Abstract
Background
Interventions to prevent and control childhood obesity have shown mixed results in terms of short- and long-term changes.
Objectives
“MOVE/me Muevo” was a two-year family- and recreation center-based randomized controlled trial to promote healthy eating and physical activity among 5-8 year old children. It was hypothesized that children in the intervention group would demonstrate lower post-intervention BMI values and improve obesity-related behaviors compared to control group children.
Methods
Thirty recreation centers in San Diego County, California were randomized to an intervention or control condition. Five hundred and forty-one families were enrolled and children’s body mass index (BMI), diet, physical activity and other health indicators were tracked from baseline to two years post-baseline. Analyses followed an intent-to-treat approach using mixed effects models.
Results
No significant intervention effects were observed for the primary outcomes of child or parent BMI and child waist circumference. Moderator analyses however showed girls (but not boys) in the intervention condition reduced their BMI. At the two-year follow-up, intervention condition parents reported that their children were consuming fewer high-fat foods and sugary beverages.
Conclusions
Favorable implementation fidelity and high retention rates support the feasibility of this intervention in a large metropolitan area; however, interventions of greater intensity may be needed to achieve effects on child’s BMI. Also, further research is needed to develop gender-specific intervention strategies so that both genders may benefit from such efforts.
INTRODUCTION
The prevalence of overweight and obesity among U.S. children is now 32% and 17%, respectively (1). Rates are higher among racially/ethnically diverse and low-income families, and are further pronounced among Latino/Hispanic children in the U.S. (2). Overweight and obesity in childhood have adverse consequences on premature mortality and morbidity in adulthood (3), making it a public health priority (4). Despite the vast literature describing obesity prevention interventions among children, study results are inconsistent on child anthropometric outcomes (5, 6).
Diet, physical activity, and sedentary behaviors are the key behavioral targets for preventing and controlling childhood obesity and it is important to consider the physical and social contexts in which these behaviors occur (7). According to the socio-ecological framework (7, 8), obesity-related behaviors are influenced by proximal (e.g., family influence) and distal (e.g., availability of recreation facilities) factors that may have independent and synergistic effects on them. In the present study, proximal factors included aspects of parenting and the family home. Distal factors comprised community recreational environments, specifically recreation centers close to the families’ homes.
Parents are agents of change (9) and are ultimately responsible for what their children eat and do (10, 11). Parents influence children through modeling (12, 13) and supporting (14, 15) healthy and unhealthy behaviors (12, 13), monitoring eating and activity (16), controlling resources and access to foods and physical activity, and reducing unhealthy food consumption and sedentary behavior (9, 17). Thus, the role of the parent must be emphasized in obesity prevention efforts.
The community environment influences risk for child obesity through many factors including availability of recreation centers, parks, and other green spaces that promote active play, and retail food outlets such as corner stores, mobile vendors, and fast food restaurants (18). Most of children’s physical activity occurs outside school, such as at home and at community centers (19). City recreation centers and other community facilities comprise important public resources; however, their contribution to health promotion is not fully understood (20). In addition to their potential to promote physical activity through program, policy, and environmental changes, city recreation centers have the potential to improve diet by regulating vending machine access and content and improving food quality at center events (21). Well-designed research studies examining the efficacy of implementing health promotion interventions in city recreation centers are few and limited (19), but pilot research is promising (21).
This paper describes the design and evaluation of a two-year family- and recreation center-based obesity prevention and control intervention for 5-8 year old children and their families compared with a measurement-only control condition. The primary study hypothesis was that children in the intervention condition would have lower BMI z-scores compared to children in the control condition after the two years. Secondary study hypotheses were that compared to the control children, children in the intervention condition would spend more time in moderate-to-vigorous physical activity and less time doing sedentary behaviors, consume fewer high-fat foods and sugary beverages, and more fruits, vegetables, and water.
METHODS AND PROCEDURES
Study Design, Recreation Centers and Participants
MOVE/me Muevo (MOVE study) was a randomized community trial with a two-group by three repeated measures design, occurring between May 2007 – May 2009. Thirty public recreation centers in San Diego County were recruited and randomly assigned to either intervention (n=15) or control condition (n=15). A recreation center for the current study was defined as a) a public agency managed by a city or county parks and recreation department; b) having a facility usable for physical activity; and c) currently offering some type of physical activity program to youth.
A total of 541 families with children between the ages of 5 and 8 years old were enrolled into the study. Inclusion criteria were: 1) lived within two miles of one of the centers, 2) participated or were willing to participate in activities at the recreation centers, 3) willing to participate in the study for two years, 4) willing to be randomly assigned to the intervention or control condition, and 5) able to speak, read, and understand either English or Spanish. Children were excluded if they had a medical and/or psychological condition that affected their diet, physical activity, or weight. Families were recruited through targeted phone calls; 8600 telephone numbers were obtained from a research marketing company. In addition, 1000 families were contacted at public locations, such as libraries, schools, community events (street fairs, special gatherings) and the 30 participating recreation centers. In accordance with the study design, recreation centers were the unit of randomization and individual participating families were the unit of analysis (~18 families per recreation center). Parents provided written informed consent and children verbal assent to participate. This study was approved by the sponsoring university’s Institutional Review Board.
Intervention
Feasibility study
A feasibility study was conducted with a non-eligible recreation center and families living within 1 mile of that center. At the recreation center, a half-day training was held for recreation center staff focusing on implementation of physical activity and healthy eating recreation center policies. Four weekly family workshops were held at the center and a pilot test of home visits was conducted using the intervention materials and approaches, process evaluation instruments, and height and weight measurement protocols. It was found that parents rarely used educational materials that were inside a folder or binder. As a result, one- and two-page tip sheets were created. Each tip sheet focused on strategies that the parents could use to promote healthy eating and physical activity in their children.
Intervention Staff Training
The intervention team consisted of two full-time Family Health Coaches (FHCs), a full-time Recreation Specialist (RS), a half-time Recreation Assistant (RA), and a full-time Intervention Coordinator (IC). Bilingual and bicultural FHCs were recruited based on previous experience working with families and children and motivation to promote health. The FHCs, RS, and IC all received 44 hours of training that started one month prior to intervention initiation and ended three months before termination. Training included family and center intervention procedures, motivational interviewing skills, and role-playing scenarios, with additional practice for FHCs and RS provided as needed. Daily oversight and weekly meetings helped ensure intervention fidelity and observations of homes and centers provided additional evidence of compliance.
