ABSTRACT
BACKGROUND
Recent clinical trials of male circumcision, oral pre-exposure prophylaxis (PrEP), and a vaginal microbicide gel have shown partial effectiveness at reducing HIV transmission, stimulating interest in implementing portfolios of biomedical prevention programs.
OBJECTIVE
To evaluate the effectiveness and cost-effectiveness of combination biomedical HIV prevention and treatment scale-up in South Africa, given uncertainty in program effectiveness.
DESIGN
Dynamic HIV transmission and disease progression model with Monte Carlo simulation and cost-effectiveness analysis.
PARTICIPANTS
Men and women aged 15 to 49 years in South Africa.
INTERVENTIONS
HIV screening and counseling, antiretroviral therapy (ART), male circumcision, PrEP, microbicide, and select combinations.
MAIN MEASURES
HIV incidence, prevalence, discounted costs, discounted quality-adjusted life years (QALYs), and incremental cost-effectiveness ratios.
KEY RESULTS
Providing half of all uninfected persons with PrEP averts 28 % of future HIV infections for $9,000/QALY gained, but the affordability of such a program is questionable. Given limited resources, annual HIV screening and ART utilization by 75 % of eligible infected persons could avert one-third of new HIV infections, for approximately $1,000/QALY gained. Male circumcision is more cost-effective, but disproportionately benefits men. A comprehensive portfolio of expanded screening, ART, male circumcision, microbicides, and PrEP could avert 62 % of new HIV infections, reducing HIV prevalence from a projected 14 % to 10 % after 10 years. This strategy doubles treatment initiation and adds 31 million QALYs to the population. Despite uncertainty in program effectiveness, a comprehensive portfolio costs less than $10,000/QALY gained in 33 % of simulation iterations and less than $30,000/QALY gained in 90 % of iterations, assuming an annual microbicide cost of $100.
CONCLUSIONS
A portfolio of modestly-effective biomedical HIV prevention programs, including male circumcision, vaginal microbicides, and oral PrEP, could substantially reduce HIV incidence and prevalence in South Africa and be likely cost-effective. Given limited resources, PrEP is the least cost-effective intervention of those considered.
Electronic supplementary material
The online version of this article (doi:10.1007/s11606-013-2417-1) contains supplementary material, which is available to authorized users.
KEY WORDS: HIV epidemic, mathematical model, simulation, cost-effectiveness analysis, combination HIV prevention
INTRODUCTION
HIV/AIDS accounts for 12 % of deaths worldwide among individuals aged 15 to 49—the leading cause of death in women and third-leading cause in men—with the disease continuing to afflict many resource-limited countries.1–3 With 5.6 million people living with HIV, or 19 % of the adult population, South Africa is home to the largest HIV epidemic in the world.4 Despite progress in scaling up access to antiretroviral therapy (ART), approximately 60 % of those in need of treatment in South Africa do not receive it, based on 2010 World Health Organization (WHO) guidelines.4 Global HIV resources available amounted to $16 billion in 2010, far short of the estimated $22–24 billion needed in low-income and middle-income countries.5 In 2011, the Joint United Nations Programme on HIV/AIDS proposed a radical new framework to encourage investment in “the most effective programs based on local context”, make decisions based on “rational resource allocation”, and “increase efficiency in HIV prevention, treatment, care and support”.6 Identifying the optimal investment in increased HIV prevention, diagnostic, and treatment efforts continues to be a global health priority.
Significant advances in biomedical interventions in the last 5 years have changed the landscape of HIV care worldwide. Clinical trials investigating voluntary male circumcision,7–10 vaginal microbicides,11 and oral pre-exposure prophylaxis (PrEP)12–15 have shown partial effectiveness at reducing sexual HIV transmission. Many public health experts state that a multi-faceted “combination prevention” approach is necessary to curb the epidemic’s growth.16–19
With numerous biomedical prevention modalities to choose from, implementing the most efficient portfolio based on regional epidemic characteristics requires systematically comparing the relative costs and benefits of alternative allocation strategies. Estimating the population-level health benefits of scaling up these programs individually or in combination can shed light on possible synergistic effects,20 and help determine whether a portfolio of partially effective interventions could theoretically curb the epidemic. In the absence of costly, multi-intervention clinical trials, mathematical models play a critical role by augmenting existing data sources and forecasting future epidemic trends under different scenarios. Additionally, estimating the cost-effectiveness of combinations of HIV programs can assist policymakers with allocating limited resources most effectively and efficiently.
