Abstract
Background
The burden and significance of vancomycin-resistant enterococci (VRE) colonization in the ICU is not clearly understood.
Methods
We searched PubMed and EMBASE up to May 2013 for studies reporting the prevalence of VRE upon admission to the ICU and performed a meta-analysis to assess rates and trends of VRE colonization. We calculated the prevalence of VRE on admission and the acquisition (colonization and/or infection) rates to estimate time trends and the impact of colonization on ensuing VRE infections.
Findings
Across 37 studies (62,959 patients at risk), the estimated prevalence of VRE on admission to the ICU was 8.8% (7.1-10.6). Estimates were more consistent when cultures were obtained within 24 hours from admission. The VRE acquisition rate was 8.8% (95% CI 6.9-11.0) across 26 evaluable studies (35,364 patients at risk). Across US studies, VRE acquisition rate was 10.2% (95% CI 7.7-13.0) and demonstrated significant decline in annual trends. We used the US estimate of colonization on admission [12.3% (10.5-14.3)] to evaluate the impact of VRE colonization on admission in overall VRE prevalence. We demonstrated that VRE colonization on admission is a major determinant of the overall VRE burden in the ICU. Importantly, among colonized patients (including admitted and/or acquired cases) the VRE infection rates vary widely from 0-45% (with the risk of VRE bacteremia being reported from 0-16%) and <2% among those without a proven colonization.
Conclusion
In summary, up to 10.6% of patients admitted in the ICU are colonized with VRE on admission and a similar percentage will acquire VRE during their ICU stay. Importantly, colonization on admission is a major determinant of VRE dynamics in the ICU and the risk of VRE-related infections is close related to colonization.
Introduction
The emergence of drug-resistant bacteria in the ICU has been well documented [1-3]. Among these drug resistant pathogens, vancomycin-resistant enterococci (VRE) account for significant excess morbidity and costs [4-6]. Interestingly, VRE is uncommon (<1%) among otherwise healthy individuals [7,8], but it is present in most ICUs. Moreover, ICUs are major reservoirs of VRE that sustain VRE presence in the health care setting [9]. Although the impact of VRE infection in the ICU is significant, the association between VRE colonization and infection has not been established [10,11]. The rationale for conducting this study was to assess the magnitude and significance of VRE colonization at admission in the ICU, as well as its impact in VRE infections.
Materials and Methods
Study Selection
MEDLINE and EMBASE were searched for studies in English providing data in VRE rectal colonization upon admission in the ICU. Applied search terms were “VRE OR (vancomycin AND resistant AND enterococ*) AND (ICU OR (critically AND ill) OR (intensive AND care))”. Last access was on May 17, 2013. Relevance to the topic was initially assessed by title and abstract reading. Pertinent articles were accessed in full text to determine eligibility and extract data. The reference lists of eligible studies were screened for additional articles. The PRISMA guidelines were followed (Appendix S1) [12].
Studies that had extractable data on VRE rectal colonization upon admission in the ICU were included in the meta-analysis. Neonatal and pediatric ICUs were excluded from analysis. Abstracts, conference proceedings, and unpublished material were not considered.
Outcomes of interest
We defined three outcomes of interest: (a). The prevalence of VRE colonization upon admission. (b) Acquisition rates, calculated as the proportion of VRE negative patients at ICU admission that acquire VRE colonization/infection during ICU stay. If the denominator was not provided, it was approximated by subtracting the number of patients colonized with VRE at admission from the total number of patients at risk. (c) The association of admission VRE colonization with ensuing VRE associated infections in the ICU [13,14].
Data Extraction
Two authors (PZ, RT) independently retrieved and extracted data and consensus was reached in cases of discrepancies. For each study apart from prevalence, we extracted the period of recruitment, country of origin, time lapsed from admission to screening and ICU type, and predominant VRE resistance phenotype.
We extrapolated stratified data by ICU type, calendar year and intervention. If stratified data were not reported, we used the aggregated data. We crudely adjusted for any time-trends by using the mid-year of study recruitment as index year of the study. Date of study publication was not used, because it is not consistent to the time that the study was actually conducted.
Quality assessment
Studies were given quality points based on items regarding optimal research design and quality of reporting as previously described for schizophrenia [15]. The modified chart with assigned scores is provided with the appendix S2. Studies with quality scores above the 75th percentile were considered of higher quality.
Data Analysis
We performed a meta-analysis of random-effects (RE) to estimate the pooled (combined) prevalence and 95% confidence intervals, using the Freeman-Tukey arcsine methodology to address stabilizing variances [16]. Der-Simonian & Laird weights were applied [17]. We used the between-study variance τ2 to measure statistical heterogeneity [17,18]. Small study effects were addressed with Egger’s test for publication bias [19]. The “trim & fill” method was used to adjust effects for theoretically missing studies [20]. We incorporated a subgroup and meta-regression technique to adjust for potential sources of heterogeneity. For time trends, model coefficients were transformed to rates and fitted values were plotted against the index year along with observed prevalence rates.
VRE prevalence estimates from U.S.A. studies were used to simulate an approximation of VRE endemic burden in the ICU. Assuming that colonized VRE patients remain colonized throughout their length of stay [21,22] and represent the major source of VRE transmission in the ICU, then the predicted endemic prevalence of VRE yp is derived by solving the following equation: R(p,q)= [yp (1+δφ)-(δ+1)φ]/[yp(1-yp)] [23]. For any given δ, φ, R(p,q), the solution is a quadratic equation with two solutions (one negative and one positive yp) when the discriminant (D) is D>0. Only the positive solution applies to our simulation. R(p,q) represents the effective reproductive number for an ICU, δ the proportional increase in length of stay for colonized patients and the φ admission prevalence. The effective reproductive number is a core parameter in infectious disease dynamics within an ICU and it measures the performance of infection control measures. If it is lower than unit, that is R(p,q)<1, transmission alone is unable to sustain VRE endemic in the ICU. That implies that even in ICUs with very low effective reproductive number, i.e R(p,q)<<1, which suggests highly effective preventive measures, introduction of VRE colonized patients will remain the main factor to sustain VRE transmission, and φ will be the lower boundary of endemic prevalence [23]. VRE colonization dynamics were simulated for R=0.9 to approximate the outmost boundary to control VRE endemic in ICU and R=0.5 a modest scenario for an effective restriction policy in the ICU.
The Stata version 11 software package (Stata Corporation, College Station, TX) and StatsDirect version 2.7.9 (StatsDirect Ltd, UK) were used for data analysis.
Results
Initial search yielded a total of 1,659 potentially relevant publications. A total of 1,569 were excluded on title and abstract reading, leaving 90 studies for full-text evaluation. Thirty-eight studies were deemed appropriate for analysis, of which one was linked to another due to overlapping data [24,25]. Manual search of references lists did not add any additional publications, leaving 37 studies eligible for final analysis (coded from 38 published manuscripts that included 62,959 patients at risk) (Appendix S3-Flow diagram). The summary of studies included in our analysis is presented in Table 1 [10,11,24-59]. VRE colonization rates on admission varied widely from 0.1-42.6% (median 8.7%), and the population at risk from 47 to 8203 patients (median 662 patients). The majority of studies (21/37, 57%) originated in the US, followed in descending order by studies originating in Asia (6/37, 16%), Europe (4/37, 11%), Oceania (3/37, 8%) and S. America (3/37, 8%). Time to VRE screening was up to 24h in 17 studies, up to 48h in 14 studies, and up to 72h or longer in 5 studies. In two studies surveillance screening was performed within the first week of admission (Table 1). Cultures were used for surveillance screening, with the exception of a single study [37] where PCR was used.
