Abstract
INTRODUCTION
Transcatheter aortic valve implantation (TAVI) represents an emerging therapy for valve replacement in patients not suitable for traditional open repair. As awareness of the procedure grows, case numbers are increasing worldwide. Though this procedure represents a less invasive approach to aortic valve replacement, it is not without complications.
PRESENTATION OF CASE
This case presentation describes a serious, previously unreported, complication incurred in an 83-year-old male in whom TAVI was attempted. During deployment of the valve at the aortic annulus, both the valve and accompanying balloon embolised into the thoracic aorta and this was further complicated by migration of the balloon into the abdominal aorta and an aortic dissection. The false lumen of the dissection at the level of the infrarenal aorta was tacked to the aortic adventitial wall using interrupted sutures through a laparotomy. A completion angiogram demonstrated that a flow limited dissection did extend up to both common iliac arteries. This was managed with balloon-expandable covered stents deployed in both common iliac arteries with satisfactory outcome.
DISCUSSION
This case occurred as a combination of multiple factors that include lack of burst pacing and poor timing of the balloon inflation. The aortic balloon and the valve had to be removed urgently to avoid ventricular embolization of these structures that can result in a fatal situation.
CONCLUSION
This case presentation describes the management of these complications using a combined open and endovascular approach in a well-equipped hybrid operating theatre, resulting in the patient survival.
Keywords: Aortic valve, Embolization, Aortic stenosis
1. Background
The development of TAVI dates back to the early 1960s when Davies et al. first described a catheter-mounted valve for the treatment of aortic insufficiency in an animal model.1 The first successful TAVI in a human was described by Cribier et al. in 2002 who used a transseptal catheter to implant a newly developed percutaneous heart valve in a patient who was too high risk for conventional open surgery.2
The technique is gaining popularity and now becoming the preferred treatment option for patients with severe aortic stenosis unsuitable for open valve replacement. The two main approaches for TAVI are the transfemoral retrograde arterial approach and the antegrade transapical route.3 The two main devices currently available are the Edward Sapien XT (Edwards Life sciences, Irvine, CA, USA) and the Medtronic Core Valve® system (Medtronic, Minneapolis, USA). The Edwards Sapien prosthesis is a bovine pericardial valve on a balloon-expandable cobalt chromium frame, which has been approved for implantation via both the transfemoral and transapical route.3 The Core Valve® is a self-expanding tri-leaflet porcine valve mounted on a nitinol stent frame.4
In this article, we report the challenge in the management of an unusual complication during a TAVI procedure, which necessitated a complex and tenuous hybrid approach. At this time, there have been no reports in the literature of distal aortic valve and balloon embolization up to the orifice of the great vessels complicated by a traumatic acute aortic dissection during retrieval of the devices percutaneously.
2. Case report
An 83-year-old man with severe symptomatic calcific aortic stenosis and a background of previous coronary artery bypass grafting, hypertension and hyperlipidaemia, presented to the cardiologists after being deemed unsuitable for traditional open repair by the cardiothoracic team. Over the preceding 4 months he had been complaining of worsening exertional dyspnoea and dizziness and was becoming increasingly functionally incapacitated. His NYHA functional class was 3. He had a frailty index of 3, STS score of 6% and logistic euroscore of 17%. A transoesophageal echocardiogram (TOE) showed a normal left ventricular ejection fraction (LVEF) with mild mitral regurgitation (MR) and severe aortic stenosis (AS) (mean aortic gradient of 46 mmHg). After a full pre-operative workup, which included a coronary (demonstrates patents coronary