Abstract
Objectives
Behavioral models for mobile phone-based diabetes interventions are lacking. This study explores the potential mechanisms by which a text message-based diabetes program affected self-management among African-Americans.
Methods
We conducted in-depth, individual interviews among 18 African-American patients with type 2 diabetes who completed a 4-week text message-based diabetes program. Each interview was audio- taped, transcribed verbatim, and imported into Atlas.ti software. Coding was done iteratively. Emergent themes were mapped onto existing behavioral constructs and then used to develop a novel behavioral model for mobile phone-based diabetes self-management programs.
Results
The effects of the text message-based program went beyond automated reminders. The constant, daily communications reduced denial of diabetes and reinforced the importance of self-management (Rosenstock Health Belief Model). Responding positively to questions about self-management increased mastery experience (Bandura Self-Efficacy). Most surprisingly, participants perceived the automated program as a “friend” and “support group” that monitored and supported their self-management behaviors (Barrera Social Support).
Conclusions
A mobile phone-based diabetes program affected self-management through multiple behavioral constructs including health beliefs, self-efficacy, and social support. Practice implications: Disease management programs that utilize mobile technologies should be designed to leverage existing models of behavior change and can address barriers to self-management associated with health disparities.
Keywords: Patient education, Patient–provider communication, Text messaging, Diabetes, African American
1. Introduction
Type 2 diabetes affects over 9% of the U.S. adult population and even higher proportions of African-Americans, who also experience higher rates of complications [1], [2], [3] and [4]. Self-management is a cornerstone of diabetes care, yet significant barriers remain [5] and [6]. This is particularly true in African-Americans, who disproportionately face barriers to self-management including limited health literacy, social support, and access to health care [7], [8], [9] and [10].
Mobile phones are emerging as an ideal platform for improving chronic disease management because they are ubiquitous, low-cost, and reliable [11] and [12]. Mobile phone-based interventions (or “mobile health applications”) for diabetes include weekly clinical support via text messaging, personalized diabetes management messages, and blood glucose transfer and advice [13]. Mobile health applications are particularly promising for addressing health disparities because mobile phones are one of the few technologies that enjoy wider usage among African-Americans than whites and reverse the digital divide [14].
Studies of mobile phone-based interventions have had varied success in improving self-management and glycemic control in individuals with diabetes [13] and [15]. One explanation is that mobile phones are a platform, not a solution in itself, and interventions vary widely. A major gap in the literature is the lack of behavioral models to explain how these interventions improve diabetes self-management [16]. Reviews of diabetes self-management interventions indicate the need for better theoretical grounding [17] and [18], and yet studies of mobile phone applications to date have been largely atheoretical [16]. The prevailing theoretical assumption is that mobile phone-based interventions lead to behavior change through prompts and conditioning [19]: that is, patients receive a reminder to take their medication, and so they take their medication more frequently. However, barriers to self-management are complex, and it is unlikely that sustained behavior change can be observed through conditioning alone.
In the present study, we explore the potential mechanisms by which a mobile phone-based intervention improved diabetes self-management and develop a behavioral model that may be used to design and evaluate mobile health applications. The analysis is based on in-depth, one-on-one interviews with a sample of African-Americans who completed a 4-week text messaging pilot program designed to provide automated self-care reminders. The results of this pilot study have been published elsewhere [20], but briefly, demonstrated a high degree of acceptance among participants and a sustained improvement in diabetes self-efficacy and self-reported medication adherence and daily foot care.
2. Methods
We conducted 18 in-depth, individual, semi-structured interviews among African-Americans with type 2 diabetes who completed a 4-week text message-based diabetes self-management program. Each interview lasted approximately 60 min.
2.1. Patient recruitment
After receiving approval from the Institutional Review Board, patients were recruited from the University of Chicago Primary Care Group’s Resident Clinic from November 1, 2009 to January 31, 2010. Culturally tailored, low-literacy flyers were posted in each examination room and resident-physicians were asked to recommend patients for the study. Eligible patients were adults with type 2 diabetes on oral hypoglycemic agents and/or insulin. Patients were required to have a personal cell phone and those who had been hospitalized in the prior 2 months were excluded. Participants received $25 to cover text messaging costs and $30 for participation. Sociodemographic and clinical information were collected on enrollment as were baseline data on cellular phone and text messaging usage.
Of the 56 patients identified, 45 patients were successfully contacted and 35 expressed interest in participating. Twenty-eight of those interested had cell phones and 26 of these had not been hospitalized in the past 2 months. Of these 26 patients, 19 were successfully enrolled with the balance missing and unable to reschedule their enrollment interview. One patient left the study because of poor health. All remaining 18 participants completed the pilot intervention and the follow-up interview.