Family Intervention
The family intervention was delivered by two FHCs and tailored to the family’s needs to target physical and social aspects of the home environment, including setting household rules. As outlined in Table 1, to engage families in the intervention with the FHC and at the recreation center, the first six months of the family intervention consisted of a ten-minute telephone survey about the families’ recreation center use followed by an introductory 1½ hour group workshop at the recreation center, and a one-hour home visit. Families were introduced to the tip sheets during the introductory workshop and then received tip sheets by mail and two ten-minute follow-up phone calls during the intervention. The tip sheets offered simple strategies for parents to use to promote healthy eating and physical activity in their children. For families with children in the normal weight range, the intervention focused on maintaining healthy eating and physical activity habits. Parents were instructed to select one tip to try for a week and then report progress or challenges with the FHC during the phone consultation. During the phone consultations, the FHCs used motivational interviewing techniques to help the primary caregiver identify how the tips could be used to promote healthy lifestyles in their family, problem solve challenges, and identify benefits. Self-monitoring and goal setting were individualized to the participating families’ progress and preferences. A total of four group workshops were conducted, two each year, during the remainder of the intervention. Among families who were difficult to reach and engage, additional approaches were incorporated such as email and drop-by visits.
Table 1.
Summary of intervention components and implementation fidelity.
| Intervention Components | Intended Delivery | Fidelity | % Received |
|---|---|---|---|
| Telephone survey about the family’s recreation center use (10 minutes; prior to introductory workshop) |
1 | 203/272 | 75% |
| Introductory group workshop at the recreation center (1½ hours; month 1 of intervention) |
1 | 155/272 | 57% |
| Home visit (1 hour; within the first 6 months of intervention) |
1 | 248/272 | 91% |
| Mailed tip sheets (approximately monthly during intervention) |
8 | 239/239 | 100% |
| Phone consultations on tip sheet (10 minutes; twice per tip sheet) |
18 | 179/239 | 75% |
| Group workshops at the recreation center (1½ hours; quarterly during intervention) |
3 | 143/239 | 60% |
Fidelity: number of participants that received the intended intervention component divided by total number of intervention participants.
The targeted nutrition behaviors addressed by the FHCs included: (1) increase consumption of vegetables and fruits through modifications in meal and snack purchasing and preparation, (2) decrease consumption of sugary beverages through changes in food purchasing and limit setting, (3) increase healthy portions by modifying food consumption behaviors, (4) reduce eating out and when eating out, select healthy options, (5) increase availability and accessibility of healthy foods and beverages in the home, (6) reduce screen time and avoid eating in front of the television, and (7) increase the number of meals eaten together as a family.
The targeted physical activity behaviors included: (1) increase the amount of moderate to vigorous physical activity to 60 minutes per day on most days of the week, (2) increase availability and accessibility of physical activity opportunities in the home and community, and (3) increase the variety of fun, developmentally appropriate, and culturally appropriate physical activity opportunities.
Recreation Center Intervention
The recreation center intervention emphasized making changes in the quantity and quality of physical activity and healthy food and beverage offerings within the centers and targeted center policies, programs, and facilities. A recreation specialist (RS) was hired and trained by the study team to work with recreation center directors to increase overall attendance of community members and enrollment of children in physical activity programs. The RS met monthly with intervention centers’ personnel throughout the intervention to develop an action plan, monitor progress, and implement sustainable health policies. During the first six months, the RS gathered information from the recreation center on how to achieve the overall goal to help families identify the recreation center as a prominent community resource for physical activity. The RS conducted four meetings with the center director and meetings with each recreation staff member, attended a recreation or city council meeting, and conducted a structured observation of the recreation center and audits of two physical activity programs in addition to a meeting with the instructor. A summary report was created and presented to each center director that provided an overview of: (1) current physical activity and healthy food opportunities for children ages 5-8 at the recreation centers, (2) the MOVE families’ utilization, experiences, and views of the center and park as a place for physical activity, and (3) instructor and recreation staff views regarding the benefits received and resources needed to attain the goal of the MOVE/me Muevo recreation component. From this report, it was determined that staff trainings focused on activity programming were not feasible to implement given reductions in staffing and increased use of contractual staff. Instead, the focus was placed on addressing gaps in promotional and other customer service related activities, particularly for families who were unfamiliar with the center. During the remainder of the intervention period, the RS worked with the recreation centers to develop action plans for promoting the center and engaging customers in their activities and services.
Control Condition
Families and recreation centers assigned to the control condition completed measures on the same schedule as those in the intervention conditions. To promote cohort retention, at the one-year measurements, interactive booths were set up at the recreation center for families to receive take-home information and giveaways on non-obesity related topics. Children participated in crafts and science experiments. Families received information on dental care, fire safety, environmental awareness, and video game ratings. After the completion of the study, control condition families were invited to a modified group workshop, and received the family intervention materials. Control centers were provided with an overview and copies of the recreation center materials.
Measures: Primary outcome, secondary outcomes and demographics
Body Mass Index
Parent and child height and weight were measured with shoes off using a standard portable stadiometer and a standard scale, and BMI was calculated using the Quetelet index (kg/m2). Child BMI for age- and gender- was calculated using the CDC 2000 reference data. Parent and child weight categories were classified based on standard cut points.
Waist Circumference
Waist circumference was measured by locating the narrowest part of the child’s torso and placing a measuring tape snugly around the abdomen, without causing compressions on the skin. The measurements were repeated until the difference between two consecutive trials was less than 1 centimeter.
Total Percent Body Fat
The RJL Quantum II Body Composition Analyzer (Clinton Township, MI) was used to measure children’s total percent body fat. Children lay in a supine position on a mat on the floor with arms adjacent to, but not touching the body, palms flat against the mat, and legs adjacent to each other but not touching. Two surface self-adhesive spot electrodes were placed on the dorsal surface of the right hand and two electrodes on the dorsal surface of the right foot. Measurements were repeated until the difference in values between two trials was less than 1.0%. A prediction equation for children was used to calculate child percent fat (22).
Physical Activity and Sedentary Time
Physical activity was assessed objectively in a subsample of participants (n=178 at baseline and n=373 at 2-year follow-up) using the Actigraph accelerometer (Pensacola, FL). Accelerometry data were analyzed using a batch processing program (MAHUffe: http://www.mrc-epid.cam.ac.uk) to remove any data recorded after 11pm and before 6am; periods of 30 minutes or more that had continuous zero activity counts, and any days with less than 540 minutes of recording (the cut-off used to define a valid day) (23). Children with fewer than three of seven valid days of recording (including at least one weekend-day and two weekdays) were also excluded (24). The data were examined as time spent in moderate and vigorous physical activity (MVPA) derived using age specific equations (25, 26) to determine activity over 4.5 METS. Valid minutes spent below 100 counts per minute were used as an estimate of sedentary time (27). Before being applied to the data, the cut-points were divided by two in order to get a 30-second cut-point to match the 30-second data collection epoch.
