Abstract
Background
The forehead, which occupies about one third of the face, is one of the major determinants of a feminine or masculine look. Various methods have been used for the augmentation of the forehead using autologous fat grafts or alloplastic materials. Methylmethacrylate (MMA) is the most appropriate material for augmentation of the forehead, and we have used an injection-molding technique with MMA to achieve satisfactory results.
Methods
Under local anesthesia with intravenous (IV) sedation, an incision was made on the scalp and a meticulous and delicate subperiosteal dissection was then performed. MMA monomers and polymers were mixed, the dough was injected into the space created, and manual molding was performed along with direct inspection. This surgery was indicated for patients who wanted to correct an unattractive appearance by forehead augmentation. Every patient in this study visited our clinics 3 months after surgery to evaluate the results. We judged the postoperative results in terms of re-operation rates caused by the dissatisfaction of the patients and complications.
Results
During a 13-year period, 516 patients underwent forehead augmentation with MMA. With the injection-molding technique, the inner surface of the MMA implant is positioned close to the underlying frontal bone, which minimizes the gap between the implant and bone. The borders of the implant should be tapered sufficiently until no longer palpable or visible. Only 28 patients (5.4%) underwent a re-operation due to an undesirable postoperative appearance.
Conclusions
The injection-molding technique using MMA is a simple, safe, and ideal method for the augmentation of the forehead.
Keywords: Forehead; Methylmethacrylate; Surgery, plastic
INTRODUCTION
The demand for aesthetic forehead contouring surgery has been increasing steadily over the past few years because the forehead, which occupies about one third of the face, is one of the major determinants of a feminine or masculine look. People consider a broad, convex, and smoothly shaped forehead to appear more feminine and attractive than a flat or sunken one [1]. Accordingly, a number of methods have been developed for forehead contouring surgery. Forehead augmentation methods can be categorized as soft tissue augmentation and skeletal augmentation. In our opinion, soft tissue augmentation is a temporary solution while skeletal augmentation gives long-term results.
Skeletal augmentation can be defined as forehead augmentation with alloplastic materials such as silicone, bone cement, and expanded polytetrafluoroethylene. Ideal implants for facial skeletal augmentation have some prerequisites: 1) The rigidity of the implant should be similar to bone, so that the external surface of the augmented forehead can mimic the shape of the bone; 2) the inner surface of the implant should be able to fit closely to the bone to minimize dead space between the implant and bone; 3) the edges of the implant should be tapered so that they are not visible or palpable; and 4) immobilization of the implant should be ensured. We have been using Methylmethacrylate (MMA) as an implant for augmentation of the forehead because it has many favorable characteristics: MMA is non-allergenic, non-thermoconductive, inexpensive, induces minimal inflammatory reactions, and gives a predictable resultant shape [2]. We have developed an injection-molding technique with MMA that is a single stage procedure for forehead contouring surgery. Our patients show satisfactory outcomes with the MMA injection-molding technique on long-term follow-up.
METHODS
Patients
A total of 547 patients underwent aesthetic augmentation of the forehead with MMA between January 1999 and December 2011. Thirty-one of the 547 patients were excluded from this study because they did not visit our clinics 3 months after surgery for a postoperative evaluation. This study was conducted retrospectively by reviewing medical records and clinical photographs. There were 45 male and 471 female patients ranging in age from 21 to 62 years, with a mean age of 29 years. In this study, 480 patients (93.0%) underwent primary augmentation and 36 patients (7.0%) underwent secondary augmentation. Of the 36 patients with secondary augmentation, 21 had undergone ugmentation of the forehead with silicone implants, 11 patients with autologous fat, and 4 patients with a filler.