2.2. Pilot study
The methods for the pilot study have been described in detail elsewhere [18], but are summarized here. On enrollment, participants were provided a tutorial on text messaging and queried for their preferences on message timing and content. This information was entered into an automated text messaging software called SMS-DMCare, and participants began receiving text messages the following day. Each participant was required to have the following types of messages: a daily medication reminder (e.g., “Time to take your diabetes medications”), a daily or semi-weekly question about medication adherence (e.g., “How many times did you take your medication?”), a weekly question about foot care (e.g., “How many times did you check your feet this week?”), and appointment reminders for diabetes-related visits. Finally, patients were permitted to request additional messages related to diabetes care such as reminders about glucose monitoring. Participants were expected to respond to question messages (e.g., “Did you take your medications today?”) using free text (e.g., “No”, “Nah”, etc.).
Participants were enrolled into SMS-DMCare by a text administrator (M.S.) who is also a certified diabetes educator (CDE). Her role was to enroll participants in the system in-person and then conduct weekly interviews by phone to solicit feedback on their experience and, if necessary, make adjustments to their personalized SMS-DMCare program (e.g., change content or timing of messages). She did not provide teaching, counseling, or other services typically performed by a CDE. After 4 weeks the intervention was discontinued and exit interviews were scheduled.
2.3. Study instruments
Topic guides were created for the in-depth interviews with the goal of exploring the following: participant perceptions of the automated text messaging program, barriers and facilitators of the program, and the perceived impact of the program on their self-care and health.
The guide consisted of a list of open-ended questions and follow-up probes. Queries began with “In general, do you think the cell phone system helped you in any way?” and followed with probes such as “Which specific messages or aspects of the program were helpful and why?” We also asked about hypothetical situations (e.g., “If you did not receive weekly phone calls from the text administrator, do you think the program would have been as helpful to you?”), comparative experiences (e.g., “Since the text messaging program ended how have things been different for you?”), and suggestions for improvement (e.g., “How could we make the texting pilot better?”).
2.4. Data analysis and synthesis
Individual interviews were audio-taped, transcribed verbatim, and imported into Atlas.ti 4.2 software. All de-identified, anonymous transcripts were coded using the constant comparative method, with no a priori hypotheses, by a team of six investigators with experience in medicine, diabetes education, and public health [21]. A number of themes emerged related to the interpersonal effects of the text messaging program, which were unanticipated and novel. Coded transcripts of these themes were distributed equally among the four investigators (S.N., J.D., M.S., and M.P.) for in-depth analysis. Investigators were asked to review and summarize each transcript with the lens of understanding how the text messaging program provided the participant self-management support beyond the automated reminders. Summaries of each transcript were discussed with the entire research group in an iterative manner until consensus emerged around how the program provided self-management support. Several of the themes were found to map onto existing theoretical frameworks – Barrera’s social support model, Rosenstock’s Health Belief Model, and Bandura’s Self-Efficacy Model – and were used to formulate a new behavioral model. Other behavioral frameworks (e.g., Patient Activation Model, the Social Ecological Model, and Theory of Planned Behavior) were considered by the group but ultimately considered to not fit the data as well.
3. Results
3.1. Patient characteristics
The majority of study participants were female (67%) and approximately three-quarters were between ages 40 and 64 years (Table 1). All participants were African-American. Sixty-one percent of study participants had completed at least “some college”. Approximately one-third had Medicaid with the remainder on private insurance or a combination of Medicare and private insurance. The average duration of diabetes was 8 years with a wide range (<1–22 years). The vast majority was comfortable making and receiving phone calls on their mobile phones (94%) but only a small majority was comfortable with text messaging at the beginning of the study (56%).
Table 1.
Participant characteristics.
| N | % | |
|---|---|---|
| Participant demographics | ||
| Age, years (mean, range) | 55 [38–72] | |
| 18–39 | 1 | 6 |
| 40–54 | 8 | 44 |
| 55–64 | 6 | 33 |
| 65–74 | 3 | 17 |
| Female gender | 12 | 67 |
| Race | ||
| African-American | 18 | 100 |
| Other | 0 | 0 |
| Marital status | ||
| Single | 7 | 39 |
| Married/living as married | 8 | 44 |
| Separated/divorced/widowed | 3 | 17 |
| Education | ||
| Some high school or less | 4 | 22 |
| High school graduate | 3 | 17 |
| Some college | 8 | 44 |
| College graduate or higher | 3 | 17 |
| Employment | ||
| Employed | 6 | 33 |
| Unemployed | 8 | 44 |
| Retired | 4 | 22 |
| Insurance | ||
| Uninsured | 0 | 0 |
| Medicaid | 6 | 33 |
| Medicare | 0 | 0 |
| Medicare + Medicaid | 0 | 0 |
| Private insurance | 7 | 39 |
| Medicare + Private | 5 | 28 |
| Years of diabetes (mean, range) | 8 [0.75–22] | |
| <1 | 1 | 6 |
| 1–3 | 4 | 22 |
| 4–7 | 4 | 22 |
| 8–10 | 6 | 33 |
| >10 | 3 | 17 |
| Medication regimen | ||
| Oral hypoglycemic agents | 11 | 61 |
| Insulin | 5 | 28 |
| Oral hypoglycemics agents and insulin | 2 | 11 |
| Prior participant experience with cellular phone calling and text messaging | ||
| Years owning cell phone | ||
| 0–5 | 6 | 33 |
| 6–10 | 8 | 44 |
| >10 | 4 | 22 |
| Comfort level making/receiving calls | ||
| Very or somewhat comfortable | 17 | 94 |
| Not comfortable nor uncomfortable | 0 | 0 |
| Very or somewhat uncomfortable | 1 | 6 |
| Total calls made/received per day | ||
| <5 | 5 | 28 |
| 6–10 | 5 | 28 |
| 11–20 | 2 | 11 |
| >20 | 6 | 33 |
| Comfort level with texting | ||
| Very or somewhat comfortable | 10 | 56 |
| Not comfortable nor uncomfortable | 0 | 0 |
| Very or somewhat uncomfortable | 8 | 44 |
| Total texts sent/received per day | ||
| 0 | 6 | 33 |
| 1–5 | 5 | 28 |
| 6–10 | 2 | 11 |
| >10 | 5 | 28 |
3.2. Themes
A number of themes emerged concerning the unanticipated interpersonal and behavioral effects of the text messaging program (Table 2).