Self-Report Measures
Parents completed a self-administered survey in either Spanish or English. The survey included questions concerning the child’s diet, demographics and acculturation.
Demographics
Child and parent demographics included ethnicity, gender and age for both, and parental education, income, employment, and marital status.
Parent Acculturation
A shortened version of the Short Acculturation Scale for Hispanics (SASH) was used to measure primarily language-based acculturation (28). The original scale showed an internal consistency of α=0.92 (34) and was α=0.93 in the MOVE study sample. The scale produces a summary acculturation score with a higher score indicating greater acculturation.
Child Diet
Fat consumption was assessed using a previously validated 21-item screener developed for the Patient-Centered Assessment and Counseling for Exercise Plus Nutrition (PACE+) Health and Environment Survey (29). Intraclass correlation (ICC) = 0.64 and test-retest reliability and internal consistency of the scale were high (α=0.88). Validation of the screener was confirmed using 3-day food records (r=0.36, P<.01) (35). In the current study, the internal consistency was α=0.62. Examples of assessed food items include hot dogs, bacon, and cold cuts/lunch meats. Responses made by the parents on behalf of the children were summed to generate a child’s total fat consumption score (range: 0-105), with higher scores indicating greater consumption of high fat foods.
Sugary beverage consumption was assessed using three items from a previously validated scale: non-diet soda, non-carbonated sugary drinks, and sports drinks (30). Validation was confirmed in a previous study using 24-hour recalls (r=0.54) (36) and internal consistency of the scale was good in the present study (α=0.52). Response options for non-diet soda were based upon consumption of a 12-oz can/glass and included: never/less than 1 per month, 1-3 cans/glasses per month, 1 can/glass per week, 2-6 cans/glasses per week, 1 can/glass per day, and 2 or more cans/glasses per day. Responses for each item were converted to mean daily servings and then summed. Higher scores indicated greater mean daily servings of sugary beverages.
Consumption of 100% fruit juice was assessed using one item from the previously validated scale for sugary beverage consumption (30). Response options were based upon frequency of consumption of an 8 oz. glass and included: never/less than 1 per month, 1-3 glasses per month, 1 glass per week, 2-6 glasses per week, 1 glass per day, and 2 or more glasses per day. Responses were converted to mean daily servings, then dichotomized into meeting or not meeting recommended guidelines for 100% fruit juice consumption of no more than four to six oz/day for children ages one through six years and eight to 12 oz/day for older children (31).
Fruit and vegetable consumption were assessed by parents reporting how many servings of fruit, not counting fruit juice or other drinks, their child eats in a typical day and how many servings of vegetables, not counting French fries, onion rings, potato chips or fried vegetables, their child eats in a typical day. Previous test-retest intraclass correlation ranged from ICC=0.80 to ICC=0.47 for same day retest to retest up to 1 month. Previous validation of the fruit and vegetable screener was confirmed using a 3-day food record (r=0.23) (32), with an internal consistency of α=0.65 in the current study. Response options included none, one, two, three, or four or more daily servings. Responses for fruit consumption were dichotomized into meeting or not meeting the recommended guidelines of 1.5 cups of fruit per day for both boys and girls ages 4-8 years old (33). Responses for vegetable consumption were dichotomized into meeting or not meeting the recommended guidelines of 1.5 cups of vegetables per day and 1 cup of vegetables per day, respectively, for boys and girls ages 4-8 years old (33).
Water consumption was assessed by asking parents how often their child consumes an 8-oz. glass of water. Responses were dichotomized into meeting or not meeting recommendations for water intake of 1.7 L/day and 1.5 L/day, respectively, for boys and girls ages 6-11 years old (34).
Process evaluation
Process data related to intervention fidelity included tabulations of the number and types of contacts completed for each participating family. Table 1 describes the family and recreation center intervention components and their respective implementation fidelity measures.
Analyses
Primary and Secondary Outcomes
All analyses were based on the intention-to-treat approach. Each outcome was examined using mixed effects models for normal outcomes (SAS Proc Mixed) (Cary, NC) or generalized linear mixed effects models for non-normal outcomes (SAS Proc Glimmix). For non-normal outcomes, appropriate error distribution and link functions were chosen according to the type of outcome. For dichotomous variables (e.g., meeting dietary guidelines), a logistic-type model was used with a binomial error and logit link. For counting outcomes (e.g., fruit or vegetable servings), either a Poisson or negative binomial regression was chosen according to which provided the best model fit. All models accounted for clustering of recreation centers by including a random effect term. When both 1-year and 2-year follow-up measures were available, repeated measures were accounted for in the model and a condition-by-time interaction was included to assess a differential intervention effect over time. If the interaction term was not significant, the interaction was dropped from the model and a second model was fitted. The test for condition main effect is based on the second model. Most models adjusted for baseline level. For the physical activity measures, sample sizes at baseline were quite small relative to the samples available at 2-year follow-up. Therefore no adjustment is made at baseline since the available sample size would be reduced considerably. For each model, all available data were utilized. Thus, although a participant may have data missing at 1-year or 2-year follow-up, data available at non-missing time points were still included in the analysis. For dietary outcomes all models adjusted for caregiver ethnicity, acculturation, education and age, and child gender and BMI. Some models for dietary outcomes were adjusted for physical activity level. However, since the smaller sample size for physical activity reduced the number of children available for analysis, the physical activity covariate was removed from all models. For physical activity outcomes, models were adjusted for amount of time accelerometer was worn, child age, gender and BMI.
Intraclass correlations which assess the degree of recreation center clustering for the primary outcomes and continuous secondary measures ranged from 0 to .056. These ICCs were well within the range anticipated by the study.
Moderator Analyses
Moderation by gender and acculturation were examined given evidence that they are important moderators of childhood obesity (35). Moderation was examined by adding an interaction term to a model between the potential moderator and the condition main effect.
Power Calculation
The power calculation was based on our hypothesized effect size based on the available sample at 2-year follow-up. The total sample size at 2-year follow-up was 494, although all participants who contributed at least one measure at 1-year or 2-year follow-up were included in the analyses (analytic sample was n=489). Effect sizes were determined based on differences in BMI at 2-year follow-up. To determine effect size, information was obtained from the 2000 CDC BMI-for-age growth charts. We calculated the average BMI change at the 50th percentile that occurred for 7 and 8 year old boys and girls over a two-year period. That is, we took the difference in BMI between the 7-year olds and 9-year olds at the 50th percentile, and between the 8-year olds and 10-year olds. The average change was an increase of 0.843 k/m2 over two years. This amount was assumed to approximate the change expected without intervention in this age group. We hypothesized no change in BMI in the intervention group over two years. Therefore the hypothesized difference between the intervention and control group means was 0.843 k/m2. An estimate of standard deviation was derived from the SCAN project based on a baseline estimate of 2.80 k/m2. The estimated correlation in BMI from baseline to two years within child was 0.74. From this information and using the formula in Donner and Klar (36), the standard deviation for a two-year change score was estimated as 2.0 k/m2. Consequently the standardized effect size was estimated to be 0.42. The clustering attributed to recreation centers for BMI from our current sample was 0.038. Based on the information above and a significance level of 0.05 (two-sided), the power to detect an intervention effect was 94%.
