Abstract
Background
It remains unclear whether the American College of Surgeons Committee on Trauma (ACSCOT) “step 1” field physiologic criteria could be further restricted without substantially sacrificing sensitivity. We assessed whether more restrictive physiologic criteria would improve the specificity of this triage step without missing high-risk patients.
Methods
We analyzed an out-of-hospital, consecutive patient, prospective cohort of injured adults ≥15 years collected from December 1, 2005, to February 28, 2007, by 237 emergency medical service agencies transporting to 207 acute care hospitals in 11 sites across the United States and Canada. Patients were included based on ACSCOT field decision scheme physiologic criteria systolic blood pressure ≤90, respiratory rate <10 or >29 breaths/min, Glasgow Coma Scale score ≤12, or field intubation. Seven field physiologic variables and four additional demographic and mechanism variables were included in the analysis. The composite outcome was mortality (field or in-hospital) or hospital length of stay >2 days.
Results
Of 7,127 injured persons, 6,259 had complete outcome information and were included in the analysis. There were 3,631 (58.0%) persons with death or LOS >2 days. Using only physiologic measures, the derived rule included advanced airway intervention, shock index >1.4, Glasgow Coma Scale <11, and pulse oximetry <93%. Rule validation demonstrated sensitivity 72% (95% confidence interval: 70%–74%) and specificity 69% (95% confidence interval: 67%–72%). Inclusion of demographic and mechanism variables did not significantly improve performance measures.
Conclusions
We were unable to omit or further restrict any ACSCOT step 1 physiologic measures in a decision rule practical for field use without missing high-risk trauma patients.
Keywords: Trauma, Physiologic, Emergency medical services, Out-of-hospital, Triage
Out-of-hospital trauma triage is the process of using field-based information to determine which patients require immediate transport to a trauma center. Although simple in concept, the practice of out-of-hospital triage is quite complex. Identification of high-risk injured patients in the field is based on limited information obtained during a relatively short period of time in an often chaotic setting, all of which contribute to an imperfect process. The original out-of-hospital trauma triage criteria were generated by national consensus conferences and published by the American College of Surgeons Committee on Trauma (ACSCOT) in 1976.1 The first “step” of these criteria includes physiologic measures, which are intended to identify the highest risk trauma patients. Target ranges for the three core physiologic measures (i.e., Glasgow Coma Scale [GCS] score, systolic blood pressure [SBP], and respiratory rate) have changed very little during the last 20 years.1,2 Although there have been numerous studies evaluating the out-of-hospital trauma triage guidelines,3-16 few studies have rigorously evaluated potential revisions of the ACSCOT step 1 physiologic criteria.
The current step 1 physiologic criteria are believed to identify the highest risk trauma patients,4,5,7,8,12,13 although questions persist regarding the utility of certain components of the criteria (e.g., respiratory rate), the ranges used, and whether additional physiologic measures would further improve predictive value. Previous studies assessing these measures have primarily focused on patients transported directly to major trauma centers, which can introduce selection bias and inflate the apparent predictive value of the criteria. The potential value of additional physiologic measures (e.g., shock index [pulse/SBP], pulse rate, and pulse oximetry) remains unclear, as does the relative utility of combining physiologic measures. Further, although out-of-hospital intubation has been suggested to be predictive of mortality and poor neurologic outcome,17 intubation is not explicitly included in the ACSCOT guidelines. Other authors have questioned field intubation as an indicator of resource need.18 Improving field triage guidelines may allow for more accurate selection of patients in need of immediate trauma center resources, identification of those most likely to benefit from early aggressive resuscitative care, and assist in selecting appropriate patients for field-based interventional therapies.
Among injured adults evaluated by emergency medical service (EMS) providers in 11 North American sites, we sought to (1) provide an unbiased estimate of the incidence of mortality and prolonged hospital stay among patients meeting ACSCOT step 1 field physiologic criteria and (2) assess whether more restrictive criteria (with or without demographic and mechanism information) would improve the specificity of this step without missing an excessive number of high-risk patients.
PATIENTS AND METHODS
Study Design
We analyzed an out-of-hospital, consecutive patient, prospective cohort registry of injured adults ≥15 years for whom field resuscitation was attempted and field-based physiologic abnormality was present.
Setting
These data were collected as part of the Resuscitation Outcomes Consortium (ROC) out-of-hospital epidemiologic trauma registry (the “ROC Epistry-Trauma”), described in detail elsewhere.19 Population-based data were collected from December 1, 2005, through February 28, 2007, by 237 EMS agencies transporting to 207 acute care hospitals (trauma and nontrauma centers) in 11 sites across the United States and Canada. The 11 participating sites included 8 US locations (Birmingham, AL; Dallas, TX; Iowa; Milwaukee, WI; Pittsburgh, PA; Portland, OR; San Diego, CA; and King County, WA) and 3 Canadian locations (Ottawa, Toronto, and Vancouver). The 11 sites vary in size (e.g., cities, counties, portions of states, and Canadian provinces), location, geographic diversity, and EMS system structure, and are described in detail in a separate publication.20 Overall, >36,000 EMS providers within these sites have varying certification levels and serve a combined population of ~23.7 million persons from diverse urban, suburban, rural, and frontier regions.
One hundred fifty-three Institutional Review Boards/Research Ethics Boards (127 hospital based and 26 EMS agency based) in both the United States and Canada reviewed and approved the ROC Epistry-Trauma project and waived the requirement for informed consent.
Selection of Participants
The study cohort consisted of consecutive injured adults (age ≥ 15 years) requiring activation of the emergency 9-1-1 system within predefined geographic regions at each ROC site. To be included in the cohort, patients must have received EMS provider evaluation and met any of the following field-based physiologic inclusion criteria at any point during out-of-hospital evaluation: SBP ≤90 mm Hg, respiratory rate <10 or >29 breaths per minute, GCS ≤12, or field intubation. The inclusion criteria were based on ACSCOT “step 1” field trauma triage guidelines that have previously demonstrated high specificity for serious injury and need for specialized trauma resources.3-16 “Injury” was broadly defined as any blunt, penetrating, or burn mechanism where the EMS provider(s) thought trauma to be the primary clinical insult. Injured persons meeting the above criteria were included in the study regardless of subsequent events (e.g., transport), the type of hospital to which they were transported (i.e., trauma center vs. nontrauma center), whether they were subsequently transferred to another acute care hospital, hospital admission, or injury severity. The absence of such additional, non–field-based inclusion criteria is a distinction of the Epistry sampling design relative to most trauma registries and provides a relatively unbiased cohort of injured patients with out-of-hospital physiologic abnormality and EMS evaluation.
Patients judged by EMS responders to be dead on EMS arrival and therefore had no resuscitation attempted were excluded from this analysis. Children (younger than 15 years) were also excluded from the analysis due to different responses to injury, different “normal” physiologic ranges, age-based variability in EMS procedure use (e.g., intubation), and differing implications and application of triage processes relative to adults. The dates for enrollment and resulting sample size were based on the initial inception of the ROC Epistry-Trauma database (December 1, 2005) through the most recent date demonstrating complete case capture and a high rate of outcome completion (February 28, 2007).
Methods of Measurement
Eleven out-of-hospital variables routinely collected by field providers were included in the analysis. These variables included seven physiologic measures: SBP (mm Hg), respiratory rate (breaths/min), GCS, pulse rate (bpm), pulse oximetry (percentage oxyhemoglobin saturation), shock index (pulse rate/SBP), plus need for an advanced airway management (attempted intubation, supraglottic airway, or cricothyrotomy) at any point during the field evaluation. The primary analysis was based on initial physiologic measures to minimize the potential bias inherent in analyzing subsequent values (e.g., sicker patients or those with longer transport times may be more likely to have repeat vital signs), to avoid the difficulty in interpreting vital signs recorded after EMS interventions (e.g., intravenous fluid, use of sedatives or paralytics, and intubation), and because many triage/transport decisions need to be made shortly after the initial field assessment. However, as a supplemental analysis, we assessed the “worst” out-of-hospital physiologic values (either on-scene or en route) to examine the extent to which considering only the initial vitals may have lead to misclassification of patients due to deteriorating clinical status after the initial assessment.