Procedures
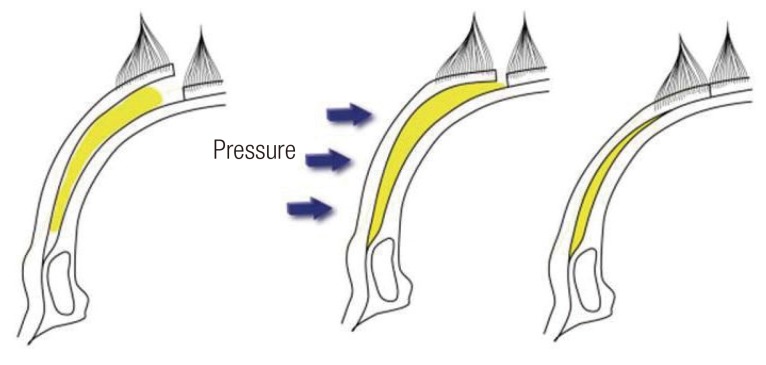
Surgery was performed on all of the patients under conscious sedation with intravenous sedatives (mixed solution of 0.5 mL ketamine hydrochloride and 0.5 mL midazolam). A 4 to 5 cm, slightly curved linear incisional line was drawn in the scalp, 4 to 6 cm behind the anterior hairline. The location of the incision was determined according to the preoperative shape of the forehead of each patient. A local anesthetic (1% lidocaine mixed with 1:100,000 epinephrine) was infiltrated along the planned dissection area and both supraorbital ridges to block the supratrochlear and supraorbital nerves. After the incision reached the level of the periosteum, a subperiosteal dissection was carefully made inferiorly to the level of the superior orbital rim and laterally to the temporal ridge, taking care not to tear the periosteum or cross over the temporal fusion line (Fig. 1).
Fig. 1.
Dissection area for onlay implant
Dissection was carried out inferiorly to the superior orbital rim and laterally to the temporal fusion line (green line).
The 20 mL of MMA monomer liquid and 40 g of polymer powder were mixed in a bowl to form a slightly sticky dough. It took about 2 to 3 minutes to form suitable dough at room temperature (about 20℃). Once the dough was in a suitable state for injection, it was injected into the dissected space (Fig. 2). Injection of the MMA was done with a custom-made syringe by cutting the tip of a standard 50-mL syringe to pour it smoothly. It was then manually molded through the skin, with frequent direct inspection, in every direction to produce the preoperatively determined shape of the forehead (Figs. 3, 4). Generally speaking, 1/3-2/3 of the total mixture was used, but the exact amount of injected MMA was determined during the operation. While the injected dough cured, it was irrigated with saline to prevent possible thermal injury by exothermic reactions. No additional manipulation of the periosteum such as a hatching incision was needed because we did not use a large enough volume of MMA to require handling of the periosteum.
Fig. 2.
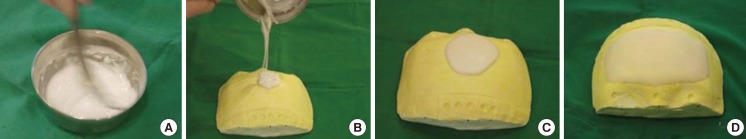
Mixing the methyl methacrylate polymer powder
(A) Mixing of Methylmethacrylate powder and liquid in a bowl. (B) Formation of a sticky dough for injection. (C) Before molding of the injected dough. (D) After molding of the injected dough.
Fig. 3.
Manual molding of methyl methacrylate dough
Fig. 4.
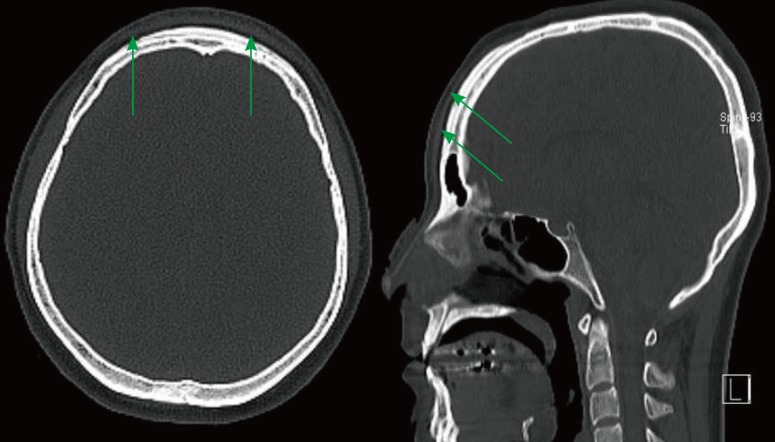
Postoperative computed tomography (axial and sagittal) views
Green arrows indicate the methyl methacrylate implant on the frontal bone.