Table 1. Summary of included studies.
| ID | Author | Year | Origin | Mid-year | ICU type | tScreen/site (detection) | VRE (%) Ad. (N) | VRE(%) Acq, (n) | Resistance phenotype | Quality Score |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Climo MW [26] | 2013 | USA | 2008 | 6 ICUs | 48h/R (NA) | NA | B | ||
| #1 | (Intervention)† | 16.3(3970) | 2.4 (3323) | NA | ||||||
| #2 | (Control) | 15.1(3842) | 3.3 (3262) | NA | ||||||
| 2 | Batis tao DW [27] | 2012 | Brasil | 2009 | ICU | 48h/R(C) | 15.0(333) | 9.9 (283) | VanC (99%) | A |
| 3 | Grabsch EA [28] | 2012 | Australia | Ad/R,F(C) | VanB(>95%) | A | ||||
| #1 | 2009 | ICU | 6.0(662) | |||||||
| #2 | 2010 | Liver | 4.7(1430) | |||||||
| #3 | 2009 | ICU | 9.1(515) | |||||||
| #4 | 2010 | Liver | 8.7(1196) | |||||||
| 4 | Kim YJ [29] | 2012 | Korea | 2010 | MICU | 48h/R(C) | 17.6(1048) | 12.3 (864) | VanA(100%) | B |
| 5 | Pan SC [30] | 2012 | Taiwan | 2008 | SICU | 24h/R(C) | 5.9(871) | 5.7 (820) | NA | B |
| 6 | Yoon YK [31] | 2012 | Korea | 2010 | MICU,SICU | Ad/R(C) | 3.4(4445) | NA | B | |
| 7 | Huang SS [32] | 2011 | USA | 2004 | 8 ICUs | Ad/R(NA) | 8.0(8203) | 2.9 (7806) | NA | B |
| 8 | Huskins WC [33] | 2011 | USA | 2006 | 48h/R(C) | NA | B | |||
| #1 | (Intervention)†† | 10 ICUs | 16.9(2286) | 14.8(2132) | ||||||
| #2 | (Control) | 8 ICUs | 22.1(1503) | 12.9(1356) | ||||||
| 9 | Minhas P [34] | 2011 | USA | 2008 | NICU | 48h/ R(C) | 2.5(766) | NA | A | |
| 10 | Climo MW [35] | 2009 | USA | 2005 | 6 ICUs | 48h/R(C) | NA | B | ||
| #1 | Soap bathing | 9.0 (2670) | 2.5(2429) | |||||||
| #2 | Chlorhexidine bathing | 8.6 (2650) | 1.2(2422) | |||||||
| 11 | Song JY [36] | 2009 | Korea | 2007 | ICU | 48h/R(C) | 4.4(780) | VanA(100%) | A | |
| 12 | Wibbenmeyer L[37] | 2009 | USA | 2007 | Burn | 48h/R (PCR) | 10.5(484) | 12.1 (423) | NA | A |
| 13 | Drees M [38] | 2008 | USA | 2002 | MICU,SICU | 48h/R (C) | 8.9(1330) | 4.1 (1212) | NA | B |
| 14 | Lambiase A [39] | 2007 | Italy | 2004 | ICU | Ad/F,U,Res (C) | 3.7(700) | VanA (77%) | B | |
| 18 | Littvik AM [40] | 2006 | Argentina | 2003 | ICU | Ad/R (C) | 8.2(147) | 4.4(135) | VanA (93%) | A |
| 15 | Peta M [41] | 2006 | Italy | 2003 | ICU | 24h/R (C) | 2.6(509) | 9.5 (453) | VanA (100%) | B |
| 16 | Shadel BN [10] | 2006 | USA | 1998 | MICU | Ad/RF (NA) | 9.7(1872) | 9.8 (1690) | NA | B |
| 17 | Vernon MO [42] | 2006 | USA | 2003 | MICU | <72h/ R(C) | NA | A | ||
| Soap and water bath | 18.0(362) | 20.2(77) | ||||||||
| Chlorhexidine bath | 16.0(462) | 7.8(77) | ||||||||
| Non-medicated cloth | 19.0(364) | 11.5(69) | ||||||||
| 19 | Furuno JP [43] | 2005 | USA | 2003 | MICU,SICU | 48h/R (C) | 10.1(2440) | NA | B | |
| 20 | Harris AD [44] | 2004 | USA | 2002 | MICU,SICU | 72h/R (C) | 10.0(1362) | NA | B | |
| 21 | Winston LG [45] | 2004 | USA | 2003 | ICUs | Twice Wk/R(C) | NA | B | ||
| (Post-switch) ‡ | 7.4(537) | 7.6 (497) | ||||||||
| (Pre-switch) | 8.3(399) | 11.5 (366) | ||||||||
| 22 | Yeh KM [46] | 2004 | Taiwan | 2000 | ICUs | Ad/R,F (C) | 8.0(4538) | VanA>>VanB | B | |
| 23 | De Jonge E [47] | 2003 | Holland | 2000 | ICU | 48h/R,Res (C) | NA | B | ||
| #1 | (Intervention)‡‡ | 1.4(432) | 1.1 (378) | |||||||
| #2 | (Control) | 0.9(436) | 1.3 (395) | |||||||
| 24 | Ho PL [48] | 2003 | Hong- Kong | 1999 | ICUs | Ad/R (C) | 0.1(1663) | VanA (one case) | A | |
| 25 | Martinez JA [49] | 2003 | USA | 1997 | MICU | 48h/R (C) | 18.9(169) | 22.6 (137) | NA | B |
| 26 | Padiglione AA [11] | 2003 | Australia | 1999 | 11 ICUs | 48h/R (C) | 0.6(3086) | 1.2 (1992) | VanB (92%) | B |
| 27 | Warren DK [50] | 2003 | USA | 2000 | MICU | Ad/R (C) | 24.5(519) | 21.0 (352) | NA | A |
| 28 | Gardiner D [51] | 2002 | USA | 1999 | MICU | 24h/R,U,F (C) | 42.6(47) | 22.2 (27) | NA | A |
| 29 | Puzniak LA [52] | 2002 | USA | 1998 | MICU | Ad/R,F (C) | 7.0(2631) | 7.8 (1684) | NA | B |
| 30 | Hendrix CW [53] | 2001 | USA | 1996 | MICU,SICU | Ad/R,U, Res (C) | 9.4(117) | 11.3 (106) | NA | B |
| 31 | Marin ME [54] | 2001 | Argentina | 2000 | ICU | Ad/R (C) | 0.7(136) | NA | A | |
| 32 | Dan M [55] | 1999 | Israel | 1996 | ICU | End of wk/R (C) | 9.8(61) | 14.5 (55) | VanA(100%) | A |