Four nonphysiologic measures were also assessed to determine whether the inclusion of such variables would improve the predictive value of field physiologic measures: age (years), sex, mechanism of injury (motor vehicle, cyclist or pedestrian, stabbing or firearm, machinery, fall, and others), and type of injury (blunt vs. penetrating). Continuous variables (SBP, respiratory rate, GCS, pulse rate, pulse oximetry, shock index, and age) were maintained in continuous form to avoid selecting arbitrary categorizations. The additional four variables were included as categorical terms.
Data Collection and Processing
All variables were collected by on-site EMS providers, rather than based on information provided after in-hospital evaluation. Investigative teams at each ROC site identified eligible out-of-hospital trauma patients from participating EMS agencies at the site. Standardized data were collected from each agency at regular intervals, processed locally, entered into standardized data forms (web-based data entry or batch upload), matched to hospital outcomes, deidentified, and submitted to a central data coordinating center. Quality assurance processes at ROC sites included EMS provider data collection training; continuing education of field providers for certain variables and their definitions (e.g., GCS score); data element range and consistency checks in both the web-based data entry forms and batch upload processes; and annual site visits to review randomly selected study records, data capture processes, and site-specific mechanisms for quality assurance.19
Outcome Measures
The primary outcome was mortality (whether out-of-hospital after resuscitative efforts or in-hospital) or hospital length of stay (LOS) >2 days. In this article, patients who died or had LOS >2 days are referred to as “high risk,” whereas survivors with a 0 day to 2 days hospital stay are considered “low risk.” Although a portion of early deaths (after resuscitation efforts) likely represented cases where further care was futile or where injuries were nonsurvivable regardless of aggressive care, we opted to include such patients in the analysis to minimize the potential for selection bias and because triage decisions need to be made before the outcome is known. Also, a portion of such fatalities may have been preventable with early aggressive trauma care, interventional therapies, or timely surgery. Hospital LOS was included in the composite outcome to serve as a surrogate marker for more serious injuries and the need for specialized trauma care among survivors (i.e., surgical intervention, blood transfusion, intensive care unit stay, prolonged ventilation). More detailed hospital-based outcomes were not available in Epistry due to resource constraints. The >2-day measure was intended to exclude survivors who were admitted for “observation” with limited or no interventions and therefore unlikely to have required immediate trauma center care (i.e., those with minor injuries); this LOS value has been used in previous trauma research.7 The discriminatory accuracy of LOS for identifying survivors with serious injury or resource use has been validated among injury cohorts with different rates of injury severity and interventions.21
Primary Data Analysis
We used descriptive statistics to compare field physiology between low- and high-risk patients. We then used binary recursive partitioning to derive a decision rule using out-of-hospital factors highly predictive of high-risk patients (death or LOS >2 days). Recursive partitioning is an analytic method well suited for identifying complex, higher-level interactions among variables, selecting appropriate cut points in continuous predictors, and generating highly sensitive decision rules.22,23 Misclassification costs were selected with a goal of producing a decision rule with high sensitivity (90% or greater) and moderate specificity (50% or greater) that was also practical for field application. We randomly selected 60% of the sample to derive the rule and used the remaining 40% of subjects for rule validation. The primary analysis was restricted to the seven physiologic measures to remain consistent with the “physiologic” step 1 of the ACSCOT field decision scheme.2 In a supplemental analysis, four additional variables (age, sex, injury mechanism, and injury type) were also included to assess whether such additional factors would improve performance of the resulting decision rule.
We used several strategies to minimize bias in the analysis. First, the monthly ROC Epistry-Trauma case enrollment was continually evaluated during data collection for each site, as well as for individual EMS agencies within each site. Sites or agencies that had substantially higher or lower case capture (relative to their average) for a given month, as determined using a Poisson distribution with a 5% cutoff, were sent inquiries in an attempt to understand whether such fluctuations were secondary to natural variation and other explainable trends versus being due to biased case capture. These assessments were used to improve identification of eligible patients and to select a time period for this sample when appropriate case capture was uniformly present.
To handle missing values in the database, we used a variety of methods, including: “surrogate splits” (a technique where a surrogate variable highly correlated with the primary splitter is used when the primary predictor is missing), single imputation, and coding missing values for a given variable in a separate predictor term (a missingness indicator) to assess whether missingness itself serves as a predictor of the outcome in the sample. Although effective in other settings, multiple imputation was not used in this analysis due to the difficulty in combining decision trees across multiply imputed datasets. Sensitivity analyses were performed using the different strategies for handling missing values to assess the potential impact of missing data on study results. For none of these analyses did the indicator of missingness enter the decision rule.
All analyses performed for this article used R v2.4.0 and the rpart library v3.1-32 (Free Software Foundation, Boston MA).
RESULTS
There were 7,127 out-of-hospital adult trauma patients meeting the physiologic inclusion criteria and having EMS field resuscitation during the 15-month period. Seven hundred twenty-four (10.2%) patients had missing outcome information and an additional 144 (2.0%) persons were enrolled in a concurrent clinical trial with embargoed outcomes. After excluding these patients, 6,259 persons had complete outcome information and were retained for the analysis. One thousand four hundred seventy-three (23.5%) patients died after EMS resuscitative efforts, of which 290 (19.7% of deaths) died in the field and were not transported. The incidence of mortality or hospital LOS greater than 2 days was 58.0% (3,631 patients) in the sample. Twenty-seven percent (1,682 patients) of the sample were discharged alive on the same day of evaluation.
Descriptive characteristics of the cohort and rates of physiologic derangement between high- and low-risk patients are provided in Table 1. The sample was predominantly young and male. The four core physiologic measures (GCS ≤12, SBP ≤90 mm Hg, respiratory rate >29 or <10, and intubation) demonstrated several differences when comparing high- and low-risk trauma patients. The use of advanced airway intervention was seen in 21% of the total sample; 32% of high-risk patients required advanced airway management versus 5% of the low-risk group. Abnormal respiratory rates were also more pronounced in the high-risk patient group (23% vs. 17%). Alternatively, field hypotension was more common in low-risk patients (40% vs. 29%). Depressed GCS was the most common physiologic abnormality among high-risk patients (54% vs. 38%). Rates of penetrating injury were more common among high-risk patients (21% vs. 11%).
TABLE 1.