After irrigation, the incision was repaired with skin staples. No drain or hemo-vac was applied. A mild compressive dressing was applied, along with an elastic bandage. The dressing was removed on the third postoperative day, and the skin staples were removed on the seventh postoperative day.
RESULTS
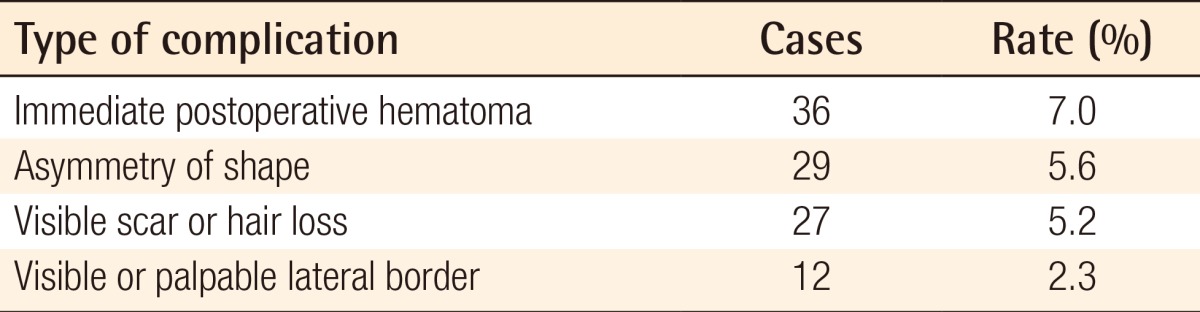
Almost all of the patients were subjectively satisfied with their postoperative appearance. Generally, we evaluated the postoperative appearance 3 months after surgery (Figs. 5, 6). No major complications were encountered, such as infection, prolonged postoperative headache, delayed hematoma, or seroma. Minor complications, such as immediate postoperative hematoma, visible or palpable lateral border, asymmetry of shape, visible scars, or hair loss were also rare (Table 1). Most patients who suffered and complained of minor complications accepted the results of their surgery because the minor complications had little effect on the overall postoperative appearance. Meanwhile, most patients who were discontented with the postoperative appearance due to a visible or palpable border wanted a reoperation.
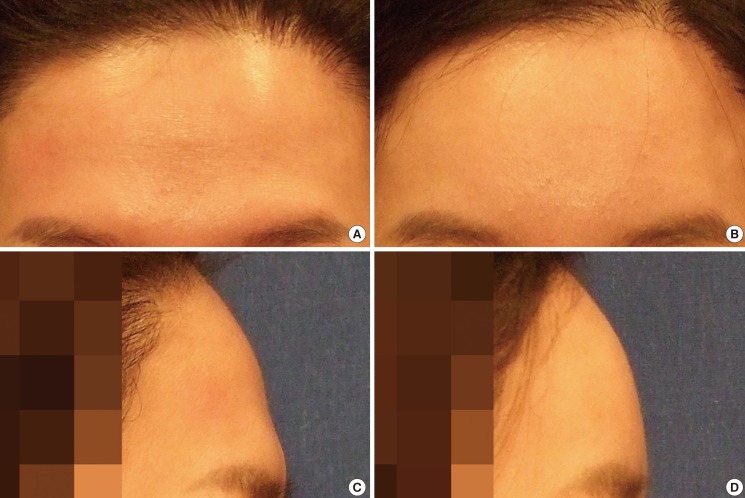
Fig. 5.
A 28-year-old female with a prominent brow
Supraorbital bossing of the preoperative appearance was corrected.
Fig. 6.
A 28-year-old female with a flat forehead
After augmentation, the patient had a round-shaped forehead with an obtuse angle.