| 33 | Grayson ML [56] | 1999 | Australia | 1997 | ICU | 72h/R,F (C) | 0.7(134) | VanB (one case) | A | |
| 34 | Ostrowsky BE [57] | 1999 | USA | 1995 | SICU | 24h/R(C) | 12.1(290) | 14.1 (78) | VanA(85%) | B |
| 35 | Zuckerman RA [58] | 1999 | USA | 1995 | SICU | 24h/R (C) | 6.3(80) | 9.8 (51) | NA | A |
| 36 | Bonten MJ [24,25] | 1998 | USA | 1995 | MICU | 48h/R, Res,G (C) | 14.3(301) | 21.3 (258) | VanA(60%) | A |
| 37 | Slaughter S [59] | 1996 | USA | 1995 | MICU | 72h/R (C) | 15.5(181) | 29.4 (153) | VanA(76%) | A |
Data stratified by year, ICU type and intervention (where available). N,n=evaluable samples, tScreen= time within screening cultures were obtained, Ad= when admitted ,C=culture based, G=groins, F=fecal, R=rectal, Res=respiratory, U=urine, NA=not available, Quality score [A (>9), B≤9]. † Chlorhexidine bathing, †† VRA/MRSA surveillance and expanded barrier precautions, ‡ from ticarcillin-clavulanate to piperacillin-tazobactam, ‡‡ selective digestive tract decontamination
VRE colonization at ICU admission
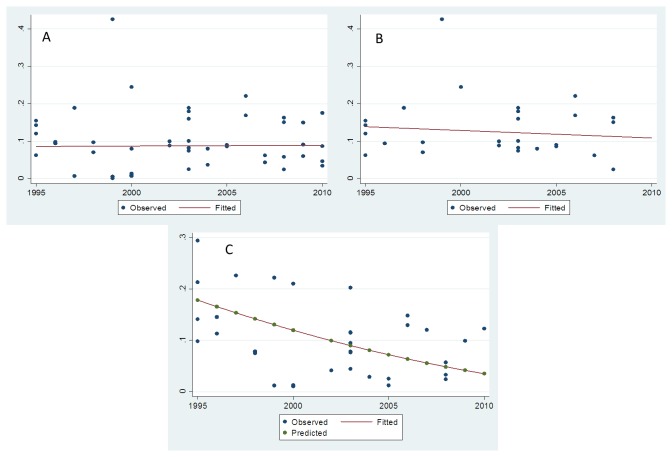
The pooled prevalence estimates are presented in Table 2 and as a forest plot (Figure 1). The estimated prevalence of VRE colonization at ICU admission was 8.8% (95% CI 7.1-10.6). The Egger’s test was insignificant, suggesting absence of small study effects. After excluding studies with observed prevalence rates higher than the 90th percentile (>19%) as potential outliers, the estimated VRE prevalence was 7.9% (95% CI 6.3-9.6). The estimated prevalence across US studies was 12.3% (95% CI 10.5-14.3) and consistent between studies (low between-study variance τ2=0.022). US prevalence estimates were higher compared to pooled estimates from European (2.7%, 95% CI 1.3-4.5), Asian (5.3%, 95% CI 2.0-10.2) and Australian (4.4%, 95% 1.5-8.8) studies.
Table 2. Summary of Effects.
| Studies (arms) | at risk (N) | Combined Effect (95% CI) | τ2 | |
|---|---|---|---|---|
| VRE colonization | ||||
| All studies | 37 (47) | 62,959 | 8.8% (7.1-10.6) | 0.045 |
| Excluding outliers (>19%) | 35 (44) | 60,890 | 7.9% (6.3-9.6). | 0.040 |
| USA | 21 (27) | 39,837 | 12.3% (10.5-14.3) | 0.022 |
| Europe | 4 (5) | 2,138 | 2.7% (1.3-4.5) | 0.009 |
| Asia | 6 (6) | 13,345 | 5.3% (2.0-10.2) | 0.051 |
| Australia | 3 (6) | 7,023 | 4.4% (1.5-8.8) | 0.049 |
| South America | 3 (3) | 616 | 7.0 (0.9-18.1) | 0.086 |
| Screened up to 24h | 17 (20) | 30,571 | 7.3% (5.4-9.4) | 0.027 |
| Screened up to 48h | 14 (18) | 28,526 | 9.2% (6.2-12.8) | 0.060 |
| Screened up to 72h | 5 (7) | 2,926 | 12.2% (8.0-17.2) | 0.031 |
| VRE acquisition | ||||
| All studies | 26 (33) | 35,364 | 8.8% (6.9-11.0) | 0.041 |
| Studies >1000 at risk | 8 (11) | 29,308 | 4.8% (2.8-7.2) | 0.030 |
| Excluding outliers (>21%) | 21 (28) | 34,437 | 7.0%, (5.3-8.9) | 0.033 |
| USA | 18 (24) | 29,989 | 10.2% (7.7-13.0) | 0.042 |
VRE colonization combined (pooled) estimates.
Figure 1. Forrest plot of studies included in the meta-analysis of VRE prevalence at ICU admission [individual study data (squares) and combined estimates (diamond)].
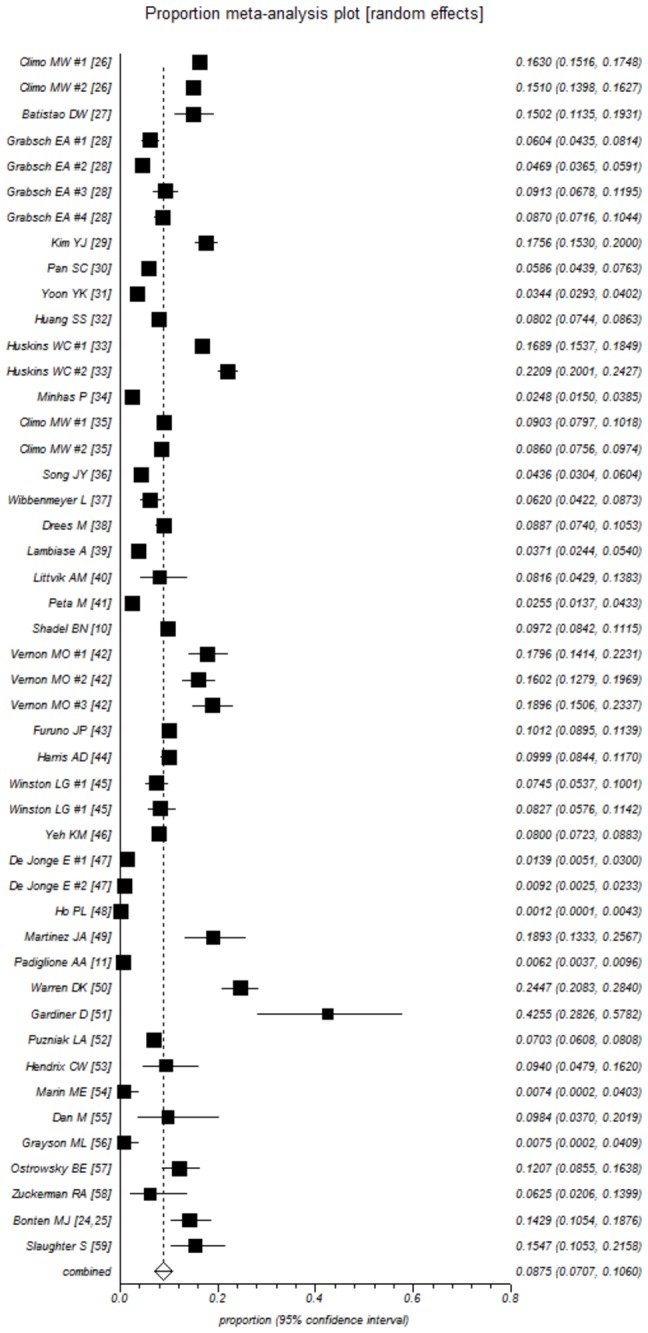
Interestingly, time to screening after ICU admission resulted in different VRE prevalence estimates, but these differences did not reach statistical significance. More specifically, rectal surveillance up to 24h after ICU admission yielded an estimated prevalence of 7.3% (95% CI 5.4-9.4). The corresponding estimates for screening up to 48h or ≥72h were 9.2 (95% CI 6.2-12.8) and 12.2 (95% CI 8.0-17.2), respectively. Effects were more consistent (between-study variance τ2 =0.027) when screening was performed within 24h of admission. The median quality score was 9 (range 6-10). Studies with higher quality scores (>9) did not differ in the prevalence of VRE (9.3%; 95% 6.0-13.2) from those with lower (≤9) quality scores (8.4%; 95% CI 6.4-10.7). A metaregression analysis was applied to address the effect of time (time trends by mid-year of study recruitment period) on VRE prevalence. No significant effect was noted for all (Figure 2A) or for US studies (Figure 2B), suggesting that on average, VRE admission prevalence has remained stable over 1995 to 2010.
