Abstract
The relationship between lipid metabolism with prediabetes (impaired fasting glucose and impaired glucose tolerance) and type 2 diabetes mellitus is poorly defined. We hypothesized that a lipidomic analysis of plasma lipids might improve the understanding of this relationship. We performed lipidomic analysis measuring 259 individual lipid species, including sphingolipids, phospholipids, glycerolipids and cholesterol esters, on fasting plasma from 117 type 2 diabetes, 64 prediabetes and 170 normal glucose tolerant participants in the Australian Diabetes, Obesity and Lifestyle Study (AusDiab) then validated our findings on 1076 individuals from the San Antonio Family Heart Study (SAFHS). Logistic regression analysis of identified associations with type 2 diabetes (135 lipids) and prediabetes (134 lipids), after adjusting for multiple covariates. In addition to the expected associations with diacylglycerol, triacylglycerol and cholesterol esters, type 2 diabetes and prediabetes were positively associated with ceramide, and its precursor dihydroceramide, along with phosphatidylethanolamine, phosphatidylglycerol and phosphatidylinositol. Significant negative associations were observed with the ether-linked phospholipids alkylphosphatidylcholine and alkenylphosphatidylcholine. Most of the significant associations in the AusDiab cohort (90%) were subsequently validated in the SAFHS cohort. The aberration of the plasma lipidome associated with type 2 diabetes is clearly present in prediabetes, prior to the onset of type 2 diabetes. Lipid classes and species associated with type 2 diabetes provide support for a number of existing paradigms of dyslipidemia and suggest new avenues of investigation.
Introduction
In Australia and globally the obesity epidemic is associated with an increase in the prevalence of type 2 diabetes mellitus (T2D). If the current trend continues in Australia, the prevalence of T2D is projected to rise from 7.6% in 2000 to 11.4% by 2025 [1]. More than a third of individuals will develop T2D within their lifetime and there will be an additional 1 million Australians with T2D by the year 2025 [1]. Dyslipidemia (raised plasma triglycerides and decreased HDL-cholesterol) is independently associated with T2D. However, triglycerides represent a large number of individual molecular species while HDL and other lipoproteins consist of many different lipid classes containing multiple molecular species within each class. The relationships between the individual molecular species of lipid and T2D have not been fully investigated.
Over the past decade, the “omics” revolution has expanded to embrace “lipidomics” as a major contributor to our understanding of biological processes in health and disease. Recent studies have identified lipids associated with T2D [2] and coronary artery disease [3] as well as changes in lipid metabolism in response to therapeutics, including statins [4] and metformin [5]. Other studies have demonstrated a link between increased lipotoxicity, including increased synthesis of fatty acids, sphingolipids and phospholipids, and the development of diabetic nephropathy [6], [7], [8] and that progression to different stages of diabetic nephropathy in T2D patients is associated with differential alterations in non-esterified and esterified fatty acids [6], [8]. Lipidomics is also starting to identify potential biomarkers for risk assessment in T2D and cardiovascular disease [3], [8].
Current technology provides the ability to measure many hundreds of lipid species from a few µL of blood. Given the intimate links between carbohydrate and lipid metabolism, it seems likely that exploration of the associations between diabetes and a wide range of lipid species will provide insights into the pathophysiology of T2D. In order to investigate these associations we performed plasma lipid profiling on participants from the Australian Diabetes, Obesity and Lifestyle Study (AusDiab) study (normal glucose tolerance, prediabetes and newly diagnosed T2D; total n = 351), then validated these findings on an independent population cohort (n = 1076) from the San Antonio Family Heart Study (SAFHS).
Materials and Methods
Ethics Statement
This study was approved by the Alfred Hospital, Ethics Committee, Project No: 104/10.
Participants
AusDiab was established to measure the prevalence of T2D and risk factors for T2D and cardiovascular disease (CVD) in a national population-based cohort. Baseline testing (in 1999–2000) involved 11,247 adults aged ≥25 years residing in 42 randomly selected areas of the six states of Australia and the Northern Territory [9]. Plasma samples were collected and stored at −75°C. Demographic information, smoking history, alcohol intake, dietary intake, history of CVD and T2D were collected by questionnaire, and blood pressure and anthropometrics were measured. A two-hour oral glucose tolerance test (OGTT), fasting plasma lipids, insulin and HbA1c were determined. Written informed consent was obtained from all participants. The study group selected from the AusDiab baseline cohort consisted of 117 participants (58 men and 59 women), non-smoking, with newly diagnosed T2D (FPG ≥7.0 mM and/or 2h post load glucose ≥11.1 mM) and BMI between 20 and 35 kg/m2. These were matched for age and sex with 234 non-smoking, T2D-free controls. The control group contained 64 participants with either impaired glucose tolerance (2h post-load glucose 7.8–11.0 mM, n = 50) or impaired fasting glucose (FPG 6.1–6.9 mM, n = 19), collectively referred to as prediabetes. Five participants with IGT also had IFG. The participant characteristics are shown in Table 1.
Table 1. Baseline characteristics of the AusDiab study cohort.
| Characteristica | NGT | Prediabetesb | T2D | NGT vs | NGT vs | Prediabetes |
| (n = 170) | (n = 64) | (n = 117) | Prediabetes | T2D | vs T2D | |
| Sex (% male)c | 47.7 (81/170) | 53.1 (34/64) | 51.3 (60/117) | 0.455 | 0.545 | 0.812 |
| Age (years)d | 60 (49–72) | 69 (58–74) | 62 (52–73) | 0.004 | 0.603 | 0.083 |
| Waistd | 90.3 (83.3–98.2) | 93.6 (88.1–100.3) | 96.5 (89.0–103.9) | 0.094 | <0.001 | 0.183 |
| BMId | 26.0 (23.6–27.9) | 26.4 (24.5–29.0) | 27.9 (25.5–30.7) | 0.637 | <0.001 | 0.018 |
| Central obesity (%)c | 29.4 (50/170) | 42.2 (27/64) | 57.3 (67/117) | 0.067 | <0.001 | 0.052 |
| SBP (mm Hg)d | 133 (121–146) | 138 (127–155) | 143 (131–154) | 0.031 | <0.001 | 0.969 |
| FPG (mM)d | 5.3 (5.1–5.6) | 5.7 (5.4–6.2) | 6.9 (5.7–7.4) | <0.001 | <0.001 | <0.001 |
| 2h-PLG (mM)d | 5.8 (4.8–6.6) | 8.6 (7.0–9.6) | 11.8 (10.7–13.3) | <0.001 | <0.001 | <0.001 |
| HbA1c (mM)d | 5.11 (4.97–5.26) | 5.33 (5.13–5.47) | 5.55 (5.31–6.07) | <0.001 | <0.001 | <0.001 |
| Insulin (pmol/L)d | 83.7 (68.8–101.4) | 84.4 (68.4–118.5) | 125.0 (79.5–164.9) | 0.674 | <0.001 | <0.001 |
| Chol (mM)d | 5.7 (5.1–6.4) | 6.0 (5.3–6.8) | 5.8 (5.3–6.6) | 0.059 | 0.127 | 0.880 |
| HDL (mM)d | 1.42 (1.20–1.67) | 1.33 (1.09–1.59) | 1.22 (1.04–1.53) | 0.139 | 0.001 | 0.678 |
| LDL (mM)d | 3.67 (3.00–4.23) | 3.72 (3.02–4.62) | 3.70 (3.15–4.25) | 0.687 | 0.995 | 0.869 |
| Triglyceride (mM)d | 1.20 (0.90–1.55) | 1.84 (1.25–2.40) | 1.94 (1.29–2.89) | <0.001 | <0.001 | 0.645 |
BMI, body mass index; SBP, systolic blood pressure; FPG, fasting plasma glucose; 2h-PLG, 2 hour-post load glucose; HbA1c, glycated haemoglobin; Chol, total cholesterol; HDL, high density cholesterol; LDL, low density cholesterol.
Prediabetes group consists of 24 IFG and 45 IGT.
Values expressed as % (number/total), p-values (Chi-squared test).
Data are expressed as median (interquartile range), p-values (Mann-Whitney U test with Dunn-Sidak correction).
The SAFHS commenced in 1991 and was designed to investigate the genetics of cardiovascular disease and its risk factors in Mexican Americans. The SAFHS included 1,431 individuals in 42 extended families [10]. Questionnaires and anthropometric measurements were performed. Plasma cholesterol, HDL-C, triglycerides, glucose and insulin were also measured. Plasma samples were collected and stored at −75°C. In this population, we were able to access samples from the whole study, and analysed samples from 1,076 participants for which plasma and complete data were available (126 prediabetes, 142 T2D of whom 69 were not on any medication). The participant characteristics are shown in Table 2.