Table 1.
Minor complications of the surgery
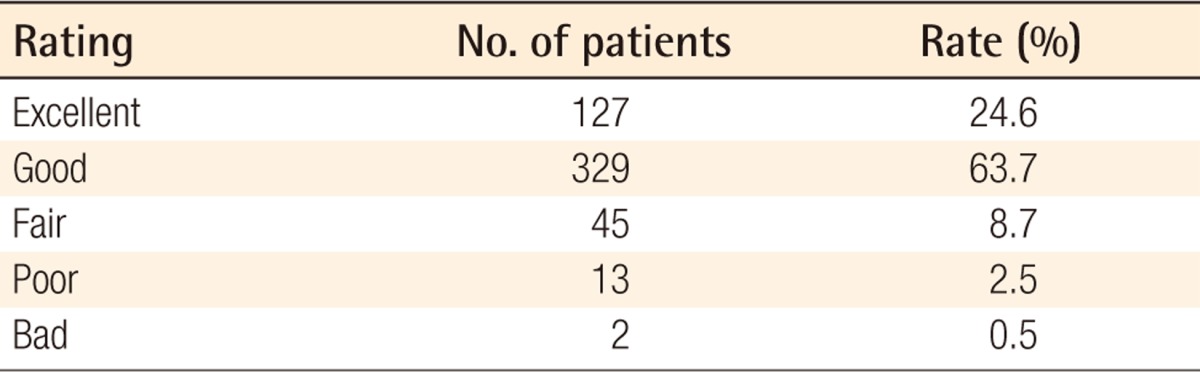
All of the patients who visited our clinics 3 months after surgery were interviewed to evaluate their satisfaction with their postoperative appearance (Table 2). Only a small number of patients (60 patients) were not satisfied with the results, and among them, some wanted to undergo revision surgery. However, an objective evaluation of postoperative results executed for purely aesthetic purposes is not sufficient because the subjective satisfaction of the patient overwhelms the other objective evaluations. In this study, an evaluation that maximally reflected the subjective judgment of the patient was also obtained by evaluating the postoperative results in terms of the rate of reoperation caused by patient dissatisfaction and complications, rather than by simply assessing the degree of patient satisfaction.
Table 2.
Patients' satisfaction rating
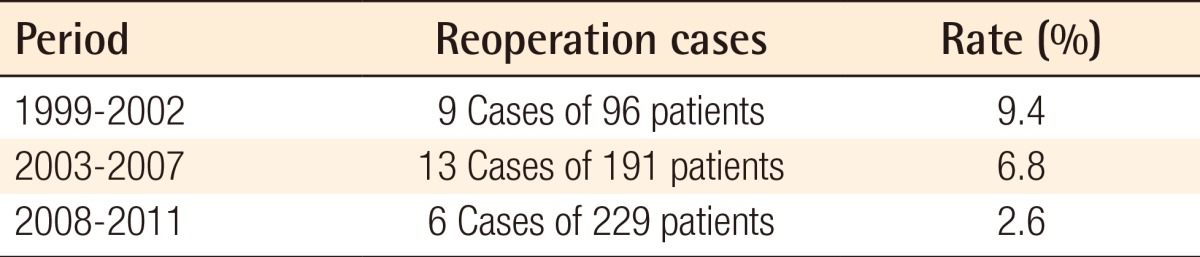
In total, 28 (5.4%) of the 516 patients underwent a reoperation due to an undesirable postoperative appearance; 10 patients (1.9%) underwent a reoperation due to visible or palpable lateral borders, and 18 patients (3.5%) underwent a reoperation due to dissatisfaction with the degree of augmentation (over-augmentation [15 patients] and under-augmentation [3 patients]). During our 13 years of experience in forehead augmentation, we have modified our operation technique twice. Since 2003, we have used a modified periosteal elevator to enable a more meticulous dissection to avoid injuring the periosteum. At 2008, we modified our technique of local anesthesia infiltration because we recognized that anesthetic injection around the temporal ridge obscured the boundary. Therefore, we divided the entire period into three stages, and the re-operation rates are shown (Table 3). The rate decreased to 2.6% in the period of 2008-2011 from 9.4% in the period of 1999-2002. The reoperation rates decrease over time.