RESULTS
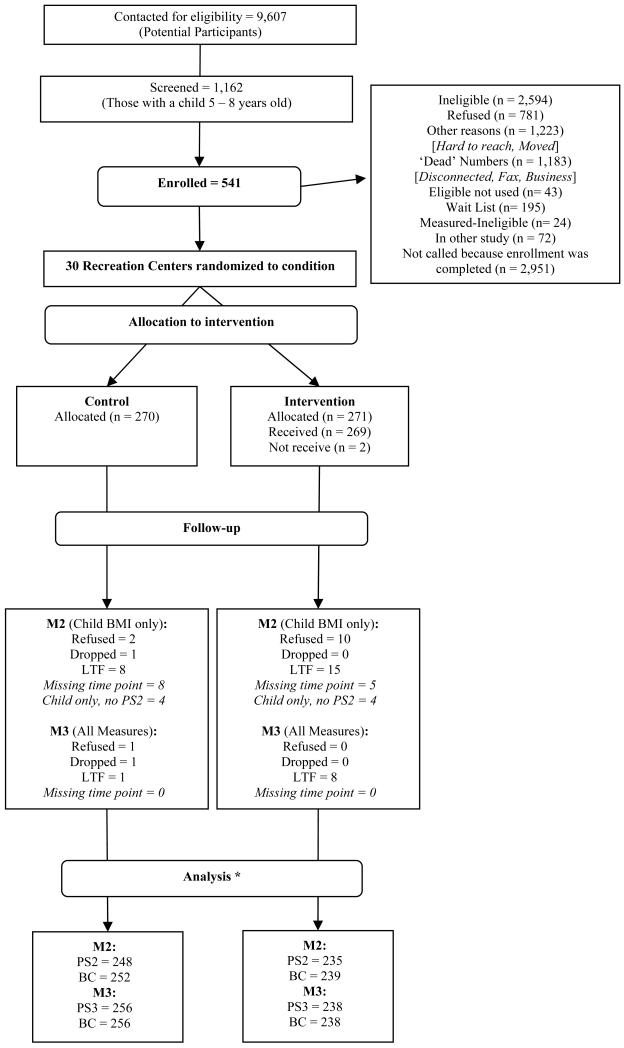
Of the 9607 parents contacted during the recruitment process, 2618 (27.3%) were ineligible, 72 (<1%) were excluded because they were already enrolled in other studies, 781 (8.1%) declined to participate, 2406 (25.0%) did not respond, and 3189 (33.2%) were not included as recruitment was complete (Figure 1). A total of 541 participants were measured at baseline and 489 completed the 2-year follow-up and are included in these analyses.
Figure 1.
CONSORT figure for the MOVE/me Muevo project reflecting recruitment and retention in the study at each measurement time point
LTF = Lost to follow-up
PS2 = M2 Parent Survey
PS3 = M3 Parent Survey
BC = Body Composition for child
The final analytic sample differs from the CONSORT figure samples due to exclusion of implausible data during analysis.
Intervention implementation varied with each component (Table 1). Participant attendance at the family workshops was somewhat low but all other intervention components were largely implemented as intended. The duration of contact with participating families varied by type of contact. For example, telephone contact ranged from 1 minute to 10 minutes (mean=4 minutes) and in-person contacts ranged from 4 minutes to 90 minutes (mean=65 minutes). The combined time for all contacts ranged from 31 minutes to 18.3 hours.
At baseline, 54.9% of the child participants were girls, 41.2% were Latino, the average age was 6.6 (SD=0.7) years, and 49.4% of families had a monthly household income over $5000 (37-39). Although there were no significant anthropometric or demographic differences between intervention and control condition parents and children at baseline, outcome analyses comparing conditions and moderators were adjusted for baseline and demographic factors.
Primary Outcomes
Table 2 presents the results for intervention effects on child BMI, waist circumference, total percent body fat and parent BMI. Results of mixed effects models after adjusting for selected covariates showed that none of the group-by-time interactions or condition main effects were statistically significant for these four variables.
Table 2.
Intervention effectsa on child BMI, waist circumference, total percent body fat, and parent BMI
| Outcomeb | Time | Group | Group*Time Interaction P-value |
Group Main Effect P-value |
|||||
|---|---|---|---|---|---|---|---|---|---|
| Intervention | Control | ||||||||
| N | Mean | SD | N | Mean | SD | ||||
| BMI | MI | 271 | 16.96 | 2.63 | 267 | 17.42 | 3.18 | ||
| M2 | 239 | 17.69 | 3.10 | 249 | 18.20 | 3.62 | |||
| M3 | 237 | 18.43 | 3.69 | 252 | 18.89 | 3.83 | |||
| Mean d | SE | Mean d | SE | ||||||
| 18.3 | .076 | 18.3 | .074 | .13 | .88 | ||||
| N | Mean | SD | N | Mean | SD | ||||
| BMI %ile | M1 | 271 | 64.99 | 26.76 | 267 | 70.66 | 23.90 | ||
| M2 | 239 | 64.69 | 27.25 | 249 | 69.94 | 24.12 | |||
| M3 | 237 | 63.97 | 28.43 | 252 | 69.86 | 24.97 | |||
| Mean d | SE | Mean d | SE | ||||||
| 67.3 | .86 | 67.5 | .84 | .81 | .88 | ||||
| N | Mean | SD | N | Mean | SD | ||||
| BMI z-score | M1 | 271 | 0.574 | 0.983 | 267 | 0.746 | 0.913 | ||
| M2 | 239 | 0.552 | 0.979 | 249 | 0.717 | 0.899 | |||
| M3 | 237 | 0.535 | 1.037 | 252 | 0.715 | 0.927 | |||
| Mean d | SE | Mean d | SE | ||||||
| .63 | .026 | .65 | .025 | .47 | .72 | ||||
| N | Mean | SD | N | Mean | SD | ||||
| WC (cm) | M1 | 271 | 56.78 | 6.13 | 269 | 57.97 | 6.96 | ||
| M3 | 238 | 62.44 | 9.45 | 254 | 64.22 | 10.11 | |||
| Mean d | SE | Mean d | SE | ||||||
| 63.4 | .32 | 63.3 | .34 | ---c | .83 | ||||
| Mean | SD | N | Mean | SD | |||||
| % Body Fat | M1 | 270 | 28.76 | 8.08 | 265 | 29.84 | 8.91 | ||
| M3 | 237 | 29.93 | 10.15 | 252 | 31.23 | 9.83 | |||
| Mean d | SE | Mean d | SE | ||||||
| 30.6 | .34 | 30.6 | .38 | ---c | .92 | ||||
| Mean | SD | N | Mean | SD | |||||
| Parent BMI | M1 | 270 | 27.53 | 6.29 | 266 | 28.67 | 6.62 | ||
| M3 | 238 | 27.81 | 5.90 | 252 | 28.67 | 6.47 | |||
| Mean d | SE | Mean d | SE | ||||||
| 27.9 | .15 | 28.0 | .17 | ---c | .83 | ||||
Mixed effects models were used to adjust for the clustering effects of recreation centers for all outcomes and repeated measures over time for BMI, BMI percentile and BMI z-score. Terms in the model: baseline level for the outcome variable, time and condition main effects. For models with repeated measures, a condition by time interaction was also included. If the interaction term was not significant, the interaction was dropped from the model and a second model was fitted. The test for condition main effect is based on the second model.
