The McIndoe operation is a widely performed surgical procedure for neovaginal reconstruction [1]. It creates a neovaginal cavity by dissecting between the bladder and rectum, and grafts skin to resurface a surgically created neovagina. A space-occupying vaginal mold is required to maintain the skin graft. An unsuitable vaginal mold could result in poor drainage, graft maceration, graft sloughing, and graft detachment, which could lead to an unsatisfactory reconstruction. Using the appropriate vaginal mold is important for achieving successful results in McIndoe neovaginal reconstruction [1].
In this report, we introduce a silicone gel sheet (Cica-Care, Smith and Nephew, Hull, UK) vaginal mold. Silicone gel sheets are produced in sterile packaging and commonly available in most hospitals. This method is cost and time efficient, easily reproducible, convenient, and causes less discomfort to patients, while it enhances excellent integration of the graft.
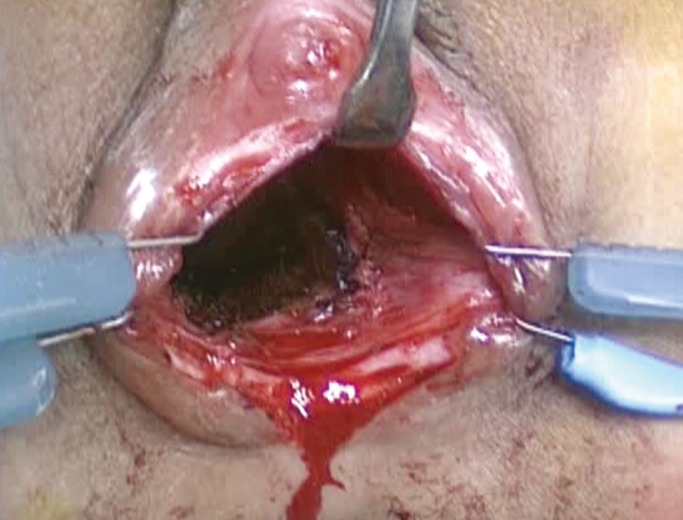
A 13-year-old female patient with congenital vaginal agenesis of the distal two-thirds was referred to our department for vaginal reconstruction. Under general anesthesia, a neovagina was constructed by a gynecological surgeon through blunt dissection between the urethra and rectum, as in a standard McIndoe vaginoplasty. The raw surface of the neovagina was 6 cm in depth and 3 cm in diameter (Fig. 1).
Fig. 1.
Preoperative view of the fabricated neovagina. A gynecological surgeon created a neovagina with a raw surface about 6 cm in depth and 2.5 to 3.0 cm in diameter.
Before the reconstruction, we made a vaginal mold using an adhesive silicone gel sheet (Cica-Care, Smith and Nephew) and a 16 French Foley urinary catheter. A 15 cm×12 cm silicone gel sheet was divided in half to make two strips to wrap around the foley catheter. Due to the adhesiveness of the silicone gel sheet, no further anchoring or bandaging was required. Histoacryl (B. Braun Dexon GmbH, Spangenberg, Germany) was applied along the Foley catheter for the initial and final adhesion with the silicone gel sheet, making the interlamellar space water-tight so as to prevent unwanted debris collection. The completed silicone vaginal mold was 6.5 cm in length and 2.5 cm in diameter, which could expand up to 3.0 cm after ballooning of the Foley catheter (Supplemental Video S1).
To reconstruct the raw surface of the neovagina, a 10 cm×7 cm split-thickness skin graft (STSG) with a thickness of 0.012 inches was harvested from her left inner thigh using a pneumatic dermatome and wrapped around the vaginal mold with the skin surface facing the vaginal mold. The inner thigh was chosen for its accessibility in the lithotomy position. A Foley catheter was then inflated with about 3 to 5 mL of saline to form a fusiform mold, and the margins of the graft were sutured with 4-0 chromic sutures. To prevent inversion or accidental detachment of the graft during insertion, the distal margin of the graft at the Foley catheter tip was also loosely approximated with suturing. After the catheter balloon was deflated, the vaginal mold wrapped with STSG was carefully inserted into the neovagina through the speculum. The Foley catheter balloon was inflated again, widening the diameter of the vaginal stent near the cervix. This wedge transformation prohibits the spontaneous ejection of the splint, but still keeps pressure low near the vaginal orifice, reducing discomfort despite the sphincter action of the vagina. The proximal free margin of the graft was sutured to the vaginal orifice using 4-0 chromic sutures. The labia majora was sutured in the midline with interrupted 3-0 Vicryl sutures to prevent unintended displacement of the vaginal mold.
