Abstract
INTRODUCTION
Lumbar hernia is a rare complication that can occur after breast reconstruction using a latissimus dorsi flap. The defect occurs within the superior lumbar triangle and may result in visceral incarceration.
PRESENTATION OF CASE
We report a 61-year-old female who presented with a left sided lumbar bulge and pain 7 years following a modified radical mastectomy and latissimus dorsi flap reconstruction. Computed tomography demonstrated a lumbar hernia with incarcerated colon. The patient underwent a successful laparoscopic repair with prosthetic mesh underlay.
DISCUSSION
Lumbar hernias may be congenital, secondary to trauma or prior surgery. Imaging studies assist in excluding soft tissue tumors, infections, hematoma or abdominal wall denervation atrophy, which may also present as a lumbar bulge. Repair may be performed in an open, laparoscopic or retroperitoneoscopic approach.
CONCLUSION
Laparoscopic lumbar hernia repair with mesh is a safe and feasible way to manage an uncommon complication after breast reconstruction with a latissimus flap.
Keywords: Lumbar hernia, Breast reconstruction, Laparoscopy
1. Introduction
Latissimus dorsi flaps are commonly performed during breast reconstruction. Lumbar hernia after flap reconstruction remains a rare complication, with only three such cases reported in the literature. Lumbar hernias arise from the posterolateral region of the abdominal wall. This region is defined by the 12th rib superiorly, the iliac crest inferiorly, the posterior border of the external oblique anteriorly and the lateral border of the erector spinae muscles posteriorly.1 The region is also subdivided into a superior triangle (Grynfelt) and an inferior triangle (Petit). The latissimus dorsi muscle defines the roof of the superior lumbar triangle and mobilization of this muscle can predispose the patient to herniation.2 We report a case of a lumbar hernia after breast reconstruction with latissimus dorsi flap reconstruction who underwent successful repair via a laparoscopic approach.
2. Presentation of case
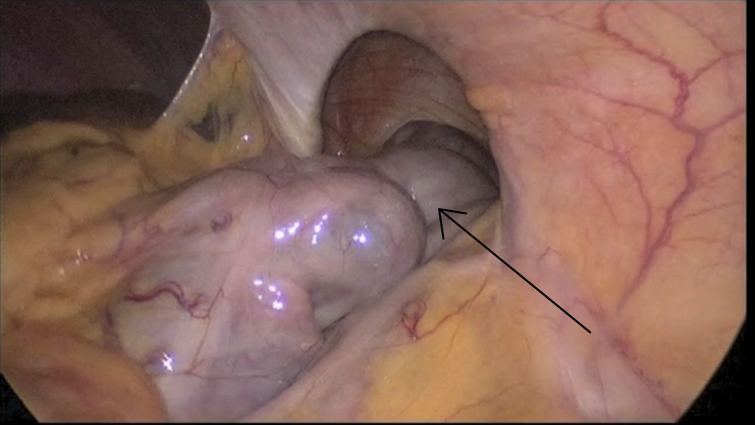
A 61-year-old female with a history of breast cancer underwent a left breast modified radical mastectomy and subsequent staged latissumus dorsi flap reconstruction. Seven years after her reconstruction, she presented with left sided flank pain and a palpable bulge on exam. A CT scan revealed a lumbar hernia with incarcerated colon (Fig. 1). The patient had no previous history of abdominal surgery although she did undergo adjuvant chemotherapy and radiation after her mastectomy.
Fig. 1.
CT of the abdomen demonstrating a left lumbar hernia with incarcerated colon (arrow).
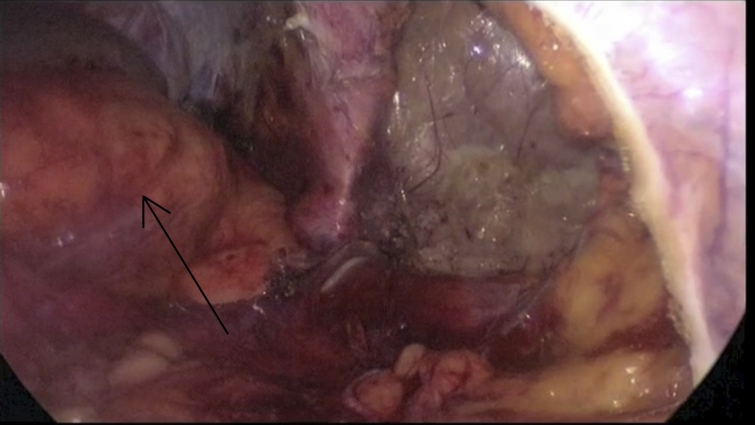
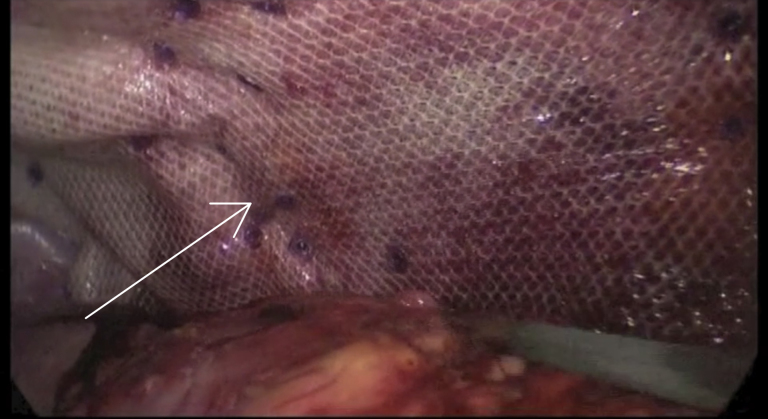
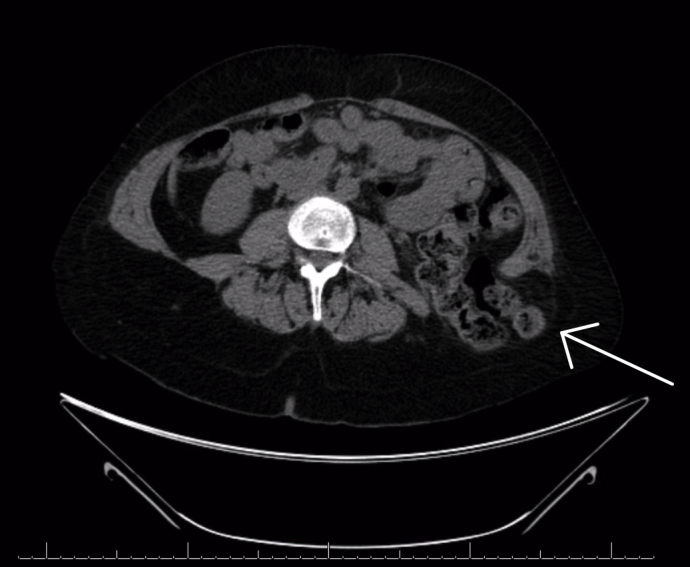
An uncomplicated laparoscopic lumbar hernia repair was performed through 4 ports using a 5 mm 30° laparoscope. The hernia defect measured 5 cm × 7 cm and the sigmoid colon was found incarcerated and adhered to the hernia sac (Fig. 2). After reducing the sigmoid colon and mobilizing the kidney, (Fig. 3) the herniorrhaphy was performed by securing a 20 cm × 25 cm polyester mesh as an underlay with absorbable tacks and transfascial sutures (Fig. 4). The length of the operation was 110 min and blood loss was minimal. The patient was discharged home on postoperative day #3 and has had no recurrence or complications at 6 months.
Fig. 2.
Lumbar hernia identified during laparoscopy. Incarcerated colon is noted in the within the hernia defect (arrow).