With the exception of caregiver BMI, all models were adjusted for child age and gender, and parent’s ethnicity, educational status, and marital status. The caregiver BMI model is adjusted for parent’s age, gender, ethnicity, educational status, and marital status.
No interaction could be tested since only M3 measure was available.
Adjusted mean from mixed effects analysis.
BMI = body mass index, BMI%ile = BMI percentile, WC = waist circumference, % body fat = total percent body fat
Moderators of Primary and Secondary Outcomes
Although the primary group-by-time interactions were not statistically significant, results of moderator analyses on the primary and secondary anthropometric outcomes indicated that child gender moderated intervention effects on child BMI outcomes and waist circumference as shown in Table 3. Subsequent contrasts stratified by gender are also shown in Table 3. All three BMI outcomes and waist circumference show a reduction for girls in the intervention condition compared to those in the control condition in the expected direction (adjusted means in Table 3), although none of the stratified comparisons were significant (p>0.05.)
Table 3.
Stratified Analyses for Significant Moderators
| Outcome | Outcome by moderator Interaction p-value |
Moderator and Strata | Condition Main Effect | ||||
|---|---|---|---|---|---|---|---|
| Control | Intervention | p-value | |||||
| Meanb | SE | Meanb | SE | ||||
| BMI | .01 | Child gender: Male | 18.2 | .09 | 18.4 | .10 | .14 |
| Female | 18.4 | .11 | 18.2 | .10 | .06 | ||
| BMI%ile | .04 | Child gender: Male | 65.8 | 1.1 | 67.4 | 1.1 | .27 |
| Female | 69.7 | 1.2 | 67.3 | 1.1 | .14 | ||
| BMI z-score | .02 | Child gender: Male | .59 | .03 | .65 | .04 | .23 |
| Female | .71 | .04 | .62 | .04 | .06 | ||
| WC (cm) | .02 | Child gender: Male | 62.7 | .30 | 63.6 | .39 | .05 |
| Female | 64.0 | .60 | 63.1 | .47 | .22 | ||
| WC (cm) | <0.01 | Parent acculturation: continuousa |
--- | --- | --- | --- | --- |
| % Body Fat | .04 | Parent acculturation: dichotomous Other/Mix |
30.0 | .53 | 30.7 | .45 | .25 |
| English only | 31.4 | .50 | 30.5 | .41 | .11 | ||
For continuous parent acculturation no stratified analyses were possible. Interpretation was based on the magnitude and direction of the regression coefficients for main effects and the acculturation by condition interaction as the language score ranged from 1 (less acculturated) to 5 (most acculturated: English only)
Adjusted means from mixed effects analysis.
Parent acculturation, measured continuously, was as a moderator for child waist circumference (interaction term p<0.05, Table 3). In exploratory analyses of the pattern of regression coefficients for the interaction and main effects terms (data not shown), it appears that intervention children with less (versus more) acculturated parents had a larger waist circumference. However, as the score increases to 5 (English only) this discrepancy diminished to near 0. Dichotomized parent acculturation was also a moderator on child percent body fat (interaction term p<0.05). The trend in the pattern of adjusted means for child percent body fat suggests that the English-only subgroup may have benefited from the intervention while the “other or mixed” acculturation group went in the opposite direction, though again, the difference is not statistically significant within this stratum.
Secondary Behavioral Outcomes
At baseline, none of the condition comparisons for secondary behavioral outcomes were statistically significant with the exception of child fat consumption with intervention children having had significantly higher fat consumption than control children (21.1 vs. 19.7, p<0.05).
Table 4 shows the results for secondary behavioral outcomes. For outcomes with repeated follow-up measures none of the condition-by-time interactions were significant, indicating that differences between intervention and control conditions do not differ over time. Two main effects for diet were statistically significant. The adjusted means for fat consumption (p<0.05) suggest that the overall mean score in the intervention condition was significantly lower than in the control condition. Sugary beverage consumption was significantly lower in the intervention condition compared with control (p<0.01). No significant differences were found on 100% fruit juice consumption, physical activity measures, and sedentary time.
Table 4.
Mixed Effects Modelsa to Evaluate Intervention Efficacy on Secondary Behavioral Outcomes
| Continuous Outcomes | Group*Time Interaction |
Group Main Effect | ||||
|---|---|---|---|---|---|---|
| Intervention | Control | p-value | ||||
| p-value | Meanf | SE | Meanf | SE | ||
| Dietary measures b | ||||||
| Fat consumption | ---e | 18.1 | .41 | 19.3 | .40 | .038 |
| Sugary beverage consumption | .49 | .38 | .03 | .50 | .03 | .008 |
| 100% fruit juice consumption | .17 | .45 | .03 | .51 | .02 | .054 |
| Log fruit servings | .64 | .75 | .02 | .73 | .02 | .67 |
| Log vegetable servings | .92 | .64 | .02 | .59 | .02 | .12 |
| Water servings per dayd | ---e | 2.41 | .09 | 2.36 | .09 | .67 |
| Physical Activity Measures c | ---e | |||||
| Active time | ---e | 391.8 | 5.5 | 395.5 | 4.3 | .59 |
| Sedentary time | ---e | 382.9 | 5.7 | 376.6 | 5.8 | .43 |
| MVPA | ---e | 59.3 | 2.3 | 58.9 | 2.3 | .89 |
| Log days meeting PA guidelines | ---e | .89 | .07 | .88 | .07 | .97 |
| Group*Time Interaction |
Condition Main Effect: Intervention vs. Control |
|||
|---|---|---|---|---|
| Meeting Dietary Guidelinesb | p-value | OR | 95% CI | p-value |
| 100% fruit juice | .99 | 2.50 | 1.28, 4.89 | .007 |
| Fruit | .92 | .84 | .60, 1.17 | .30 |
| Vegetable | .82 | 1.52 | 1.07, 2.17 | .021 |
| Waterd | ----e | 1.05 | .67, 1.62 | .84 |
| Meeting PA Guidelines c | ||||
| MVPA | ----e | 1.38 | .67, 2.86 | .39 |
Mixed effects or generalized linear mixed models were used to adjust for the clustering effects of recreation centers for all outcomes, and repeated measures over time for outcomes measured at M2 and M3. Terms in all models (with the exception of water servings and physical activity measures) included the baseline level for the outcome variable (M1), time and condition main effects. For models with repeated measures, a condition by time interaction was also included. If the interaction term was not significant, the interaction was dropped from the model and a second model was fitted. The test for condition main effect is based on the second model.