Characteristics of Injured Persons With Field Physiologic Abnormality (n = 6,259)*
| Total (N = 6,259) |
“Low Risk” (Alive and LOS 0–2 d) (N = 2,628) |
“High Risk” (Death or LOS >2 d) (N = 3,631) |
|
|---|---|---|---|
| Out-of-hospital characteristics | |||
| Age (yrs) | 44.5 (21.7) | 44.0 (21.9) | 45.0 (21.5) |
| Male | 4,244 (67.8%) | 1,598 (60.8%) | 2,646 (72.9%) |
| Mechanism of injury (%) | |||
| Motor vehicle | 1,689 (27.0) | 602 (22.9) | 1,087 (29.9) |
| Cyclist or pedestrian | 561 (8.96) | 161 (6.13) | 400 (11.0) |
| Stabbing or firearm | 984(15.7) | 263 (10.0) | 721 (19.9) |
| Machinery | 32 (0.51) | 19 (0.72) | 13 (0.36) |
| Fall | 1,975 (31.6) | 1,027 (39.1) | 948 (26.1) |
| Others | 899 (14.4) | 512 (19.5) | 387 (10.7) |
| Penetrating injury type (%) | 1,045 (16.7) | 290 (11.0) | 755 (20.8) |
| Sites (anonymized) (%) | |||
| Site A | 6(0.1) | 1 (0.04) | 5 (0.14) |
| Site B | 370 (5.91) | 38 (1.45) | 332 (9.14) |
| Site C | 541 (8.64) | 197 (7.5) | 344 (9.47) |
| Site D | 1,331 (21.3) | 720 (27.4) | 611 (16.8) |
| Site E | 348 (5.56) | 131 (4.98) | 217 (5.98) |
| Site F | 236 (3.77) | 84 (3.2) | 152 (4.19) |
| Site G | 302 (4.83) | 119 (4.53) | 183 (5.04) |
| Site H | 1,398 (22.3) | 762 (29.0) | 636 (17.5) |
| Site I | 608 (9.71) | 243 (9.25) | 365 (10.1) |
| Site J | 512 (8.18) | 150 (5.71) | 362 (9.97) |
| Site K | 607 (9.7) | 183 (6.96) | 424(11.7) |
| Out-of-hospital physiologic characteristics (%) | |||
| GCS ≤12 | 2,937 (46.9) | 996 (37.9) | 1,941 (53.5) |
| SBP ≤90 mm Hg | 2,085 (33.3) | 1,049 (39.9) | 1,036 (28.5) |
| Respiratory rate <10 or >29 | 1,289 (20.6) | 447 (17.0) | 842 (23.2) |
| Advanced airway | 1,294 (20.7) | 121 (4.6) | 1,173 (32.3) |
| Single physiologic criteria for entry to the study sample (%) | 4,184 (66.8) | 2,194 (83.5) | 1,990 (54.8) |
| GCS ≤12 | 1,679 (26.8) | 826 (31.4) | 853 (23.5) |
| SBP ≤90 mm Hg | 1,519 (24.3) | 960 (36.5) | 559 (15.4) |
| Respiratory rate <10 or >29 | 581 (9.28) | 363 (13.8) | 218 (6.0) |
| Advanced airway | 405 (6.47) | 45 (1.71) | 360 (9.91) |
| Additional physiologic information | |||
| Pulse rate (beats/min) | 90.2 (28.7) | 91.1 (22.5) | 89.4 (33.1) |
| Shock index (pulse/SBP) | 0.87 (0.38) | 0.86 (0.29) | 0.89 (0.46) |
| Pulse oximetry | 95.0 (10.5) | 97.2 (4.15) | 93.1 (13.6) |
Values presented are n (%) or mean (SD) for categorical and continuous covariates, respectively.
Advanced airway use included any of the following: intubation (oral or nasopharyngeal), supraglottic airway (e.g., combitube), or cricothyrotomy.
Two thirds of the cohort was included based on a single physiologic inclusion criterion (Table 1). This scenario was more common among low-risk patients (84%) than among high-risk patients (55%). The most common isolated physiologic abnormality among low-risk patients was SBP ≤90 mm Hg (37%), whereas only 16% of high-risk patients had hypotension as the sole inclusion criteria. There was a similar pattern demonstrated for abnormal field respiratory rate, with 14% of low-risk and 6% of high-risk patients having an abnormal respiratory rate as the sole measure of physiologic impairment. This pattern was switched for advanced airway management, with 2% of low-risk patients and 10% of high-risk patients requiring airway management without other coexistent physiologic abnormality.
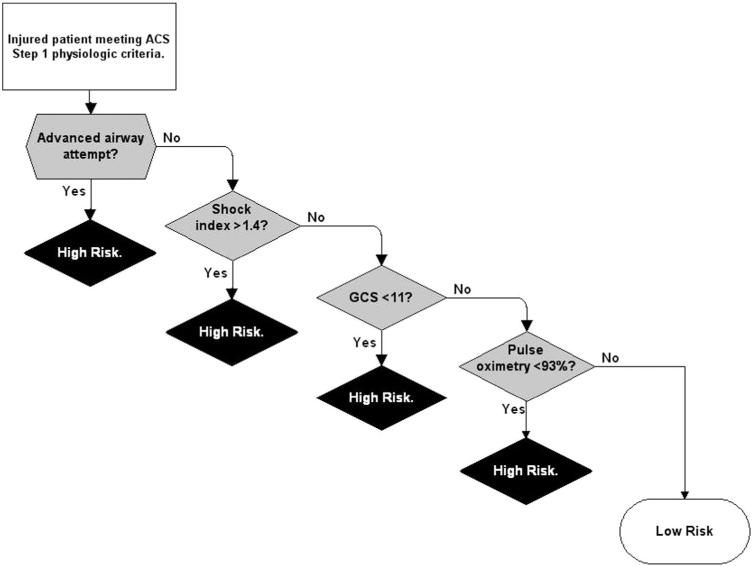
The results of examining whether more restrictive criteria could be implemented to improve the specificity of the ACSCOT step 1 criteria without missing high-risk patients are presented in Figure 1. Using the seven physiologic measures, the primary decision tree included the following four covariates: advanced airway intervention, shock index >1.4, GCS <11, and pulse oximetry <93% (Fig. 1). Additional splits were not included to maintain a parsimonious decision rule and to avoid instability observed when small portions of the test set were excluded. For the primary outcome, rule validation demonstrated sensitivity 72% (95% confidence interval: 70%–74%) and specificity 69% (95% confidence interval: 67%–72%; Table 2). In a supplemental analysis that included the seven physiologic measures plus four additional demographic and mechanism factors, the results did not qualitatively change. Sensitivity analysis using different methods for handling missing values did not substantially alter these results. Evaluation of the “worst” physiologic values changed the predicted risk group in 42 (1.7%) patients, raising sensitivity by 2.0% and lowering specificity by 1.2%.
Figure 1.
Clinical decision rule to identify high-risk trauma patients (mortality or length of stay >2 days) meeting ACSCOT step 1 criteria (validation set, n = 2,504) (event and nonevent numbers/proportions correspond to each end-node of the tree). *ACS = American College of Surgeons Committee on Trauma. Event = mortality (either field based after resuscitative efforts or in-hospital) or hospital length of stay greater than 2 days. Nonevent = survival with hospital length of stay 0 to 2 days.
TABLE 2.
Summary Accuracy Measures of the Clinical Decision Tree Using the Validation Sample (n = 2,504)*
| Estimate (95% Confidence Interval) | |
|---|---|
| Sensitivity | 0.72 (0.70–0.74) |
| Specificity | 0.69 (0.67–0.72) |
| Positive predictive value | 0.77 (0.74–0.79) |
| negative predictive value | 0.64 (0.61–0.67) |
| Positive likelihood ratio | 2.36 (2.13–2.59) |
| Negative likelihood ratio | 0.40 (0.37–0.44) |
The same decision tree (and accuracy measures) was generated when using only physiologic predictors or both physiologic and demographic predictors.
The overall proportion of missing values for the core physiologic measures were 18% for GCS, 16% for SBP, and 13% for respiratory rate. Interestingly, the pattern of missing values differed by outcome, with a higher rate among high-risk patients (GCS 21%, SBP 24%, and respiratory rate 20%) than among low-risk patients (GCS 14%, SBP 4%, and respiratory rate 4%).
DISCUSSION
In this study, we demonstrate a relatively high incidence of mortality and prolonged hospital stay among injured persons meeting ACSCOT step 1 physiologic criteria. However, there were a substantial number of patients with presumably minor injuries that were discharged alive on the same day of evaluation. The finding that 42% of patients meeting physiologic triage criteria (assumed to represent the highest acuity trauma patients) were discharged within 2 days is higher than we anticipated. In assessing whether the step 1 physiologic criteria could be further restricted (either by using more extreme physiologic cutoff values, different physiologic measures, or fewer physiologic measures), we were unable to generate a decision rule with improved specificity that was practical for field use without missing a substantial portion of high-risk patients.
Requirement for advanced airway intervention is not specifically noted in the ACSCOT step 1 criteria, however, we confirm here that such patients represent a very high-risk group, whether or not other physiologic abnormalities are present. This association has been noted in previous studies.17,24,25 Although patients requiring intubation may be inferred to have a high or low respiratory rate (therefore meeting the ACSCOT criteria), this may not always be the case. In this sample, 10% of the high-risk group had intubation as the sole reason for inclusion in the sample (i.e., did not meet any other physiologic triage criteria). These findings suggest that, despite research demonstrating variability in the use of field intubation26 and mixed use of rapid sequence intubation (RSI) among sites included in this sample, the need for advanced airway management provides prognostic information beyond standard measures of brain function (GCS) and respiratory rate. However, if EMS providers broaden the indications for or simply use airway procedures more frequently, this prognostic value may decline. Although the causal association between field intubation and adverse outcomes continues to be debated, it is likely that the selection of patients for advanced airway intervention (rather than simply the procedure itself) plays a substantial role in its predictive value.