Prior modeling studies have evaluated individual HIV interventions, but few studies21–24 have considered intervention combinations or estimated a portfolio’s cost-effectiveness. One recent study modeled combinations of expanded ART and PrEP,25 although the study omitted secondary HIV transmission, which we find to be an important consideration. A challenge with modeling the HIV epidemic is its non-additive nature due to overlaps in program participants, behavior modification in response to program availability, and the non-linear spread of infectious diseases. Our study’s objective is to assess the impact of simultaneously scaling up multiple biomedical HIV prevention programs, and to calculate the benefits of reduced secondary transmission among partners of program recipients.
METHODS
Model Overview
We develop a Portfolio HIV Epidemic Model based on our previously published HIV model for the United States.24,26 Using epidemiologic and behavioral data for South Africa, we estimate the health benefits and cost-effectiveness of alternative HIV intervention portfolios consisting of expanded ART, screening and counseling, voluntary male circumcision, vaginal microbicide use, and oral PrEP. We consider South Africa because of the extensive HIV disease burden there, although our modeling framework could be extended to other geographic settings or intervention programs. A detailed description of the methodology is given in the Appendix (available online).
Disease Transmission and Progression
Our dynamic compartmental model accounts for disease progression, mortality, morbidity and heterosexual HIV transmission in the population. Disease progression is based on a simplified Markov model of the natural history of HIV, in the absence or presence of ART. Secondary HIV transmission is a key model component, and depends on demographics (baseline HIV prevalence, population sizes), sexual behavior (number of sexual partners, per-partner transmission probability, condom use), and the presence of one or more interventions (male circumcision, vaginal microbicide, PrEP, ART). We project HIV incidence under current conditions, and we consider the impact of combination interventions by changing model parameters accordingly.
Intervention Effectiveness
In our base case analysis, we assume that individual biomedical programs reduce the probability of HIV acquisition in uninfected individuals, which we denote as “intervention effectiveness”, according to values observed in clinical trials (Table 1). However, the joint effectiveness of oral PrEP and microbicides or male circumcision has not been examined in a clinical trial setting. In the absence of such data, mathematical modeling plays an important role in evaluating joint effectiveness under different assumptions. We initially assume that efficacy is multiplicative (e.g., if circumcision is 50 % effective and PrEP is 67 % effective, then the combined effectiveness is 1–[(1-50 %)*(1–67 %)] = 83.5 %). In sensitivity analysis, we consider a more conservative assumption that maximal effectiveness holds (e.g., combined effectiveness is max {50 %, 67 %} = 67 %).
Table 1.
Intervention Effectiveness Parameters Assumed in Model
| Parameter | Value | Range | Source |
|---|---|---|---|
| Reduction in sexual infectivity due to antiretroviral therapy (ART) | 96 % | 73–99 % | 32 |
| Reduction in HIV acquisition among men due to circumcision | 50 % | 28–66 % | 7–10 |
| Reduction in HIV acquisition among women due to vaginal microbicide (tenofovir gel) | 39 % | 6–60 % | 11 |
| Reduction in HIV acquisition due to oral pre-exposure prophylaxis (PrEP) | |||
| High adherence | 67 % | 44–81 % | 13–15,33 |
| Low adherence | 21 % | –31–52 % | 13–15,33 |
| Condom use among status-unaware persons | 25 % | 20–50 % | 28,34,35 |
| Condom use among status-aware persons | |||
| Uninfected | 25 % | 20–50 % | 28,34,35 |
| HIV-infected | 50 % | 25–75 % | 28,34,35 |
Clinical trials have yielded wide confidence intervals, and questions exist about whether the efficacies seen under experimental conditions will hold in real-world settings. We explore this uncertainty in probabilistic sensitivity analysis. Using a Monte Carlo simulation, we assign a probability distribution for each model parameter and randomly sample from each distribution simultaneously for 1,000 iterations. For each biomedical intervention (male circumcision, microbicide, and PrEP) and ART, the relative risk reduction is based on the clinical trial’s sampling distribution. For all other model parameters, we assume a uniform distribution across a range of plausible values (Table 1). This methodology simultaneously captures multiple-parameter uncertainty, generating an entire probability distribution for each outcome.
Outcomes
For each portfolio, we calculate HIV incidence and prevalence over 10 years, as well as discounted healthcare costs (2010 international dollars) and discounted quality-adjusted life years (QALYs), assuming a lifetime horizon.27 Because we compare expanded ART vis-à-vis HIV prevention, it is important to apply a universal metric such as QALYs, which include benefits to both uninfected (via reduced transmission) and infected (via reduced morbidity and mortality) persons. To investigate whether a portfolio of partially effective interventions is warranted given limited resources, we calculate the cost-effectiveness of select portfolios, based on average program costs of existing programs and reasonable assumptions about the costs of newer biomedical interventions.