All dietary outcome models were adjusted for caregiver ethnicity, acculturation, education and age, child gender, and BMI.
All physical activity outcome models were adjusted for time accelerometer was worn, child age, gender, and BMI. No adjustments were made for M1 due to the small sample size at M1.
For water servings per day, no adjustment was made for M1.
No interaction could be tested since only M3 measure was available.
Adjusted mean from mixed effects analysis.
MVPA= moderate and vigorous physical activity.
The results for meeting the dietary and PA guidelines are also shown in Table 4. The odds ratios are interpreted as the odds of meeting the guidelines by the intervention condition compared to the control condition. None of the group-by-time interactions were significant. The odds of meeting the fruit juice guidelines were significantly higher (p ≤ 0.01) in the intervention condition but both conditions reported high rates (>90%) of meeting the guidelines (data not shown). The intervention condition had greater odds of meeting the vegetable guidelines (p=0.02).
DISCUSSION
The MOVE/me Muevo intervention for preventing and controlling childhood obesity was implemented in thirty recreation centers within five cities throughout San Diego County, California (primarily in the city of San Diego). It involved activities at recreation centers and participants’ homes, telephone calls from health coaches, and mailings of simple tip sheets. No significant BMI or waist circumference differences between intervention and control conditions were found post-intervention. In a post-hoc examination of subgroup differences, the intervention did appear to have a salutary effect on limiting girls’ weight gain. Boys in the study’s intervention arm, however, trended toward relatively more weight gain and neutralized the overall main effect.
A variety of reasons may be posited for the overall null results. First, although the intervention lasted two years, the overall dose was limited (Table 1). Intervention activities did not reach their full pace until the second year, due to challenges reaching participants by telephone. Meanwhile, recreation centers were affected by a municipal, then a statewide economic downturn resulting in increased responsibilities of recreational staff, decreased staffing, and reduced hours and programs due to downsizing of municipal government. Moreover, many families did not patronize the recreation centers regularly. Parent and child attendance at the recreation center family workshops was imperfect (Table 1), and some parents did not complete the home-based activities. Novel strategies are needed for establishing and maintaining regular and reliable contact with participants to ensure intervention fidelity. Ensuring sufficient dose is essential for behavior change (40), although guidance on how much and at what frequency contact should occur is still relatively limited in childhood obesity prevention and control research (35). Based on the results of this study and on our experience in delivering this intervention, we recommend researchers enact better and more frequent tracking of intervention fidelity data in order to identify participants who may not be receiving the intended dose of intervention. The results suggest that the intervention dose may have been sufficient to reduce BMI among girls. Thus a greater dose and/or gender-tailored strategies may be needed to elicit reductions in BMI among boys. It is not possible from our data to tease out which intervention components may be more appropriate for boys and what additional level of dose may be needed to achieve favorable changes in BMI. This is an important area of research that needs further study.
Promising results were realized on two important fronts. First, key dietary changes were apparent for fat and sugary beverage (and to a lesser extent fruit juice) consumption, indicating that parents and children in the intervention group did take some of the recommended actions or were at least likely to have increased their awareness of these behaviors. Although these data cannot tell us why these particular behaviors appeared to change, it is possible that reducing fat and sugary beverage consumption are relatively easy behaviors for participating families to implement compared to the more complex, multidimensional behavior of physical activity (39). It is possible that the large and highly varied number of health messages was too much for participants to act on in such a short time period. Nonetheless, the literature suggests that obesity interventions targeting physical activity combined with nutrition are associated with significant improvements in BMI (41).
There was a positive direction of effect among girls, apparently offset by the boys’ results. The recent Cochrane review on interventions for preventing obesity in children found 19 studies examining gender differences in intervention effects, with eight studies finding no difference, four being more effective for boys, and seven being more effective for girls (35). This review, along with our results, seems to suggest that targeting interventions specifically for boys or girls and possibly other sub-groups of children is warranted. These findings also appear to highlight the importance of investigating moderators in interventions to inform future strategies.
It is possible that the heterogeneity of the population (various ethnicities, home languages, and baseline body weights ranging from normal weight to obese) ultimately posed too much of a challenge for the intervention. For example, a recent review showed that interventions targeting only overweight and obese children appear to be more effective than those targeting normal weight children (41). Anecdotally, some parents of apparently normal weight children, although generally motivated to see their child in a health promotion program, seemed puzzled about an attempt to prevent rather than treat obesity. Perhaps the converse was also the case: parents of obese children may have wondered why their children were mixed with normal weight kids given the topics of healthy body weight, nutrition and physical activity. Future studies should further examine how parents’ perceptions of their children’s weight status articulate with their motivation to be in an obesity-themed intervention.
In summary, the MOVE/me Muevo study, implemented in all neighborhoods of an economically and culturally diverse metropolitan area, had excellent participant retention over two years. Participants’ baseline weights as well as their ethnicities, and socioeconomic statuses ranged widely. Ironically, the study’s strength in terms of the generalizability of this population may have simultaneously proven to be its weakness as the intervention was not tailored to any one specific subgroup. Promising results in terms of healthy weight change among girls and trends toward healthier diets overall warrant further testing of the present intervention. Special attention may need to be paid, however, to tailoring the intervention to gender and ethnic groups and to baseline weight categories. The search for more effective programs for boys also seems especially warranted. This type of program may ultimately prove most effective by only including participants in more homogeneous categories.
What is already known about this subject?
Child overweight and obesity is a significant public health problem.
Mixed method approaches that involve parents and community organizations are promising approaches to prevent and control childhood obesity.