Table 2. Baseline characteristics of the SAHFS study cohort.
| Characteristica | NGTb | Prediabetesc | T2Dd | NGT vs | NGT vs | Prediabetes |
| (n = 808) | (n = 126) | (n = 142) | Prediabetes | T2D | vs T2D | |
| Sex (% male)e | 40.6 (328/808) | 32.5% (41/126) | 36.6 (52/142) | 0.085 | 0.372 | 0.484 |
| Age (years)f | 31 (23–44) | 46 (36–54) | 51 (44–63) | <0.001 | <0.001 | 0.001 |
| Waistf | 90.0 (79.7–100.0) | 103.0 (92.4–18.5) | 102.8 (96.2–116.5) | <0.001 | <0.001 | 0.705 |
| BMIf | 27.5 (24.0–31.5) | 31.5 (27.8–36.6) | 30.9 (28.5–36.0) | <0.001 | <0.001 | 1.000 |
| Central obesity (%)e | 37.9 (306/808) | 77.8 (98/126) | 73.9 (105/142) | <0.001 | <0.001 | 0.465 |
| SBP (mm Hg)f | 114 (106–123) | 121 (112–138) | 131 (118–147) | <0.001 | <0.001 | 0.001 |
| FPG (mM)f | 4.7 (4.4–5.0) | 5.30 (4.9–5.7) | 8.8 (7.1–12.5) | <0.001 | <0.001 | <0.001 |
| 2h-PLG (mM)f | 5.1 (4.3–6.0) | 8.5 (7.9–9.3) | 17.8 (14.0–20.7) | <0.001 | <0.001 | <0.001 |
| Insulin (pmol/L)f | 66.9 (43.6–103.3) | 107.5 (70.8–164.9) | 122.2 (77.8–221.2) | <0.001 | <0.001 | 0.530 |
| Chol (mM)f | 4.7 (4.1–5.4) | 5.1 (4.4–5.7) | 5.2 (4.6–6.1) | 0.001 | <0.001 | 0.503 |
| HDL (mM)f | 1.24 (1.09–1.50) | 1.24 (1.03–1.42) | 1.20 (1.03–1.45) | 0.493 | 0.067 | 0.876 |
| LDL (mM)f | 2.83 (2.29–3.37) | 2.99 (2.46–3.50) | 3.06 (2.53–3.71) | 0.191 | 0.002 | 0.606 |
| Triglyceride (mM)f | 1.22 (0.87–1.66) | 1.84 (1.26–2.42) | 1.94 (1.46–2.55) | <0.001 | <0.001 | 0.213 |
BMI, body mass index; SBP, systolic blood pressure; FPG, fasting plasma glucose; 2h-PLG, 2 hour-post load glucose; HbA1c, glycated haemoglobin; Chol, total cholesterol; HDL, high density lipoprotein cholesterol; LDL, low density lipoprotein cholesterol.
NGT group contains 12 individuals on lipid lowering medication.
Prediabetes group consists of 14 IFG and 112 IGT, 4 individuals were on diabetes or lipid lowering medication.
Type 2 diabetes group consists of 69 untreated and 73 treated (diabetes or lipid lowering medication).
Values expressed as % (number/total), p-values (Chi-squared test).
Expressed as median (interquartile range), p-values (Mann-Whitney U test with Dunn-Sidak correction).
Sample preparation and lipid extraction
The order of the plasma samples was randomised prior to lipid extraction and analysis for each cohort. Quality control plasma samples were included at a ratio of 1∶11 (AusDiab) and 1∶18 (SAFHS). Total lipid extraction from a 10 µL aliquot of plasma was performed by a single phase chloroform:methanol (2∶1) extraction [3].
High performance liquid chromatography-mass spectrometry analysis
Lipid analysis was performed by liquid chromatography, electrospray ionisation-tandem mass spectrometry using a Agilent 1200 liquid chromatography system combined with an Applied Biosystems API 4000 Q/TRAP mass spectrometer with a turbo-ionspray source (350°C) and Analyst 1.5 data system [3]. We have previously reported the use of precursor ion and neutral loss scans on control plasma extracts to identify the predominant lipid species of the following lipid classes: dihydroceramide (dhCer), ceramide (Cer), monohexosylceramide (MHC), dihexosylceramide (DHC), trihexosylcermide (THC), GM3 ganglioside (GM3), sphingomyelin (SM), phosphatidylcholine (PC), alkylphosphatidylcholine (PC(O)), alkenylphosphatidylcholine (plasmalogen, PC(P)), lysophosphatidylcholine (LPC), lysoalkylphosphatidylcholine (lysoplatelet activating factor, LPC(O)), phosphatidylethanolamine (PE), phosphatidylinositol (PI), phosphatidylserine (PS), phosphatidylglycerol (PG), cholesterol ester (CE), free cholesterol (COH), diacylglycerol (DG) and triaclyglycerol (TG) [3], [11], [12]. The abbreviations shown above are only used when referring to individual lipid species as in LPC 22∶6 which defines a lysophosphatidylcholine with a fatty acid containing 22 carbons and six double bonds. For a number of the lipids which contain two fatty acid chains the mass spectrometry based measurements here do not directly determine the constituent fatty acids but rather the sum of the number of carbons and the sum of the number of double bonds across both fatty acids. Accordingly, we denote these species as the combined length and number of double bonds, e.g. PC 36∶4. It is worth noting however that based on previous work by us and others the identity of at least the major fatty acids making up such a species in plasma may be reasonably inferred.
Multiple Reaction Monitoring (MRM) experiments were established for the major species of each lipid class identified in plasma. A total of 65 diacylglycerol and triacylglycerol species and 194 other lipid species were analysed in two separate experiments. Relative lipid amounts were calculated by relating the peak area of each species to the peak area of the corresponding stable isotope or non-physiological internal standard. Total lipid classes were calculated from the sum of the individual lipid species within each class [3].
Statistical analysis
Percentage coefficient of variation for each lipid species across each analytical run (AusDiab or SAFHS) was calculated as the standard deviation divided by the mean of the quality control samples. Binary logistic regression adjusted for age, sex, waist circumference and systolic blood pressure (SBP) was used to determine the strength of association of each lipid species and each lipid class with T2D and prediabetes. Linear regression adjusted for age, sex, waist circumference and SBP was used to describe the linear relationship between lipids and FPG or 2h-PLG. Samples with missing covariate values were excluded from the analysis. The odds ratio obtained for each lipid or lipid class represents the number of times an individual with a lipid measurement in the 75th percentile is more likely to have T2D or prediabetes than an individual with a lipid measurement in the 25th percentile. The beta-coefficients obtained represent the change in outcome measure (FPG or 2h-PLG) associated with an interquartile range increase in the lipid measurement. All p-values obtained were corrected for multiple comparisons using the Benjamini-Hochberg approach [13]. A corrected p-value of <0.05 was considered to be statistically significant. Linear and logistic regression were initially performed on subjects from the AusDiab cohort and subsequently repeated on the SAFHS cohort. Pearson's linear correlation was used to determine the agreement of odds ratios and beta-coefficients between the two cohorts.
Results
Preliminary analyses showed that the lipid profiles characterising T2D and prediabetes were similar to each other, and that restricting analyses to comparisons of those with and without diabetes might mask important findings. Results are therefore presented separately for the three groups (NGT, prediabetes and T2D).
Study cohort
In the AusDiab cohort the median age of the prediabetes group was greater than the NGT group and the T2D group (Table 1). There was no difference in waist circumference between the T2D and prediabetes groups but mean waist circumference was significantly higher in the T2D group compared to the NGT group. Both T2D and prediabetes showed a higher SBP, total cholesterol and triglyceride concentrations relative to the NGT group. FPG, 2h-PLG, HbA1c and fasting insulin levels were also significantly different between groups (Table 1).
The SAFHS cohort had a prevalence of T2D of 13.2% (6.4% not on any medication) and a prevalence of prediabetes (IFG or IGT) of 11.7%. Comparing SAFHS to AusDiab, SAFHS had fewer men (39.1% vs 49.9%), and were significantly younger (median age of 35.7 vs 61.7 years), and SBP was correspondingly lower (median of 117 vs 140 mmHg). Measures of plasma lipids were also substantially lower in the SAFHS cohort (Table 2).
Lipid measurements
Determination of relative lipid levels was performed using scheduled multiple-reaction monitoring (MRM) in positive ion mode [3], [11], [12], [14], [15], [16] (Table S1 in File S1). The median percentage coefficient of variation (% CV) for the individual lipid species within the quality control samples of the AusDiab analysis was 10.3% with 90% of lipids below 17.0%. In the SAFHS analysis the median % CV was 14.3% with 90% of lipids below 24.7%.
Association of lipids with type 2 diabetes and prediabetes
When the relative amounts of the lipid species within each lipid class were summed (total lipid classes), we found that, compared to the NGT group, and after adjusting for age, sex, waist circumference and SBP, each of the following lipid classes were significantly associated with the presence of T2D and with prediabetes: dihydroceramide, ceramide, alkylphosphatidylcholine, phosphatidylethanolamine, phosphatidylinositol, phosphatidylglycerol, cholesterol ester, diacylglycerol and triacylglycerol, (all p<0.05, Table 3). Alkenylphosphatidylcholine showed a similar effect size to alkylphosphatidylcholine (OR = 0.66 and 0.63 respectively); however, this was not significant. Free cholesterol was significantly associated with prediabetes but not T2D.