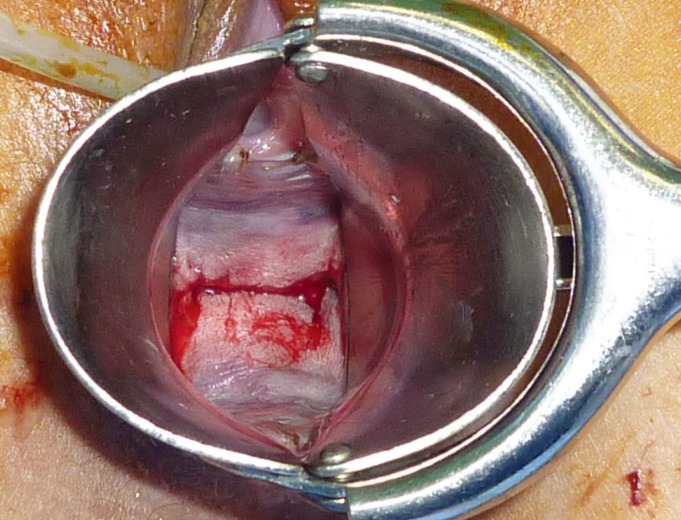
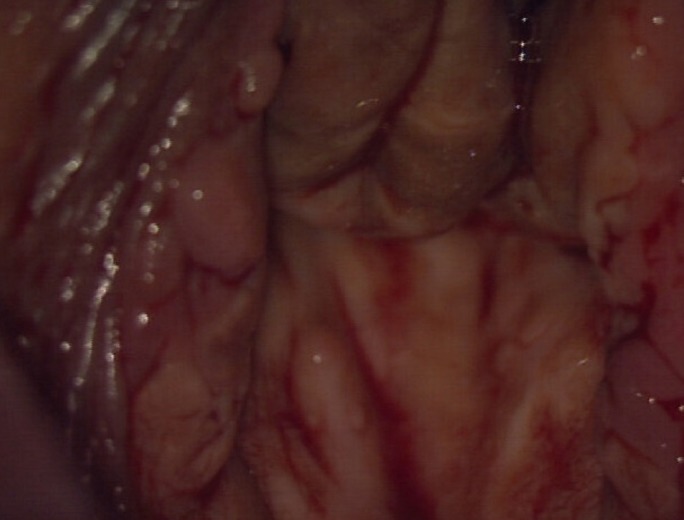
Five days after the operation, the vaginal mold could be removed smoothly without any difficulty after deflation of the catheter (Fig. 2). The vaginal mold was reused as a postoperative vaginal stent to prevent contracture of the canal for 6 to 10 months. It was reinserted with a lubricated condom. On the 12th postoperative day, the skin grafts had taken without any complications, and the patient was discharged with the vaginal stent inserted (Fig. 3). After 18 months, the neovagina was found to be satisfactorily reconstructed (Fig. 4). The patient is having regular menstrual cycles and receiving no hormonal therapy. In follow-up visits at an outpatient clinic, the size of the silicone vaginal stent was reduced due to some pain experienced when changing the stent.
Fig. 2.
Five days after the operation. The graft had taken. The vaginal mold was reused as a postoperative vaginal stent.
Fig. 3.
Six months after the operation. The patient used the vaginal stent to prevent contracture of the canal for 6 to 10 months.
Fig. 4.
Eighteen months after the operation. The neovagina was well reconstructed.