Few studies have targeted city recreation centers to promote healthy eating and physical activity behaviors.
What does this study add?
This study presents the primary results of a family- and recreation center-based childhood obesity prevention and control intervention.
The study was carried out in all neighborhoods of a socioeconomically diverse county of more than 1,000,000 inhabitants.
Primary results showed no significant reductions in child BMI; however secondary analyses showed that girls in the intervention condition reduced BMI significantly more than girls in the control condition.
Children in the intervention condition improved on several obesity-related behaviors compared to those in the control condition.
ACKNOWLEDGMENTS
We thank all the families and recreation centers who participated in this study and the study staff for their important contributions. This study was supported by the National Institutes of Health grant NIDDK R01DK072994. NCC was supported by grants T32HL079891 and F31KD079345. KC was supported by the Medical Research Council Epidemiology Unit [Unit Programme number U106179474] and the Centre for Diet and Activity Research (CEDAR), a UKCRC Public Health Research: Centre of Excellence. Funding from the British Heart Foundation, Economic and Social Research Council, Medical Research Council, the National Institute for Health Research, and the Wellcome Trust, under the auspices of the UK Clinical Research Collaboration, is gratefully acknowledged. All authors were involved in writing the paper and had final approval of the submitted and published versions. JP, NC, KC, JM, TM, NL and GA drafted the entire manuscript. DJ and NC carried out the data analyses.
Footnotes
CONFLICT OF INTEREST STATEMENT
The authors have no disclosures or conflict of interest to declare.
Contributor Information
John P. Elder, Institute for Behavioral and Community Health and Graduate School of Public Health at San Diego State University
Noe C. Crespo, School of Nutrition and Health Promotion, Arizona State University, Arizona
Kirsten Corder, MRC Epidemiology Unit, Cambridge, UK & Centre for Diet and Activity Research (CEDAR), Institute of Public Health, University of Cambridge, UK.
Guadalupe X. Ayala, Institute for Behavioral and Community Health and Graduate School of Public Health at San Diego State University
Donald J. Slymen, Institute for Behavioral and Community Health
Nanette V. Lopez, Institute for Behavioral and Community Health
Jamie S. Moody, Institute for Behavioral and Community Health
Thomas L. McKenzie, Institute for Behavioral and Community Health
REFERENCES
- 1.Flegal KM, Carroll MD, Ogden CL, Curtin LR. Prevalence and trends in obesity among US adults, 1999-2008. JAMA. 2010;303(3):235–241. doi: 10.1001/jama.2009.2014. [DOI] [PubMed] [Google Scholar]
- 2.Ogden CL, Lamb MM, Carroll MD, Flegal KM. Obesity and socioeconomic status in adults: United States 2005-2008. NCHS Data Brief. 2010;(50):1–8. [PubMed] [Google Scholar]
- 3.Reilly JJ, Kelly J. Long-term impact of overweight and obesity in childhood and adolescence on morbidity and premature mortality in adulthood: systematic review. Int J Obesity (London) 2011;35(7):891–898. doi: 10.1038/ijo.2010.222. [DOI] [PubMed] [Google Scholar]
- 4.Haemer M, Cluett S, Hassink SG, et al. Building capacity for childhood obesity prevention and treatment in the medical community: call to action. Pediatrics. 2011;128(Suppl 2):S71–77. doi: 10.1542/peds.2011-0480G. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hillier F, Pedley C, Summerbell C. Evidence base for primary prevention of obesity in children and adolescents. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2011;54(3):259–264. doi: 10.1007/s00103-010-1227-4. [DOI] [PubMed] [Google Scholar]
- 6.Campbell KJ, Hesketh KD. Strategies which aim to positively impact on weight, physical activity, diet and sedentary behaviours in children from zero to five years. A systematic review of the literature. Obes Rev. 2007;8(4):327–338. doi: 10.1111/j.1467-789X.2006.00305.x. [DOI] [PubMed] [Google Scholar]
- 7.Bartholomew KL, Parcel GS, Kok G, Gottlieb NH. Planning Health Promotion Programs. An Intervention Mapping Approach. Second edition Jossey-Bass; San Francisco: 2006. pp. 1–767. [Google Scholar]
- 8.Elder JP, Lytle L, Sallis JF, et al. A description of the social-ecological framework used in the trial of activity for adolescent girls (TAAG) Health Educ Res. 2007;22(2):155–165. doi: 10.1093/her/cyl059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Faith MS, Van Horn L, Appel LJ, et al. Evaluating parents and adult caregivers as “agents of change” for treating obese children: Evidence for parent behavior change strategies and research gaps: A scientific statement from the American Heart Association. Circulation. 2012;125(9):1186–1207. doi: 10.1161/CIR.0b013e31824607ee. [DOI] [PubMed] [Google Scholar]
- 10.Lopez NV, Ayala GX, Corder K, et al. Parent support and parent-mediated behaviors are associated with children’s sugary beverage consumption. J Acad Nutr Diet. 2012;12(4):541–547. doi: 10.1016/j.jand.2011.11.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Giles-Corti B, Kelty SF, Zubrick SR, Villanueva KP. Encouraging walking for transport and physical activity in children and adolescents: how important is the built environment? Sports Med. 2009;39(12):995–1009. doi: 10.2165/11319620-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 12.Grimm GC, Harnack L, Story M. Factors associated with soft drink consumption in school-aged children. J Am Diet Assoc. 2004;104(8):1244–1249. doi: 10.1016/j.jada.2004.05.206. [DOI] [PubMed] [Google Scholar]
- 13.Edwardson CL, Gorely T. Activity-related parenting practices and children’s objectively measured physical activity. Pediatr Exerc Sci. 2010;22(1):105–113. doi: 10.1123/pes.22.1.105. [DOI] [PubMed] [Google Scholar]
- 14.Arredondo EM, Elder JP, Ayala GX, Campbell N, Baquero B, Duerksen S. Is parenting style related to chidlren’s healthy eating and physical activity in Latino families? Health Educ Res. 2006;21(6):862–871. doi: 10.1093/her/cyl110. [DOI] [PubMed] [Google Scholar]