Table 3. Logistic regression of lipid classes against diabetes and prediabetes in the AusDiab cohort.
| Lipid Class | Diabetes vs. NGTa | Prediabetes vs. NGTb | ||||
| Odds Ratioc | p-valued | % differencee | Odds Ratiod | p-valuee | % differenceb | |
| Dihydroceramide | 1.90 (1.37–2.64) | 6.64E-04 | 25.9 | 2.03 (1.42–2.91) | 1.07E-03 | 24.5 |
| Ceramide | 1.70 (1.13–2.55) | 3.18E-02 | 11.8 | 1.85 (1.16–2.95) | 2.43E-02 | 13.9 |
| Monohexosylceramide | 1.04 (0.74–1.47) | 9.20E-01 | −0.3 | 1.33 (0.89–2.00) | 2.57E-01 | 8.1 |
| Dihexosylceramide | 0.69 (0.48–1.00) | 1.08E-01 | −7.2 | 0.84 (0.56–1.26) | 5.47E-01 | −0.9 |
| Trihexosylceramide | 0.90 (0.60–1.34) | 8.15E-01 | −6.1 | 0.60 (0.37–0.99) | 8.64E-02 | −4.1 |
| GM3 ganglioside | 0.96 (0.65–1.42) | 9.20E-01 | −2.2 | 1.12 (0.71–1.76) | 6.88E-01 | 5.5 |
| Sphingomyelin | 0.99 (0.65–1.49) | 9.78E-01 | 0.9 | 1.18 (0.74–1.87) | 6.35E-01 | 2.8 |
| Phosphatidylcholine | 1.12 (0.81–1.55) | 7.10E-01 | 2.4 | 1.20 (0.84–1.70) | 4.65E-01 | 3.0 |
| Alkylphosphatidylcholine | 0.67 (0.49–0.93) | 3.94E-02 | −3.8 | 0.62 (0.41–0.92) | 4.18E-02 | −3.2 |
| Alkenylphosphatidylcholine | 0.67 (0.45–1.01) | 1.08E-01 | −8.0 | 0.65 (0.39–1.06) | 1.41E-01 | −4.4 |
| Lysophosphatidylcholine | 1.00 (0.72–1.40) | 9.78E-01 | −2.6 | 1.52 (1.03–2.26) | 7.46E-02 | 4.8 |
| Lysoalkylphosphatidylcholine | 0.74 (0.52–1.07) | 1.81E-01 | −8.3 | 1.00 (0.68–1.47) | 9.94E-01 | −0.8 |
| Phosphatidylethanolamine | 2.29 (1.51–3.48) | 6.64E-04 | 31.3 | 2.01 (1.25–3.21) | 1.37E-02 | 19.6 |
| Phosphatidylinositol | 1.67 (1.12–2.47) | 3.18E-02 | 10.8 | 2.08 (1.26–3.43) | 1.37E-02 | 11.1 |
| Phosphatidylserine | 1.21 (0.92–1.60) | 2.78E-01 | 11.3 | 1.08 (0.83–1.42) | 6.87E-01 | 4.1 |
| Phosphatidylglycerol | 1.85 (1.29–2.64) | 3.17E-03 | 30.7 | 2.03 (1.34–3.08) | 5.72E-03 | 25.7 |
| Free cholesterol | 1.07 (0.80–1.44) | 8.17E-01 | 2.8 | 1.72 (1.17–2.53) | 1.65E-02 | 17.0 |
| Cholesterol ester | 2.39 (1.67–3.41) | 2.89E-05 | 32.7 | 1.85 (1.22–2.80) | 1.37E-02 | 21.1 |
| Diacylglycerol | 2.98 (1.92–4.62) | 2.89E-05 | 59.9 | 2.78 (1.81–4.28) | 7.39E-05 | 49.4 |
| Triacylglycerol | 2.47 (1.68–3.62) | 4.46E-05 | 53.0 | 2.79 (1.80–4.32) | 7.39E-05 | 47.6 |
Logistic regression of T2D (n = 116) against NGT (n = 168) on lipid classes adjusted for age, sex, waist circumference and SBP.
Logistic regression of prediabetes (n = 64) against NGT (n = 168) on lipid classes adjusted for age, sex, waist circumference and SBP.
Odds ratio (95% confidence intervals) based on an interquartile range increase in predictor lipid class measurement.
Benjamini-Hochberg corrected p-value. Bold type indicates corrected p<0.05.
% difference in means between groups.
Compared to NGT, 135 of the 259 lipid species were significantly associated with T2D, and 134 lipid species were significantly associated with prediabetes, after adjustment for age, sex, waist circumference and SBP (p<0.05, Tables S2 and S3 in File S1). Within each lipid class we observed considerable variation of the odds ratio of individual lipid species for each of the outcomes. Odds ratios of the cholesterol ester species for T2D ranged from 0.91 (95% CI: 0.69–1.21, p = 0.631) for CE 20∶1 to 2.88 (95% CI: 1.89–4.39, p = .94×10−5) for CE 16∶1. While sphingomyelin and phosphatidylcholine classes were not significantly associated with T2D, individual species containing odd chain (C15∶0 and C17∶0 fatty acids) showed contrasting associations with those containing even chain fatty acids. Five of the odd chain species showed significant negative associations with T2D (odds ratios 0.45–0.58). In contrast two of the even chain species showed significant positive associations (odds ratios of 1.68 and 1.84) (Table S3 in File S1). Odd chain fatty acids are primarily derived from ruminant fat with the primary source being ruminant fat, including dairy food; linear regression analysis of the 20 odd chain species in this study against full fat dairy intake, adjusted for age, sex, waist circumference and SBP, showed 12 to be significantly associated (after correction for multiple comparisons, p values ranging from 0.015 to 4.89×10−5) including SM 39∶1, PC 33∶2 and PC 35∶2 which were negatively associated with T2D.
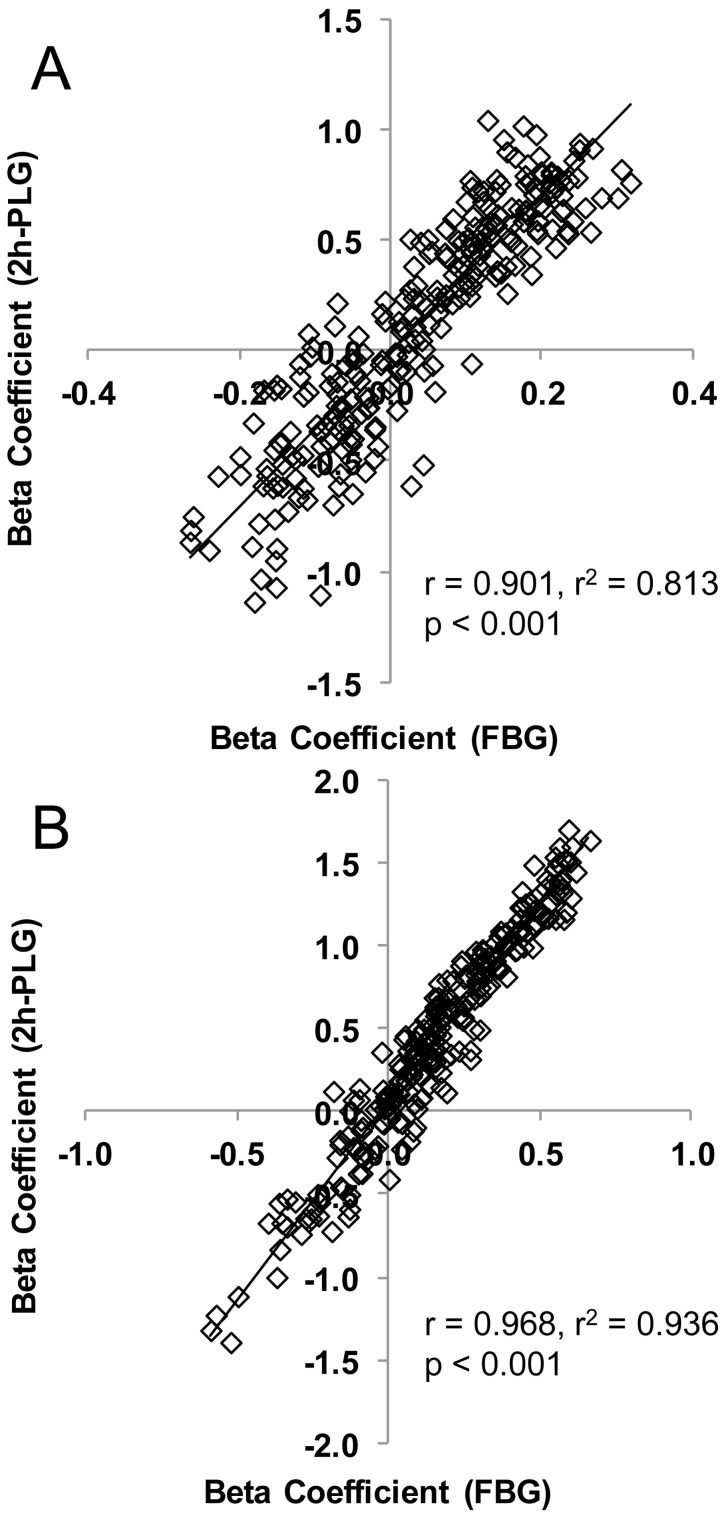
Association of lipids with fasting plasma glucose and 2h-post load glucose
As diabetes and prediabetes are based on arbitrary glucose cut-off points we also performed linear regression of lipids against FPG and 2h-post load glucose (2h-PLG), adjusting for age, sex, waist circumference and SBP. Dihydroceramide, phosphatidylethanolamine, phosphatidylglycerol, cholesterol ester, diacylglycerol and triacylglycerol lipid classes were all associated with FPG, while dihexosylceramide, lysoalkylphosphatidylcholine were negatively associated (Table 4). The same classes were also associated with 2h-PLG, or showed the same association. Interestingly the ether-linked lipids alkylphosphatidylcholine and alkenylphosphatidylcholine were also negatively associated with 2h-PLG (Table 4). There were 54 individual lipid species that were significantly associated with FPG, while 115 were significantly associated with 2h-PLG (Table S6 in File S1). Overall, the beta coefficients for FPG were highly correlated with the beta coefficients for 2h-PLG (r = 0.901, Figure 1A).