It was also interesting to note the high rate of field hypotension in low-risk patients (particularly in patients where hypotension was the sole physiologic abnormality qualifying for inclusion in the sample). These findings are in contrast to the broad clinical use of low SBP as a clinical indicator of “shock”27 and previous studies suggesting field hypotension to be a useful marker of serious injury, mortality, and resource use.7,12,14,28-32 Possible explanations for this finding include the higher rate of missing data for SBP among high-risk patients (e.g., it is possible that such patients were too sick to have a SBP recorded) and the unbiased sampling design of Epistry. Because patients in Epistry were not sampled based on hospital destination, hospital admission, injury severity, or other nonfield measures (any of which may integrate selection bias and inflate the apparent predictive value of certain field measures), our findings may better approximate the true predictive value of field physiology. This sampling design contrasts with previous studies evaluating the predictive value of hypotension among patients transported directly to trauma centers.14,28-32 In a recent phase II out-of-hospital trial of hypertonic saline and dextran for hypovolemic shock after blunt trauma, a single field measurement of SBP ≤90 mm Hg was not found to be specific enough for identifying significant blood loss (45% of patients did not require transfusion in the first 24 hours).33 These findings prompted a change in the physiologic inclusion criteria for shock in a similar out-of-hospital trial to SBP ≤70 mm Hg or SBP 71 mm Hg to 90 mm Hg with heart rate ≥108 bpm.34 Combining pulse rate with SBP (i.e., shock index) was useful in identifying high-risk patients in our final decision tree, particularly for patients who did not require intubation. Previous research suggests that shock index may have a role in predicting injury severity and resource need.35 Based on our results, the presence of isolated hypotension may be less predictive of high-risk trauma patients than previously thought. Other physiologic measures used in previous trauma triage research (radial pulse character,29,36 heart rate complexity,37 and tissue oxygen saturation38) were not evaluated in this study.
Field GCS and pulse oximetry provided additional prognostic value for identifying high-risk patients in this sample. The predictive value of out-of-hospital GCS has been demonstrated in several previous studies.7,12,13 Although the order and selection of predictor terms for decision trees can fluctuate when using recursive partitioning, GCS was most useful among nonintubated patients with relatively stable hemodynamic status in this sample. Similarly, pulse oximetry was identified as a predictive term that may have a role in identifying high-risk patients not otherwise detected by other physiologic markers. This finding contrasts with a previous study suggesting that pulse oximetry does not add predictive value beyond other vital signs and pulse character for identifying patients requiring “life-saving interventions.”29 It is also noteworthy that additional field information (i.e., demographics and mechanism of injury) did not change these results. Although it seems intuitive that patients with certain types of injuries (e.g. penetrating injuries) or within certain demographic groups (e.g. elders) may have different physiologic cut points for identifying high-risk patients, our results did not support such hypotheses.
Based on these results, trauma patients meeting the ACSCOT step 1 physiologic criteria or requiring field airway management should continue to be regarded as high-risk patients warranting trauma center evaluation, although a portion of such patients will have no serious injury. Although certain physiologic markers appear less useful in identifying high-risk persons, especially when present in isolation (e.g., hypotension and respiratory rate), our results suggest that omitting such measures from the ACSCOT step 1 criteria will miss high-risk patients. It is possible that such “missed” patients may be captured by steps 2 to 4 of the decision scheme (anatomic, mechanism, and risk factor criteria), however, the ability of additional steps in the decision scheme to capture such patients will require a broader population to assess.
There were limitations in this study. The inclusion criteria for the sample were very similar to the current ACSCOT step 1 physiologic criteria. However, restricting the sample to patients with physiologic abnormality eliminated the ability to assess whether the use of broader ranges of physiologic parameters would better identify the high-risk population of interest. Therefore, the findings in this study only apply to those patients meeting ACSCOT step 1 criteria. In addition, development of the decision trees was restricted by the need for enough simplicity to allow practical field implementation of subsequent results; this restriction further reduced the ability to produce a high sensitivity tree.
We were unable to directly assess other commonly used injury outcomes (e.g., injury severity, specific types of injury, and resource use). As previously noted, the ROC Epistry-Trauma database does not capture such measures. In addition to patients who died, including LOS >2 days in the outcome provided a surrogate measure for serious injury and the need for specialized trauma resources. The use of LOS in the composite outcome and the specific cut point used are supported by results from an external validation of LOS,21 although the use of such a surrogate measure does integrate variability and the potential for misclassification to the outcome.
For the field airway intervention term, some patients undergoing field intubation may not have had serious injury (e.g., heavily intoxicated patients) and yet received an intervention that prolonged their hospital stay, thus potentially inflating the predictive value of this term. Because the association between field intubation and adverse outcomes has been demonstrated in many previous studies,17,24,25 we think the likelihood of substantially inflating the predictive value was minimal. In addition, we did not separate out patients who had RSI from those who did not because RSI was only used by a portion of agencies in a minority of sites (i.e., use of RSI was not universally available across sites or EMS agencies). We cannot tell whether a portion of patients intubated with the assistance of RSI at one site would not have been intubated at another site that did not have RSI available. If this phenomenon was common, it would have potentially biased the predictive value of the advanced airway term. Despite these possibilities, attempted advanced airway intervention remained a strong predictor of high-risk patients and should be considered an explicit criterion in subsequent versions of ACSCOT step 1 criteria.
Patients with missing outcomes or enrolled concurrently in a clinical trial34 were omitted from the analysis. In addition, high-risk patients had a higher proportion of missing values for key physiologic measures (e.g., SBP). The omission of certain patients or the presence and pattern of missing outcome data could have altered our results. Although we used several analytic strategies to reduce the potential for bias (sampling design, close assessment of case capture, quality assurance processes, and analytic strategies), it is possible that such factors influenced our results.
CONCLUSIONS
We confirm the high-risk nature of injured patients meeting the ACSCOT step 1 physiologic criteria in a broad, unbiased EMS sample. However, there was a substantial portion of patients with field physiologic abnormality discharged alive on the same day of evaluation. Although not explicitly included in the ACSCOT criteria, attempted advanced airway management in the field was the most prominent indicator of mortality and prolonged hospital stay among patients meeting step 1 criteria. After critical assessment of step 1 criteria, we were unable to omit or further restrict any physiologic measures without missing high-risk trauma patients in this sample.
ACKNOWLEDGMENTS
We acknowledge and thank the many contributing EMS agencies, EMS providers, study coordinators, staff, and investigators (see Appendix 1) for their willingness to participate in and support this project, and for their continued dedication to improving the EMS care and outcomes for their patients.
The Resuscitation Outcome Consortium (ROC) is supported by a series of cooperative agreements to 10 regional clinical centers and one data Coordinating Center (5U01 HL077863, HL077881, HL077871 HL077872, HL077866, HL077908, HL077867, HL077885, HL077877, and HL077873) from the National Heart, Lung. and Blood Institute in partnership with the National Institute of Neurological Disorders and Stroke, U.S. Army Medical Research and Material Command, The Canadian Institutes of Health Research (CIHR)—Institute of Circulatory and Respiratory Health, Defence Research and Development Canada, the Heart and Stroke Foundation of Canada, and the American Heart Association.
APPENDIX: ROC EPISTRY CONTRIBUTORS
(Please go to the ROC website at www.uwctc.org and click on ROC for additional acknowledgments).