Table 2.
Unanticipated participant perceptions of the text message-based diabetes program.
| Self-awareness and control [62 quotations] |
|
| What did I like about it, what did I like about the texting… What I liked about the texting was that it made me more responsible…. | |
| Well I think that question of how many times. Cause see a lot of times I get down on myself and maybe take one pill. But this is before the study. And I would take one pill instead of two to see how I would do. And I think while I was on the study I was mindful of that, I should do what my doctor told me to do. The number of times I take the medicine. And so I think it helped me be honest. | |
| Reinforcement and feedback [36 quotations] | But I feel much better. And it’s not good having those low sugar reactions. And so I think that these 4 weeks have helped me to see the benefits of being on a regular schedule. |
| I wanted to be able to answer [the text query about adherence] in the affirmative that, ‘Yes, I had already done that.’ So I think it helped me. | |
| Seriousness of diabetes and acceptance [13 quotations] | Yes, I believe that it has truly helped me. Prior to the beginning of the study, I was very forgetful about taking my medication; I wasn’t taking it in a timely manner. By actually being in the study it made me become more aware of how important it was for me to take my medication at the same time everyday on a regular basis at a specific time. |
| |
| Caring and support [16 quotations] | Well I could ignore [my diabetes before the study]. You know I didn’t have any reminders. And I just figured if I felt okay then it’s okay to eat like cake whenever I wanted to or whatever. And then I would take my blood sugar and see it was high, then I would say, “oh I have to stop eating this cake”. But since I had someone else monitoring me, it wasn’t just me I felt obligated to take better care of myself. |
| |
| Role of text administrator [58 quotations] |
|
| Now I’m not much of a person on something coming through machines… So I have to have something in mind that makes me think it’s a person… And if it’s not, that message is not convincing or I can’t put a face to it or a voice to it to just a message, that I’m even going to call. I think I would over months time kind of ignore it or push it to the side. | |
| |
| Role of the physician [25 quotations] | Participant: Actually I am going to be honest, I liked the fact that each week after each week you called just to see how everything was going and I think that, that is something you don’t get a lot with your physician, sometimes you are just told that you have diabetes and not given any teaching or concern. |
| Role of family and friends [8 quotations] |
|
3.2.1. Self-awareness and control
Participants described becoming more aware of their diabetes and more in control of their illness.
“Actually I am just being more aware of taking my medication as well as being more watchful in what I eat. I notice now that if it is high, I look back to see what I have eaten to see if the food had anything to do with it. So I am now logging down what I eat because of the study.”
They also reflected on being more aware of physiological changes in their condition.
“I learned a little bit more about me. Because prior to the study I did not take my blood sugar often therefore I didn’t know when my sugar was high or low, but now I do. I now know how I feel when my sugar is high or low.”
3.2.2. Reinforcement and feedback
The messages reinforced the participants’ success in taking care of their diabetes, either from explicit feedback from a message (e.g., “great job”) or indirectly through evidence that the text messages were improving their health.
“But then, I’m like, I’m taking my, I looked at what I was doing, and what I was accomplishing, and my sugar actually’s gotten better. When I started taking my sugar, checking my glucose you call it, and uh it was much better. So it helps me a lot. I welcome the texts.”
3.2.3. Seriousness of diabetes and acceptance
Participants acknowledged an increased awareness of their personal risk of complications and of the relationship between self-care activities and diabetes outcomes.
“I wasn’t aware of the importance of [checking my feet] before the study. Well, I always knew people with high level of diabetes are prone to amputations… And that’s something very serious and I wouldn’t want that to happen to me. And I just never realized that it was so closely related.”
The program also helped participants to accept their condition and to understand the significance of having a chronic illness.
“Well, it goes back to being somewhat in denial with diabetes …With the text messages, it kind of reinforces. In reality, you have diabetes and these things should be followed through. It’s uh…discipline, you know because it makes you be aware of it, when it starts out you are kind of in denial.”
3.2.4. Caring and support
Participants often reflected that the text messaging program provided them with someone who cared about how they were doing and monitored their condition.
“But somebody is involved in being concerned about what’s going on with you besides the visits with the doctor or maybe the nurse checking up on you. This is some kind of constant something.”