Table 4. Linear regression of lipid classes in the AusDiab and SAFHS cohorts.
| FPGa (AusDiab) | 2h-PLGb (AusDiab) | FPGa (SAFHS) | 2h-PLGb (SAFHS) | |||||
| Lipid Class | Beta Coeff.c | p-valued | Beta Coeff.c | p-valued | Beta Coeff.c | p-valued | Beta Coeff.c | p-valued |
| Dihydroceramide | 0.19 (0.07–0.30) | 1.11E-02 | 0.44 (0.07–0.82) | 5.27E-02 | 0.57 (0.40–0.73) | 5.11E-10 | 1.20 (0.86–1.53) | 2.09E-11 |
| Ceramide | 0.06 (−0.09–0.22) | 5.39E-01 | 0.31 (−0.18–0.80) | 3.20E-01 | 0.54 (0.36–0.72) | 1.89E-08 | 1.33 (0.98–1.68) | 1.82E-12 |
| Monohexosylceramide | −0.17 (−0.32–−0.02) | 7.41E-02 | −0.20 (−0.67–0.28) | 4.55E-01 | −0.09 (−0.27–0.09) | 4.06E-01 | −0.12 (−0.48–0.23) | 5.70E-01 |
| Dihexosylceramide | −0.22 (−0.37–−0.08) | 1.11E-02 | −0.58 (−1.03–−0.12) | 4.09E-02 | −0.26 (−0.44–−0.08) | 9.34E-03 | −0.57 (−0.93–−0.20) | 4.25E-03 |
| Trihexosylceramide | −0.11 (−0.28–0.06) | 3.56E-01 | −0.18 (−0.72–0.36) | 5.41E-01 | −0.19 (−0.36–−0.01) | 5.67E-02 | −0.43 (−0.78–−0.09) | 2.10E-02 |
| GM3 ganglioside | −0.06 (−0.23–0.11) | 5.42E-01 | −0.25 (−0.78–0.27) | 4.02E-01 | 0.22 (0.04–0.41) | 2.94E-02 | 0.46 (0.10–0.83) | 1.96E-02 |
| Sphingomyelin | −0.08 (−0.25–0.09) | 4.86E-01 | −0.33 (−0.86–0.20) | 3.20E-01 | −0.07 (−0.27–0.12) | 5.24E-01 | −0.12 (−0.51–0.27) | 5.91E-01 |
| Phosphatidylcholine | 0.03 (−0.10–0.17) | 6.75E-01 | −0.27 (−0.69–0.15) | 3.20E-01 | 0.16 (−0.03–0.35) | 1.39E-01 | 0.64 (0.26–1.03) | 2.10E-03 |
| Alkylphosphatidylcholine | −0.08 (−0.22–0.05) | 3.56E-01 | −0.53 (−0.95–−0.11) | 4.09E-02 | −0.01 (−0.20–0.17) | 9.37E-01 | −0.30 (−0.67–0.07) | 1.40E-01 |
| Alkenylphosphatidylcholine | −0.11 (−0.28–0.06) | 3.56E-01 | −0.66 (−1.20–−0.13) | 4.09E-02 | −0.18 (−0.35–0.00) | 6.75E-02 | −0.69 (−1.03–−0.35) | 1.96E-04 |
| Lysophosphatidylcholine | −0.14 (−0.28–0.00) | 1.24E-01 | −0.34 (−0.78–0.10) | 2.67E-01 | 0.02 (−0.16–0.19) | 9.37E-01 | −0.08 (−0.43–0.27) | 6.53E-01 |
| Lysoalkylphosphatidylcholine | −0.23 (−0.38–−0.09) | 1.11E-02 | −0.27 (−0.74–0.19) | 3.47E-01 | −0.36 (−0.54–−0.18) | 2.45E-04 | −0.79 (−1.15–−0.43) | 6.35E-05 |
| Phosphatidylethanolamine | 0.24 (0.09–0.40) | 1.11E-02 | 0.76 (0.28–1.24) | 1.16E-02 | 0.62 (0.44–0.80) | 2.07E-10 | 1.68 (1.33–2.03) | 5.42E-19 |
| Phosphatidylinositol | 0.04 (−0.13–0.21) | 6.75E-01 | 0.29 (−0.23–0.81) | 3.57E-01 | 0.18 (−0.01–0.37) | 9.50E-02 | 0.65 (0.27–1.03) | 1.63E-03 |
| Phosphatidylserine | 0.05 (−0.06–0.16) | 4.86E-01 | 0.29 (−0.06–0.64) | 2.38E-01 | 0.00 (−0.14–0.15) | 9.50E-01 | 0.09 (−0.21–0.39) | 5.91E-01 |
| Phosphatidylglycerol | 0.20 (0.06–0.34) | 1.72E-02 | 0.58 (0.14–1.01) | 4.09E-02 | 0.43 (0.26–0.59) | 1.65E-06 | 1.22 (0.89–1.54) | 2.58E-12 |
| Free cholesterol | −0.05 (−0.20–0.09) | 5.42E-01 | −0.22 (−0.66–0.23) | 4.02E-01 | 0.13 (−0.05–0.31) | 1.94E-01 | 0.32 (−0.04–0.68) | 1.02E-01 |
| Cholesterol ester | 0.24 (0.11–0.37) | 5.71E-03 | 0.82 (0.41–1.23) | 9.91E-04 | 0.50 (0.33–0.67) | 8.99E-08 | 1.22 (0.88–1.57) | 2.09E-11 |
| Diacylglycerol | 0.19 (0.05–0.33) | 1.94E-02 | 1.02 (0.60–1.44) | 6.06E-05 | 0.57 (0.42–0.72) | 6.40E-12 | 1.44 (1.14–1.74) | 4.51E-19 |
| Triacylglycerol | 0.20 (0.07–0.32) | 1.11E-02 | 0.73 (0.35–1.12) | 1.74E-03 | 0.44 (0.27–0.60) | 8.18E-07 | 1.26 (0.93–1.58) | 4.06E-13 |
Linear regression of FPG on lipid classes adjusted for age, sex, waist circumference and SBP.
Linear regression of 2h-PLG on lipid classes adjusted for age, sex, waist circumference and SBP.
Beta coefficient (95% confidence intervals) based on an interquartile range increase in predictor lipid class measurement.
Benjamini-Hochberg corrected p-value. Bold type indicates corrected p<0.05.
Figure 1. The relationship between beta-coefficients (FPG) and beta-coefficients (2h-PLG) in AusDiab and SAFHS.
Linear regression of FPG and 2h-PLG on lipid species adjusted for age, sex, waist circumference and SBP were performed. Each data point represents a pair of the beta coefficients (FPG and 2h-PLG) for a single lipid species. Panel A – AusDiab; panel B – SAFHS.
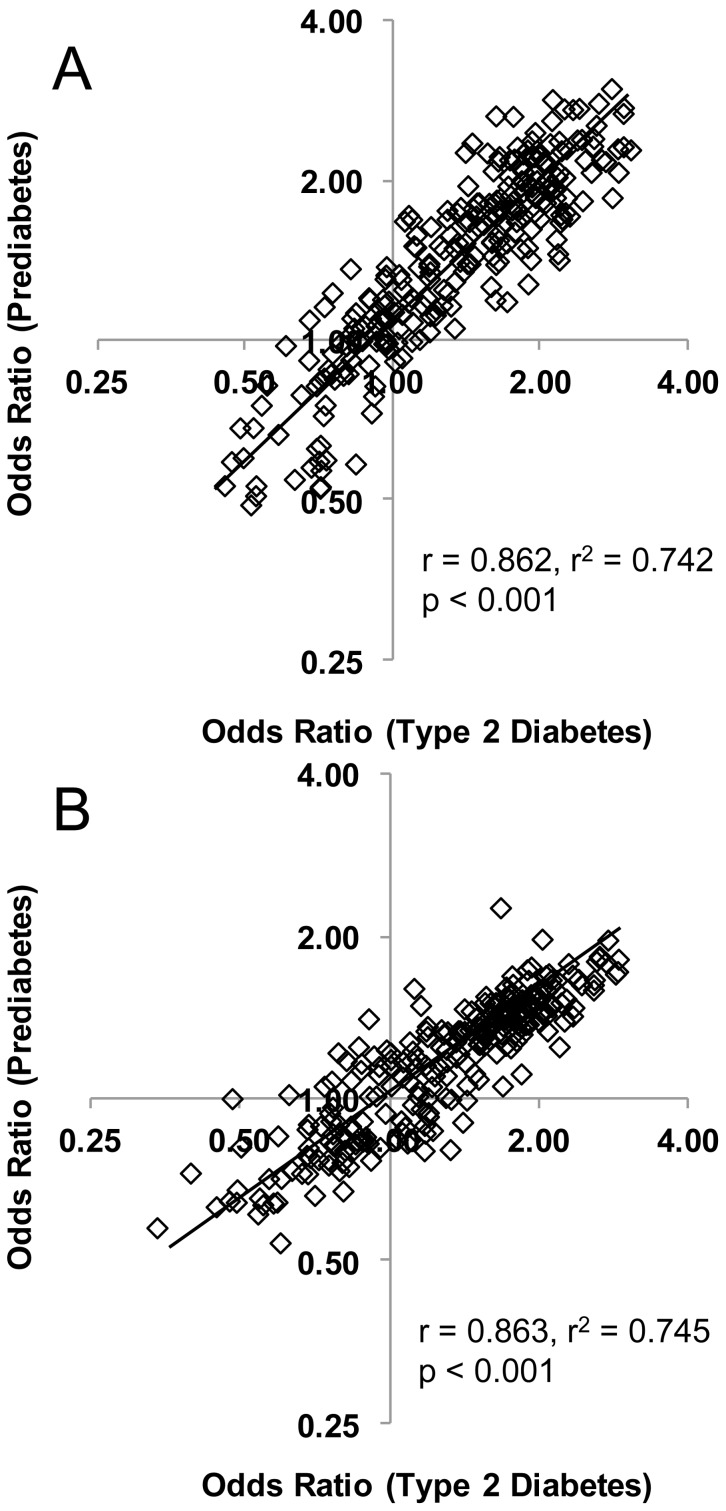
The relationship between type 2 diabetes and prediabetes
The lipid profile associated with prediabetes was strikingly similar to the lipid profile for T2D. All nine of the lipid classes associated with T2D (relative to NGT) were also associated with prediabetes (Table 3). Of the 135 lipid species associated with T2D, 111 were significantly associated with prediabetes and the remaining 24 showed non-significant associations in the same direction (Table S3 in File S1). There were no significant associations of lipid species or classes with T2D relative to prediabetes from adjusted (age, sex, waist circumference and SBP) binary logistic regression. The similarity in lipid profiles between T2D and prediabetes is further evidenced by a linear correlation coefficient of r = 0.862 between their odds ratios in the AusDiab cohort (Figure 2A).