Figure 2. VRE colonization in the ICU.
A. Observed (dots) and fitted (line) VRE prevalence estimates (all studies), by study mid-year. B. Observed (dots) and fitted (line) VRE prevalence estimates (U.S.A. studies), by study mid-year. C. Observed (blue dots), predicted (green dots) VRE acquisition estimates and quadratic fit (line) across U.S.A. studies. Data plotted by study mid-year.
VRE acquisition during ICU stay
VRE acquisition rates could be extracted in 26 studies with pertinent data. The observed rates varied widely from 1.1% to 29.4% (Table 1; combined effects are presented in Table 2). The estimated VRE acquisition rate was 8.8% (95% CI 6.9-11.0) and estimates did not vary after excluding potential outliers such as studies with observed acquisition rates higher than the 90th percentile, that is >21% (7.0%, 95% CI 5.3-8.9). The Egger’s test was significant, suggesting small study effects (bias 5.8, p=0.002). After excluding studies with <1,000 population at risk, the combined estimate was 4.8% (95% CI 2.8-7.2). As estimates were influenced by smaller studies, a trim-and-fill methodology was used for adjustment, and the estimated risk was 6.7% (95% CI 5.1-8.6).
The estimated acquisition risk across the US studies was 10.2% (95% CI 7.7-13.0). A metaregression analysis was applied to address the effect of time (time trends by index-year) on VRE acquisition across all evaluable studies and US studies only. A decline of marginal significance was noted across all studies (p=0.05). However the decline across US studies was highly significant (p=0.004) and suggested a decline in year-trends for VRE acquisition (Figure 2C).
VRE colonization and VRE infection during ICU stay
Individual study data could not be pooled because they refer either to prevalent cases at admission or acquired cases or the total number of colonized patients. A descriptive analysis is presented in Table 3. Sixteen studies provided data on VRE infections relative to colonization status. The reported risk of any VRE infection among VRE colonized (prevalent and acquired) ranged from zero [11,27] to a peak of 45% [53]. The reported risk of VRE bacteremia ranged from 0% to 16%. The risk of any VRE infection among non-colonized patients was negligible <2%.
Table 3. Descriptive summary of VRE infections by colonization status.
| Author | VRE infections |
|---|---|
| Batis tao DW,2012 [27] | No VRE infections among prevalent at admission |
| Pan SC,2012 [30] | 5/47 (11%) had VRE infection among acquired cases |
| Kim YJ, 2012 [29] | 28/184 (15%) had VRE infections among those prevalent at admission |
| Climo MW, 2009 [35] | 16/270 (6%) among colonized in soap bathing group had bacteremia (cumulative) |
| 4/226 (2%) among colonized in chlorhexidine group had bacteremia (cumulative) | |
| Wibbenmeyer L,2009 [37] | 7/30 (23%) VRE infections among prevalent at admission vs. 0/463 among VRE negative on admission |
| 0/51 infections among those acquiring VRE | |
| Lambiase E, 2007 [39] | No VRE bacteremia among prevalent at admission |
| Peta M, 2006 [41] | 2/56 (4%) VRE infections among colonized (cumulative) |
| Shadel BN, 2006 [10] | 8% VRE bacteremia among prevalent at admission vs. <1% among non-colonized |
| Yeh KM, 2004 [46] | 9/816 (1%) had bacteremia among colonized (cumulative) |
| Littvik AM, 2004 [40] | 2/18 (11%) VRE bacteremias among colonized (cumulative) |
| Martinez JA, 2003 [49] | 1/32 (3%) with VRE bacteremia among prevalent at admission |
| 1/31 (3%) with VRE bacteremia after VRE acquisition | |
| None among those without VRE colonization | |
| Padiglione AA, 2003 [11] | No VRE infections among colonized (cumulative) |
| Hendrix CW, 2001 [53] | 9/20 (45%) VRE infections among colonized (cumulative) |
| 0/94 among non-colonized | |
| Dan M, 1999 [55] | 1/6 (16%) with VRE bacteremia among prevalent at admission |
| 1/55 (2%) with VRE bacteremia among not colonized | |
| Ostrowsky BE, 1999 [57] | 1/35 (3%) with VRE infection among prevalent at admission |
| Zuckerman RA, 1999 [58] | No VRE infections among prevalent at admission |
VRE resistance phenotypes
Resistance phenotypes were underreported. Only 15 studies had relevant information to be extracted. Eleven studies reported VanA as the dominant resistance phenotype, while three (all from Australia with a low VRE prevalence) reported a VanB phenotype (Table 1). There was a single study [27] that reported VanC phenotype. The relative lack of information precludes adjusting for the effect of resistance phenotypes.
VRE admission colonization and VRE prevalence
We also performed a simulation to demonstrate to evaluate how the VRE colonization on admission could affect the overall prevalence of VRE in the ICU. VRE prevalence in the ICU was simulated assuming that preventive measures are of borderline efficacy (that is the effective reproductive number will be just below unit, R=0.9; Figure 3A) or modest efficacy (that is R=0.5; Figure 3B). We used the US estimates for admission colonization (10-15%), a realistic scenario based on our data. Of note is that patients colonized with VRE have a longer ICU stay, compared to non-colonized patients, which increases the risk of transmission [10,36,41,52]. The relative increase of stay is measured by parameter δ in our model, and we adopted a wide range from 0 to 1.0, with 0 representing same length of ICU stay for colonized and non-colonized and 1.0 representing twice the length of stay compared to non-colonized. As shown on Figure 3A and 3B, the predicted estimates suggest not only that admission prevalence defines the lower boundary of VRE colonization, but also that introduction of new cases acts as an amplifier of VRE colonization. In practice, it means that VRE prevalence in an ICU is never expected to be lower than the admission VRE colonization rates and any increase of VRE cases colonized on admission, will add to VRE prevalence in the specific ICU. Therefore, VRE admission rates should be kept low to control VRE endemic potential in the ICU.
Figure 3. Simulation of VRE endemic prevalence using US admission prevalence estimates to graphically demonstrate the amplifying effect of VRE admission prevalence.