Alabama Resuscitation Center, University of Alabama at Birmingham, Birmingham, AL: Jeffrey D. Kerby, MD, PhD, Principal Investigator; Core Investigators: Todd B. Brown, MD, MSPH, Thomas Terndrup, MD; Coordinators: Shannon W. Stephens, EMT-P, Carolyn R. Williams, BSN, BSME; EMS Investigators/Collaborators: Joe E. Acker, EMT-P, MPH, Michael L. Minor, EMT-P; Hospital Investigators/Collaborators: Paul A. MacLennan, PhD, Patrick R. Pritchard, MD, Sandra Caldwell, MA, Katherine R. Lai, BS; Participating EMS Agencies: Alabama LifeSaver, Bessemer Fire and Rescue, Birmingham Fire and Rescue, Center Point Fire District, Chelsea Fire and Rescue, American Medical Response, Homewood Fire Department, Pelham Fire Department, Rocky Ridge Fire Department, Regional Paramedic Services, Trussville Fire Department, Vestavia Hills Fire and Rescue; Dallas Center for Resuscitation Research, University of Texas Southwestern Medical Center, Dallas, TX: Ahamed H. Idris, MD, Principal Investigator; Core Investigator: Fernando Benitez, MD, Raymond Fowler, MD, Dorothy Lemecha, MD, Joseph Minei, MD, Paul Pepe, MD, Michael Ramsay, MD, Robert Simonson, MD, Jane Wigginton, MD; Coordinators: Dixie Climer, RN, Melinda Moffat, RN, Kate Newman, RN, Pamela Owens, Andrea Bennett, BS; EMS Investigators/Collaborators: Richard Black, EMT-P, Debra Cason, RN, Billy Craft, EMT-P, Lucy Detamble, RN, Ryan Dykes, EMT-P, Tony Harvey, EMT-P, Suzanne Hewitt, RN, Marshal Isaacs, MD, Joe Kay, EMT-P, Tami Kayea, EMT-P, Richard LaChance, EMT-P, Thomas Lehman, Paul Mayer, MD, Jeffrey Metzger, MD, Danny Miller, EMT-P, Kenneth Navarro, EMT-P, Steven Parker, EMT-P, Karen Pickard, RN, Warren Porter, EMT-P, TJ Starling, EMT-P, Tommy Tine, EMT-P, Chris Vinson, EMT-P; Hospital Investigators/Collaborators: David Abebefe, MD, Steven Arze, MD, Sean Black, MD, Matthew Bush, MD, Michael Forman, MD, Jeffery Goodloe, MD, Ralph Kelly, DO, Gregory Lachar, MD, Alicia Mangram, MD, Marc Morales, MD, Edward Thornton, MD, Robert Wiebe, MD; Participating EMS Agencies: Carrollton Fire Department, Dallas Fire and Rescue, DeSoto Fire Department, Duncanville Fire Department, Farmers Branch Fire Department, Garland Fire Department, Highland Park Department of Public Safety, Irving Fire Department, Lancaster Fire Department, Mesquite Fire Department, Plano Fire Department, University Park Fire Department; University of Iowa Carver College of Medicine-Iowa Resuscitation Network, University of Iowa, IA City, IA: Richard Kerber, MD, Principal Investigator; Core Investigators: Steve Hata, MD, Dianne Atkins, MD; Coordinators: Melanie Kenney, RN, MA, CPNP, Catherine Rost, Alexander Drum, EMT-P, Michael Hartley, EMT-P; Participating EMS Agencies: Area Ambulance Service, Davenport Hospital Ambulance Corporation, Covenant Health System—Covenant Ambulance, Covenant Health System—Mercy Oelwein, Covenant Health System—Sartori, City of Dubuque Fire Department, Dallas County Emergency Medical Services, West Des Moines Emergency Medical Services, Des Moines Fire Department EMS, Henry County Health Center Emergency Medical Services, Johnson County Ambulance, Siouxland Paramedics, Inc., Waterloo Fire Rescue; Milwaukee Resuscitation Research Center, Medical College of Wisconsin, Milwaukee, WI; Tom P. Aufderheide, MD, Principal Investigator; Core Investigators: Ronald G. Pirrallo, MD, MHSA, Karen J. Brasel, MD, MPH, Andrea L. Winthrop, MD, John P. Klein, PhD; Coordinators: David J. Kitscha, BS, MS, Barbara J. Burja, BA, EMT, Chris von Briesen, BA, CCRC, Christopher W. Sparks, EMT, Sara Kaebisch, BS; EMS Investigators/Collaborators: John Chianelli, MS, Rosemarie Forster, MSOLQ, RHIA, EMT-P, Michael Milbrath, EMT-P, Lauryl Pukansky, BS, RHIA, Kenneth Sternig, MS-EHS, BSN, EMT-P, Eugene Chin, RN, EMT-P, Nancy Frieberg, RN, EMT-P, Kim Krueger, RN, EMT-P, Del Szewczuga, RN, EMT-P Thomas Duerr, Rebecca Funk, BS, RHIA, EMT-B, Gail Jacobsen, BS, Janis Spitzer, Richard Demien, James Martins, John Cohn, Russell R. Spahn, MA, EMT-P, Mike Jankowski, BA, EMT-P, Timothy James, William E. Wentlandt Jr., MBA, EFO, David Berousek, Brian M. Satula, BA, NREMT, Jay B. Behling, BS, EMT-B, Dean K. Redman, BA, EFO, Steven Hook, BS, CFOD, Andrew Neargarder, Jim Singer, RN; Hospital Investigators/Collaborators: Thomas Reminga, MD, Dennis Shepherd, MD, Peter Holzhauer, MD, Jonathan Rubin, MD, Craig Skold, MD, Orlando Alvarez, MD, Heidi Harkins, MD, Edward Barthell, MD, William Haselow, MD, Albert Yee, MD, John Whitcomb, MD, Eduardo E. Castro, MD, Steven Motarjeme, MD; Participating EMS Agencies: Cudahy Fire Department, Flight for Life, Franklin Fire Department, Greendale Fire Department, Greenfield Fire Department, Hales Corners Fire Department, Milwaukee County Airport Fire Department, Milwaukee Fire Department, North Shore Fire Department, Oak Creek Fire Department, South Milwaukee Fire Department, St. Francis Fire Department, Wauwatosa Fire Department, West Allis Fire Department; Ottawa/OPALS/British Columbia RCC, Ottawa Health Research Institute, University of Ottawa, Ottawa, Ontario and St. Paul’s Hospital, University of British Columbia, British Columbia, Canada: Ian Stiell, MD, Principal Investigator; Core Investigators: Jim Christenson, MD, Morad Hameed, MD, Jean Denis Yelle, MD, Martin Osmond, MD, Christian Vaillancourt, MD, David Evans, MD, Riyad Abu-Laban, MD; Coordinators: Cathy Clement, RN, Tammy Beaudoin, CCHRA, Barb Boychuk, RN, Sarah Pennington, RN, Helen Connolly, RN, Patrick Lefaivre, PCP, Jane Banek, CCHRA, Angela Marcantonio, Rina Marcantonio, CCHRA, Christine Leclair, RN, Julie Cummins, RN; EMS Investigators/Collaborators: Matthew Stempien, MD, Jonathan Dreyer, MD, Douglas Munkley, MD, Justin Maloney, MD, Paul Colella, MD, Andrew Affleck, MD, David Waldbillig, MD, Paul Bradford, MD, Martin Lees, MD, Vincent Arcieri, MD, Ann Wilson, BSc, ACP, Kenneth Boyle, EMCA, RRT, CMA, Lorraine Luinstra-Toohey, BScN, MHA, John Trickett, BScN, Nicole Sykes, BScN, RN, Elaine Graham, ACP, Kieran Ballah, EMCA, Cathy Hedges, A-EMCA, ACP, Paul Mathers, A-EMCA, Dug Andrusiek, MSc, Dan Bishop, ACP, Ron Straight, ACP, Brian Twaites, ACP, Stuart Donn, PhD; Participating EMS Agencies: A.A. and M. Volunteer Ambulance Service, Burlington Fire and Rescue, Cambridge Fire Department, Cornwall Fire and Rescue, Cornwall SDG Emergency Medical Services, Essex-Windsor Emergency Medical Services, Essex-Windsor Fire and Rescue, Frontenac Paramedic Service, Halton Emergency Medical Services, Harrow Ambulance Service Ltd., Kawartha Lakes Emergency Medical Services, Kawartha Lakes Fire and Rescue, Kingston Fire and Rescue, Kitchener Fire Department, Lambton County Emergency Medical