Figure 2. The relationship between odds ratios (T2D) and odds ratios (prediabetes) in AusDiab and SAFHS.
Logistic regression of T2D and prediabetes on lipid species adjusted for age, sex, waist circumference and SBP were performed. Each data point represents a pair of the odds ratios (T2D and prediabetes) for a single lipid species. Panel A – AusDiab; panel B – SAFHS.
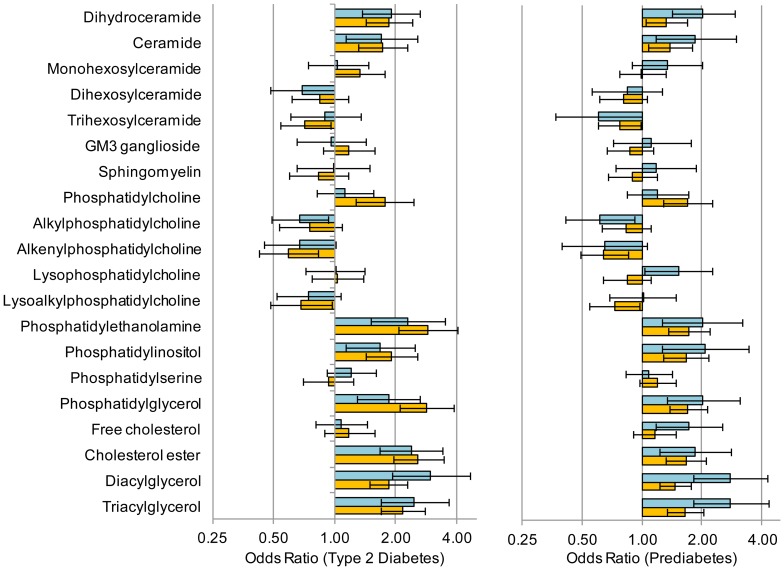
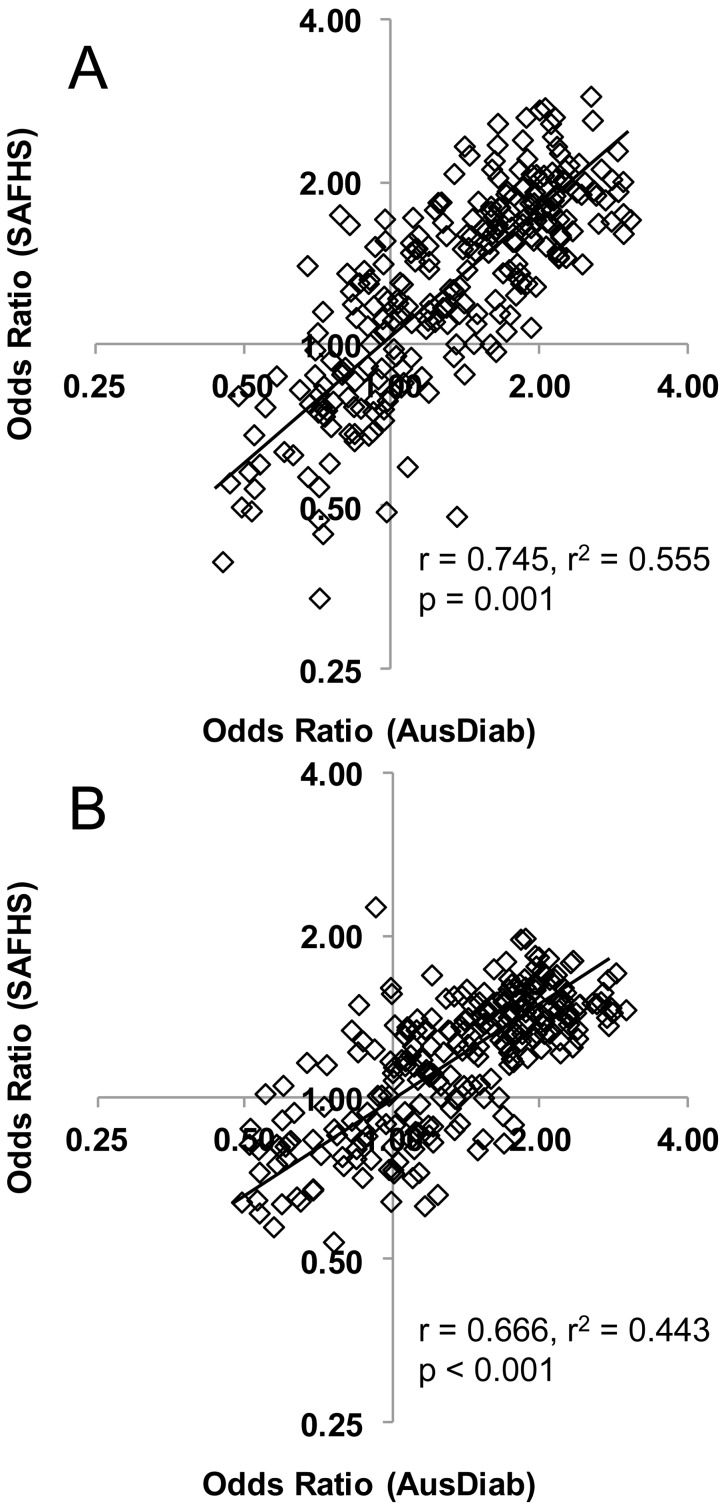
Validation of the AusDiab findings in the SAFHS
Lipid profiling was performed on the SAFHS cohort and the same logistic regression analyses performed utilising the T2D (n = 69), prediabetes (n = 122) and the NGT (n = 796) who were not on any diabetes or lipid lowering medication. Eight out of the nine lipid classes that were significantly associated with T2D and prediabetes in AusDiab were also significantly associated with each outcome in SAFHS (Figure 3). Alkylphosphatidylcholine which showed a significant negative association with both T2D and prediabetes in the AusDiab cohort showed a non-significant negative association in the SAFHS cohort. Of the 135 individual lipid species that were significantly associated with T2D in the AusDiab cohort, 121 (90%) were also significantly associated (in the same direction) with T2D in the SAFHS cohort (Tables S2 and S5 in File S1). Similarly, the associations with prediabetes were confirmed in 104 of 134 lipid species (78%) (Tables S2 and S5 in File S1). Of the 14 species which did not show a significant association with T2D in the SAFHS two were odd chain lipids and seven were diacylglycerol and triacylglycerol species, notably containing one or more linoleic acid (C18∶2). No lipids showed contrasting significant associations between the two studies. A plot of the odds ratios for T2D in the AusDiab cohort against the SAFHS cohort showed a strong linear correlation (r = 0.775), while the correlation between the odds ratios for prediabetes between AusDiab and SAFHS was r = 0.666 (Figure 4). Linear regression against FPG and 2h-PLG also showed all of the same associations with lipid classes as seen in the AusDiab cohort (Table 4). The additional power of the larger SAFHS cohort also revealed associations of FPG with ceramide and GM3 ganglioside and of 2h-PLG with ceramide, phosphatidylcholine and phosphatidylinositol, while 2h-PLG was also negatively associated with trihexosylceramide and lysoalkylphosphatidylcholine but not with alkylphosphatidylcholine (Table 4). Of the 54 species associated with FPG in the AusDiab, 47 were also associated in the SAFHS. Similarly, of the 115 species associated with 2-PLG, 97 showed the same association in the SAFHS (Table S6 in File S1). As in the AusDiab cohort the beta coefficients for FPG and 2h-PLG in the SAFHS were highly correlated (r = 0.968, Figure 1B).
Figure 3. Associations of lipid classes with T2D and prediabetes in the AusDiab and SAHFS cohorts.
Logistic regression of T2D and prediabetes on lipid species adjusted for age, sex, waist circumference and SBP were performed. Bars show the odds ratio for each lipid class, whiskers are the 95% confidence intervals. Panel A – T2D vs. NGT; panel B – prediabetes vs. NGT. Dark bars – AusDiab; light bars – SAFHS.
Figure 4. The relationship between AusDiab and SAFHS in the odds ratios (T2D) and odds ratios (prediabetes).
