p = 0.045) (see Figure 3). Similar findings were obtained for adolescents obtaining ≥10% reduction in BMI at month 12.
Figure 3.
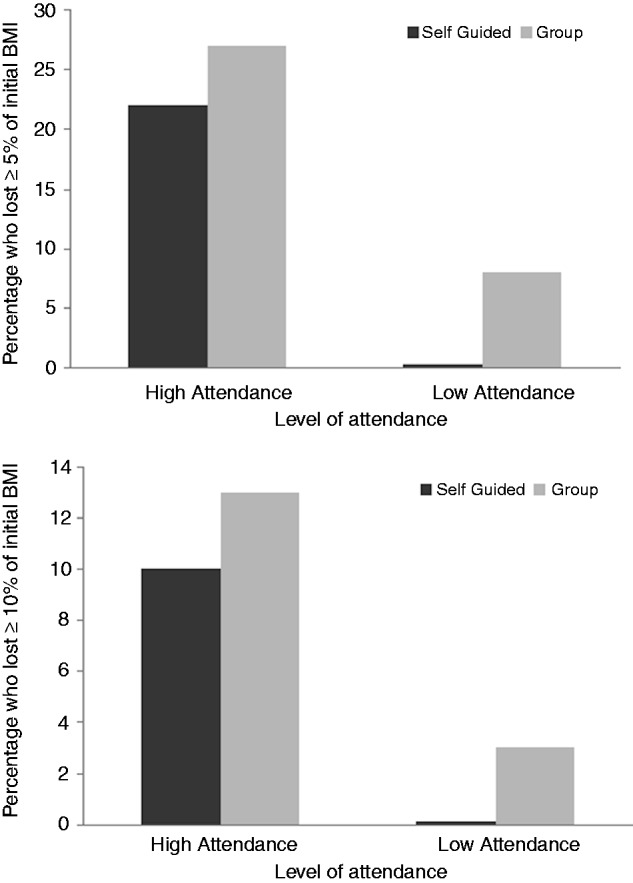
Median split demonstrating percentage of participants in Self-Guided and Group LMP who lost greater than 5% and greater than 10% of initial BMI at month 12 based on session attendance. For Self-Guided, attendance was defined as high (5–6 sessions) or low (≤4 sessions). For the Group condition, attendance was defined as high (18–23 sessions) or low (≤17 sessions). Attendance was significantly associated with achieving ≥5 or ≥10% BMI reduction from baseline to month 12 for both Self-Guided and Group LMP.
Discussion
The principal finding of this study was that an intensive LMP (Group LMP) and a less intensive home-based program (Self-Guided LMP) produced similar weight losses (i.e., percentage reduction in BMI) at 1 year. BMI decreased by 1.31% (0.95) and 1.17% (0.99), in the two groups, respectively. More than half the adolescents either lost weight or maintained their baseline BMI at month 12. The weight losses observed in the two conditions are similar to those observed in previous studies of lifestyle modification for adolescents with obesity (Barlow, 2007; McGovern et al., 2008; Oude Luttikhuis, et al., 2009; Whitlock, O'Connor, Williams, Beil, & Lutz, 2010). Of note, 18.5% of participants in the Group LMP and 12.5% of participants in the Self-Guided LMP lost 5% or more of their initial BMI (p = 0.29), a common criterion of success.
The Self-Guided LMP was specifically designed to be a brief in-clinic intervention (six sessions over 12 months) with primarily home-based behavior change efforts by adolescents and caregivers. This study is among the few tests of this approach compared with the more intensive Group LMP, which has been the gold standard in adolescent intervention studies. (Steele et al., also have recently developed a brief approach [Steele et al., 2012].) Our Self-Guided LMP may be useful for weight management in primary care, delivered by health coaches, as it required only six clinic visits, compared with 23 in the Group LMP. The present findings await replication to confirm the potential benefit of the Self-Guided LMP for youth with obesity treated in primary care.
Our hypothesis that the more intensive Group LMP would produce a greater reduction in initial BMI than Self-Guided LMP was not supported. A possible explanation is that the six Self-Guided LMP sessions, combined with families reviewing intervention materials at home, provided a critical threshold dose of therapy, similar to the more intensive in-clinic Group LMP. However, data regarding adherence to home sessions in the Self-Guided LMP are not available. In addition, the treatment was delivered primarily by professionals typically working in pediatric clinics (i.e., nurses, dietitians, and master’s level counselors) rather than primarily by doctoral level psychologists who are extensively trained in behavioral weight management.