Some participants went further to describe the text messaging as a friend, sponsor, or social group.
“Participant: The text messages became my friend.
Interviewer: Okay.
Participant: And a friend helped me do the right things.
Interviewer: Alright.
Participant: So the texting became a friend to me. And it was telling me, ‘It’s time to take your medicine,’ ‘Did you take your medicine today,’ ‘Did you check your feet.’ So therefore I had someone reminding me.”
3.2.5. Role of the text administrator
Participants also reflected on the role of the text administrator who enrolled them in the study and called them weekly to modify their personalized text messaging program. Some participants believed that the text messages were being sent directly from the text administrator, rather than from an automated computer program, while others knowingly anthropomorphized the text messaging program.
Although responses varied, some participants felt that regular contact with the text administrator facilitated their engagement with the text messaging program.
“I would not like [a system without an text administrator]. If nobody is going to check the program, especially if you make it a more responsive program, then why am I responding?”
The text administrator also gave participants the sense that they were being monitored, even though they were explicitly instructed that the text administrator did not review responses in real-time and would not provide any clinical support. Self-management improved in part because participants felt more confident with someone monitoring them and in part because they wanted the approval of the text administrator.
“Interviewer: So, in many ways reporting to someone is more important than helping yourself internally?
Participant: Hmm….
Interviewer: Heavy question, huh??
Participant: Yes it is. It’s…to me it’s about 50/50.
Interviewer: Okay.
Participant: Because I think deep down within I want to please or satisfy a person or a condition at the same time helping myself…”
3.2.6. Role of the physician
Physicians were not explicitly included in the study or text messaging program. Most participants felt that the cell phone pilot complemented their routine medical care.
“Interviewer: How would you like for the physician to be part of this whole process?
Participant: Well, the physician really wouldn’t have to be. Because the physician has already told you, what you should do, what you shouldn’t do, what you should eat, what you shouldn’t eat; So therefore she has already done her job. So now it’s up to you to carry it through.”
3.2.7. Role of family and friends
A few participants observed that the text messaging program reduced the burden of self-management support on caregivers. One participant noted that their family members were supportive of the program:
“Actually they really didn’t know [about the pilot study] until I told them. I told some family members and how helpful it was and they encouraged me to stick with it.”
3.3. Mapping onto existing frameworks
The themes of “caring and support” and the “role of the text administrator” were found to map onto the Barrera’s Model of Social Support. The “seriousness of diabetes and acceptance” theme mapped onto Rosenstock’s Health Belief Model. The themes of “self-awareness and control” and “reinforcement and feedback” mapped onto Bandura’s Model of Self-Efficacy. The “role of the physician” and “role of family and friends” themes did not significantly contribute to the effect of the texting program on self-management and therefore were excluded from further analysis.
3.3.1. Social support
Barrera [22] described three types of social support: perceived support, enacted support, and social integration. Perceived support is the recipient’s subjective judgment that others will offer or have offered help. Some participants perceived that the text administrator was personally sending them text messages to help them self-manage their diabetes, even though the system was automated. Others reported that they benefited from the feeling that someone was monitoring them and that if needed help was available. Enacted support includes specific supportive actions offered by providers during times of need. Reminders helped participants organize their diabetes care through reminders, and weekly phone calls with the text administrator kept some participants engaged in their diabetes care even though direct teaching or counseling was not provided. Social integration is the extent to which a recipient is connected within a social network. Some participants likened the text messaging program to a “friend” or “support group,” and many valued the daily interaction the system provided, which complemented their traditional support structures.
3.3.2. Health belief
The original health belief model described by Rosenstock [23] included four constructs: perceived susceptibility, perceived severity, perceived barriers, and perceived benefits. Perceived susceptibility describes an individual’s assessment of his or her risk of getting a condition. While all the patients in the study already had diabetes, weekly messages about self-foot care increased their perceived susceptibility to diabetic foot complications. Perceived severity is an individual’s assessment of the seriousness of a condition. Participants reported that the frequency of communication about their diabetes decreased denial and made them appreciate the seriousness of living with a chronic illness. Perceived barriers are an individual’s assessment of the influences that facilitate or discourage adoption of the promoted behavior. By providing reminders about a discrete self-care activity (e.g., checking your feet today), the pilot helped participants break down self-management into more manageable steps. Perceived benefits are an individual’s assessment of the positive consequences of adopting a behavior. Through its emphasis on self-care behaviors, the program helped participants appreciate the causal relationship between their self-management behaviors and their health.
3.3.3. Self-efficacy
Bandura [24] and [25] identified four factors affecting self-efficacy including mastery experience, social persuasions, physiological factors, and social modeling, of which the first three related to the themes which emerged. Mastery experience or enactive attainment describes how success raises self-efficacy. As participants experienced fewer symptoms such as less hypoglycemic events, the program reinforced positive behavioral changes. Social persuasions are encouragements or discouragements that affect an individual’s self-efficacy. Participants described the desire to ‘not let down’ the text administrator and to receive positive feedback when they responded affirmatively to queries about adherence. Physiological factors are an individual’s perceptions of physiological responses that can alter his or her self-efficacy. Some participants began associating high or low glucose readings with the symptoms they were experiencing.