Logistic regression of T2D and prediabetes on lipid species adjusted for age, sex, waist circumference and SBP were performed in the AusDiab and SAFHS cohorts. Each data point represents a pair of the odds ratios (AusDiab and SAFHS) for a single lipid species. Panel A – Odds ratios for T2D; panel B – Odds ratios for prediabetes.
Discussion
Our lipidomic analysis of a large case control cohort from the AusDiab study has identified a range of novel associations at both the lipid class and lipid species level. The plasma lipid profiles demonstrate that the differences in plasma lipids between T2D and NGT are clearly established in the prediabetes state.
Many lipidomic studies have been limited by small sample sizes resulting in a lack of statistical power and/or the inability to provide an independent validation of the findings. In this study we were able to utilise 351 participants of the AusDiab study to provide sufficient power to show significant associations with both prediabetes and T2D independent of each other and other covariates. Importantly, 90% of the lipids that were significantly associated with T2D in the AusDiab cohort were also significantly associated, and showed the same direction of association, with T2D in the larger population-based SAFHS cohort.
The initial cross-sectional case-control design from the AusDiab cohort in this study matched 117 cases (T2D) with 234 controls (NGT, IFG and IGT) for age, sex and waist circumference. Preliminary analyses identified that the plasma lipid profiles of the prediabetes individuals (IFG and IGT) were more similar to the T2D group than the NGT group. Stratification of the cohort into NGT and prediabetes groups resulted in significant differences in age and waist circumference requiring adjustment in the subsequent logistic regression analyses. Further to this, the SAFHS validation cohort (n = 1076) was limited by a number of factors; the SAFHS cohort had fewer males (39% vs. 50%), was substantially younger (median age of 35 vs. 62) and had lower blood pressure (median SBP of 117 vs. 137) compared to the AusDiab cohort. The SAFHS was a population study (as opposed to the AusDiab case/control study) and so had smaller proportions of T2D and prediabetes relative to NGT (n = 69, 122 and 796 respectively) not on diabetes lipid lowering medication. Nonetheless, most of the observed associations in the AusDiab cohort were confirmed in the SAFHS cohort in adjusted logistic regression. However, we note that the odds ratios were indicative of a greater effect size in the AusDiab cohort compared to the SAFHS cohort. This may relate to differences in the population structure (in terms of covariates) as outlined above but may also relate to the differences in the size and relative proportions of T2D and prediabetes (IGT and IFG) groups in relation to NGT group in each cohort. In contrast to the effect size, there were more lipids significant associated with T2D in the larger SAFHS cohort than the AusDiab cohort (135 vs. 166) with generally lower p-values. It is therefore likely that larger cohorts may identify additional lipids as significant, although these will likely have smaller effect sizes.
The prediabetes group consisted of both IFG and IGT which have been reported to have different etiologies with respect to basal insulin secretion and resistance of glucose production to suppression by insulin [17]. However, despite the different etiologies in these conditions we observed very similar associations between plasma lipids and FPG and plasma lipids and 2h-PLG (Figure 1) suggesting that the aberrant lipid metabolism associated with the prediabetes state is similar in both etiologies.
The positive association of both ceramide and its biosynthetic precursor dihydroceramide with T2D and prediabetes (Figure 3) firmly places the ceramide biosynthetic pathway as a key metabolic process in T2D. This was validated in the SAFHS cohort, although the association of dihydroceramide with prediabetes was not significant after correcting for multiple comparisons (Table S4 in File S1). The apparent upregulation of de novo ceramide synthesis did not flow through to other ceramide metabolites such as sphingomyelin and the glysosphingolipids, in fact dihexosylceramide showed a negative association with T2D in the AusDiab cohort while we also observed a significant negative association with trihexosylceramide in the SAFHS cohort (Figure 5, Table 3, Table S4 in File S1).
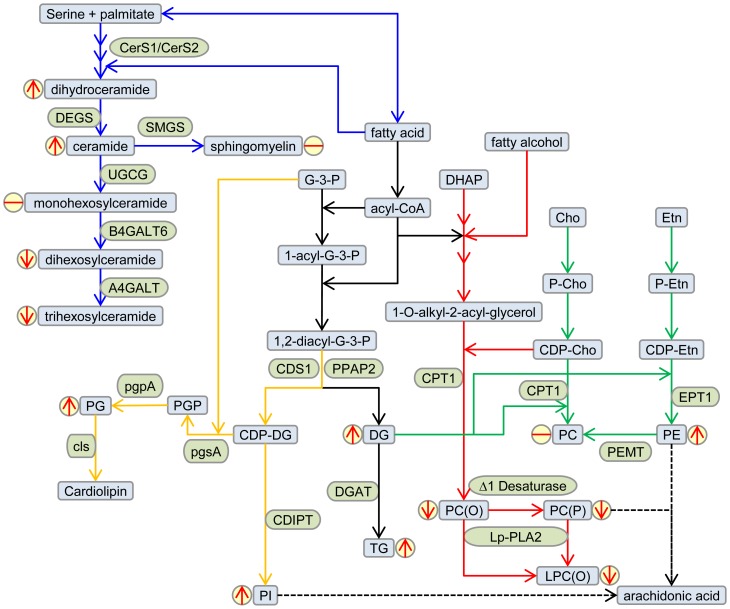
Figure 5. Metabolic pathways altered in type 2 diabetes.
Partial lipid metabolic pathways show the major lipids associated with T2D (blue boxes) and the enzymes involved (green boxes). The sphingolipid (blue arrows), cardiolipin (orange arrows), triacylglycerol (black arrows), plasmalogen (red arrows) and phosphatidylcholine/phosphatidylethanolamine (green arrows) biosynthetic pathways are shown. The direction of association between lipids and T2D is indicated by the red arrows in yellow circles. Only partial pathways have been shown for clarity. Metabolite abbreviations: Cho, choline; DG, diacylglycerol; DHAP, dihydroxyacetonephosphate; Etn, ethanolamine; LPC(O), lysoalkylphosphatidylcholine; PC, phosphatidylcholine; PE, phosphatidylethanolamine; PC(O), alkylphosphatidylcholine; PC(P), alenylphosphatidylcholine; PG, phosphatidylglycerol; PGP, phosphatidylglycerolphosphate; PI, phosphatidylinositol; TG, triacylglycerol. Enzyme abbreviations: A4GALT, lactosylceramide 4-alpha-galactosyltransferase; B4GALT6, beta-1,4-galactosyltransferase 6; CDIPT, CDP-diacylglycerol-inositol 3-phosphatidyltransferase; CDS1, phosphatidate cytidylyltransferase; CerS, ceramide synthasecls, cardiolipin synthase; CPT1, diacylglycerol cholinephosphotransferase; DEGS, sphingolipid delta-4 desaturase; DGAT, diacylglycerol O-acyltransferase; EPT1, PEMT, phosphatidylethanolamine N-methyltransferase; ethanolaminephosphotransferase, pgpA, phosphatidylglycerophosphatase A; pgsA, CDP-diacylglycerol – glycerol-3-phosphate 3-phosphatidyltransferase; PPAP2, phosphatidate phosphatase; SMGS, sphingomyelin synthase; UGCG, ceramide glucosyltransferase.
When we examined the association with the individual ceramide species and their precursors dihydroceramide, we observed that, despite being one of the least abundant dihydroceramide species, dhCer 18∶0 showed the strongest association with both T2D (IQR odds ratio = 2.95, 95% CI: 1.93–4.50, p = 5.23×10−5) and prediabetes (IQR odds ratio = 2.32, 95% CI: 1.57–3.42, p = 3.75×10−4) (Table S3 in File S1), and the corresponding ceramide species also showed the strongest associations. Ceramide synthase 1 (CerS 1) is reported to be specific for the synthesis of dhCer 18∶0/Cer 18∶0 [18] and its expression in muscle has been shown to be inversely associated with alterations in glucose tolerance in a mouse model of insulin resistance [19]. CerS 4 also shows specificity for C18∶0 and C20∶0 acyl chains but is primarily expressed in kidney, heart, spleen, and lung with only weak expression in liver and muscle [18]. CerS 2 is the predominant form in liver and shows specificity for the longer chain acyl species C20∶0, C22∶0, C24∶0 and C24∶1. Interestingly Cer 16∶0 did not show a significant association with either T2D or prediabetes and dhCer 16∶0 was only significantly associated with T2D. CerS 5 and CerS 6 are reported to have specificity for the C16∶0 acyl chain and are expressed primarily in lung and intestine/kidney respectively [20], [21]. Taken together, these results suggest an up regulation of ceramide synthesis, most likely involving CerS 1 in muscle and CerS 2 in liver. This may be further exacerbated by a down regulation of the glycosyltransferases responsible for the conversion of ceramide to dihexosylceramide and trihexosylceramide.
Although there was no significant difference between the clinical measure of total cholesterol in the NGT, T2D and prediabetes groups, the total cholesterol ester and most cholesterol ester species (determined by mass spectrometry) were strongly associated with T2D and prediabetes after adjusting for age, sex, waist circumference and SBP. This likely relates to the higher triglyceridemia and increased VLDL production associated with prediabetes and T2D [22]. Phosphatidylethanolamine, phosphatidylinositol and phosphatidylglycerol, but not phosphatidylcholine, also showed positive associations with T2D and prediabetes (Figure 5). While these associations may also relate to increased lipoprotein production, the respective roles of these lipids as a source of arachidonic acid for the production of proinflammatory eicosinoids (phosphatidylethanolamine and phosphatidylinositol) and as a substrate for the production for the mitochondrial specific lipid cardiolipin (phosphatidylglycerol) provide future avenues for investigation. A recent study has also identified phosphatidylethanolamine as a positive modulator of the membrane disruption induced by IAPP (islet amyloid polypeptide protein), an amyloidogenic protein involved in type II diabetes [23].
