Abstract
INTRODUCTION
Primary hyperparathyroidism is a common endocrine disorder, with an incidence of 21.6 per 100,000 person-years. Asymptomatic elevated serum calcium levels on routine biochemical investigations accounts for 80% of newly diagnosed primary hyperparathyroidism. Solitary adenoma is the commonest cause of primary hyperparathyroidism and can be treated by excision of a single gland.
PRESENTATION OF CASE
We present a case of primary hyperparathyroidism in a 74-year-old female was referred to our surgery endocrine outpatients for assessment of a persistently elevated calcium level, lower abdominal pain and constipation. Biochemical analysis revealed corrected serum calcium of 3.13 mmol/L (reference range 2.17–2.51 mmol/L) and an intact parathyroid hormone level (iPTH) of 488.9 ng/L (reference range 15–65 ng/L). Sestamibi scan localised a persistent increased area of activity inferior to the lower pole of the left lobe of thyroid gland.
DISCUSSION
The patient underwent a minimally invasive parathyroidectomy using a 3 cm incision with intra-op radionucliotide localisation. At surgery a single large parathyroid gland measuring 5.5 cm was excised without complication. Grossly the parathyroid gland was an encapsulated tan mass measuring 5.5 cm × 2.5 cm × 2 cm and weight 13 g and histological assessment revealed a water-clear cell (WCC) adenoma. She made an uneventful post op recovery with normalisation of her serum calcium.
CONCLUSION
WCC adenomas have a “low endocrinological activity” in which serum calcium levels do not elevate until the adenoma has reached considerable size. Our case supports this hypothesis and aids to the understanding of these rare tumours.
Keywords: Water clear cell adenoma, Parathyroid adenoma, Hypercalcaemia
1. Background
Primary hyperparathyroidism is a common endocrine disorder, with an incidence of 21.6 per 100,000 person-years.1 Asymptomatic elevated serum calcium levels on routine biochemical investigations accounts for 80% of newly diagnosed primary hyperparathyroidism. Solitary adenoma is the commonest cause of primary hyperparathyroidism and can be treated by excision of a single gland. We present a case of primary hyperparathyroidism caused by Water-clear cell adenoma (WCC), a rare form of solitary parathyroid adenoma.
2. Case presentation
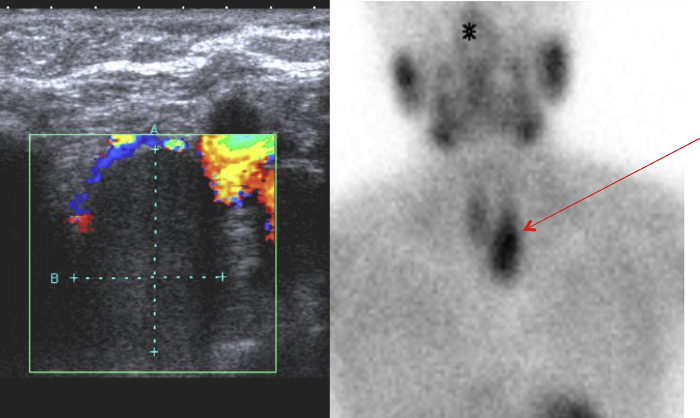
A 74-year-old female was referred to our surgery endocrine outpatients for assessment of a persistently elevated calcium level. She was symptomatic with lower abdominal pain, constipation and lethargy. Of note she did not suffer from depression, and she had no previous history of nephrolithiasis. She had a non-contributory past medical history and reported no family history of multiple endocrine neoplasia type 1 (MEN-1). Biochemical analysis revealed corrected serum calcium of 3.13 mmol/L (reference range 2.17–2.51 mmol/L) and an intact Parathyroid hormone level (iPTH) of 488.9 ng/L (reference range 15–65 ng/L). An ultrasound scan demonstrated a 4.8 cm × 2.2 cm × 1.7 cm hypoechoic well defined structure inferior to the lower pole of the left lobe of thyroid gland. Given the biochemical and radiological results, a provisional diagnosis parathyroid adenoma. A Sestamibi scan localised a persistent increased area of activity corresponding that seen on ultrasound, confirming a parathyroid adenoma (Fig. 1).
Fig. 1.
Ultrasound and Sestamibi scans demonstrating left lower parathyroid gland adenoma.