A skin graft is a simple method that can reconstruct vaginal wall defects. Various materials, such as hollow vulcanite wood, a condom packed with iodoform gauze, Surgi-Stuf (Ethox, Buffalo, NY, USA) [2], Orfit "S" material (Wijnegem, Belgium) [3], a silicone-coated acrylic vaginal stent, inflatable vaginal stents [4], a solid plastic mold, a detachable porous plastic tube, and a perforated Pyrex glass mold [5], have been recommended as vaginal molds that could ensure graft immobilization.
Rigid or semi-rigid molds tend to develop several complications, such as graft loss, pressure-related bladder or rectum perforations, fibrosis, contracture formation, and most importantly, patient discomfort [2]. On the other hand, soft molds have less association with the above mentioned complications, but other drawbacks exist, including instability, complexity of assembly, and lack of commercial availability.
In this report, we used Cica-Care as the key material. It is a self-adhesive silicone gel sheet with a soft gel-like consistency, which provides ultimate comfort and wide applicability to uneven three-dimensional defects. The length and diameter of the mold can be easily adjusted by cutting the silicone gel sheet to the desired length or by changing the number of wrappings around the Foley catheter according to the patient's age and size of the vaginal raw surface. Moreover, the long-term durability of the silicone gel sheet makes it reusable as a postoperative dilator, which may be a benefit in terms of reducing hypertrophic scar formation or contracture. The product itself is provided in a sterile package and manufactured to withstand repetitive sterilization.
For patients receiving McIndoe vaginoplasty with skin grafting, a vaginal mold using a silicone gel sheet can be applied to ensure graft take and prevent vaginal stenosis from hypertrophic scar formation. This technique is simple, easily reproducible, diversely adjustable, cost-effective, and less time-consuming, with minimal discomfort for the patient. We also recommend using this vaginal mold for the postoperative management of McIndoe vaginoplasty patients. Successful McIndoe neovaginal reconstruction was achieved using a silicone gel sheet vaginal mold. This vaginal mold was not only used during the immediate postoperative period, but it was also used for stenting in postoperative management.
Footnotes
This article contains supplemental Video S1.
This research was supported by Seoul St. Mary's Clinical Medicine Research Program (2011) through The Catholic University of Korea.
No potential conflict of interest relevant to this article was reported.
Supplemental Video S1.
Vaginal mold made with silicone gel sheet. A vaginal mold was made with an adhesive silicone gel sheet and 16 French Foley urinary catheter.
Supplemental data can be found at: http://e-aps.org/src/sm/aps-40-652-s001.avi
References
- 1.McIndoe A. The treatment of congenital absence and obliterative conditions of the vagina. Br J Plast Surg. 1950;2:254–267. [PubMed] [Google Scholar]
- 2.Concannon MJ, Croll GH, Puckett CL. An intraoperative stent for McIndoe vaginal construction. Plast Reconstr Surg. 1993;91:367–368. doi: 10.1097/00006534-199302000-00027. [DOI] [PubMed] [Google Scholar]
- 3.Chen TH. Refinement of McIndoe's vaginal reconstruction with ORFIT "S" vaginal stent. Plast Reconstr Surg. 1994;94:394–396. doi: 10.1097/00006534-199408000-00030. [DOI] [PubMed] [Google Scholar]
- 4.Sabino Neto M, Baracat EC, Ferreira LM. Vaginal reconstruction by McIndoe technique with a vaginal expander mold. Int J Gynaecol Obstet. 2001;73:165–167. doi: 10.1016/s0020-7292(00)00333-7. [DOI] [PubMed] [Google Scholar]
- 5.Ozek C, Gurler T, Alper M, et al. Modified McIndoe procedure for vaginal agenesis. Ann Plast Surg. 1999;43:393–396. doi: 10.1097/00000637-199910000-00009. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Vaginal mold made with silicone gel sheet. A vaginal mold was made with an adhesive silicone gel sheet and 16 French Foley urinary catheter.
Supplemental data can be found at: http://e-aps.org/src/sm/aps-40-652-s001.avi