Of interest was the negative association of some phosphatidylcholine and sphingomyelin species containing odd chain fatty acids (C15∶0 and C17∶0) with prediabetes and T2D (Table S3 in File S1). These odd chain fatty acids are products of ruminant digestion and in human diets are derived primarily from dairy fats; a number of studies have validated the association between odd chain fatty acids and dairy intake [24], [25]. This would support a protective role for dairy against T2D and is in agreement with a mounting body of epidemiological data [26], [27], [28] as well as specific measurement of fatty acid composition that have demonstrated negative associations between C15∶0 and C17∶0 with incident T2D [29], [30] and a recent study of Mozaffarian et al. who reported a negative association between the dairy derived fatty acid, trans-palmitoleate, and incidence of T2D [31].
Negative associations with prediabetes and T2D were also observed for the ether and vinyl ether-linked phosphatidylcholine species alkylphosphatidylcholine and alkenylphosphatidylcholine. These associations were species specific (Table S3 in File S1) suggesting a complex relationship with different stages of disease. The vinyl ether linkage of the plasmalogens is particularly susceptible to oxidation by reactive oxygen species [32], [33] and as such they are proposed to play an antioxidant role in membranes and lipoproteins [34], [35], While the ether linkage of the alkylphosphatidylcholine species is not susceptible to oxidation the high proportion of polyunsaturated fatty acids in these lipids render them also susceptible to oxidative modification. Alternatively, decreased levels of these lipids in plasma may relate to a decreased biosynthesis which is thought to be controlled by the formation and availability of the long chain fatty alcohol used to produce the 1-O-alky-dihydroxyacetonephosphate in the peroxisome, an early process in plasmalogens biosynthesis [35]. Likely, it is a combination of effects controlling plasma levels and further work will be required to fully understand the drivers and consequences of alkyl- and alkenylphosphatidylcholine metabolism in T2D.
All three species of lysoalkylphosphatidylcholine [LPC(O-22∶0), LPC(O-24∶1) and LPC(O-24∶2)] were also negatively associated with T2D (Figure 5, Table S3 in File S1). This lipid, also known as lysoplatelet activating factor, is formed by the action of platelet activating factor acetylhydrolase (PAF-AH) also known as lipoprotein phospholipase A2 (Lp-PLA2) on platelet activating factor (PAF). PAF is a proinflammatory signalling lipid that is controlled by the concerted action of the biosynthetic enzyme lysophosphatidylcholine acyltransferase 2 (LPCAT2) and the catabolic action of PAF-AH/Lp-PLA2. While PAF-AH/Lp-PLA2 has been reported to be elevated in T2D [36], [37] its distribution between LDL and HDL is altered in T2D [38] and may be a critical factor in controlling the level of PAF/lyso-PAF as well as other oxidised species of phospholipid. Fan et al. investigated the HDL associated PAF-AH/Lp-PLA2 in polycystic ovary syndrome patients and observed lower PAF-AH/Lp-PLA2 in affected patients, which was associated with insulin resistance [39]. Thus PAF metabolism and/or metabolism of oxidised phosphatidylcholine species may be important processes in the progression to T2D.
Many of the alterations in lipid metabolic pathways identified in this study are linked to free fatty acids (Figure 5) which highlights the central role of elevated free fatty acids in the dysregulation of lipid homeostasis associated with T2D. The driving force of the elevated free fatty acids combined with differential regulation of metabolic pathways as well as spatial effects resulting from tissue and or plasma compartmentalisation, leads to a complex metabolic phenotype. Lipidomic studies can provide new insight for existing paradigms of lipid dysregulation, and identify new avenues to investigate the complex relationship between lipid metabolism, plasma lipids and T2D.
Supporting Information
Contains: Table S1. Conditions for precursor ion scan and MRM acquisition methods for lipid identification and analysis. Table S2. Lipid species associated with diabetes and prediabetes in the AusDiab and SAFHS cohorts. Table S3. Logistic regression of lipids against diabetes and prediabetes in the AusDiab cohort. Table S4. Logistic regression of lipid classes in the SAFHS cohort. Table S5. Logistic regression of lipids against diabetes and prediabetes in the SAFHS cohort. Table S6. Linear regression of lipid species in the AusDiab and SAFHS cohorts.
(DOCX)
Acknowledgments
The AusDiab study co-coordinated by the Baker IDI Heart and Diabetes Institute, gratefully acknowledges the study participants. We are also grateful to the participants of the San Antonio Family Heart Study.
Funding Statement
This work was supported by funding from the Dairy Health and Nutrition Consortium, Australia, The National Health and Medical Research Council of Australia, the OIS Program of the Victorian Government, Australia and by Award Number 1R01DK088972-01 from the National Institute of Diabetes and Digestive and Kidney Diseases, National Institutes of Health, USA. The content is solely the responsibility of the authors and does not necessarily represent the official views of the aforementioned funding bodies. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. The AusDiab study co-coordinated by the Baker IDI Heart and Diabetes Institute, gratefully acknowledges the generous support given by: The National Health and Medical Research Council (NHMRC grant 233200), Australian Government Department of Health and Ageing, the Dairy Health and Nutrition Consortium, Abbott Australasia Pty Ltd, Alphapharm Pty Ltd, AstraZeneca, Bristol-Myers Squibb, City Health Centre-Diabetes Service-Canberra, Department of Health and Community Services – Northern Territory, Department of Health and Human Services – Tasmania, Department of Health – New South Wales, Department of Health – Western Australia, Department of Health – South Australia, Department of Human Services – Victoria, Diabetes Australia, Diabetes Australia Northern Territory, Eli Lilly Australia, Estate of the Late Edward Wilson, GlaxoSmithKline, Jack Brockhoff Foundation, Janssen-Cilag,, Kidney Health Australia, Marian & FH Flack Trust, Menzies Research Institute, Merck Sharp & Dohme, Novartis Pharmaceuticals, Novo Nordisk Pharmaceuticals, Pfizer Pty Ltd, Pratt Foundation, Queensland Health, Roche Diagnostics Australia, Royal Prince Alfred Hospital, Sydney, Sanofi Aventis and sanofi-synthelabo. Also, for their invaluable contribution to the set-up and field activities of AusDiab, we are enormously grateful to A Allman, B Atkins, S Bennett, S Chadban, M de Courten, M Dalton, D Dunstan, T Dwyer, D Jolley, D McCarty, A Meehan, S Murray, P Phillips, C Reid, A Stewart, R Tapp, H Taylor, and F Wilson (Baker IDI Heart and Diabetes Institute). Data collection for the SAFHS was supported by grant P01 HL045522 from the National Institutes of Health (to JB). Additional work was supported by National Institutes of Health awards R01 DK082610 and R01 DK079169 (to JC), and R01 HL091035 (to JB). Parts of this investigation were conducted in facilities constructed with support from Research Facilities Improvement Program grants C06 RR013556 and C06 RR017515 from the National Center for Research Resources of the National Institutes of Health.