Clinic session attendance (a measure of treatment adherence) in both LMP conditions was associated with significantly greater weight loss, using the 5 and 10% responder categories. Greater adherence to treatment is an important goal, as it appears to facilitate clinically significant weight loss (Berkowitz, Wadden, Tershakovec, & Cronquist, 2003; Wadden et al., 2005, 2009). Additional research is needed to identify methods to foster treatment adherence.
The strengths of the study include the treatment of medically underserved, urban African American and rural Caucasian adolescents from diverse geographic locations using an LMP designed to be implemented by staff typically working in pediatric primary care settings. One limitation of the current study was the higher level of attrition in the Self-Guided LMP compared with the Group LMP. Given the 75% retention rate in the Group LMP, future studies may seek to combine the successful components of the two treatment conditions to improve retention of adolescents receiving weight loss treatment. The study did not include youth with serious co-morbid conditions, such as diabetes mellitus or psychiatric illness (e.g., major depressive disorder, behavioral or academic problems), because we did not have the resources to provide appropriate pediatric or mental health care. Thus, our findings cannot be generalized to youth with more serious co-morbid conditions. Studies are needed which include youth with medical and psychiatric illness, as encountered in routine pediatric practices.
The present results for Self-Guided LMP provide initial support for using LMPs for adolescents with obesity in pediatric primary care settings where overall health care is coordinated. The use of the brief Self-Guided LMP with six clinic visits and materials to be reviewed in the home setting is consistent with the need for novel, practical interventions within pediatric primary care. This treatment model requires further study in larger community-based studies of typical patient populations. In addition, the Self-Guided LMP should be compared with other low-intensity interventions delivered using electronic media, including use of the Internet (Harvey-Berino et al., 2010; Tate, Jackvony, & Wing, 2003) and smartphones (Donnelly et al., 2007).
In summary, both the Group-LMP and Self-Guided LMP were effective in reducing BMI in adolescents with obesity. Given its brevity, the Self-Guided LMP offers an innovative, feasible, and potentially cost-effective approach to weight management that is adaptable for primary care settings. This efficient model may be broadly disseminated, yet tailored to the needs of individual families. Future research is needed to confirm the effectiveness of this approach and to extend the duration of treatment to facilitate the maintenance of weight loss.
Acknowledgments
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center for Research Resources or the National Institutes of Health. The authors acknowledge the diligence and perseverance of our study research coordinators and vital staff (Joanna Cronquist, Natalie Trumpikas, Priscilla Costa, Dorothy Moerlein, Chelsie Hauer, Cindy Grubb, and Samantha Crabbe). They also thank our statistical team (Jesse Chittams, Catherine Wilson, and Shaun Fernandes). Further, we would like to thank all the families who participated in this study.
Funding
This study was supported by grants SAP4100033130 (RIB) from the Pennsylvania Department of Health and K24-DK065018 (TAW) from the National Institutes of Health and grant UL1RR024134 from the National Center for Research Resources.
Conflicts of interest: None declared.
References
- Barlow S E. Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: Summary report. Pediatrics. 2007;120:S164–S192. doi: 10.1542/peds.2007-2329C. doi:DOI 10.1542/peds.2007-2329C. [DOI] [PubMed] [Google Scholar]
- Berkowitz R I, Wadden T A, Tershakovec A M, Cronquist J L. Behavior therapy and sibutramine for the treatment of adolescent obesity: A randomized controlled trial. JAMA. 2003;289:1805–1812. doi: 10.1001/jama.289.14.1805. doi:10.1001/jama.289.14.1805289/14/1805 [pii] [DOI] [PubMed] [Google Scholar]