RESULTS
Epidemic Projections
In 2008, approximately 20 % of men and 29 % of women in South Africa received an HIV test in the prior 12 months.28 In 2010, approximately 1 million HIV-infected persons received ART, amounting to 37 % of those in need.4 If these screening and treatment rates persist, we project that HIV prevalence will decline from 15 % to 12 % among men, and from 24 % to 16 % among women over 10 years (Fig. 1), with 1.58 million and 1.85 million infections occurring in men and women, respectively (Table 2), which is broadly consistent with other epidemic projections.29
Figure 1.
HIV prevalence over 10 years. Projected HIV prevalence in men (dashed lines) and women (solid lines) under the status quo (black circles); annual HIV screening and 75 % ART utilization (red triangles); 75 % male circumcision coverage within 5 years, 50 % microbicide utilization, and 50 % PrEP utilization (blue squares); or a combination portfolio of all 5 programs (cyan diamonds). ART = antiretroviral therapy; PrEP = oral pre-exposure prophylaxis.
Table 2.
Health Outcomes and Cost-Effectiveness of Select Portfolios
| Intervention strategy | HIV infections over 10 years (million) | Fraction of HIV infections averted (%)* | Discounted QALYs (million)† | Discounted Costs (billion)† | Incremental Cost-Effectiveness ($/QALY)‡ | ||
|---|---|---|---|---|---|---|---|
| Men | Women | Total | |||||
| Status quo | 3.43 | – | – | – | 626.7 | 658.9 | – |
| Single interventions | |||||||
| Screening | 2.87 | 14.3 % | 17.8 % | 16.2 % | +6.1 | +0.9 | $151 |
| ART (CD4 < 350 cells/mm3) | 2.93 | 15.5 % | 14.0 % | 14.7 % | +13.9 | +16.0 | $1,149 |
| Circumcision | 3.01 | 18.6 % | 6.6 % | 12.1 % | +3.3 | −2.3 | Cost-saving‡ |
| Microbicide | 2.94 | 6.8 % | 20.4 % | 14.1 % | +4.0 | +2.1 | $526 |
| PrEP | 2.45 | 28.6 % | 28.3 % | 28.4 % | +9.3 | +84.0 | $9,009 |
| Multiple interventions | |||||||
| Screening & ART | 2.25 | 33.0 % | 35.6 % | 34.4 % | +21.8 | +16.8 | $1,033‡ |
| Circumcision, Microbicide & PrEP | 1.94 | 42.7 % | 44.2 % | 43.5 % | +16.1 | +92.1 | $5,739 |
| Combination portfolio | 1.31 | 60.2 % | 63.3 % | 61.9 % | +31.0 | +108.4 | $9,937‡ |
Each strategy includes a scale-up of select programs as follows: Screening with annual frequency; ART with 75 % utilization; Male circumcision with 75 % coverage within 5 years; Microbicide with 50 % utilization; PrEP with 50 % utilization; Combination portfolio includes all five programs
QALY quality-adjusted life year, ART antiretroviral therapy, PrEP pre-exposure prophylaxis (oral)
*Fraction of HIV infections averted are relative to the Status quo
†For each intervention strategy, discounted QALYs and costs (2010 international dollars) are relative to the Status quo. These include direct costs of the intervention over 10 years, and future lifetime QALYs and costs for everyone alive at the end of 10 years
‡For strategies on the cost-effectiveness frontier, incremental cost-effectiveness ratios ($/QALY) are relative to the next-best strategy
Single Interventions
We first consider a unilateral increase in HIV screening or treatment. Achieving 75 % ART utilization with initiation at CD4 < 350 cells/mm3 prevents 15 % of new HIV infections due to reduced infectivity in ART recipients, but modestly decreases HIV prevalence because of longer life expectancy among ART recipients. Alternatively, an annual HIV screening program could prevent 16 % of new infections.
Next, we evaluate strategies that increase use of biomedical interventions only, assuming HIV screening and ART utilization remain at current levels. A scale-up of male circumcision to 75 % of adult men within 5 years reduces new infections among men by 19 %. A vaginal microbicide gel containing tenofovir,11 if regularly utilized by 50 % of women, could reduce HIV incidence among women by 20 %. Although circumcision and microbicides predominantly benefit men and women, respectively, we also find a modest, but important, reduction in incidence among the opposite gender due to reduced secondary transmission (i.e., female partners of circumcised men and male partners of women using microbicides experience reduced HIV acquisition if their partner avoids infection). Alternatively, use of PrEP by 50 % of all uninfected persons (with half maintaining high and low adherence) reduces overall HIV incidence by 28 % with similar effects in men and women.