References
- 1. Magliano DJ, Shaw JE, Shortreed SM, Nusselder WJ, Liew D, et al. (2008) Lifetime risk and projected population prevalence of diabetes. Diabetologia 51: 2179–2186. [DOI] [PubMed] [Google Scholar]
- 2. Haus JM, Kashyap SR, Kasumov T, Zhang R, Kelly KR, et al. (2009) Plasma ceramides are elevated in obese subjects with type 2 diabetes and correlate with the severity of insulin resistance. Diabetes 58: 337–343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Meikle PJ, Wong G, Tsorotes D, Barlow CK, Weir JM, et al. (2011) Plasma lipidomic analysis of stable and unstable coronary artery disease. Arterioscler Thromb Vasc Biol 31: 2723–2732. [DOI] [PubMed] [Google Scholar]
- 4. Kaddurah-Daouk R, Baillie RA, Zhu H, Zeng ZB, Wiest MM, et al. (2010) Lipidomic analysis of variation in response to simvastatin in the Cholesterol and Pharmacogenetics Study. Metabolomics 6: 191–201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Huo T, Cai S, Lu X, Sha Y, Yu M, et al. (2009) Metabonomic study of biochemical changes in the serum of type 2 diabetes mellitus patients after the treatment of metformin hydrochloride. J Pharm Biomed Anal 49: 976–982. [DOI] [PubMed] [Google Scholar]
- 6. Han L-D, Xia J-F, Liang Q-L, Wang Y, Wang Y-M, et al. (2011) Plasma esterified and non-esterified fatty acids metabolic profiling using gas chromatography–mass spectrometry and its application in the study of diabetic mellitus and diabetic nephropathy. Analytica Chimica Acta 689: 85–91. [DOI] [PubMed] [Google Scholar]
- 7. Liu G, Han F, Yang Y, Xie Y, Jiang H, et al. (2011) Evaluation of sphingolipid metabolism in renal cortex of rats with streptozotocin-induced diabetes and the effects of rapamycin. Nephrology Dialysis Transplantation 26: 1493–1502. [DOI] [PubMed] [Google Scholar]
- 8. Zhu C, Liang Q-l, Hu P, Wang Y-m, Luo G-a (2011) Phospholipidomic identification of potential plasma biomarkers associated with type 2 diabetes mellitus and diabetic nephropathy. Talanta 85: 1711–1720. [DOI] [PubMed] [Google Scholar]
- 9. Dunstan DW, Zimmet PZ, Welborn TA, Cameron AJ, Shaw J, et al. (2002) The Australian Diabetes, Obesity and Lifestyle Study (AusDiab) – methods and response rates. Diabetes Res Clin Pract 57: 119–129. [DOI] [PubMed] [Google Scholar]
- 10. Mitchell BD, Kammerer CM, Blangero J, Mahaney MC, Rainwater DL, et al. (1996) Genetic and environmental contributions to cardiovascular risk factors in Mexican Americans. The San Antonio Family Heart Study. Circulation 94: 2159–2170. [DOI] [PubMed] [Google Scholar]
- 11. Borg ML, Andrews ZB, Duh EJ, Zechner R, Meikle PJ, et al. (2011) Pigment epithelium-derived factor regulates lipid metabolism via adipose triglyceride lipase. Diabetes 60: 1458–1466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Boslem E, MacIntosh G, Preston AM, Bartley C, Busch AK, et al. (2011) A lipidomic screen of palmitate-treated MIN6 beta-cells links sphingolipid metabolites with endoplasmic reticulum (ER) stress and impaired protein trafficking. Biochem J 435: 267–276. [DOI] [PubMed] [Google Scholar]
- 13. Benjamini Y, Hochberg Y (1995) Controlling the False Discovery Rate: A Practical and Powerful Approach to Multiple Testing. Journal of the Royal Statistical Society Series B (Methodological) 57: 289–300. [Google Scholar]
- 14. Drew BG, Carey AL, Natoli AK, Formosa MF, Vizi D, et al. (2011) Reconstituted high-density lipoprotein infusion modulates fatty acid metabolism in patients with type 2 diabetes mellitus. J Lipid Res 52: 572–581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Murphy RC, James PF, McAnoy AM, Krank J, Duchoslav E, et al. (2007) Detection of the abundance of diacylglycerol and triacylglycerol molecular species in cells using neutral loss mass spectrometry. Anal Biochem 366: 59–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Tandy S, Chung RW, Kamili A, Wat E, Weir JM, et al. (2010) Hydrogenated phosphatidylcholine supplementation reduces hepatic lipid levels in mice fed a high-fat diet. Atherosclerosis 213: 142–147. [DOI] [PubMed] [Google Scholar]
- 17. Meyer C, Pimenta W, Woerle HJ, Van Haeften T, Szoke E, et al. (2006) Different mechanisms for impaired fasting glucose and impaired postprandial glucose tolerance in humans. Diabetes Care 29: 1909–1914. [DOI] [PubMed] [Google Scholar]
- 18. Riebeling C, Allegood JC, Wang E, Merrill AH Jr, Futerman AH (2003) Two mammalian longevity assurance gene (LAG1) family members, trh1 and trh4, regulate dihydroceramide synthesis using different fatty acyl-CoA donors. J Biol Chem 278: 43452–43459. [DOI] [PubMed] [Google Scholar]
- 19. Frangioudakis G, Garrard J, Raddatz K, Nadler JL, Mitchell TW, et al. (2010) Saturated- and n-6 polyunsaturated-fat diets each induce ceramide accumulation in mouse skeletal muscle: reversal and improvement of glucose tolerance by lipid metabolism inhibitors. Endocrinology 151: 4187–4196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Stiban J, Tidhar R, Futerman AH (2010) Ceramide synthases: roles in cell physiology and signaling. Adv Exp Med Biol 688: 60–71. [DOI] [PubMed] [Google Scholar]
- 21. Xu Z, Zhou J, McCoy DM, Mallampalli RK (2005) LASS5 is the predominant ceramide synthase isoform involved in de novo sphingolipid synthesis in lung epithelia. J Lipid Res 46: 1229–1238. [DOI] [PubMed] [Google Scholar]
- 22. Adiels M, Boren J, Caslake MJ, Stewart P, Soro A, et al. (2005) Overproduction of VLDL1 driven by hyperglycemia is a dominant feature of diabetic dyslipidemia. Arterioscler Thromb Vasc Biol 25: 1697–1703. [DOI] [PubMed] [Google Scholar]
- 23. Sciacca MF, Brender JR, Lee DK, Ramamoorthy A (2012) Phosphatidylethanolamine enhances amyloid fiber-dependent membrane fragmentation. Biochemistry 51: 7676–7684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Hodge AM, Simpson JA, Gibson RA, Sinclair AJ, Makrides M, et al. (2007) Plasma phospholipid fatty acid composition as a biomarker of habitual dietary fat intake in an ethnically diverse cohort. Nutr Metab Cardiovasc Dis 17: 415–426. [DOI] [PubMed] [Google Scholar]
- 25. Wolk A, Furuheim M, Vessby B (2001) Fatty acid composition of adipose tissue and serum lipids are valid biological markers of dairy fat intake in men. J Nutr 131: 828–833. [DOI] [PubMed] [Google Scholar]
- 26. Elwood PC, Pickering JE, Givens DI, Gallacher JE (2010) The consumption of milk and dairy foods and the incidence of vascular disease and diabetes: an overview of the evidence. Lipids 45: 925–939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Grantham NM, Magliano DJ, Hodge A, Jowett J, Meikle P, et al.. (2012) The association between dairy food intake and the incidence of diabetes in Australia: the Australian Diabetes Obesity and Lifestyle Study (AusDiab). Public Health Nutr: 1–7. [DOI] [PMC free article] [PubMed]
- 28. Villegas R, Gao YT, Dai Q, Yang G, Cai H, et al. (2009) Dietary calcium and magnesium intakes and the risk of type 2 diabetes: the Shanghai Women's Health Study. Am J Clin Nutr 89: 1059–1067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Kroger J, Zietemann V, Enzenbach C, Weikert C, Jansen EH, et al. (2011) Erythrocyte membrane phospholipid fatty acids, desaturase activity, and dietary fatty acids in relation to risk of type 2 diabetes in the European Prospective Investigation into Cancer and Nutrition (EPIC)-Potsdam Study. Am J Clin Nutr 93: 127–142. [DOI] [PubMed] [Google Scholar]
- 30. Patel PS, Sharp SJ, Jansen E, Luben RN, Khaw KT, et al. (2010) Fatty acids measured in plasma and erythrocyte-membrane phospholipids and derived by food-frequency questionnaire and the risk of new-onset type 2 diabetes: a pilot study in the European Prospective Investigation into Cancer and Nutrition (EPIC)-Norfolk cohort. Am J Clin Nutr 92: 1214–1222. [DOI] [PubMed] [Google Scholar]
- 31. Mozaffarian D, Cao H, King IB, Lemaitre RN, Song X, et al. (2010) Trans-palmitoleic acid, metabolic risk factors, and new-onset diabetes in U.S. adults: a cohort study. Ann Intern Med 153: 790–799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Ford DA (2010) Lipid oxidation by hypochlorous acid: chlorinated lipids in atherosclerosis and myocardial ischemia. Clin Lipidol 5: 835–852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Skaff O, Pattison DI, Davies MJ (2008) The vinyl ether linkages of plasmalogens are favored targets for myeloperoxidase-derived oxidants: a kinetic study. Biochemistry 47: 8237–8245. [DOI] [PubMed] [Google Scholar]
- 34. Lessig J, Fuchs B (2009) Plasmalogens in biological systems: their role in oxidative processes in biological membranes, their contribution to pathological processes and aging and plasmalogen analysis. Curr Med Chem 16: 2021–2041. [DOI] [PubMed] [Google Scholar]
- 35. Wallner S, Schmitz G (2011) Plasmalogens the neglected regulatory and scavenging lipid species. Chem Phys Lipids 164: 573–589. [DOI] [PubMed] [Google Scholar]
- 36. Nelson TL, Biggs ML, Kizer JR, Cushman M, Hokanson JE, et al. (2012) Lipoprotein-associated phospholipase A2 (Lp-PLA2) and future risk of type 2 diabetes: results from the Cardiovascular Health Study. J Clin Endocrinol Metab 97: 1695–1701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Serban M, Tanaseanu C, Kosaka T, Vidulescu C, Stoian I, et al. (2002) Significance of platelet-activating factor acetylhydrolase in patients with non-insulin-dependent (type 2) diabetes mellitus. J Cell Mol Med 6: 643–647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Sanchez-Quesada JL, Vinagre I, de Juan-Franco E, Sanchez-Hernandez J, Blanco-Vaca F, et al. (2012) Effect of improving glycemic control in patients with type 2 diabetes mellitus on low-density lipoprotein size, electronegative low-density lipoprotein and lipoprotein-associated phospholipase A2 distribution. Am J Cardiol 110: 67–71. [DOI] [PubMed] [Google Scholar]
- 39. Fan P, Liu H, Wang Y, Zhang F, Bai H (2012) Apolipoprotein E-containing HDL-associated platelet-activating factor acetylhydrolase activities and malondialdehyde concentrations in patients with PCOS. Reprod Biomed Online 24: 197–205. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Contains: Table S1. Conditions for precursor ion scan and MRM acquisition methods for lipid identification and analysis. Table S2. Lipid species associated with diabetes and prediabetes in the AusDiab and SAFHS cohorts. Table S3. Logistic regression of lipids against diabetes and prediabetes in the AusDiab cohort. Table S4. Logistic regression of lipid classes in the SAFHS cohort. Table S5. Logistic regression of lipids against diabetes and prediabetes in the SAFHS cohort. Table S6. Linear regression of lipid species in the AusDiab and SAFHS cohorts.
(DOCX)