bypass grafts) and aortobifemoral angiogram, he was deemed suitable for valve replacement via a transfemoral approach using an Edward Sapien XT 26 mm valve. However, the valve becoming unseated during deployment under burst pacing due to an excessive ventricular contraction. The valve embolised from the annulus distally and lodged at the aortic arch causing an obstruction to flow into the innominate and left common carotid artery. Being a bovine arch, this caused a degree of compromise to cerebral blood flow. An attempt was made to retrieve the device percutaneously utilising the deployment balloon but this was unsuccessful and further complicated the procedure by causing a traumatic acute aortic dissection, extending from the ascending aorta to the descending thoracic aorta, as well as resulting in the nose-cone of the TAVI balloon bursting and embolising into the abdominal aorta (Fig. 1). The patient subsequently underwent an emergency redo-sternotomy by the cardiothoracic surgeons. The prosthetic valve was retrieved from the aortic arch under a brief period of total circulatory arrest (15 min) and the diseased aortic valve was replaced with a 21 mm Carpentier-Edwards Perimount Magna tissue valve. The cross clamp time was 146 min (in two episodes) with a bypass time of 276 min. The hemiarch and ascending aortic root was replaced using a 26 mm Dacron graft that was anastomosed to the residual supracoronary region of aorta and the pre-existing saphenous vein grafts were mobilised on an island of relatively healthy aorta and sutured onto the aortic graft itself. However, the TAVI balloon in the abdominal aorta could not be retrieved during the same procedure. The patient was managed in intensive care post-operatively and upon discussion with the vascular surgical team, a decision was made to retrieve the aortic valve balloon percutaneously via a transfemoral approach. The balloon was snared up to the aortic bifurcation using an En Snare® (Merit Medical, Utah, USA) but could not be extricated beyond the aortic bifurcation (Fig. 2a). A laparotomy was performed and the infrarenal abdominal aorta was exposed through a trans-peritoneal approach. Despite the aortic dissection, all visceral branches of the aorta were patent and an anterior longitudinal aortotomy was performed to retrieve the balloon. The false lumen of the dissection at the level of the infrarenal aorta was then was tacked to the aortic adventitial wall using an interrupted prolene suture. The aorta was closed primarily in a single layer. While on the operating table, it was noted that the femoral pulse was weak on the left side and nearly impalpable on the right side. An aortogram demonstrated that the dissection had further extended up to the proximal third of both common iliac arteries and was now compromising flow into the lower limbs. Advanta V12 (Atrium Medical Corp, Hudson, NH) balloon-expandable covered stents were deployed in both common iliac arteries in a ‘kissing’ configuration and lower limb blood flow was re-established (Fig. 2b). The outcome was satisfactory and patient was transferred to the high dependency ward stable with strong, bilateral femoral pulses. Despite a prolonged inpatient stay and rehabilitation, the patient ultimately made a good recovery. He spends 15 days in ICU and the full hospital stay was 30 days.
Fig. 1.
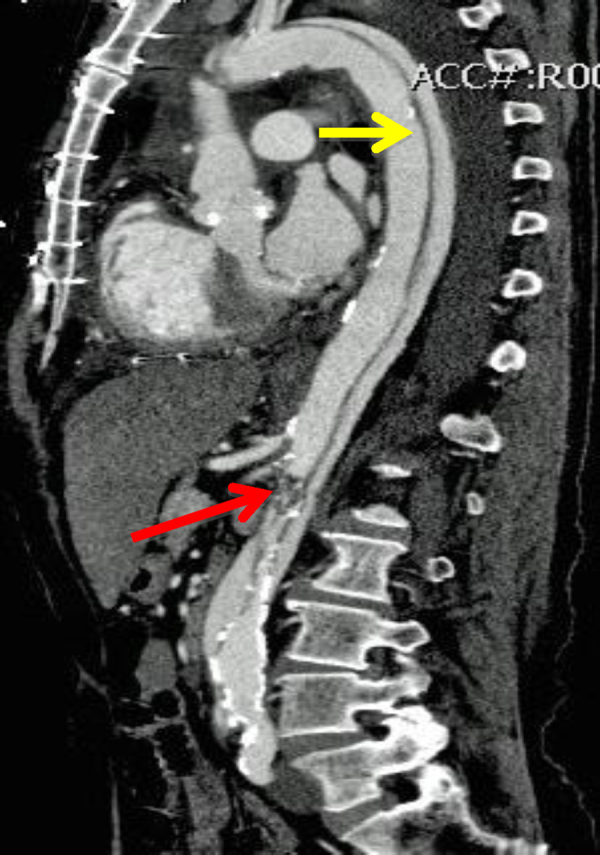
The balloon cone can easily be seen in the coronal view, which showed a filling defect (red arrow), just adjacent to the SMA and renal arteries. The dissection is clearly visualised with the mesenteric vessels originating from the true lumen (yellow arrow). (For interpretation of the references to color in figure legend, the reader is referred to the web version of the article.)
Fig. 2.
(a) The balloon cone (red arrow) could not be snared beyond the aortic bifurcation. (b) Completion angiogram after retrieval of the balloon through an opened aortotomy, then follow by aorto-iliac kissing stenting with Advanta V12 stents (9 mm × 59 mm). (For interpretation of the references to color in figure legend, the reader is referred to the web version of the article.)