Services, Lasalle Fire Department, London Fire Department, Niagara Emergency Medical Services, Niagara Falls Fire and Rescue, Northumberland Emergency Medical Service, Oakville Fire Department, Ottawa Fire and Rescue, Ottawa Paramedic Service, Peterborough Emergency Medical System, Peterborough Fire Department, Prescott-Russell Emergency Medical Services, Sarnia Fire Services, St. Catharine’s Fire and Rescue, Sudbury Emergency Medical Services, Sudbury Fire and Rescue, SunParlour Emergency Services Inc., Superior North Emergency Medical Services, Tecumseh Fire Department, Thames Emergency Medical Services, Thunder Bay Fire and Rescue, Waterloo Fire and Rescue, Waterloo Regional Emergency Medical Services, Welland Fire and Rescue, Windsor Fire and Rescue, British Columbia Ambulance Service, Abbotsford Fire Department, Aggassiz Valley Fire Department, Burnaby Fire Department, Campbell River Fire Department, Central Saanich Fire Department, City of North Vancouver Fire Department, Coquitlam Fire Department, Delta Fire Department, Esquimalt Fire Department, Kamloops Fire Department, Kelowna Fire Department, Lake Country V Fire Department, Langford Fire Department, Langley City Fire Department, Langley Township Fire Department, Maple Ridge Fire Department, Mission Fire Department, Nanaimo Fire Department, New Westminster Fire Department, North Vancouver District Fire Department, Oak Bay Fire Department, Peachland Valley Fire Department, Pitt Meadows Fire Department, Port Coquitlam Fire Rescue, Port Moody Fire Department, Prince George Fire Department, Prince Rupert Fire Department, Qualicum Beach Fire Department, Richmond Fire Department, Saanich Fire Department, Sooke V Fire Department, Squamish Fire Department, Surrey Fire Department, Trail Fire Department, Vancouver Fire Department, Victoria Fire Department, West Vancouver Fire Department, Whistler Fire Department, White Rock Fire Department; Pittsburgh Resuscitation Network, the University of Pittsburgh, Pittsburgh, PA: Clifton Callaway, MD, PhD, Principal Investigator; Core Investigators: Samuel Tisherman, MD, Jon Rittenberger, MD, David Hostler, PhD; Coordinators: Joseph Condle, Mitch Kampmeyer, Timothy Markham, Maureen Morgan; EMS Investigators/Collaborators: Paul Sabol, Gina Sicchitano, Scott Sherry, Anthony Shrader, Greg Stull, Manuel Torres, MS, William Groft, Robert McCaughan, Rodney Rohrer, John Cole, MD, David Fuchs, MD, Francis Guyette, MD, MS, William Jenkins, MD, Ronald Roth, MD, Heather Walker, MD; Hospital Investigators/Collaborators: Alain Corcos, MD, Ankur Doshi, MD, Adrian Ong, MD, Andrew Peitzman, MD; Participating EMS Agencies: Washington Ambulance and Chair, Pittsburgh Bureau of Emergency Medical Services, Pittsburgh Bureau of Fire, Mutual Aid Ambulance Service, STAT Medevac; Portland Resuscitation Outcomes Consortium, OR Health and Science University, Portland, OR: Jerris R. Hedges, MD, MS, Principal Investigator; Core Investigators: Craig D. Newgard, MD, MPH, Mohamud R. Daya, MD, MS, Robert A. Lowe, MD, MPH; Coordinators: Denise Griffiths, BS, John Brett, EMT-P, Dana Zive, MPH, Abdolaziz Yekrang, MPA, MA, Yoko Nakamura, MD, Brooke Frakes, BS, Aaron Monnig, EMT-P; EMS Investigators/Collaborators: Jonathan Jui, MD, MPH, Terri A. Schmidt, MD, MS, Ritu Sahni, MD, Craig R. Warden, MD, MPH, Marc D. Muhr, EMT-P2, John A. Stouffer, EMT-P, Kyle Gorman, MBA, EMT-P, Pontine Rosteck EMT-P, Karl Koenig EMT-P, Jan Lee EMT-P, Roxy Barnes EMT-P, Heather Tucker, EMT-P, Brad Allen, EMT-P, TJ Bishop, EMT-P, Adam Glaser, EMT-P; Hospital Investigators/Collaborators: Martin A. Schreiber, MD, Jim Anderson, MD, Ameen I. Ramzy, MD, K. Dean Gubler, DO, Lynn K. Wittwer, MD, Samantha Underwood, MS, Brooke Barone, BS, Denise Haun-Taylor, RN, Elizabeth Bryant, RN, Joanne Miller, ARNP; Participating EMS Agencies: American Medical Response—Clackamas, Clark, and Multnomah Counties, Camas Fire Department, Clackamas County Fire District #1, Clark County Fire District #6, Lake Oswego Fire Department, LifeFlight, MetroWest Ambulance, North Country Ambulance, Tualatin Valley Fire and Rescue, Vancouver Fire Department, Portland Fire and Rescue, Portland International Airport Fire Department, Gresham Fire and Emergency Services; UCSD-San Diego Resuscitation Research Center, University of California at San Diego, San Diego, CA: Daniel Davis, MD, Principal Investigator; Core Investigators: David Hoyt, MD, Raul Coimbra, MD, PhD, Gary Vilke, MD; Coordinators: Donna Kelly, RN, Lana McCallum-Brown, RN; EMS Investigators/Collaborators: Bruce Haynes, MD, Brad Schwartz, MD; Hospital Investigators/Collaborators: Michael Size, MD, Frank Kennedy, MD, Fred Simon, MD, Gail Tominaga, MD, John Steele, MD; Participating EMS Agencies: Alpine Fire Protection District, American Medical Response, Barona Fire Department, Bonita/Sunnyside Fire Protection, Borrego Springs Fire Protection District, Carlsbad Fire Department, Chula Vista Fire Department, Coronado Fire Department, CSA-17 ALS Transporting Agency, Deer Springs, Del Mar Fire Department, East County Fire Protection District, El Cajon Fire Department, Elfin Forest CSA 107, Encinitas Fire Protection District, Escondido Fire Department, Federal Fire Department San Diego, Imperial Beach Fire Department, Julian-Cuyamaca Fire Department, La Mesa Fire Department, Lakeside Fire Protection District, Lemon Grove Fire Department, Mercy Air, Miramar Fire Department, National City Fire Department, North County Fire, Oceanside Fire Department, Pala Fire Department, Poway Fire Department, Ramona Fire Department, Rancho Santa Fe Fire Protection District, San Diego Rural Fire Protection District, San Marcos Fire Department, San Miguel Fire Protection District, Santee Fire Department, Solana Beach Fire Department, Sycuan Fire Department, Valley Center/Mercy Ambulance, Viejas Fire Department, Vista Fire Department; Seattle-King County Center for Resuscitation Research at the University of Washington, University of Washington, Seattle, WA: Peter J. Kudenchuk, MD, Principal Investigator; Core Investigators: Tom D. Rea, MD, Eileen Bulger, MD, Mickey S. Eisenberg, MD, Michael Copass, MD; Coordinators: Michele Olsufka, RN, Sally Ragsdale, ARNP, Debi Solberg, RN, MN, Susan Damon, RN, Randi Phelps, Jeanne O’Brien, RN, MN; EMS Investigators/Collaborators: Earl Sodeman, Marty LaFave, James Boehl, Dave Jones, Gary Somers, Deborah Ayrs, Adrian Whorton, Sam Warren, Jim Fogarty, Jonathan Larsen, Mike Helbock; Participating EMS Agencies: Bellevue Fire Department, Redmond Fire Department, Seattle Fire Department, Shoreline Fire Department, King Co Medic 1, Vashon Island Medic One, Bothell Fire Department, Burien