Table 3.
Reoperation rate
In our opinion, patients tend to consider an over-augmented shape as more unacceptable compared to an under-augmented shape. Hence, this should be kept in mind during the preoperative interview with the patient. The frequency of visible or palpable borders could be decreased by fine-tuning operative techniques. Some immediate postoperative hematoma occurred, but no recurrence occurred after aspiration. Seroma, which is commonly associated with augmentation using silicone implants, did not occur in our patients.
DISCUSSION
MMA was developed in 1939 and first used by Kleinschmidt in 1940. It still is the most frequently used alloplastic material in orthopedic and neurosurgery and is considered the best choice for skull reconstruction worldwide [3]. Gonzalez Ulloa and Stevens [4] first described the use of MMA for forehead contouring in 1964, and it is now recognized as a useful implant material for augmentations [5].
MMA is a cost-effective, strong material that has a similar density to that of cranial bone. It is inert, with minimal inflammatory reactions, and is non-thermoconductive. The resultant shape is predictable, and it can be managed perioperatively. Furthermore, fine adjustment of an MMA implant can be made by adding additional MMA or by contouring with a burr. MMA has the characteristics of a lack of tissue ingrowth and minimal adherence to bone. These characteristics also make MMA easy to remove when patients want to do so.
Various methods for forehead contouring surgery have been described in the literature [4,6-8]. Silicone is one of the most widely used implant materials for skeletal augmentation of the forehead. Most surgeons who have used silicone implants have usually fabricated patient-specific tailored implants. Accurate molding of silicone to exactly fit the patient's forehead contour is very difficult, so gaps between the existing forehead and the implant are inevitable. If the patient has a thin skin texture, the borders of the silicone implant can be identified by inspection or palpation.
Fat injection or autologous fat grafting for facial contouring is one of most frequently used methods because it is easy and is a relatively minor invasive procedure. However, it has the critical pitfalls of unpredictable resorption over time and the risk of uneven distribution of fat throughout the area that the surgeon wants to modify [9]. Goretex implants have a problem with volume shrinkage over time.
Autologous bone grafts are not a choice for forehead augmentation because such a large amount of bone is required that it would leave the donor site with inevitable morbidity. This method is also prone to unavoidable and unpredictable resorption of the graft [10].
Compared with augmentation with silicone implants, augmentation with MMA implants can create an implant that more closely fits with the underlying bone. It can be done as a single-stage procedure with perioperative molding. The injection-molding technique using MMA makes possible more delicate molding to the bone, so the gap between the existing bone and the implant can be minimized.
Any space that remains between the bone and implant can cause unsatisfactory surgical results for two reasons. The gap can result in over-augmentation beyond the desired previously determined shape and can also be a potential space for the formation of hematomas and seromas. Compared with autologous fat grafts, the MMA injection procedure has many advantages. Above all, there is the advantage of reliable long-term results.
No major complications such as infection, headache, or delayed hematoma or seroma occurred in our patients. In our opinion, the subperiosteal dissection should not cross over the temporal fusion line and any irritation to the temporalis muscle should be avoided during the dissection in order to prevent postoperative headaches.
The implant formed by the MMA injection-molding technique has many advantages over other methods of forehead augmentation: 1) Unlike silicone implants, there is no need for a preoperative molding of the implant; 2) A minimal gap to none at all forms between the implant and the underlying bone, which can prevent postoperative hematoma, seroma, and displacement of the implant; 3) MMA has a physical similarity to bone, so the patient may feel less of a foreign body sensation in the forehead; and 4) the surgeon can adjust contouring during the operation. However, this technique should be conducted by an experienced surgeon because the process from the formation of the relevant dough to the molding before complete curing is the key procedure and is highly dependent on the surgeon's skill.