Multiple Interventions
Simultaneously expanding HIV screening and ART prevents 34 % of infections, more than the sum of the individual programs. Screening and ART act synergistically because each program complements the other: individuals must first be diagnosed before initiating treatment.24 A focus instead on scaling up biomedical programs (male circumcision, microbicides, and PrEP) averts 44 % of new infections, substantially less than the sum of individual programs, because of secondary transmission (i.e., a future HIV infection cannot be prevented more than once). A comprehensive portfolio of HIV screening, ART, male circumcision, microbicides, and PrEP prevents 2.1 million infections over 10 years, reducing overall incidence by 62 %. Under this scenario, overall HIV prevalence declines to 10 % after 10 years (9 % in men, 12 % in women).
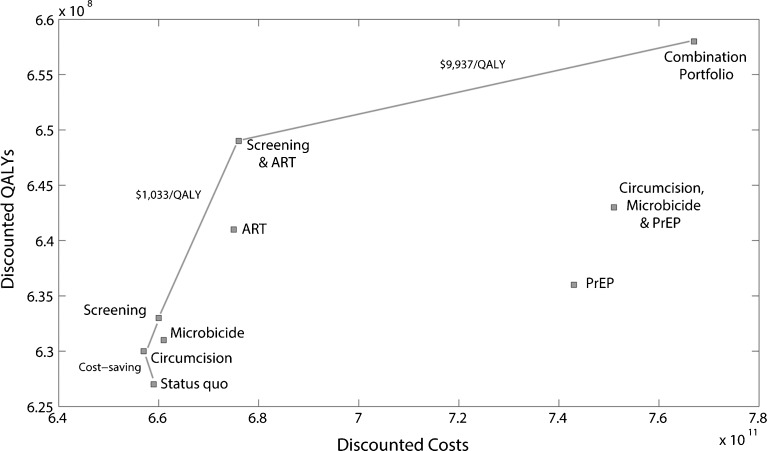
Cost-Effectiveness Analysis
Male circumcision is the most economically efficient strategy, increasing QALYs while decreasing costs, relative to the status quo (Table 2, Fig. 2). Although a microbicide’s price is inherently unknown as it is not yet available, if we assume an annual price of $100, this strategy costs approximately $500 per QALY gained (with regular use by 50 % of uninfected women). HIV screening annually costs $150 per QALY gained, whereas screening every 2 years costs less than $100 per QALY gained, but results in 50 % fewer QALYs.
Figure 2.
Cost-effectiveness analysis. Discounted costs and discounted QALYs over 10 years are shown for select portfolios: 75 % ART utilization; annual HIV screening; 75 % male circumcision coverage within 5 years; 50 % microbicide utilization; 50 % PrEP utilization; or select combinations of all five programs. The solid line corresponds to the cost-effectiveness frontier (strategies that are most economically efficient) with the incremental cost-effectiveness ratios given. QALY = quality-adjusted life year; ART = antiretroviral therapy; PrEP = oral pre-exposure prophylaxis.
In contrast to these relatively cost-effective interventions, a PrEP program offered to half of all uninfected persons, with 50 % high adherence, costs more than $9,000 per QALY gained. If all individuals are highly adherent, cost-effectiveness improves to $6,300 per QALY gained. If the price of PrEP falls to $400 per year, cost-effectiveness improves to $4,300 per QALY gained.