3.4. Behavioral model
Fig. 1 depicts the conceptual model that has emerged from this analysis. This behavioral model is based on participants’ perceptions of how the texting program affected them – findings that will need to validated in future studies. The model hypothesizes that the SMS-DMCare text messages and phone calls directly improved self-management through reminders, but also indirectly by improving social support, modifying health beliefs, and increasing self-efficacy. In the model, daily text messages from SMS-DMCare modify participants’ health beliefs about diabetes. Feedback about participants’ self-management behaviors increases self-efficacy. Finally, frequent contact from the automated text messages and phone calls from the text administrators increases social support. Health beliefs, self-efficacy, and social support affect self-management directly; in addition, the effect of social support on self-management is mediated by self-efficacy through social persuasion. Some of these effects are also hypothesized to be bidirectional: self-management modifies health beliefs by reducing the perceived barriers to diabetes care and also increases self-efficacy through mastery experience.
Fig. 1.
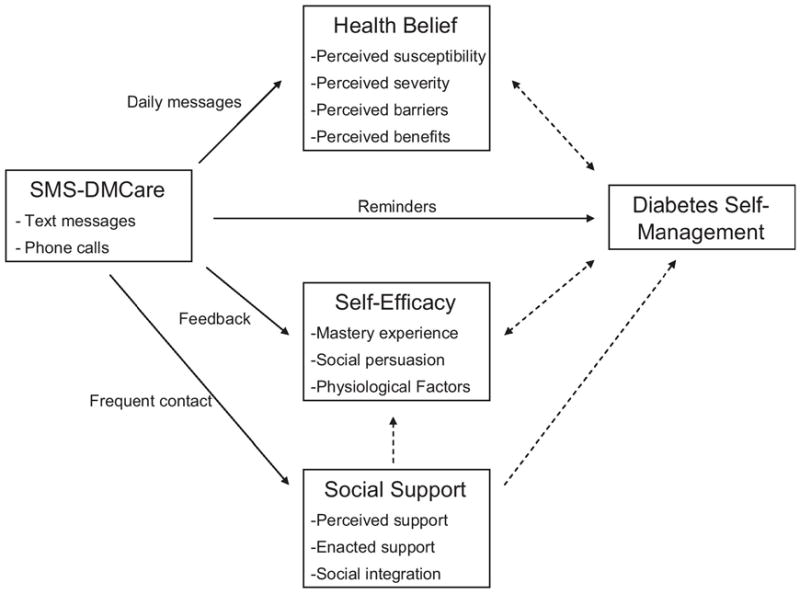
Proposed behavioral model for mobile phone-based diabetes self-management programs. The arrows represent causal pathways according to participants’ perceptions. The solid arrows are pathways directed by physical processes (e.g., text messages and phone calls); the dashed arrows are non-physical processes.
4. Discussion and conclusion
4.1. Discussion
This study, which was conducted among African-Americans with type 2 diabetes, explores the mechanisms by which mobile phone-based interventions may affect self-management. It builds upon prior qualitative work in telehealth and mobile health demonstrating that patients can form strong personal relationships with technology [26], that remote monitoring increases confidence about self-management and reduces anxiety [27] and [28], and that frequent communication increases awareness of their health condition and empowerment [29]. However, it goes further by formalizing a theoretical model for how mobile health interventions may affect self-management beyond cues to action. A recent review of mobile health applications found that among 20 studies of disease management only one specified a theoretical basis for the intervention [16]. The authors conclude that current theories “appear inadequate to inform mobile intervention development” and call for new models to support “a theory-driven iterative model of mobile intervention development.” This study seeks to fill this gap by proposing a behavioral model for mobile phone-based self-management interventions mediated by social support, health beliefs, and self-efficacy.
Although the mobile health intervention studied here consisted largely of automated text messages, participants perceived high levels of social support. Participants felt cared for by a person despite the fact that many of the participants knew the messages were automated. The literature supports the positive influence of social support, both from family and friends and from health care professionals, on diabetes self-management behaviors [30], [31], [32], [33] and [34]. A recent study of urban African Americans and Latinos found that family and friend support was associated with improved glucose monitoring while non-physician professional support was important for foot care and nutrition [35]. In our study, participants viewed the text messaging program as both a peer and an extension of the health care system, which suggests it may integrate across these domains. For some participants, the construct of social support was facilitated by regular contact with the text administrator. For others, the bidirectional communication provided by SMS-DMCare created the sense that ‘somebody somewhere’ was monitoring them.
In addition, the text messaging program modified participants’ beliefs about their illness and their self-management behaviors. Although messages were not explicitly educational in nature, the frequency of self-care reminders raised the overall importance of diabetes and of self-management, emphasized the seriousness of the condition, and reduced denial. Studies demonstrate that health beliefs are associated with self-management behaviors in individuals with diabetes [36], [37] and [38]. Denial and the failure to recognize the risks and consequences of asymptomatic conditions have been found to be particularly prevalent in African-Americans [8].