The patient underwent a minimally invasive parathyroidectomy using a 3 cm incision with intra-op radionucliotide localisation under general anaesthetic (Fig. 2). At surgery a single large parathyroid gland measuring 5.5 cm was excised without complication (Fig. 3). Grossly the parathyroid gland was an encapsulated tan mass measuring 5.5 cm × 2.5 cm × 2 cm and weight 13 g. Serial sections and histological analysis revealed a WCC adenoma with a thin capsule. Parathyroid tissue was seen at the periphery as well as surrounding fat. Lymphovascular invasion and extracapsular extension was not present (Fig. 4). She made an uneventful post op recovery and her serum calcium returned to the normal range with resolution of her lower abdominal pain and constipation.
Fig. 2.

Minimally invasive parathyroidectomy using a 3 cm incision with intra-op radionucliotide localisation.
Fig. 3.
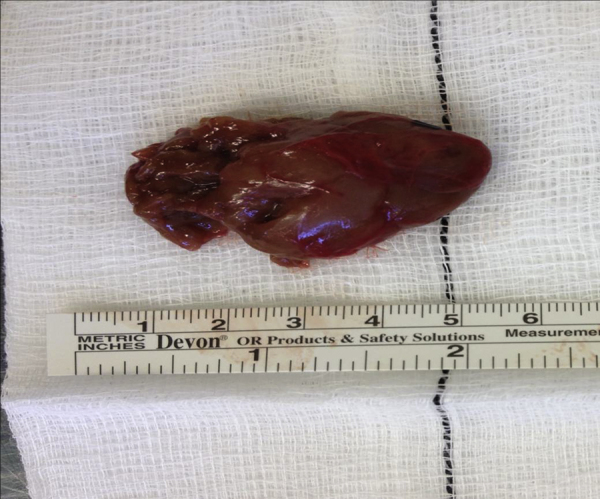
Large parathyroid gland.
Fig. 4.
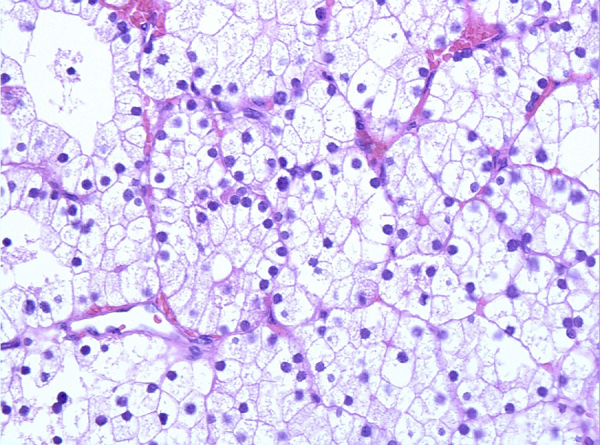
Water-clear cell adenoma (H&E stain).
3. Discussion
Parathyroid adenoma is the most common cause of primary hyperparathyroidism, accounting for approximately 85% of cases. Histologically parathyroid adenomas are composed of functioning parathyroid tissue containing a mixed population cell population, consisting primarily of chief cells.2 While lesions have also been described containing clear cells and oxyphilic cells,3 a parathyroid adenoma consisting entirely of water-cell cells, such as in the case in our patient, is extremely rare.
First described by Kovacs et al. in 1994,4 there are only 10 reported cases of WCC parathyroid adenomas in literature.5 Unlike typical parathyroid adenomas, a water clear cell adenoma is composed of large clear cells with optically clear cytoplasm due to multiple vesicles and glycogen5 (Fig. 4). These histological features were first described in the context of WCC parathyroid hyperplasia by Albright in 1934.6 WCC hyperplasia is more common than the corresponding adenoma, but it remains a rarity in clinical practice. In our case, the diagnosis of parathyroid adenoma was favoured over hyperplasia due to pre operative localisation and return of biochemical markers to the normal range after excision of a single gland. Furthermore our patient has remained normocalcaecmic in the initial 3-month follow up period.