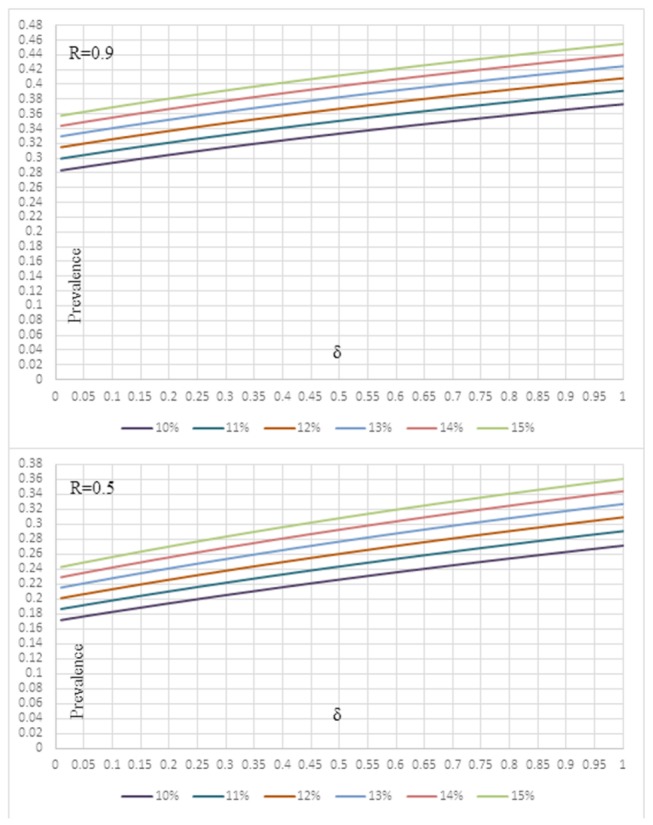
A. for an effective reproductive number R(p,q)=0.9 B. for an effective reproductive number R(p,q)=0.5.
Discussion
We performed a meta-analysis of prevalence rates for VRE colonization at ICU admission and evaluated the significance of VRE colonization on admission to the ICU. Overall, 7.1-10.6% of patients admitted to the ICU are colonized with VRE on admission. Excluding studies with observed rates beyond the 90th percentile as outliers, resulted in a more conservative expectation of VRE colonization at ICU admission (6.3-9.6%). A similar percent (6.9-11.0%) will acquire VRE during their ICU stay (adjusted estimate 5.1-8.6%, after accounting for missing studies). We also found that VRE screening within the first 24 hours of submission gives the most consistent estimate of VRE colonization, compared to studies screening patients within 48h or 72h after ICU admission. The VRE infection rates ranged from 0-45% among colonized patients, while the risk of VRE infection among non-colonized was consistently <2%. Interestingly, as seen in the simulation examples, we demonstrated how VRE colonization on admission to the ICU will determine, in a large degree, the VRE prevalence in the ICU.
The estimate of VRE colonization on admission to the ICU was higher across US studies (12.3%), compared to studies from Europe (2.7%), S. America (7.0%), Asia (5.3%) and Oceania (4.4%). Geographic variations are not unusual for drug-resistant bacteria, as different antibiotic consumption policies and compliance with isolation practices, infection control and antibiotic stewardship programs and cultural differences that affect behavior among the health care personnel, account for this differences [60,61]. Moreover, studies in molecular epidemiology have shown that the worldwide emergence of VRE is related to a specific Enterococcus faecium subpopulation CC17. This clade emerged in the U.S., and is likely a major reason why the results in the US are different than elsewhere [62]. Indeed, previous surveillance data have shown that Europe had a lower incidence of VRE [9,63,64]. Interestingly, surveillance data from Europe indicate that the VRE rate might be rising [63,65,66], but ICU data are limited. In analysis, the rate of VRE at admission in the ICU appears to be stable and, since the data from outside the US are sparse, trends and differences between continents should be interpreted with caution. Here it should be noted that as a meta-analysis this study is limited by the quality of included studies, while the exclusion of non-English literature might also expose this analysis to additional bias.
Although as noted above our data showed that the VRE colonization on admission to the ICU has remained stable, the acquisition rates in the US have declined significantly from 1995 to 2010. A plausible explanation is that colonization on admission mostly depends upon factors that can be marginally modified. Such factors include advanced age, prolonged hospitalization, debilitating illness, prior exposure to antibiotics or transfer from other institutions [67]. However, VRE transmission can be prevented by restriction measures and the expanding knowledge in recognition and prevention of VRE infections in the ICU may have contributed for the longitudinal decline in acquisition rates [2]. This analysis indicates that strict control efforts throughout the healthcare system can reduce admission prevalence and contribute significantly to the control of VRE burden within the ICU. It should be emphasized that screening and surveillance for VRE constitute only a part of infection control programs with policies varying across countries and institutions, and their relative impact in overall control cannot be objectively estimated.
Interestingly, we found considerable diversity in the impact of VRE colonization on ensuing VRE-related infections among studies. Overall, our findings indicate that the risk of VRE infection, is not negligible and closely associated to colonization. More specifically, the risk of VRE infection in the ICU among colonized patients varied from 0-45%, while the risk of VRE infection among non-colonized cases was <2%. Of note is that the range of infection among colonized patients varies widely and depends on host factors and population heterogeneity and differences in VRE epidemiology account for these differences. For example, the risk of VRE infection is relatively low in the general hospital setting and in a US study it was 4% [68], but it is higher for high risk populations, such as solid organ transplant recipients (11.3%) [69], cancer patients (29.3%) [70] and allogeneic hematopoietic stem cell transplant recipients (34.2%) [71]. In addition to host factors, the type and virulence of the VRE strain might also influence the risk of VRE infection. For example, studies that focused on the colonization by the vanC genotype of E. faecium reported no VRE infections [27] or <1% incidence of VRE bacteremia (9-year study among bone marrow transplant recipients) [72].
In conclusion, VRE prevalence on admission to the ICU varied based on geographic location and local epidemiology, but there is no evidence of significant variation over the years. and the observed decline in acquisition rates in the ICU is encouraging. However, the risk of VRE infections it is almost exclusively confined to VRE colonized patients and admission prevalence is the major determinant of VRE dynamics in the ICU. Adequate control of VRE in the ICU can only be achieved by reducing VRE colonization throughout the health system.
Supporting Information
PRISMA Checklist S1.
(DOC)
Study quality data (assigned scores).
(XLSX)
Flow diagram of meta-analysis.
(DOCX)
Acknowledgments
The authors want to thank Eleni A. Ziaka, MSc for providing assistance regarding the mathematical properties of the VRE model.
Funding Statement
The authors have no support or funding to report.