Based on our experience from the past 13 years, we suggest several tips for achieving satisfactory results in this surgery: 1) The surgeon should not injure the periosteum during the dissection and curing. Delicate and meticulous subperiosteal dissection is essential. If there is a tear in the periosteum, surface irregularity inevitably develops. Therefore, manipulation of periosteum is forbidden rather than not required. 2) The surgeon should not cross over the zone of fixation. 3) The surgeon should not augment too much. Generally, most patients tend not to accept the artificial appearance caused by over-augmentation. Hence, a preoperative interview with the patient is important. Usually, we show the patient preoperative and postoperative photographs of other patients who have undergone forehead augmentation so that they can anticipate their postoperative appearance. Finally, 4) the operator should try to conserve the hair follicles. We use a beveled incision to minimize alopecia and scar width.
We have encountered 28 cases of re-operation, which can be categorized into three groups; visible/palpable border, under-augmentation, and over-augmentation. The visible or palpable border was corrected by rasping the protruding border. If the patients felt that the primary surgery resulted in an under-augmentation or an unnatural appearance due to over-augmentation, it was corrected by removal of the previously injected implant and conducting a secondary augmentation.
In our opinion, skeletal augmentation of the forehead is an appropriate method for facial contouring surgery. MMA is one of the most ideal alloplastic implant materials for forehead reconstruction. We have developed an injection-molding technique for better results in augmentation surgery without complications. During the past 13 years, many patients have undergone forehead augmentation and most patients were satisfied. According to our surgical results, the injection-molding technique using MMA is a reliable, effective, and safe method of forehead augmentation.
Footnotes
This article was presented at the 4th World Congress of Minimally Invasive Plastic Surgery on September 1, 2012 in Seoul, Korea.
No potential conflict of interest relevant to this article was reported.
References
- 1.Altman K. Facial feminization surgery: current state of the art. Int J Oral Maxillofac Surg. 2012;41:885–894. doi: 10.1016/j.ijom.2012.04.024. [DOI] [PubMed] [Google Scholar]
- 2.Blum KS, Schneider SJ, Rosenthal AD. Methyl methacrylate cranioplasty in children: long-term results. Pediatr Neurosurg. 1997;26:33–35. doi: 10.1159/000121158. [DOI] [PubMed] [Google Scholar]
- 3.Gosain AK, Persing JA. Biomaterials in the face: benefits and risks. J Craniofac Surg. 1999;10:404–414. doi: 10.1097/00001665-199909000-00006. [DOI] [PubMed] [Google Scholar]
- 4.Gonzalez Ulloa M, Stevens E. Implants in the face; a review of our experience in the subcutaneous use of methylmethacrylate. Plast Reconstr Surg. 1964;33:532–542. [PubMed] [Google Scholar]
- 5.Seo JD, You YJ, Ko RY, et al. Forehead augmentation with methylmethacrylate. J Korean Soc Aesthetic Plast Surg. 2001;7:135–139. [Google Scholar]
- 6.Kang JH, Jung SW, Lee YH, et al. Contouring of forehead and temple area with auto-fat injection. J Korean Soc Plast Reconstr Surg. 2011;38:166–172. [Google Scholar]
- 7.Kim CY, Lee KM, Hong SE. Forehead and temporal augmentation with medium porosity and high density ePTFE. J Korean Soc Aesthetic Plast Surg. 2009;15:218–223. [Google Scholar]
- 8.Park CS, Hyon WS, Park YJ, et al. Correction of facial depression using precisely-shaped silicone implants. J Korean Soc Plast Reconstr Surg. 2000;27:87–91. [Google Scholar]
- 9.Kim SB, Kim DW, Yoon ES. Facial fat injection: long-term follow-up results. J Korean Soc Aesthetic Plast Surg. 2010;16:35–40. [Google Scholar]
- 10.Moreira-Gonzalez A, Jackson IT, Miyawaki T, et al. Clinical outcome in cranioplasty: critical review in long-term followup. J Craniofac Surg. 2003;14:144–153. doi: 10.1097/00001665-200303000-00003. [DOI] [PubMed] [Google Scholar]