Lastly, the texting program increased participants’ self-efficacy by providing feedback on their self-management and relating their symptoms to their self-care activities. For example, by responding to queries about adherence, participants were able to build their sense of mastery experience. Self-efficacy has been shown to be associated with self-management behaviors in diabetes, including in African-Americans [39], [40], [41] and [42]. The fact that participants selected their own messages and then had an opportunity to modify them weekly may have strengthened this effect. This allowed them to choose which self-management domains they wanted to focus on each week (e.g., glucose monitoring). Patient participation is a key principle of shared decision-making [43] and has particular salience in African-Americans [44].
4.2. Conclusion
African-American patients with type 2 diabetes perceived the effects of an automated text messaging diabetes program to extend beyond self-care reminders to include improved social support, increased self-efficacy, and modified health beliefs. This suggests that mobile health applications can affect self-management through behavioral constructs typically associated with traditional self-management support programs.
This study has important limitations. First, because this study utilizes a sample of patients who completed a specific text messaging intervention, the results may not generalize to other mobile phone interventions. In particular, the weekly phone calls with the text administrator in our study may have contributed to the high levels of social support perceived by participants. In mobile phone applications without this interaction, the relative importance of social support may be diminished. Despite this limitation, we found evidence that elements of the intervention other than the text administrator led to increased social support, and our overall purpose was to explore how mobile phone-based interventions may influence self-management rather than to identify the relative importance of one mechanism over another. Second, because the pilot study was relatively brief, the participant perceptions we observed may not generalize to longer interventions. Because diabetes is a chronic illness, it will be important for future studies to assess the behavioral effects of mobile phone applications over longer time intervals. Third, the study took place in an academic medical center that serves a predominantly urban, working class African-American population. As described above, African-Americans disproportionately face barriers to self-management, which may limit the generalizability of our findings to non-ethnic and racial minorities. Finally, the behavioral model we developed is based on post hoc participant interviews rather than pre-post survey instruments. The resulting model should be construed to represent hypothetical relationships, which future studies should seek to validate.
Nonetheless, our study has several strengths. First, all the participants completed a 4-week diabetes text message-based self-management program prior to the interview. This provided a rich set of experiences that participants could draw from. Second, every participant who completed the intervention also participated in the in-depth interviews, which minimized selection bias. Finally, the analysis was done without a priori hypotheses, which reduced interview bias.
4.3. Practice implications
As mobile health and telemedicine are integrated into routine medical care it will become increasingly important to understand how the introduction of these technologies affects self-management, particularly in vulnerable health populations. This study suggests that these technologies can be used to not only send automated reminders but also to address key drivers of health disparities by modifying health beliefs and increasing social support and self-efficacy. Care models using mobile technologies should be designed to leverage these behavioral constructs to develop effective, targeted interventions. For example, designating a single staff member to enroll and track a cohort of patients may improve self-management by increasing perceived support.
Acknowledgments
Dr. Nundy is supported by the Agency for Healthcare Research and Quality Health Services Research Training Program (T32 HS00084). Dr. Peek received support from the Robert Wood Johnson Foundation (RWJF) Harold Amos Medical Faculty Development program and the Mentored Patient-Oriented Career Development Award of the NIDDK (K23 DK075006). This research was also supported by the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) (R18DK083946), Diabetes Research and Training Center (P60 DK20595), the Chicago Center for Diabetes Translation Research (P30 DK092949), and the Alliance to Reduce Disparities in Diabetes of the Merck Company Foundation.
Footnotes
Conflicts of interest statement
Dr. Nundy previously cofounded and was part-owner of mHealth Solutions, LLC, a mobile health software company, but currently has no financial relationship or affiliation with the company. Dr. Dick cofounded and is part-owner of mHealth Solutions, LLC. The other authors have no conflicts of interest to disclose.