Of the five individual programs, expanded ART offers the largest gain in health benefits (14 million additional QALYs) for $1,150 per QALY gained. Because of the synergistic nature of screening and treatment, scaling up these two programs simultaneously is economically efficient at $1,000 per QALY gained. Augmenting this strategy with a comprehensive portfolio of all three biomedical programs offers the greatest net gain in health benefits for approximately $9,900 per QALY gained. This portfolio of expanded HIV screening, treatment, male circumcision, microbicides, and PrEP would be considered “very cost-effective” in South Africa based on the WHO’s Commission on Macroeconomics and Health guidelines.30
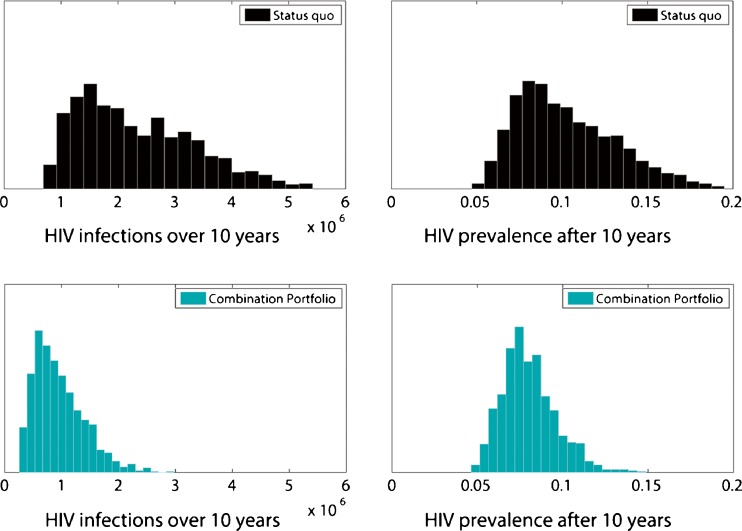
Sensitivity Analysis
Program Effectiveness
Given the inherent uncertainty in model parameters—especially the wide confidence intervals on intervention efficacy reported in clinical trials—we translate multiple sources of uncertainty into variability in future epidemic projections. Figure 3 shows the distribution of new HIV infections based on the Monte Carlo simulation, under current conditions or a combination portfolio. Even with considerable uncertainty in program effectiveness, a comprehensive portfolio substantially reduces HIV incidence and prevalence over 10 years. With this portfolio, in two-thirds of simulation iterations, more than 1 million HIV infections are prevented over 10 years, a 30 % reduction from the 3.4 million infections projected under current conditions (Appendix Figure A3).
Figure 3.
Probabilistic sensitivity analysis. Frequency distribution showing the projected number of HIV infections over 10 years (left charts) and overall HIV prevalence after 10 years (right charts) under the status quo (top, black) or combination portfolio of all five programs (bottom, cyan), based on a Monte Carlo simulation with 1,000 iterations. Each bar shows the relative frequency of projected HIV infections or HIV prevalence.
Program Utilization
Potential utilization of each program is uncertain, and we find that lower uptake attenuates some of the benefits. However, even with modest uptake (50 % ART utilization, HIV screening every 2 years, 75 % male circumcision coverage after 10 years, 25 % utilization of microbicides and PrEP), more than 1.2 million HIV infections are prevented (36 % of the projected total), suggesting that a multi-faceted approach has the greatest chance of mitigating the HIV epidemic in South Africa.
Joint Effectiveness
Under an alternative assumption that joint effectiveness is the maximum of individual program effectiveness, a portfolio of expanded male circumcision, microbicides, and PrEP averts 37 % of infections (compared to 44 % in the base case). An interpretation of this finding is that multiple interventions create redundancy: a portfolio of partially effective interventions helps ensure that uninfected persons likely receive at least one intervention.
Condom Use
The behavioral impact following HIV screening and counseling may vary. Even with no change in condom use among HIV-infected persons who learn their status, an annual screening program averts 6 % of projected infections because screening identifies people earlier, allowing them to begin ART sooner. Under this pessimistic assumption, annual screening costs $900 per QALY gained versus $150 in the base case.
Time Horizon
We initially modeled HIV transmission over 10 years, to capture the short-term benefits of implementing an HIV prevention portfolio, although our model does include future lifetime costs and QALYs of those alive after 10 years. With a longer time horizon, additional uncertainty exists about the availability of newer interventions such as a vaccine. We find that the benefits of an intervention portfolio only improve with a longer time horizon. A comprehensive portfolio prevents nearly 70 % of HIV infections over 20 years, compared to 62 % over 10 years, because future infections are continually prevented. ART scale-up appears more favorable, with a cost-effectiveness of $700 per QALY gained, versus $1,150 over 10 years, because the reduction in infectivity continues beyond 10 years.
Probabilistic Cost-Effectiveness Analysis
The cost-effectiveness of combination interventions is uncertain, in part due to uncertainty in each program’s effectiveness at reducing HIV transmission and the epidemic’s future trajectory. Our Monte Carlo simulation aggregates multiple sources of uncertainty and provides a full distribution of projected costs and QALYs. Figure 4a illustrates 1,000 iterations for three scenarios considered: the status quo; a scale-up of HIV screening and ART; and a comprehensive portfolio consisting of screening, ART, and all three biomedical interventions. In general, we find there is a wide range in projected costs and QALYs, but expanded HIV screening and ART generally results in more QALYs (the red triangles fall slightly above the black circles). The combination portfolio results in both greater QALYs and higher costs.
Figure 4.