References
- 1. Sandiumenge A, Rello J (2012) Ventilator-associated pneumonia caused by ESKAPE organisms: cause, clinical features, and management. Curr Opin Pulm Med 18: 187-193. doi:10.1097/MCP.0b013e328351f974. PubMed: 22366995. [DOI] [PubMed] [Google Scholar]
- 2. Doyle JS, Buising KL, Thursky KA, Worth LJ, Richards MJ (2011) Epidemiology of infections acquired in intensive care units. Semin Respir Crit Care Med 32: 115-138. doi:10.1055/s-0031-1275525. PubMed: 21506049. [DOI] [PubMed] [Google Scholar]
- 3. Freire-Moran L, Aronsson B, Manz C, Gyssens IC, So AD et al. (2011) Critical shortage of new antibiotics in development against multidrug-resistant bacteria-Time to react is now. Drug Resist Update 14: 118-124. doi:10.1016/j.drup.2011.02.003. PubMed: 21435939. [DOI] [PubMed] [Google Scholar]
- 4. de Kraker ME, Jarlier V, Monen JC, Heuer OE, van de Sande N et al. (2012) The changing epidemiology of bacteraemias in Europe: trends from the European Antimicrobial Resistance Surveillance System. Clin Microbiol Infect. [DOI] [PubMed] [Google Scholar]
- 5. Ramsey AM, Zilberberg MD (2009) Secular trends of hospitalization with vancomycin-resistant enterococcus infection in the United States, 2000-2006. Infect Control Hosp Epidemiol 30: 184-186. doi:10.1086/593956. PubMed: 19125679. [DOI] [PubMed] [Google Scholar]
- 6. Salgado CD (2008) The risk of developing a vancomycin-resistant Enterococcus bloodstream infection for colonized patients. Am J Infect Control 36: S175: e175-e178. [DOI] [PubMed] [Google Scholar]
- 7. Padiglione AA, Grabsch EA, Olden D, Hellard M, Sinclair MI et al. (2000) Fecal colonization with vancomycin-resistant enterococci in Australia. Emerg Infect Dis 6: 534-536. doi:10.3201/eid0605.000514. PubMed: 11202974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Song JY, Hwang IS, Eom JS, Cheong HJ, Bae WK et al. (2005) Prevalence and molecular epidemiology of vancomycin-resistant enterococci (VRE) strains isolated from animals and humans in Korea. Korean J Intern Med 20: 55-62. doi:10.3904/kjim.2005.20.1.55. PubMed: 15906954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Lin MY, Hayden MK (2010) Methicillin-resistant Staphylococcus aureus and vancomycin-resistant enterococcus: recognition and prevention in intensive care units. Crit Care Med 38: S335-S344. doi:10.1097/CCM.0b013e3181b4a334. PubMed: 20647791. [DOI] [PubMed] [Google Scholar]
- 10. Shadel BN, Puzniak LA, Gillespie KN, Lawrence SJ, Kollef M et al. (2006) Surveillance for vancomycin-resistant enterococci: type, rates, costs, and implications. Infect Control Hosp Epidemiol 27: 1068-1075. doi:10.1086/507960. PubMed: 17006814. [DOI] [PubMed] [Google Scholar]
- 11. Padiglione AA, Wolfe R, Grabsch EA, Olden D, Pearson S et al. (2003) Risk factors for new detection of vancomycin-resistant enterococci in acute-care hospitals that employ strict infection control procedures. Antimicrob Agents Chemother 47: 2492-2498. doi:10.1128/AAC.47.8.2492-2498.2003. PubMed: 12878510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Moher D, Liberati A, Tetzlaff J, Altman DG, Group P (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ 339: b2535 doi:10.1136/bmj.b2535. PubMed: 19622551. [Google Scholar]
- 13. Garner JS, Jarvis WR, Emori TG, Horan TC, Hughes JM (1988) CDC definitions for nosocomial infections, 1988. Am J Infect Control 16: 128-140. doi:10.1016/0196-6553(88)90053-3. PubMed: 2841893. [DOI] [PubMed] [Google Scholar]
- 14. Horan TC, Andrus M, Dudeck MA (2008) CDC/NHSN surveillance definition of health care-associated infection and criteria for specific types of infections in the acute care setting. Am J Infect Control 36: 309-332. doi:10.1016/j.ajic.2008.03.002. PubMed: 18538699. [DOI] [PubMed] [Google Scholar]
- 15. Saha S, Chant D, Welham J, McGrath J (2005) A systematic review of the prevalence of schizophrenia. PLOS Med 2: e141. doi:10.1371/journal.pmed.0020141. PubMed: 15916472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Fazel S, Khosla V, Doll H, Geddes J (2008) The prevalence of mental disorders among the homeless in western countries: systematic review and meta-regression analysis. PLOS Med 5: e225. doi:10.1371/journal.pmed.0050225. PubMed: 19053169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. DerSimonian R, Laird N (1986) Meta-analysis in clinical trials. Control Clin Trials 7: 177-188. doi:10.1016/0197-2456(86)90046-2. PubMed: 3802833. [DOI] [PubMed] [Google Scholar]
- 18. Rücker G, Schwarzer G, Carpenter JR, Schumacher M (2008) Undue reliance on I(2) in assessing heterogeneity may mislead. BMC Med Res Methodol 8: 79. doi:10.1186/1471-2288-8-79. PubMed: 19036172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Egger M, Davey Smith G, Schneider M, Minder C (1997) Bias in meta-analysis detected by a simple, graphical test. BMJ 315: 629-634. doi:10.1136/bmj.315.7109.629. PubMed: 9310563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Duval S, Tweedie R (2000) Trim and fill: A simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics 56: 455-463. doi:10.1111/j.0006-341X.2000.00455.x. PubMed: 10877304. [DOI] [PubMed] [Google Scholar]
- 21. Baden LR, Thiemke W, Skolnik A, Chambers R, Strymish J et al. (2001) Prolonged colonization with vancomycin-resistant Enterococcus faecium in long-term care patients and the significance of "clearance". Clin Infect Dis 33: 1654-1660. doi:10.1086/323762. PubMed: 11595985. [DOI] [PubMed] [Google Scholar]
- 22. Mascini EM, Jalink KP, Kamp-Hopmans TE, Blok HE, Verhoef J et al. (2003) Acquisition and duration of vancomycin-resistant enterococcal carriage in relation to strain type. J Clin Microbiol 41: 5377-5383. doi:10.1128/JCM.41.12.5377-5383.2003. PubMed: 14662914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Austin DJ, Bonten MJ, Weinstein RA, Slaughter S, Anderson RM (1999) Vancomycin-resistant enterococci in intensive-care hospital settings: transmission dynamics, persistence, and the impact of infection control programs. Proc Natl Acad Sci U S A 96: 6908-6913. doi:10.1073/pnas.96.12.6908. PubMed: 10359812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Bonten MJ, Hayden MK, Nathan C, van Voorhis J, Matushek M et al. (1996) Epidemiology of colonisation of patients and environment with vancomycin-resistant enterococci. Lancet 348: 1615-1619. doi:10.1016/S0140-6736(96)02331-8. PubMed: 8961991. [DOI] [PubMed] [Google Scholar]
- 25. Bonten MJ, Slaughter S, Hayden MK, Nathan C, van Voorhis J et al. (1998) External sources of vancomycin-resistant enterococci for intensive care units. Crit Care Med 26: 2001-2004. doi:10.1097/00003246-199812000-00029. PubMed: 9875911. [DOI] [PubMed] [Google Scholar]
- 26. Climo MW, Yokoe DS, Warren DK, Perl TM, Bolon M et al. (2013) Effect of daily chlorhexidine bathing on hospital-acquired infection. N Engl J Med 368: 533-542. doi:10.1056/NEJMoa1113849. PubMed: 23388005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Batistão DW, Gontijo-Filho PP, Conceição N, Oliveira AG, Ribas RM (2012) Risk factors for vancomycin-resistant enterococci colonisation in critically ill patients. Mem Inst Oswaldo Cruz 107: 57-63. doi:10.1590/S0074-02762012000100008. PubMed: 22310536. [DOI] [PubMed] [Google Scholar]