References
- 1.National Institute of Diabetes and Digestive and Kidney Diseases. National Diabetes Statistics fact sheet: general information and national estimates on diabetes in the United States. Govt. Printing Office; Washington, DC: 2005. NIH publ. no. 06-3892. [Google Scholar]
- 2.Peek ME, Cargill A, Huang ES. Diabetes health disparities: a systematic review of health care interventions. Med Care Res Rev. 2007;64:101S–56S. doi: 10.1177/1077558707305409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Carter JS, Pugh JA, Monterrosa A. Non-insulin dependent diabetes mellitus in minorities in the United States. Ann Intern Med. 1996;125:221–232. doi: 10.7326/0003-4819-125-3-199608010-00011. [DOI] [PubMed] [Google Scholar]
- 4.Lanting LC, Joung IM, Mackenbach JP, Lamberts SW, Bootsma AH. Ethnic differences in mortality, end-stage complications, and quality of care among diabetic patients: a review. Diabetes Care. 2005;28:2280–2288. doi: 10.2337/diacare.28.9.2280. [DOI] [PubMed] [Google Scholar]
- 5.American Diabetes Association. Standards of medical care in diabetes—2011. Diabetes Care. 2011;34:S11–S61. doi: 10.2337/dc11-S011. http://dx.doi.org/10.2337/dc11-S011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Funnell MM, Brown TL, Childs BP, Haas LB, Hosey GM, Jensen B, et al. National standards for diabetes self-management education. Diabetes Care. 2012;35(Suppl):S101–S108. doi: 10.2337/dc12-s101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Schectman JM, Nadkarni MM, Voss JD. The association between diabetes metabolic control and drug adherence in an indigent population. Diabetes Care. 2002;25:1015–1021. doi: 10.2337/diacare.25.6.1015. [DOI] [PubMed] [Google Scholar]
- 8.Gazmararian JA, Ziemer DC, Barnes C. Perception of barriers to self-care management among diabetic patients. Diabetes Educ. 2009;35:778–788. doi: 10.1177/0145721709338527. [DOI] [PubMed] [Google Scholar]
- 9.Chlebowy DO, Garvin BJ. Social support, self-efficacy, and outcome expectations: impact on self-care behaviors and glycemic control in Caucasian and African American adults with type 2 diabetes. Diabetes Educ. 2006;32:777–786. doi: 10.1177/0145721706291760. [DOI] [PubMed] [Google Scholar]
- 10.Tang TS, Brown MB, Funnell MM, Anderson RM. Social support, quality of life, and self-care behaviors among African Americans with type 2 diabetes. Diabetes Educ. 2008;34:266–276. doi: 10.1177/0145721708315680. [DOI] [PubMed] [Google Scholar]
- 11.Krishna S, Boren SA, Balas EA. Healthcare via cell phones: a systematic review. Telemed J E Health. 2009;15:231–240. doi: 10.1089/tmj.2008.0099. [DOI] [PubMed] [Google Scholar]
- 12.Boland P. The emerging role of cell phone technology in ambulatory care. J Ambul Care Manage. 2007;30:126–133. doi: 10.1097/01.JAC.0000264602.19629.84. [DOI] [PubMed] [Google Scholar]
- 13.Krishna S, Boren SA. Diabetes self-management care via cell phone: a systematic review. J Diabetes Sci Technol. 2008;2:509–517. doi: 10.1177/193229680800200324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mobile Access 2010. Pew Internet and American life project. 2010 http://pewinternet.org/Reports/2010/Mobile-Access-2010.aspx.
- 15.Holtz B, Lauckner C. Diabetes management via mobile phones: a systematic review. Telemed J E Health. 2012;18:175–184. doi: 10.1089/tmj.2011.0119. [DOI] [PubMed] [Google Scholar]
- 16.Riley WT, Rivera DE, Atienza AA, Nilsen W, Allison SM, Mermelstein R. Health behavior models in the age of mobile interventions: are our theories up to the task? Transl Behav Med. 2011;1:53–71. doi: 10.1007/s13142-011-0021-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hampson SE, Skinner TC, Hart J, Storey L, Gage H, Foxcroft D, et al. Effects of educational and psychosocial interventions for adolescents with diabetes mellitus: a systematic review. Health Technol Assess. 2001;5:1–79. doi: 10.3310/hta5100. [DOI] [PubMed] [Google Scholar]
- 18.Griffin S, Kinmonth AL, Skinner C, Kelly JC. Educational and psychosocial interventions for adults with diabetes: a survey of the range and types of interventions, the extent to which they have been evaluated in controlled trials and a description of their relative effectiveness as reported in existing reviews. British Diabetic Association; London: 1999. [Google Scholar]
- 19.Watson JB. Behaviorism. Norton; New York: 1925. [Google Scholar]
- 20.Dick JJ, Nundy S, Solomon MC, Bishop KN, Chin MH, Peek ME. Feasibility and usability of a text message-based program for diabetes self-management in an urban African-American population. J Diabetes Sci Technol. 2011;5:1246–1254. doi: 10.1177/193229681100500534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Morgan DL. Focus groups as qualitative research. Sage Publications; Thousand Oaks, CA: 1997. [Google Scholar]
- 22.Barrera M. Distinctions between social support concepts, measures, and models. Am J Community Psychol. 1986;14:413–445. [Google Scholar]
- 23.Rosenstock IM. Why people use health services. Milbank Mem Fund Q. 1966;44:94–127. [PubMed] [Google Scholar]