Probabilistic cost-effectiveness analysis. a Discounted costs and discounted QALYs over 10 years are shown for select portfolios: status quo (black dots); annual HIV screening and 75 % ART utilization (red triangles); or a combination portfolio of annual HIV screening, 75 % ART utilization, 75 % male circumcision coverage within 5 years, 50 % microbicide utilization, and 50 % PrEP utilization (cyan diamonds). b Cumulative probability distributions for the cost-effectiveness of annual HIV screening and 75 % ART utilization versus the status quo (red line); or a combination portfolio of annual HIV screening, 75 % ART utilization, 75 % male circumcision coverage within 5 years, 50 % microbicide utilization, and 50 % PrEP utilization versus screening and ART only (cyan line). The graph shows the probability that the select portfolio has a cost-effectiveness ratio less than the value on the x-axis, given a Monte Carlo simulation with 1,000 iterations. QALY = quality-adjusted life year; ART = antiretroviral therapy; PrEP = oral pre-exposure prophylaxis.
A cumulative probability distribution is shown for two key portfolios (Fig. 4b). Expanded HIV screening and ART appears very cost-effective, costing less than $5,000 per QALY gained with 97 % probability. Alternatively, a comprehensive portfolio costs less $10,000 per QALY gained with 32 % probability, and less than $30,000 per QALY gained with 92 % probability. This provides a level of confidence on portfolio cost-effectiveness given policymakers’ willingness-to-pay for one additional QALY gained.
Optimal Resource Allocation
In addition to assessing specific portfolios (Table 2), we evaluate varying combinations of each program to determine the optimal portfolio given a particular budget. If policymakers aim to maximize QALYs, the optimal portfolio should always increase male circumcision because it is cost-saving. As the budget increases, more frequent HIV screening should be implemented, followed by microbicides, ART, and finally PrEP, only after the other programs have been scaled up (Appendix Figure A4). If a limited budget does not allow for implementation of all programs, a portfolio consisting of HIV testing every 6 months, full ART access, male circumcision, and regular microbicide use could offer 90 % of the benefits, for less than 25 % of the cost, compared to the same portfolio with PrEP added. This illustrates the possibility of achieving substantial health benefits with limited resources by implementing an efficient portfolio.
DISCUSSION
Our modeling framework generates a number of insights about the relative costs and benefits of combinations of new HIV prevention technologies in South Africa, highlighting the importance of not considering partially effective programs in isolation, but rather as one component of a multi-faceted approach to HIV epidemic control. This study lends support to the ongoing debate about whether implementation of modestly effective interventions is warranted, and our novel HIV portfolio model is uniquely well-suited to address these questions.
Our results suggest that a combination portfolio that includes screening, treatment, male circumcision, microbicides, and PrEP could substantially reduce the HIV epidemic in South Africa, adding millions of life-years to the population, and would likely be cost-effective. Given a limited budget, resources should be allocated first to increased male circumcision, then more frequent HIV screening, vaginal microbicides, and increased ART. As more resources become available, investment could be extended to oral PrEP.
As program utilization increases, the effectiveness at reducing transmission becomes a central source of uncertainty21 due to variations in program accessibility, patient adherence, and potential behavior risk compensation. The aggregate impact of implementing multiple, partially effective programs compounds this uncertainty and has previously not been systematically investigated. Our modeling framework evaluates this uncertainty, using sampling distributions from clinical trials when available. An important consideration with scaling up gender-specific programs is the degree to which recipients’ sexual partners may benefit. Our model captures primary and secondary HIV transmission in the population, to estimate the indirect benefits of a particular intervention. In particular, we find that male circumcision and microbicides predominantly benefit men and women, respectively, but a significant proportion of infections are subsequently averted in the opposite sex.
Our study has several limitations. Similar to many HIV epidemic models, we utilize a dynamic compartmental model, which does not include a level of granularity in sexual behavior seen in the real world, and simplifies the complexity of the natural history of HIV.31 We do not account for potential drug resistance resulting from a scale-up of PrEP; if this occurs, cost-effectiveness will likely worsen. We assume a reasonable price for a microbicide gel, which is unavoidable, given that one is not yet commercially available. We include the marginal cost of expanding prevention and treatment, but we do not perform a full cost accounting of labor, lost productivity, etc. We do not forecast a decline in ART prices; if prices drop substantially, this will only make the combination portfolio more favorable. Our analysis is based on current estimates of program costs and effectiveness, and these estimates can be updated once additional data become available. Lastly, we do not include age-adjusted quality of life and we report outcomes in terms of QALYs gained. If life years or disability-adjusted life years (DALYs) were instead calculated, we expect the interventions to appear slightly more cost-effective, as preventing an HIV infection in younger people results in more future life-years accrued.
In the absence of multi-intervention randomized clinical or observational trials, a mathematical HIV epidemic model provides useful insights about the aggregate benefit of implementing a portfolio of biomedical, diagnostic, and treatment programs, even with substantial uncertainty in individual program effectiveness. Allocating limited available resources for HIV control in South Africa is a key priority, and our study indicates that a multi-intervention HIV portfolio could avert nearly two-thirds of projected new HIV infections, and is a cost-effective use of resources.