- 28. Grabsch EA, Mahony AA, Cameron DR, Martin RD, Heland M et al. (2012) Significant reduction in vancomycin-resistant enterococcus colonization and bacteraemia after introduction of a bleach-based cleaning-disinfection programme. J Hosp Infect 82: 234-242. doi:10.1016/j.jhin.2012.08.010. PubMed: 23103245. [DOI] [PubMed] [Google Scholar]
- 29. Kim YJ, Kim SI, Kim YR, Lee JY, Park YJ et al. (2012) Risk factors for vancomycin-resistant enterococci infection and mortality in colonized patients on intensive care unit admission. Am J Infect Control 40: 1018-1019. doi:10.1016/j.ajic.2012.01.009. PubMed: 22483236. [DOI] [PubMed] [Google Scholar]
- 30. Pan SC, Wang JT, Chen YC, Chang YY, Chen ML et al. (2012) Incidence of and risk factors for infection or colonization of vancomycin-resistant enterococci in patients in the intensive care unit. PLOS ONE 7: e47297. doi:10.1371/journal.pone.0047297. PubMed: 23071778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Yoon YK, Kim HJ, Lee WJ, Lee SE, Yang KS et al. (2012) Clinical prediction rule for identifying patients with vancomycin-resistant enterococci (VRE) at the time of admission to the intensive care unit in a low VRE prevalence setting. J Antimicrob Chemother 67: 2963-2969. doi:10.1093/jac/dks303. PubMed: 22888271. [DOI] [PubMed] [Google Scholar]
- 32. Huang SS, Datta R, Rifas-Shiman S, Kleinman K, Placzek H et al. (2011) Colonization with antibiotic-susceptible strains protects against methicillin-resistant Staphylococcus aureus but not vancomycin-resistant enterococci acquisition: a nested case-control study. Crit Care 15: R210. doi:10.1186/cc9630. PubMed: 21914221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Huskins WC, Huckabee CM, O’Grady NP, Murray P, Kopetskie H et al. (2011) Intervention to reduce transmission of resistant bacteria in intensive care. N Engl J Med 364: 1407-1418. doi:10.1056/NEJMoa1000373. PubMed: 21488763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Minhas P, Perl TM, Carroll KC, Shepard JW, Shangraw KA et al. (2011) Risk factors for positive admission surveillance cultures for methicillin-resistant Staphylococcus aureus and vancomycin-resistant enterococci in a neurocritical care unit. Crit Care Med 39: 2322-2329. doi:10.1097/CCM.0b013e3182227222. PubMed: 21705905. [DOI] [PubMed] [Google Scholar]
- 35. Climo MW, Sepkowitz KA, Zuccotti G, Fraser VJ, Warren DK et al. (2009) The effect of daily bathing with chlorhexidine on the acquisition of methicillin-resistant Staphylococcus aureus, vancomycin-resistant Enterococcus, and healthcare-associated bloodstream infections: results of a quasi-experimental multicenter trial. Crit Care Med 37: 1858-1865. doi:10.1097/CCM.0b013e31819ffe6d. PubMed: 19384220. [DOI] [PubMed] [Google Scholar]
- 36. Song JY, Cheong HJ, Jo YM, Choi WS, Noh JY et al. (2009) Vancomycin-resistant Enterococcus colonization before admission to the intensive care unit: a clinico-epidemiologic analysis. Am J Infect Control 37: 734-740. doi:10.1016/j.ajic.2008.09.025. PubMed: 19188004. [DOI] [PubMed] [Google Scholar]
- 37. Wibbenmeyer L, Appelgate D, Williams I, Light T, Latenser B et al. (2009) Effectiveness of universal screening for vancomycin-resistant enterococcus and methicillin-resistant Staphylococcus aureus on admission to a burn-trauma step-down unit. J Burn Care Res 30: 648-656. doi:10.1097/BCR.0b013e3181abff7e. PubMed: 19506499. [DOI] [PubMed] [Google Scholar]
- 38. Drees M, Snydman DR, Schmid CH, Barefoot L, Hansjosten K et al. (2008) Antibiotic exposure and room contamination among patients colonized with vancomycin-resistant enterococci. Infect Control Hosp Epidemiol 29: 709-715. doi:10.1086/589582. PubMed: 18631116. [DOI] [PubMed] [Google Scholar]
- 39. Lambiase A, Del Pezzo M, Piazza O, Petagna C, De Luca C et al. (2007) Typing of vancomycin-resistant Enterococcus faecium strains in a cohort of patients in an Italian intensive care Unit. Infection 35: 428-433. doi:10.1007/s15010-007-6288-4. PubMed: 18034209. [DOI] [PubMed] [Google Scholar]
- 40. Littvik AM, López TN, González SE, Fernández CM, Pavan JV (2006) Colonization with vancomycin-resistant enterococci (VRE) in intensive care unit patients in Córdoba City, Argentina. Rev Argent Microbiol 38: 28-30. PubMed: 16784130. [PubMed] [Google Scholar]
- 41. Peta M, Carretto E, Barbarini D, Zamperoni A, Carnevale L et al. (2006) Outbreak of vancomycin-resistant Enterococcus spp. in an Italian general intensive care unit. Clin Microbiol Infect 12: 163-169. doi:10.1111/j.1469-0691.2005.01331.x. PubMed: 16441455. [DOI] [PubMed] [Google Scholar]
- 42. Vernon MO, Hayden MK, Trick WE, Hayes RA, Blom DW et al. (2006) Chlorhexidine gluconate to cleanse patients in a medical intensive care unit: the effectiveness of source control to reduce the bioburden of vancomycin-resistant enterococci. Arch Intern Med 166: 306-312. doi:10.1001/archinte.166.3.306. PubMed: 16476870. [DOI] [PubMed] [Google Scholar]
- 43. Furuno JP, Perencevich EN, Johnson JA, Wright MO, McGregor JC et al. (2005) Methicillin-resistant Staphylococcus aureus and vancomycin-resistant Enterococci co-colonization. Emerg Infect Dis 11: 1539-1544. doi:10.3201/eid1110.050508. PubMed: 16318693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Harris AD, Nemoy L, Johnson JA, Martin-Carnahan A, Smith DL et al. (2004) Co-carriage rates of vancomycin-resistant Enterococcus and extended-spectrum beta-lactamase-producing bacteria among a cohort of intensive care unit patients: implications for an active surveillance program. Infect Control Hosp Epidemiol 25: 105-108. doi:10.1086/502358. PubMed: 14994933. [DOI] [PubMed] [Google Scholar]
- 45. Winston LG, Charlebois ED, Pang S, Bangsberg DR, Perdreau-Remington F et al. (2004) Impact of a formulary switch from ticarcillin-clavulanate to piperacillin-tazobactam on colonization with vancomycin-resistant enterococci. Am J Infect Control 32: 462-469. doi:10.1016/j.ajic.2004.07.004. PubMed: 15573053. [DOI] [PubMed] [Google Scholar]
- 46. Yeh KM, Siu LK, Chang JC, Chang FY (2004) Vancomycin-resistant enterococcus (VRE) carriage and infection in intensive care units. Microb Drug Resist 10: 177-183. doi:10.1089/1076629041310091. PubMed: 15256034. [DOI] [PubMed] [Google Scholar]
- 47. de Jonge E, Schultz MJ, Spanjaard L, Bossuyt PM, Vroom MB et al. (2003) Effects of selective decontamination of digestive tract on mortality and acquisition of resistant bacteria in intensive care: a randomised controlled trial. Lancet 362: 1011-1016. doi:10.1016/S0140-6736(03)14409-1. PubMed: 14522530. [DOI] [PubMed] [Google Scholar]
- 48. Ho PL. (2003) Hong Kong intensive care unit antimicrobial resistance study G (2003) Carriage of methicillin-resistant Staphylococcus aureus, ceftazidime-resistant Gram-negative bacilli, and vancomycin-resistant enterococci before and after intensive care unit admission. Crit Care Med 31: 1175-1182. doi:10.1097/01.CCM.0000059437.01924.97. PubMed: 12682490. [DOI] [PubMed] [Google Scholar]