- Butryn M L, Wadden T A, Rukstalis M R, Bishop-Gilyard C, Xanthopoulos M S, Louden D, Berkowitz R I. Maintenance of weight loss in adolescents: Current status and future directions. Journal of Obesity. 2010;2010:789280. doi: 10.1155/2010/789280. doi:10.1155/2010/789280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. A SAS program for the CDC growth charts. 2005. Retrieved from http://www.cdc.gov/nccdphp/dnpao/growthcharts/resources/sas.htm. [Google Scholar]
- Davis J N, Ventura E E, Tung A, Munevar M A, Hasson R E, Byrd-Williams C, Vanni A K, Spruijt-Metz D, Weigensberg M, Goran M I. Effects of a randomized maintenance intervention on adiposity and metabolic risk factors in overweight minority adolescents. Pediatric Obesity. 2012;7:16–27. doi: 10.1111/j.2047-6310.2011.00002.x. doi:10.1111/j.2047-6310.2011.00002.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeBar L L, Stevens V J, Perrin N, Wu P, Pearson J, Yarborough B J, Dickerson J, Lynch F. A primary care-based, multicomponent lifestyle intervention for overweight adolescent females. Pediatrics. 2012;129:e611–e620. doi: 10.1542/peds.2011-0863. doi:peds.2011-0863 [pii]10.1542/peds.2011-0863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dolinsky D H, Armstrong S C, Walter E B, Kemper A R. The effectiveness of a primary care-based pediatric obesity program. Clinical Pediatrics (Phila) 2012;51:345–353. doi: 10.1177/0009922811425232. doi:0009922811425232 [pii]10.1177/0009922811425232. [DOI] [PubMed] [Google Scholar]
- Donnelly J E, Smith B K, Dunn L, Mayo M M, Jacobsen D J, Stewart E E, Gibson C, Sullivan D K. Comparison of a phone vs clinic approach to achieve 10% weight loss. International Journal of Obesity (Lond) 2007;31:1270–1276. doi: 10.1038/sj.ijo.0803568. doi:0803568 [pii]10.1038/sj.ijo.0803568. [DOI] [PubMed] [Google Scholar]
- Epi Info. Database & statistics software for public health professionals. Atlanta, GA: Epidemiology Program Office at the Center for Disease Control and Prevention; 2002. [Google Scholar]
- Harvey-Berino J, West D, Krukowski R, Prewitt E, VanBiervliet A, Ashikaga T, Skelly J. Internet delivered behavioral obesity treatment. Preventive Medicine. 2010;51:123–128. doi: 10.1016/j.ypmed.2010.04.018. doi:S0091-7435(10)00173-8 [pii]10.1016/j.ypmed.2010.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jeffery R W, Sherwood N E, Brelje K, Pronk N P, Boyle R, Boucher J L, Hase K. Mail and phone interventions for weight loss in a managed-care setting: Weigh-To-Be one-year outcomes. International Journal of Obesity and Related Metabolic Disorders. 2003;27:1584–1592. doi: 10.1038/sj.ijo.0802473. doi:10.1038/sj.ijo.08024730802473 [pii] [DOI] [PubMed] [Google Scholar]
- Krebs N F, Jacobson M S. Prevention of pediatric overweight and obesity. Pediatrics. 2003;112:424–430. doi: 10.1542/peds.112.2.424. [DOI] [PubMed] [Google Scholar]
- Kwapiszewski R M, Lee Wallace A. A pilot program to identify and reverse childhood obesity in a primary care clinic. Clinical Pediatrics (Phila) 2011;50:630–635. doi: 10.1177/0009922811398389. doi:0009922811398389 [pii]10.1177/0009922811398389. [DOI] [PubMed] [Google Scholar]
- Lane-Tillerson C, Davis B L, Killion C M, Baker S. Evaluating nursing outcomes: A mixed-methods approach. Journal of National Black Nurses Association. 2005;16:20–26. [PubMed] [Google Scholar]
- McGovern L, Johnson J N, Paulo R, Hettinger A, Singhal V, Kamath C, Erwin PJ, Montori VM. Clinical review: Treatment of pediatric obesity: A systematic review and meta-analysis of randomized trials. The Journal of Clinical Endocrinology and Metabolism. 2008;93:4600–4605. doi: 10.1210/jc.2006-2409. doi:jc.2006-2409 [pii]10.1210/jc.2006-2409. [DOI] [PubMed] [Google Scholar]
- Moyer V A. Screening for and management of obesity in adults: U.S. Preventive Services Task Force recommendation statement. Annals of Internal Medicine. 2012;157:373–378. doi: 10.7326/0003-4819-157-5-201209040-00475. doi:1200996 [pii]10.7326/0003-4819-157-5-201209040-00475. [DOI] [PubMed] [Google Scholar]