Electronic supplementary material
(PDF 286 kb)
Acknowledgements
We wish to thank Margaret Brandeau and Edward Kaplan for their valuable suggestions for improving the manuscript. This study was supported in part by a grant from the National Institute on Drug Abuse (R01-DA15612). An earlier version of this paper was presented at the Society for Medical Decision Making Annual Meeting in October 2011.
Conflicts Of Interest
The authors declare that they have no conflicts of interest.
Author Contributions
Elisa F. Long: study design, model building and coding, data analysis, data interpretation, writing of the manuscript.
Robert R. Stavert: literature search, data collection, data analysis.
REFERENCES
- 1.Lozano R, Naghavi M, Foreman K, et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2013;380(9859):2095–2128. doi: 10.1016/S0140-6736(12)61728-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Salomon JA, Vos T, Hogan DR, et al. Common values in assessing health outcomes from disease and injury: disability weights measurement study for the Global Burden of Disease Study 2010. Lancet. 2013;380(9859):2129–2143. doi: 10.1016/S0140-6736(12)61680-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wang H, Dwyer-Lindgren L, Lofgren KT, et al. Age-specific and sex-specific mortality in 187 countries, 1970-2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2013;380(9859):2071–2094. doi: 10.1016/S0140-6736(12)61719-X. [DOI] [PubMed] [Google Scholar]
- 4.Joint United Nations Programme on HIV/AIDS (UNAIDS). Report on the global AIDS epidemic. Geneva 2010.
- 5.Kates J, Boortz K, Lief E, Avila C, Bobet G. Financing the Response to AIDS in Low- and Middle-Income Countries: International Assistance from the G8, European Commission and Other Donor Governments in 2009, Washington, DC: Kaiser Family Foundation and UNAIDS; 2010. [Google Scholar]
- 6.Joint United Nations Programme on HIV/AIDS (UNAIDS). World AIDS Day Report. Geneva 2011.
- 7.Auvert B, Taljaard D, Lagarde E, Sobngwi-Tambekou J, Sitta R, Puren A. Randomized, controlled intervention trial of male circumcision for reduction of HIV infection risk: the ANRS 1265 Trial. PLoS Med. 2005;2(11):e298. doi: 10.1371/journal.pmed.0020298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bailey RC, Moses S, Parker CB, et al. Male circumcision for HIV prevention in young men in Kisumu, Kenya: a randomised controlled trial. Lancet. 2007;369(9562):643–656. doi: 10.1016/S0140-6736(07)60312-2. [DOI] [PubMed] [Google Scholar]
- 9.Gray RH, Kigozi G, Serwadda D, et al. Male circumcision for HIV prevention in men in Rakai, Uganda: a randomised trial. Lancet. 2007;369(9562):657–666. doi: 10.1016/S0140-6736(07)60313-4. [DOI] [PubMed] [Google Scholar]
- 10.Siegfried N, Muller M, Deeks JJ, Volmink J. Male circumcision for prevention of heterosexual acquisition of HIV in men. Cochrane database of systematic reviews (Online). 2009(2):CD003362. [DOI] [PubMed]
- 11.Abdool Karim Q, Abdool Karim SS, Frohlich JA, et al. Effectiveness and safety of tenofovir gel, an antiretroviral microbicide, for the prevention of HIV infection in women. Science. 2010;329(5996):1168–1174. doi: 10.1126/science.1193748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Grant RM, Lama JR, Anderson PL, et al. Preexposure chemoprophylaxis for HIV prevention in men who have sex with men. N Engl J Med. 2010;363(27):2587–2599. doi: 10.1056/NEJMoa1011205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Van Damme L, Corneli A, Ahmed K, et al. Preexposure prophylaxis for HIV infection among African women. N Engl J Med. 2012;367(5):411–422. doi: 10.1056/NEJMoa1202614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Baeten JM, Donnell D, Ndase P, et al. Antiretroviral prophylaxis for HIV prevention in heterosexual men and women. N Engl J Med. 2012;367(5):399–410. doi: 10.1056/NEJMoa1108524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Thigpen MC, Kebaabetswe PM, Paxton LA, et al. Antiretroviral preexposure prophylaxis for heterosexual HIV transmission in Botswana. N Engl J Med. 2012;367(5):423–434. doi: 10.1056/NEJMoa1110711. [DOI] [PubMed] [Google Scholar]
- 16.Hankins CA, de Zalduondo BO. Combination prevention: a deeper understanding of effective HIV prevention. AIDS. 2010;24(Suppl 4):S70–80. doi: 10.1097/01.aids.0000390709.04255.fd. [DOI] [PubMed] [Google Scholar]
- 17.Kurth AE, Celum C, Baeten JM, Vermund SH, Wasserheit JN. Combination HIV prevention: significance, challenges, and opportunities. Curr HIV/AIDS Rep. 2011;8(1):62–72. doi: 10.1007/s11904-010-0063-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Folkers GK, Fauci AS. Controlling and ultimately ending the HIV/AIDS pandemic: a feasible goal. JAMA. 2010;304(3):350–351. doi: 10.1001/jama.2010.957. [DOI] [PubMed] [Google Scholar]
- 19.National Institute of Allergy and Infectious Diseases (NIAID). HIV Study Named 2011 Breakthrough of the Year by Science. 2011; http://www.niaid.nih.gov/news/newsreleases/2011/Pages/HPTN052Breakthrough.aspx. Accessed January 25, 2013.