3. Discussion
TAVI is a challenging and evolving technique. With increased understanding and experience of the technique, success rates of the procedure are improving. Zahn et al. recently published the biggest reported series of TAVIs in a multi-centre registry. From 666 patients who underwent percutaneous TAVIs, they reported a technical success rate was 95.6%.4 The in-hospital mortality was considerably less via a transfemoral route (7.5%) compared to trans-apical TAVIs (22.6%).4 Al Ali et al. have described that an initial positioning error and utilizing an undersized valve are the two most frequent factors associated with valve malposition.5 It was also found that the incidence of subvalvular malposition and ventricular embolization was more frequently observed using the transapical route as the prosthetic valve does not move toward the aorta during balloon inflation as happens in the transfemoral approach.5 Other factors contributing to malposition and hence poorer outcomes include suboptimal visualization, lack of burst pacing, poor timing of balloon inflation, lack of predilatation, and interference from cardiac structures. Our case occurred as a result of multiple factors that include lack of burst pacing and poor timing of balloon inflation. The aortic balloon and the valve had to be removed urgently to avoid ventricular embolization of these structures that can result in a fatal situation.
Careful pre-procedural planning will help to minimize the risk of complications. Embolization is almost always subvalvular in a transapical approach making endoluminal retrieval almost impossible,6 thus careful consideration needs to be made when choosing this approach. Appropriate imaging of the aortic root with angiography, TOE and CTA should be performed, with particular attention to the size and shape of the annulus, as well as the location and distribution of any calcification.7 Careful sizing is essential in achieving good fixation as well as preventing paravalvular regurgitation. At present the method employed is to use a prosthesis that is 10–20% larger than the annulus5.
4. Conclusion
This case has shown clearly that a procedure that is minimally invasive has resulted in a patient undergoing two major surgical procedures but with a satisfactory outcome. The understanding of the complication and the hybrid procedure has resulted in removal of the foreign body and patient survival.
Conflict of interests
Non-financial competing interests.
Funding
None.
Ethical approval
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the series editor of this journal.
Authors’ contributions
RN participated in the coordination and helped to draft the manuscript JLP helped to draft the manuscript, VV helped to draft the manuscript and BPM finalize the manuscript and prepare the figures. All authors read and approved the final manuscript.
Footnotes
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
References
- 1.Davies H. Catheter-mounted valve for temporary relief of aortic Insufficiency. Lancet. 1965;1:250. [Google Scholar]
- 2.Cribier A., Eltchaninoff H., Bash A., Borenstein N., Tron C., Bauer F. Percutaneous transcatheter implantation of an aortic valve prosthesis for calcific aortic stenosis: first human case description. Circulation. 2002;106(24):3006–3008. doi: 10.1161/01.cir.0000047200.36165.b8. [DOI] [PubMed] [Google Scholar]
- 3.Bleiziffer S., Ruge H., Mazzitelli D., Schreiber C., Hutter A., Laborde J.C. Results of percutaneous and transapical transcatheter aortic valve implantation performed by a surgical team. European Journal Cardio-Thoracic Surgery. 2009;35(4):615–620. doi: 10.1016/j.ejcts.2008.12.041. [DOI] [PubMed] [Google Scholar]
- 4.Zahn R., Gerckens U., Grube E., Linke A., Sievert H., Eggebrecht H. Transcatheter aortic valve implantation: first results from a multi-centre real-world registry. European Heart Journal. 2011;32(2):198–204. doi: 10.1093/eurheartj/ehq339. [DOI] [PubMed] [Google Scholar]
- 5.Al Ali A., Altwegg L., Horlick E., Feindel C., Thompson C.R., Cheung A. Prevention and management of transcatheter balloon expandable aortic valve malposition. Catheterization and Cardiovascular Interventions. 2008;72(4):573–578. doi: 10.1002/ccd.21667. [DOI] [PubMed] [Google Scholar]
- 6.Masson J.B., Kovac J., Schuler G., Ye J., Cheung A., Kapadia S. Transcatheter aortic valve implantation: review of the nature, management and avoidance of procedural complications. JACC: Cardiovascular Interventions. 2009;2(9):811–820. doi: 10.1016/j.jcin.2009.07.005. [DOI] [PubMed] [Google Scholar]
- 7.Tuzcu E.M. Transcatheter aortic valve replacement malposition and embolization: innovation brings solutions also new challenges. Catheterization and Cardiovascular Interventions. 2008;72(4):579–580. doi: 10.1002/ccd.21788. [DOI] [PubMed] [Google Scholar]