- Nguyen B, Shrewsbury V A, O'Connor J, Steinbeck K S, Hill A J, Shah S, Kohn MR, Torvaldsen S, Baur LA. Two-year outcomes of an adjunctive telephone coaching and electronic contact intervention for adolescent weight-loss maintenance: The Loozit randomized controlled trial. International Journal of Obesity (Lond) 2012;37:468–472. doi: 10.1038/ijo.2012.74. doi:ijo201274 [pii]10.1038/ijo.2012.74. [DOI] [PubMed] [Google Scholar]
- Ogden C L, Carroll M D. NCHS Health EStat: Prevalence of obesity among children and adolescents: United States, Trends 1963-1965 Through 2007-2008. 2010. Retrieved from http://www.cdc.gov/nchs/data/hestat/obesity_child_07_08/obesity_child_07_08.pdf. [Google Scholar]
- Ogden C L, Carroll M D, Kit B K, Flegal K M. Prevalence of obesity and trends in body mass index among US children and adolescents, 1999-2010. JAMA. 2012;307:483–490. doi: 10.1001/jama.2012.40. doi:jama.2012.40 [pii]10.1001/jama.2012.40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oude Luttikhuis H, Baur L, Jansen H, Shrewsbury V A, O'Malley C, Stolk R P, Summerbell CD. Interventions for treating obesity in children. Cochrane Database of Systematic Reviews. 2009;1:CD001872. doi: 10.1002/14651858.CD001872.pub2. doi:10.1002/14651858.CD001872.pub2. [DOI] [PubMed] [Google Scholar]
- Saelens B E, Sallis J F, Wilfley D E, Patrick K, Cella J A, Buchta R. Behavioral weight control for overweight adolescents initiated in primary care. Obesity Research. 2002;10:22–32. doi: 10.1038/oby.2002.4. doi:10.1038/oby.2002.4. [DOI] [PubMed] [Google Scholar]
- Sothern M S, Von Almen T K, Schumacher H. Trim kids: The proven 12-week plan that has helped thousands of children achieve a healthier weight. New York: HarperResource; 2002. [Google Scholar]
- Steele R G, Aylward B S, Jensen C D, Cushing C C, Davis A M, Bovaird J A. Comparison of a family-based group intervention for youths with obesity to a brief individual family intervention: A practical clinical trial of positively fit. Journal of Pediatric Psychology. 2012;37:53–63. doi: 10.1093/jpepsy/jsr057. doi:jsr057 [pii]10.1093/jpepsy/jsr057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tate D F, Jackvony E H, Wing R R. Effects of Internet behavioral counseling on weight loss in adults at risk for type 2 diabetes: A randomized trial. JAMA. 2003;289:1833–1836. doi: 10.1001/jama.289.14.1833. doi:10.1001/jama.289.14.1833289/14/1833 [pii] [DOI] [PubMed] [Google Scholar]
- USDA. MyPyramid. 2009. Retrieved from www.mypyramid.gov. [Google Scholar]
- Wadden T A, Berkowitz R I, Womble L G, Sarwer D B, Phelan S, Cato R K, Hesson LA, Osei SY, Kaplan R, Stunkard AJ. Randomized trial of lifestyle modification and pharmacotherapy for obesity. The New England Journal of Medicine. 2005;353:2111–2120. doi: 10.1056/NEJMoa050156. doi:353/20/2111 [pii]10.1056/NEJMoa050156. [DOI] [PubMed] [Google Scholar]
- Wadden T A, Berkowtiz R I. Weight Reduction and Pride (WRAP) program: Parents' edition. Philadelphia: University of Pennsylvania; 2001. [Google Scholar]
- Wadden T A, Stunkard A J, Rich L, Rubin C J, Sweidel G, McKinney S. Obesity in black adolescent girls: A controlled clinical trial of treatment by diet, behavior modification, and parental support. Pediatrics. 1990;85:345–352. [PubMed] [Google Scholar]
- Wadden T A, West D S, Neiberg R H, Wing R R, Ryan D H, Johnson K C, Foryet K, Hill JO, Trence D, Vitolins M. One-year weight losses in the Look AHEAD study: Factors associated with success. Obesity (Silver Spring) 2009;17:713–722. doi: 10.1038/oby.2008.637. doi:oby2008637 [pii]10.1038/oby.2008.637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whitlock E P, O'Connor E A, Williams S B, Beil T L, Lutz K W. Effectiveness of weight management interventions in children: A targeted systematic review for the USPSTF. Pediatrics. 2010;125:e396–418. doi: 10.1542/peds.2009-1955. doi:peds.2009-1955 [pii]10.1542/peds.2009-1955. [DOI] [PubMed] [Google Scholar]
- World Health Organization. Measuring obesity: Classification and distribution of anthropometric data. Copenhagen: WHO. [Nutr Ud, Eur/ICP/Nut 125]; 1989. [Google Scholar]