- 20.Excler JL, Rida W, Priddy F, et al. AIDS vaccines and preexposure prophylaxis: is synergy possible? AIDS Res Hum Retroviruses. 2011;27(6):669–680. doi: 10.1089/aid.2010.0206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Stover J, Bertozzi S, Gutierrez JP, et al. The global impact of scaling up HIV/AIDS prevention programs in low- and middle-income countries. Science. 2006;311(5766):1474–1476. doi: 10.1126/science.1121176. [DOI] [PubMed] [Google Scholar]
- 22.Hogan DR, Baltussen R, Hayashi C, Lauer JA, Salomon JA. Cost effectiveness analysis of strategies to combat HIV/AIDS in developing countries. BMJ. 2005;331(7530):1431–1437. doi: 10.1136/bmj.38643.368692.68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Salomon JA, Hogan DR, Stover J, et al. Integrating HIV prevention and treatment: from slogans to impact. PLoS Med. 2005;2(1):e16. doi: 10.1371/journal.pmed.0020016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Long EF, Brandeau ML, Owens DK. The cost-effectiveness and population outcomes of expanded HIV screening and antiretroviral treatment in the United States. Ann Intern Med. 2010;153:778–789. doi: 10.7326/0003-4819-153-12-201012210-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hallett TB, Baeten JM, Heffron R, et al. Optimal Uses of Antiretrovirals for Prevention in HIV-1 Serodiscordant Heterosexual Couples in South Africa: A Modelling Study. PLoS Med. 2011;8(11):e1001123. doi: 10.1371/journal.pmed.1001123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Long EF, Brandeau ML, Owens DK. Potential population health outcomes and expenditures of HIV vaccination strategies in the United States. Vaccine. 2009;27(39):5402–5410. doi: 10.1016/j.vaccine.2009.06.063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gold MR, Siegel JE, Russell LB, Weinstein MC, editors. Cost-Effectiveness in Health and Medicine. New York: Oxford University Press; 1996. [Google Scholar]
- 28.Shisana O, Rehle T, Simbayi L, et al. South African national HIV prevalence, HIV incidence, behaviour and communication survey, 2008: A turning tide among teenagers? Cape Town: HSRC Press; 2009. [Google Scholar]
- 29.Country progress report on the Declaration of Commitment on HIV/AIDS. Pretoria: Department of Health; 2010. [Google Scholar]
- 30.World Health Organization Commission on Macroeconomics and Health. Macroeconomics and Health: Investing in Health for Economic Development. Geneva 2001.
- 31.Freedberg KA, Losina E, Weinstein MC, et al. The cost effectiveness of combination antiretroviral therapy for HIV disease. N Engl J Med. 2001;344(11):824–831. doi: 10.1056/NEJM200103153441108. [DOI] [PubMed] [Google Scholar]
- 32.Cohen MS, Chen YQ, McCauley M, et al. Prevention of HIV-1 infection with early antiretroviral therapy. N Engl J Med. 2011;365(6):493–505. doi: 10.1056/NEJMoa1105243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cohen MS, Baden LR. Preexposure prophylaxis for HIV–where do we go from here? N Engl J Med. 2012;367(5):459–461. doi: 10.1056/NEJMe1207438. [DOI] [PubMed] [Google Scholar]
- 34.Shisana O, Rehle T, Simbayi L, et al. South African national HIV prevalence, HIV incidence, behaviour and communication survey, 2005. Cape Town: HSRC Press; 2005. [Google Scholar]
- 35.South Africa Department of Health, Medical Research Council. South Africa demographic and health survey 2003. Pretoria: Department of Health; 2007.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF 286 kb)