- 15.McKenzie TL, Baquero B, Crespo NC, Arredondo EM, Campbell NR, Elder JP. Environmental correlates of physical activity in Mexican American children at home. J Phys Act Health. 2008;5(4):579–591. doi: 10.1123/jpah.5.4.579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gubbels JS, Kremers SP, Stafleu A, et al. Association between parenting practices and children’s dietary intake, activity behavior and development of body mass index: the KOALA Birth Cohort Study. Int J Behav Nutr Phys Act. 2011;8:18. doi: 10.1186/1479-5868-8-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Davis MM, Gance-Cleveland B, Hassink S, Johnson R, Paradis G, Resnicow K. Recommendations for prevention of childhood obesity. Pediatrics. 2007;120(Suppl 4):S229–253. doi: 10.1542/peds.2007-2329E. [DOI] [PubMed] [Google Scholar]
- 18.Corder K, Sallis JF, Crespo NC, Elder JP. Active children use more locations for physical activity. Health Place. 2011;17(4):911–919. doi: 10.1016/j.healthplace.2011.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Moody JS, Prochaska JJ, Sallis JF, McKenzie TL, Brown M, Conway TL. Viability of parks and recreation centers as sites for youth physical activity promotion. Health Promot Pract. 2004;5(4):438–443. doi: 10.1177/1524839903258222. [DOI] [PubMed] [Google Scholar]
- 20.Kelly B, Baur LA, Bauman AE, King L, Chapman K, Smith BJ. Examining opportunities for promotion of healthy eating at children’s sports clubs. Aust N Z J Public Health. 2010;34(6):583–588. doi: 10.1111/j.1753-6405.2010.00619.x. [DOI] [PubMed] [Google Scholar]
- 21.Baker AD, Gilley J, James J, Kimani M. High Five to Healthy Living”: A Health Intervention Program for Youth at an Inner City Community Center. J Community Health. 2012;37(1):1–9. doi: 10.1007/s10900-011-9387-1. [DOI] [PubMed] [Google Scholar]
- 22.PRB staff World Population Highlights: Key Findings From PRB’ 2009 World Population Data Sheet. Population Bulletin. 2009;64(3) [Google Scholar]
- 23.Cliff DP, Reilly JJ, Okely AD. Methodological considerations in using accelerometers to assess habitual physical activity in children aged 0-5 years. J Sci Med Sport. 2009;12(5):557–567. doi: 10.1016/j.jsams.2008.10.008. [DOI] [PubMed] [Google Scholar]
- 24.Penpraze V, Reilly JJ, MacLean C, et al. Monitoring of Physical Activity in Young Children: How Much Is Enough? Ped Exerc Sci. 2006;18(4):483–491. doi: 10.1123/pes.18.4.483. [DOI] [PubMed] [Google Scholar]
- 25.Freedson PS, Melanson E, Sirard J. Calibration of the Computer Science and Applications, Inc. accelerometer. Med Sci Sports Exerc. 1998;30(5):777–781. doi: 10.1097/00005768-199805000-00021. [DOI] [PubMed] [Google Scholar]
- 26.Trost SG, McIver KL, Pate RR. Conducting Accelerometer-Based Activity Assessments in Field-Based Research. Med Sci Sports Exerc. 2005;37(11):531–543. doi: 10.1249/01.mss.0000185657.86065.98. [DOI] [PubMed] [Google Scholar]
- 27.Treuth M, Schmitz K, Catellier DJ, et al. Defining accelerometer thresholds for activity intensities in adolescent girls. Med Sci Sports Exerc. 2004;36(7):1259–1266. [PMC free article] [PubMed] [Google Scholar]
- 28.Marin G, Sabogal F, VanOss Marin B, Otero-Sabogal R, Perez-Stable EJ. Development of a short acculturation scale for Hispanics. Hisp J Behav Sci. 1987;9(2):183–205. [Google Scholar]
- 29.Prochaska JJ, Sallis JF, Rupp J. Screening measure for assessing dietary fat intake among adolescents. Prev Med. 2001;33(6):699–706. doi: 10.1006/pmed.2001.0951. [DOI] [PubMed] [Google Scholar]
- 30.Rockett HRH, Breitenbach M, Frazier AL, et al. Validation of a youth/adolescent food frequency questionnaire. Prev Med. 1997;26(6):808–816. doi: 10.1006/pmed.1997.0200. [DOI] [PubMed] [Google Scholar]
- 31.Committee on Nutrition The use and misuse of fruit juice in pediatrics. Pediatrics. 2001;107(5):1210–1213. doi: 10.1542/peds.107.5.1210. [DOI] [PubMed] [Google Scholar]
- 32.Prochaska JJ, Sallis JF. Reliability and validity of a fruit and vegetable screening measure for adolescents. J Adolesc Health. 2004;34(4):163–165. doi: 10.1016/j.jadohealth.2003.07.001. [DOI] [PubMed] [Google Scholar]
- 33.Gidding SS, Dennison BA, Birch LL, et al. Dietary recommendations for children and adolescents: A guide for practitioners. Pediatrics. 2006;117:544–559. doi: 10.1542/peds.2005-2374. [DOI] [PubMed] [Google Scholar]
- 34.Ballauff A, Kersting M, Manz F. Do children have an adequate fluid intake? Water balance studies carried out at home. Ann Nutr Metab. 1988;32:332–339. doi: 10.1159/000177483. [DOI] [PubMed] [Google Scholar]
- 35.Waters E, de Silva-Sanigorski A, Hall BJ, et al. Interventions for preventing obesity in children. Cochrane Database Syst Rev. 2011;7(12):CD001871. doi: 10.1002/14651858.CD001871.pub3. [DOI] [PubMed] [Google Scholar]
- 36.Donner A, Klar A. Design and Analysis of Cluster Randomization Trials in Health Research. Arnold; London: 2000. pp. 1–192. [Google Scholar]
- 37.Eisenberg CM, Ayala GX, Crespo NC, et al. Examining multiple parenting behaviors on young children’s dietary fat consumption. J Nutr Educ Behav. 2012;44(4):302–309. doi: 10.1016/j.jneb.2011.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Corder K, Crespo NC, van Sluijs EM, et al. Predictors of change in sports participation in Latino and non-Latino children. Br J Sports Med. 2011 Sep 7; doi: 10.1136/bjsports-2011-090105. epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Corder K, van Sluijs EM, McMinn AM, Ekelund U, Cassidy A, Griffin SJ. Perception versus reality awareness of physical activity levels of British children. Am J Prev Med. 2010;38(1):1–8. doi: 10.1016/j.amepre.2009.08.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Bellg AJ, Borrelli B, Resnick B, et al. Enhancing treatment fidelity in health behavior change studies: Best practices and recommendations From the NIH Behavior Change Consortium. Health Psychol. 2004;23(5):443–451. doi: 10.1037/0278-6133.23.5.443. [DOI] [PubMed] [Google Scholar]
- 41.Lavelle HV, Mackay DF, Pell JP. Systematic review and meta-analysis of school-based interventions to reduce body mass index. J Public Health (Oxf) 2012 Jan 20; doi: 10.1093/pubmed/fdr116. Epub ahead of print. [DOI] [PubMed] [Google Scholar]