Fire Department, Kirkland Fire Department, Renton Fire Department, Snoqualmie Fire Department, Duvall Fire Department, Eastside Fire and Rescue, Enumclaw Fire Department, Fall City Fire Department, Skyway Fire Department, Kent Fire Department, Maple Valley Fire and Life Safety, Mercer Island Fire Department, King County Fire District #44, North Highline Fire Department, Northshore/Kenmore Fire Department, Port of Seattle Fire Department, King County Fire District #47, King County Fire District #40, SeaTac Fire Department, Skykomish Fire Department, Snoqualmie Pass, South King Co Medic 1, South King Fire and Rescue, Tukwila Fire Department, Valley Regional Fire Authority, Vashon Island Fire and Rescue, Woodinville Fire Department; Toronto Regional Resuscitation Research Out of Hospital Network (Toronto Regional RESCUeNET), University of Toronto, Toronto, Ontario, Canada: Arthur Slutsky, Principal Investigator; Core Investigators: Laurie Morrison, Paul Dorian; Coordinators: Craig Beers, Blair Bigham, Dina Braga, Grace Burgess, Bruce Cameron, Suzanne Chung, Pete De Maio, Steve Driscoll, Lynne Fell, Jamie Frank, Mark McLennan, Lesley Ann Molyneaux, Welson Ryan, Angela Schotsman, Jacob Simonini, Lynda Turcotte, Flo Veel, Amy Wassenaar, Cathy Zahn; EMS Investigators/Collaborators: Dana Bradshaw, Rob Burgess, Bruce Cameron, Sandra Chad, Sheldon Cheskes, Allan Craig, Steve Dewar, Tim Dodd, Rob Duquette, Marty Epp, Michael Feldman, Verena Jones, Russell MacDonald, Larry MacKay, Steve McNenley, Judy Moore, Philip Moran, Michael Murray, Michael Nemeth, Russ Olnyk, Tyrone Perreira, Richard Renaud, Karen Roche, Jennifer Shield, Doug Silver, Jacob Stevens, Rick Verbeek, Tim Waite, Ken Webb, Michelle Welsford; Hospital Investigators/Collaborators: Rosemarie Farrell, Jamie Hutchison; Participating EMS Agencies: Ajax Fire and Emergency Services, Barrie Fire and Emergency Service, Beausoleil First Nation Emergency Medical Services, Bradford West Gwillimbury Fire and Emergency Services, Brampton Fire and Emergency Services, Brock Township Fire Department, Caledon Fire and Emergency Services, City of Hamilton Emergency Services—EMS, City of Hamilton Emergency Services—Fire, City of Orillia Fire Department, Clarington Emergency and Fire Services, County of Simcoe Paramedic Services, Durham Regional Emergency Medical Services, Innisfil Fire and Rescue Service, Mississauga Fire and Emergency Services, Mnjikaning Fire Rescue Service, Muskoka Ambulance Service, Muskoka Ambulance Communication Center, New Tecumseth Fire Department, OrngeTransport Medicine, Oro Medonte Fire and Emergency Services, Oshawa Fire Services, Pickering Fire Services, The Ramara Township Fire and Rescue Service, Peel Regional Paramedic Services, Toronto EMS, Toronto Fire Services, Township of Essa Fire Department, Township of Georgian Bay Fire Department, Township of Scugog Fire Department, Township of Uxbridge Fire Department, Wasaga Beach Fire Department, Whitby Fire and Emergency Services, Durham Regional Basehospital, Sunnybrook Osler Center for Prehospital Care, Hamilton Health Sciences Paramedic Base Hospital Program, Simcoe Muskoka Basehospital; Steering Committee: Chair, Myron Weisfeldt, MD, Johns Hopkins University School of Medicine, Baltimore, MD, Co-Chair-Cardiac, Joseph P. Ornato, MD, Virginia Commonwealth University Health System, Richmond, VA, Co-Chair-Trauma, David B. Hoyt, MD, University of California at San Diego, San Diego, CA, replacing Col. John B. Holcomb, MD, Commander, U.S. Army ISR; National Heart, Lung, and Blood Institute, Bethesda, MD: Tracey Hoke, MD, George Sopko, MD, MPH, David Lathrop, PhD, Alice Mascette, MD, Patrice Desvigne Nickens, MD; Clinical Trial Center, University of Washington, Seattle, WA: Al Hallstrom, PhD, Graham Nichol, MD, MPH, Scott Emerson, MD, PhD, Judy Powell, BSN, Gena Sears, BSN, Berit Bardarson, RN, Lois Van Ottingham, BSN, Anna Leonen, MS, Robert B. Ledingham, MS, Chris Finley, Richard Moore, BS, Ben Bergsten-Buret.
Footnotes
Presentation as an abstract at the Resuscitation Science Symposium held during the American Heart Association annual meeting in November 2007 held in Orlando, Florida.
REFERENCES
- 1.Mackersie RC. History of trauma field triage development and the American College of Surgeons criteria. Prehosp Emerg Care. 2006;10:287–294. doi: 10.1080/10903120600721636. [DOI] [PubMed] [Google Scholar]
- 2.Committee on Trauma . Resources for Optimal Care of the Injured Patient. American College of Surgeons; Chicago, IL: 2006. [Google Scholar]
- 3.Cottington EM, Young JC, Shufflebarger CM, Kyes F, Peterson FV, Jr, Diamond DL. The utility of physiologic status, injury site, and injury mechanism in identifying patients with major trauma. J Trauma. 1988;28:305–311. doi: 10.1097/00005373-198803000-00005. [DOI] [PubMed] [Google Scholar]
- 4.Esposito TJ, Offner PJ, Jurkovich GJ, Griffith J, Maier RV. Do prehospital trauma center triage criteria identify major trauma victims? Arch Surg. 1995;130:171–176. doi: 10.1001/archsurg.1995.01430020061010. [DOI] [PubMed] [Google Scholar]
- 5.Kane G, Engelhardt R, Celentano J, et al. Empirical development and evaluation of out of hospital trauma triage instruments. J Trauma. 1985;25:482–489. doi: 10.1097/00005373-198506000-00002. [DOI] [PubMed] [Google Scholar]
- 6.Norcross ED, Ford DW, Cooper ME, Zone-Smith L, Byrne TK, Yarbrough DR., III Application of American college of surgeons’ field triage guidelines by pre-hospital personnel. J Am Coll Surg. 1995;181:539–544. [PubMed] [Google Scholar]
- 7.Henry MC, Hollander JE, Alicandro JM, Cassara G, O’Malley S, Thode HC., Jr Incremental benefit of individual American College of Surgeons trauma triage criteria. Acad Emerg Med. 1996;3:992–1000. doi: 10.1111/j.1553-2712.1996.tb03340.x. [DOI] [PubMed] [Google Scholar]
- 8.Henry MC, Alicandro JM, Hollander JE, Moldashel JG, Cassara G, Thode HC., Jr Evaluation of American College of Surgeons trauma triage criteria in a suburban and rural setting. Am J Emerg Med. 1996;14:124–129. doi: 10.1016/S0735-6757(96)90117-5. [DOI] [PubMed] [Google Scholar]
- 9.Knopp R, Yanagi A, Kallsen G, Geide A, Doehring L. Mechanism of injury and anatomic injury as criteria for out of hospital trauma triage. Ann Emerg Med. 1988;17:895–902. doi: 10.1016/s0196-0644(88)80666-8. [DOI] [PubMed] [Google Scholar]
- 10.Long WB, Bachulis BL, Hynes GD. Accuracy and relationship of mechanisms of injury, trauma score, and injury severity score in identifying major trauma. Am J Surg. 1986;151:581–584. doi: 10.1016/0002-9610(86)90553-2. [DOI] [PubMed] [Google Scholar]