- 49. Martínez JA, Ruthazer R, Hansjosten K, Barefoot L, Snydman DR (2003) Role of environmental contamination as a risk factor for acquisition of vancomycin-resistant enterococci in patients treated in a medical intensive care unit. Arch Intern Med 163: 1905-1912. doi:10.1001/archinte.163.16.1905. PubMed: 12963563. [DOI] [PubMed] [Google Scholar]
- 50. Warren DK, Kollef MH, Seiler SM, Fridkin SK, Fraser VJ (2003) The epidemiology of vancomycin-resistant Enterococcus colonization in a medical intensive care unit. Infect Control Hosp Epidemiol 24: 257-263. doi:10.1086/502199. PubMed: 12725354. [DOI] [PubMed] [Google Scholar]
- 51. Gardiner D, Murphey S, Ossman E, Jungkind D (2002) Prevalence and acquisition of vancomycin-resistant enterococci in a medical intensive care unit. Infect Control Hosp Epidemiol 23: 466-468. doi:10.1086/502087. PubMed: 12186214. [DOI] [PubMed] [Google Scholar]
- 52. Puzniak LA, Leet T, Mayfield J, Kollef M, Mundy LM (2002) To gown or not to gown: the effect on acquisition of vancomycin-resistant enterococci. Clin Infect Dis 35: 18-25. doi:10.1086/340739. PubMed: 12060870. [DOI] [PubMed] [Google Scholar]
- 53. Hendrix CW, Hammond JM, Swoboda SM, Merz WG, Harrington SM et al. (2001) Surveillance strategies and impact of vancomycin-resistant enterococcal colonization and infection in critically ill patients. Ann Surg 233: 259-265. doi:10.1097/00000658-200102000-00016. PubMed: 11176133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Marín ME, Podestá O, Llambías P, Galdón F, Scilingo VM et al. (2001) Detection of carriage of vancomycin-resistant enterococci in an intensive care unit in Buenos Aires. Infect Control Hosp Epidemiol 22: 332-333. doi:10.1086/503402. PubMed: 11519907. [DOI] [PubMed] [Google Scholar]
- 55. Dan M, Poch F, Leibson L, Smetana S, Priel I (1999) Rectal colonization with vancomycin-resistant enterococci among high-risk patients in an Israeli hospital. J Hosp Infect 43: 231-238. doi:10.1053/jhin.1998.0641. PubMed: 10582190. [DOI] [PubMed] [Google Scholar]
- 56. Grayson ML, Grabsch EA, Johnson PD, Olden D, Aberline M et al. (1999) Outcome of a screening program for vancomycin-resistant enterococci in a hospital in Victoria. Med J Aust 171: 133-136. PubMed: 10474604. [DOI] [PubMed] [Google Scholar]
- 57. Ostrowsky BE, Venkataraman L, D’Agata EM, Gold HS, DeGirolami PC et al. (1999) Vancomycin-resistant enterococci in intensive care units: high frequency of stool carriage during a non-outbreak period. Arch Intern Med 159: 1467-1472. doi:10.1001/archinte.159.13.1467. PubMed: 10399898. [DOI] [PubMed] [Google Scholar]
- 58. Zuckerman RA, Steele L, Venezia RA, Tobin EH (1999) Undetected vancomycin-resistant Enterococcus in surgical intensive care unit patients. Infect Control Hosp Epidemiol 20: 685-686. doi:10.1086/501565. PubMed: 10530646. [DOI] [PubMed] [Google Scholar]
- 59. Slaughter S, Hayden MK, Nathan C, Hu TC, Rice T et al. (1996) A comparison of the effect of universal use of gloves and gowns with that of glove use alone on acquisition of vancomycin-resistant enterococci in a medical intensive care unit. Ann Intern Med 125: 448-456. doi:10.7326/0003-4819-125-6-199609150-00004. PubMed: 8779456. [DOI] [PubMed] [Google Scholar]
- 60. Pogorzelska M, Stone PW, Larson EL (2012) Certification in infection control matters: Impact of infection control department characteristics and policies on rates of multidrug-resistant infections. Am J Infect Control 40: 96-101. doi:10.1016/j.ajic.2011.10.002. PubMed: 22381222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Borg MA, Camilleri L, Waisfisz B (2012) Understanding the epidemiology of MRSA in Europe: do we need to think outside the box? J Hosp Infect 81: 251-256. doi:10.1016/j.jhin.2012.05.001. PubMed: 22695171. [DOI] [PubMed] [Google Scholar]
- 62. Top J, Willems R, Bonten M (2008) Emergence of CC17 Enterococcus faecium: from commensal to hospital-adapted pathogen. FEMS Immunol Med Microbiol 52: 297-308. doi:10.1111/j.1348-0421.2008.00039.x. PubMed: 18279340. [DOI] [PubMed] [Google Scholar]
- 63. Werner G, Coque TM, Hammerum AM, Hope R, Hryniewicz W et al. (2008) Emergence and spread of vancomycin resistance among enterococci in Europe. Euro Surveill 13: ([MedlinePgn:]) PubMed: 19021959. [PubMed] [Google Scholar]
- 64. Hidron AI, Edwards JR, Patel J, Horan TC, Sievert DM et al. (2008) NHSN annual update: antimicrobial-resistant pathogens associated with healthcare-associated infections: annual summary of data reported to the National Healthcare Safety Network at the Centers for Disease Control and Prevention, 2006-2007. Infect Control Hosp Epidemiol 29: 996-1011. doi:10.1086/591861. PubMed: 18947320. [DOI] [PubMed] [Google Scholar]
- 65. Meyer E, Schwab F, Schroeren-Boersch B, Gastmeier P (2010) Dramatic increase of third-generation cephalosporin-resistant E. coli in German intensive care units: secular trends in antibiotic drug use and bacterial resistance, 2001 to 2008. Crit Care 14: R113. doi:10.1186/cc8345. PubMed: 20546564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Bourdon N, Fines-Guyon M, Thiolet JM, Maugat S, Coignard B et al. (2011) Changing trends in vancomycin-resistant enterococci in French hospitals, 2001-08. J Antimicrob Chemother 66: 713-721. doi:10.1093/jac/dkq524. PubMed: 21393182. [DOI] [PubMed] [Google Scholar]
- 67. Safdar N, Maki DG (2002) The commonality of risk factors for nosocomial colonization and infection with antimicrobial-resistant Staphylococcus aureus, enterococcus, gram-negative bacilli, Clostridium difficile, and Candida. Ann Intern Med 136: 834-844. doi:10.7326/0003-4819-136-11-200206040-00013. PubMed: 12044132. [DOI] [PubMed] [Google Scholar]
- 68. Olivier CN, Blake RK, Steed LL, Salgado CD (2008) Risk of vancomycin-resistant Enterococcus (VRE) bloodstream infection among patients colonized with VRE. Infect Control Hosp Epidemiol 29: 404-409. doi:10.1086/587647. PubMed: 18419361. [DOI] [PubMed] [Google Scholar]
- 69. Patel R, Allen SL, Manahan JM, Wright AJ, Krom RA et al. (2001) Natural history of vancomycin-resistant enterococcal colonization in liver and kidney transplant recipients. Liver Transpl 7: 27-31. doi:10.1053/jlts.2001.20784. PubMed: 11150418. [DOI] [PubMed] [Google Scholar]
- 70. Matar MJ, Tarrand J, Raad I, Rolston KV (2006) Colonization and infection with vancomycin-resistant Enterococcus among patients with cancer. Am J Infect Control 34: 534-536. doi:10.1016/j.ajic.2006.04.205. PubMed: 17015161. [DOI] [PubMed] [Google Scholar]
- 71. Weinstock DM, Conlon M, Iovino C, Aubrey T, Gudiol C et al. (2007) Colonization, bloodstream infection, and mortality caused by vancomycin-resistant enterococcus early after allogeneic hematopoietic stem cell transplant. Biol Blood Marrow Transplant 13: 615-621. doi:10.1016/j.bbmt.2007.01.078. PubMed: 17448922. [DOI] [PubMed] [Google Scholar]
- 72. Tschudin Sutter S, Frei R, Dangel M, Gratwohl A, Bonten M et al. (2010) Not all patients with vancomycin-resistant enterococci need to be isolated. Clin Infect Dis 51: 678-683. doi:10.1086/655824. PubMed: 20687839. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
PRISMA Checklist S1.
(DOC)
Study quality data (assigned scores).
(XLSX)
Flow diagram of meta-analysis.
(DOCX)