Our patient underwent minimally invasive parathyroidectomy, which has been shown to by Udelsman et al. to be a superior to traditional bilateral neck exploration. As well as demonstrating improvements in cure rate and complications rates, the study also illustrated the economic benefits of minimally invasive surgery with a shorted hospital stay and total cost of treatment.7 Given the higher incidence of WCC hyperplasia over adenoma our patient will continue to be followed up closely for recurrence of her hyperparathyroidism as her other parathyroid glands were not explored at time off operation. However the normalisation of her biochemical parameters is reassuring. The data published on long term follow up of such patients indicated that there is no statistical significant difference in hyperparathyroidism persistence or recurrence in those who undergo minimally invasive surgery compared with the traditional exploration.8
In our case, despite the high PTH level, serum calcium was not overtly elevated and our patient was relatively asymptomatic. Kanda et al. hypothesised that due to the large size of the adenoma compared with the biochemical and clinical features, WCC adenomas have a “low endocrinological activity” and that calcium does not elevate until the adenoma has reached a considerable size.3 Our case supports this hypothesis and aids to the understanding of these rare tumours.
Conflict of interest
No conflict of interest.
Funding
Nil
Ethical approval
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Author's contribution
RPP contributed in writing of the manuscript. PSW involved in review of the manuscript prior to submission. JA had made images. FC involved in review of the pathology. MJK had done final review and design of manuscript prior to submission.
Footnotes
This is an open-access article distributed under the terms of the Creative Commons Attribution-NonCommercial-No Derivative Works License, which permits non-commercial use, distribution, and reproduction in any medium, provided the original author and source are credited.
References
- 1.Wermers R.A., Khosla S., Atkinson E.J., Achenbach S.J., Oberg A.L., Grant C.S. Incidence of primary hyperparathyroidism in Rochester, Minnesota, 1993–2001: an update on the changing epidemiology of the disease. Journal of Bone and Mineral Research: the Official Journal of the American Society for Bone and Mineral Research. 2006;21(1):171–177. doi: 10.1359/JBMR.050910. Epub 2005/12/16. [DOI] [PubMed] [Google Scholar]
- 2.Bedetti C.D., Dekker A., Watson C.G. Functioning oxyphil cell adenoma of the parathyroid gland: a clinicopathologic study of ten patients with hyperparathyroidism. Human Pathology. 1984;15(12):1121–1126. doi: 10.1016/s0046-8177(84)80306-8. Epub 1984/12/01. [DOI] [PubMed] [Google Scholar]
- 3.Kanda K., Okada Y., Tanikawa T., Morita E., Tsurudome Y., Konishi T. A rare case of primary hyperparathyroidism with clear cell adenoma. Endocrine Journal. 2004;51(2):207–212. doi: 10.1507/endocrj.51.207. [DOI] [PubMed] [Google Scholar]
- 4.Kovacs K., Horvath E., Ozawa Y., Yamada S., Matushita H. Large clear cell adenoma of the parathyroid in a patient with MEN-1 syndrome. Ultrastructural study of the tumour exhibiting unusual RER formations. Acta Biologica Hungarica. 1994;45(2–4):275–284. [PubMed] [Google Scholar]
- 5.Murakami K., Watanabe M., Nakashima N., Fujimori K., Ishida K., Ohuchi N. Water-clear cell adenoma associated with primary hyperparathyroidism: report of a case. Surgery Today. 2013 doi: 10.1007/s00595-013-0568-7. Epub 2013/03/30. [DOI] [PubMed] [Google Scholar]
- 6.Albright F., Bloomberg E., Castleman B., Churchill E.D. Hyperparathyroidism due to diffuse hyperplasia of all parathyroid glands rather than adenoma of one: clinical studies on three such cases. Archives of Internal Medicine. 1934;54(3):315–329. [Google Scholar]
- 7.Udelsman R., Lin Z., Donovan P. The superiority of minimally invasive parathyroidectomy based on 1650 consecutive patients with primary hyperparathyroidism. Annals of Surgery. 2011;253(3):585–591. doi: 10.1097/SLA.0b013e318208fed9. [DOI] [PubMed] [Google Scholar]
- 8.Schneider D.F., Mazeh H., Sippel R.S., Chen H. Is minimally invasive parathyroidectomy associated with greater recurrence compared to bilateral exploration? Analysis of more than 1000 cases. Surgery. 2012;152(6):1008–1015. doi: 10.1016/j.surg.2012.08.022. [DOI] [PMC free article] [PubMed] [Google Scholar]