- 24.Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev. 1977;84:191–215. doi: 10.1037//0033-295x.84.2.191. [DOI] [PubMed] [Google Scholar]
- 25.Bandura A. Self-efficacy mechanism in human agency. Am Psychol. 1982;37:122–147. [Google Scholar]
- 26.Kaplan B, Farzanfar R, Friedman RH. Personal relationships with an intelligent interactive telephone health behaviour advisor system: a multimethod study using surveys and ethnographic interviews. Int J Med Inf. 2003;71:33–41. doi: 10.1016/s1386-5056(03)00072-8. [DOI] [PubMed] [Google Scholar]
- 27.Ralston JD, Revere D, Robins LS, Goldberg HI. Patients’ experience with a diabetes support programme based on an interactive electronic medical record: qualitative study. Br Med J. 2004;328:1159–1162. doi: 10.1136/bmj.328.7449.1159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pinnock H, Slack R, Pagliari C, Price D, Sheikh A. Understanding the potential role of mobile phone-based monitoring on asthma self-management: qualitative study. Clin Exp Allergy. 2007;37:794–802. doi: 10.1111/j.1365-2222.2007.02708.x. [DOI] [PubMed] [Google Scholar]
- 29.Seto E, Leonard KJ, Cafazzo JA, Barnsley J, Masino C, Ross HJ. Perceptions and experiences of heart failure patients and clinicians on the use of mobile phone-based telemonitoring. J Med Internet Res. 2012;14:e25. doi: 10.2196/jmir.1912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Griffith LS, Field BJ, Lustman PJ. Life stress and social support in diabetes: association with glycemic control. Int J Psychiatry Med. 1990;20:365–372. doi: 10.2190/APH4-YMBG-NVRL-VLWD. [DOI] [PubMed] [Google Scholar]
- 31.Wang CY, Fenske MM. Self-care of adults with non-insulin-dependent diabetes mellitus: influence of family and friends. Diabetes Educ. 1996;22:465–470. doi: 10.1177/014572179602200506. [DOI] [PubMed] [Google Scholar]
- 32.Garay-Sevilla ME, Nava LE, Malacara JM, Huerta R, Díaz de León J, Mena A, et al. Adherence to treatment and social support in patients with non-insulin dependent diabetes mellitus. J Diabetes Complications. 1995;9:81–86. doi: 10.1016/1056-8727(94)00021-f. [DOI] [PubMed] [Google Scholar]
- 33.Ford ME, Tilley BC, McDonald PE. Social support among African-American adults with diabetes. Part 2. A review. J Natl Med Assoc. 1998;90:425–432. [PMC free article] [PubMed] [Google Scholar]
- 34.McDonald PE, Wykle ML, Misra R, Suwonnaroop N, Burant CJ. Predictors of social support, acceptance, health-promoting behaviors, and glycemic control in African-Americans with type 2 diabetes. J Natl Black Nurses Assoc. 2002;13:23–30. [PubMed] [Google Scholar]
- 35.Rosland AM, Kieffer E, Israel B, Cofield M, Palmisano G, Sinco B, et al. When is social support important? The association of family support and professional support with specific diabetes self-management behaviors. J Gen Intern Med. 2008;23:1992–1999. doi: 10.1007/s11606-008-0814-7. Epub 2008 Oct 15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Harvey JN, Lawson VL. The importance of health belief models in determining self-care behaviour in diabetes. Diabet Med. 2009;26:5–13. doi: 10.1111/j.1464-5491.2008.02628.x. Review. [DOI] [PubMed] [Google Scholar]
- 37.Schafer LC, Glasgow RE, McCaul KD, Dreher M. Adherence to IDDM regimens: relationship to psychosocial variables and metabolic control. Diabetes Care. 1983;6:493–498. doi: 10.2337/diacare.6.5.493. [DOI] [PubMed] [Google Scholar]
- 38.Cerkoney KA, Hart LK. The relationship between the health belief model and compliance of persons with diabetes mellitus. Diabetes Care. 1980;3:594–598. doi: 10.2337/diacare.3.5.594. [DOI] [PubMed] [Google Scholar]
- 39.Sarkar U, Fisher L, Schillinger D. Is self-efficacy associated with diabetes self-management across race/ethnicity and health literacy? Diabetes Care. 2006;29:823–829. doi: 10.2337/diacare.29.04.06.dc05-1615. [DOI] [PubMed] [Google Scholar]
- 40.Skelly AH, Marshall JR, Haughey BP, Davis PJ, Dunford RG. Self-efficacy and confidence in outcomes as determinants of self-care practices in inner-city African-American women with non-insulin-dependent diabetes. Diabetes Educ. 1995;21:38–46. doi: 10.1177/014572179502100107. [DOI] [PubMed] [Google Scholar]
- 41.Hurley AC, Shea CA. Self-efficacy: strategy for enhancing diabetes self-care. Diabetes Educ. 1992;18:146–150. doi: 10.1177/014572179201800208. [DOI] [PubMed] [Google Scholar]
- 42.Aljasem LI, Peyrot M, Wissow L, Rubin RR. The impact of barriers and self-efficacy on self-care behaviors in type 2 diabetes. Diabetes Educ. 2001;27:393–404. doi: 10.1177/014572170102700309. [DOI] [PubMed] [Google Scholar]
- 43.Charles C, Gafni A, Whelan T. Decision-making in the physician-patient encounter: revisiting the shared treatment decision-making model. Soc Sci Med. 1999;49:651–661. doi: 10.1016/s0277-9536(99)00145-8. [DOI] [PubMed] [Google Scholar]
- 44.Peek ME, Quinn MT, Gorawara-Bhat R, Odoms-Young A, Wilson SC, Chin MH. How is shared decision-making defined among African-Americans with diabetes? Patient Educ Couns. 2008;72:450–458. doi: 10.1016/j.pec.2008.05.018. [DOI] [PMC free article] [PubMed] [Google Scholar]