- 11.Bond RJ, Kortbeek JB, Preshaw RM. Field trauma triage: combining mechanism of injury with the out-of-hospital index for an improved trauma triage tool. J Trauma. 1997;43:283–287. doi: 10.1097/00005373-199708000-00013. [DOI] [PubMed] [Google Scholar]
- 12.Hannan EL, Farrell LS, Cooper A, Henry M, Simon B, Simon R. Physiologic trauma triage criteria in adult trauma patients: are they effective in saving lives by transporting patients to trauma centers? J Am Coll Surg. 2005;200:584–592. doi: 10.1016/j.jamcollsurg.2004.12.016. [DOI] [PubMed] [Google Scholar]
- 13.Norwood SH, McAuley CE, Berne JD, Vallina VL, Creath RG, McLarty J. A out-of-hospital Glasgow Coma Scale score ≤ 14 accurately predicts the need for full trauma team activation and patient hospitalization after motor vehicle collisions. J Trauma. 2002;53:503–507. doi: 10.1097/00005373-200209000-00018. [DOI] [PubMed] [Google Scholar]
- 14.Baxt WG, Jones G, Fortlage D. The Trauma Triage Rule: a new, resource-based approach to the out-of-hospital identification of major trauma victims. Ann Emerg Med. 1990;19:1401–1406. doi: 10.1016/s0196-0644(05)82608-3. [DOI] [PubMed] [Google Scholar]
- 15.Zechnich AD, Hedges JR, Spackman K, Jui J, Mullins RJ. Applying the trauma triage rule to blunt trauma patients. Acad Emerg Med. 1995;2:1043–1052. doi: 10.1111/j.1553-2712.1995.tb03148.x. [DOI] [PubMed] [Google Scholar]
- 16.Lerner EB. Studies evaluating current field triage: 1966–2005. Prehosp Emerg Care. 2006;10:303–306. doi: 10.1080/10903120600723921. [DOI] [PubMed] [Google Scholar]
- 17.Wang HE, Yealy DM. Out-of-hospital endotracheal intubation: where are we? Ann Emerg Med. 2006;47:532–541. doi: 10.1016/j.annemergmed.2006.01.016. [DOI] [PubMed] [Google Scholar]
- 18.Ciesla DJ, Moore EE, Moore JB, et al. Intubation alone does not mandate trauma surgeon presence on patient arrival to the emergency department. J Trauma. 2004;56:937–941. doi: 10.1097/01.ta.0000127768.21385.81. [DOI] [PubMed] [Google Scholar]
- 19.Newgard CD, Sears GK, Rea TD, et al. The Resuscitation Outcomes Consortium Epistry-Trauma: Design, Development, and Implementation of a North American Epidemiologic Out-of-hospital Trauma Registry. Resuscitation. 2008;78:170–178. doi: 10.1016/j.resuscitation.2008.01.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Davis DP, Garberson LA, Andrusiek D, et al. A descriptive analysis of emergency medical service systems participating in a large, out-of-hospital resuscitation research network. Prehosp Emerg Care. 2007;11:369–382. doi: 10.1080/10903120701537147. [DOI] [PubMed] [Google Scholar]
- 21.Newgard CD, Fleischman R, Choo E, et al. Validation of length of hospital stay as a surrogate measure for injury severity and resource use among injury survivors. Acad Emerg Med. doi: 10.1111/j.1553-2712.2009.00647.x. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Breiman L, Freidman JH, Olshen RA, Stone CJ. Classification and Regression Trees. Chapman & Hall; New York: 1984. [Google Scholar]
- 23.Stiell IG, Wells GA. Methodologic standard for the development of clinical decision rules in emergency medicine. Ann Emerg Med. 1999;33:437–447. doi: 10.1016/s0196-0644(99)70309-4. [DOI] [PubMed] [Google Scholar]
- 24.Wang HE, Peitzman AB, Cassidy LD, Adelson PD, Yealy DM. Out-of-hospital endotracheal intubation and outcome after traumatic brain injury. Ann Emerg Med. 2004;44:439–450. doi: 10.1016/j.annemergmed.2004.04.008. [DOI] [PubMed] [Google Scholar]
- 25.Davis DP, Hoyt DB, Ochs M, et al. The effect of paramedic rapid sequence intubation on outcome in patients with severe traumatic brain injury. J Trauma. 2003;54:444–453. doi: 10.1097/01.TA.0000053396.02126.CD. [DOI] [PubMed] [Google Scholar]
- 26.Bulger EM, Nathens AB, Rivara FP, MacKenzie E, Sabath DR, Jurkovich GJ. National variability in out-of-hospital treatment after traumatic injury. Ann Emerg Med. 2007;49:293–301. doi: 10.1016/j.annemergmed.2006.06.038. [DOI] [PubMed] [Google Scholar]
- 27.Committee on Trauma . ATLS for Trauma Student Course Manual. 6th ed. American College of Surgeons; Chicago, IL: 1997. [Google Scholar]
- 28.Eastridge BJ, Salinas J, McManus JG, et al. Hypotension begins at 110 mm Hg: redefining “hypotension” with data. J Trauma. 2007;63:291–299. doi: 10.1097/TA.0b013e31809ed924. [DOI] [PubMed] [Google Scholar]
- 29.Holcomb JB, Salinas J, McManus JM, Miller CC, Cooke WH, Convertino VA. Manual vital signs reliably predict need for life-saving interventions in trauma patients. J Trauma. 2005;59:821–829. doi: 10.1097/01.ta.0000188125.44129.7c. [DOI] [PubMed] [Google Scholar]
- 30.Arbabi S, Jurkovich GJ, Wahl WL, et al. A comparison of prehospital and hospital data in trauma patients. J Trauma. 56:1029–1032. doi: 10.1097/01.ta.0000123036.20919.4b. 200. [DOI] [PubMed] [Google Scholar]
- 31.Franklin GA, Boaz PW, Spain DA, Lukan JK, Carrillo EH, Richardson JD. Prehospital hypotension as a valid indicator of trauma team activation. J Trauma. 2000;48:1034–1039. doi: 10.1097/00005373-200006000-00006. [DOI] [PubMed] [Google Scholar]
- 32.Lipsky AM, Gausche-Hill M, Henneman PL, et al. Prehospital hypotension is a predictor of the need for an emergent, therapeutic operation in trauma patients with normal systolic blood pressure in the emergency department. J Trauma. 2006;61:1228–1233. doi: 10.1097/01.ta.0000196694.52615.84. [DOI] [PubMed] [Google Scholar]
- 33.Bulger EM, Jurkovich GJ, Nathens AB, et al. Hypertonic resuscitation of hypovolemic shock after blunt trauma. Arch Surg. 2008;143:139–148. doi: 10.1001/archsurg.2007.41. [DOI] [PubMed] [Google Scholar]
- 34.Brasel KJ, Bulger E, Cook AJ, et al. Hypertonic resuscitation: design and implementation of a prehospital intervention trial. J Am Coll Surg. 2008;206:220–232. doi: 10.1016/j.jamcollsurg.2007.07.020. [DOI] [PubMed] [Google Scholar]
- 35.King RW, Plewa MC, Buderer NM, Knotts FB. Shock index as a marker for significant injury in trauma patients. Acad Emerg Med. 1996;3:1041–1045. doi: 10.1111/j.1553-2712.1996.tb03351.x. [DOI] [PubMed] [Google Scholar]
- 36.McManus J, Yershov AL, Ludwig D, et al. Radial pulse character relationships to systolic blood pressure and trauma outcomes. Prehosp Emerg Care. 2005;9:423–428. doi: 10.1080/10903120500255891. [DOI] [PubMed] [Google Scholar]
- 37.Cancio LC, Batchinsky AI, Salinas J, et al. Heart-rate complexity for prediction of prehospital lifesaving interventions in trauma patients. J Trauma. 2008;65:813–819. doi: 10.1097/TA.0b013e3181848241. [DOI] [PubMed] [Google Scholar]
- 38.Cohn SM, Nathens AB, Moore FA, et al. Tissue oxygen saturation predicts the development of organ dysfunction during traumatic shock resuscitation. J Trauma. 2007;62:44–55. doi: 10.1097/TA.0b013e31802eb817. [DOI] [PubMed] [Google Scholar]