Fig. 3.
Lumbar hernia with colon reduced and kidney (arrow) mobilized to allow for adequate placement of mesh.
Fig. 4.
Completed laparoscopic lumbar hernia repair with mesh (arrow).
3. Discussion
Lumbar hernias are rare and may be congenital or acquired.1,3–5 Fewer than 300 cases have been reported in the literature an only three such cases have been reported after latissimus dorsi flap reconstruction.2,4,6,7 This complication can be avoided with proper harvesting of the latissimus flap by dissecting along the deep surface of the latissimus dorsi muscle first and then by transecting the aponeurosis from this deeper plane to prevent compromising the deeper fascia where the two are joined.2 However, lumbar hernias may occur after other surgical procedures such as nephrectomy, adrenalectomy, aortic aneurism repair or iliac crest bone harvesting.8
Patients may present with pain, a palpable or reducible bulge or even with intestinal obstruction.3,5,6,9 Pain may occur along the sciatic nerve distribution or along the anterior abdomen if viscera are incarcerated.10 Imaging studies such as computed tomography (CT) assists in confirming the diagnosis as well as the identifying the presence of incarcerated or strangulated viscera.11 Differential diagnosis includes tumor (i.e. lipoma, fibroma, sarcoma, rhabdomyoma, renal tumor), hematoma, abscess, renal hydrocele, panniculitis or pannicular lumbosacriliac hernia.10–14 Finally, lumbar hernias must be distinguished from abdominal wall denervation atrophy, as this may present as an abdominal wall bulge but does not incur a true fascial defect.12
Lumbar hernias are managed operatively and can be repaired using either an open, laparoscopic or retroperitoneoscopic approach.9,10,15–18 Laparoscopy offers many advantages including optimal exposure and characterization of the hernia defect as well as identification of its contents. It also permits an underlay repair and mesh fixation that can extend beyond the limits of the defect, ideally greater than 5 cm. Finally, a minimally invasive approach often results in less incisional pain, shorter hospital stays and fewer wound complications.
4. Conclusions
Breast reconstruction with latissimus dorsi flap may result in a lumbar hernia, which can cause pain and visceral incarceration. Imaging studies assist with the diagnosis and also rules out other causes of posterolateral abdominal wall bulging. Laparoscopic management of lumbar hernias is ideal as it provides optimal exposure of the defect, allows for an underlay repair with prosthetic mesh and can be done with less chance for wound complications.
Conflict of interest statement
None.
Funding
None.
Ethical approval
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Author contributions
Varban O – First author and faculty surgeon in charge of the patient's care. Primary surgeon who performed the operation and provided follow up care. Obtained consent, diagnostic and intraoperative imaging. Performed literature review.
Footnotes
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
References
- 1.SWARTZWT Lumbar hernias. Journal of Kentucky State Medical Association. 1954;52:673–678. [PubMed] [Google Scholar]
- 2.Mickel T.J., Barton F.E.J., Rohrich R.J., Daniel L.B., Conner W.C. Management and prevention of lumbar herniation following a latissimus dorsi flap. Plastic and Reconstructive Surgery. 1999;103:1473–1475. doi: 10.1097/00006534-199904050-00018. [DOI] [PubMed] [Google Scholar]
- 3.Consiglio G., Consiglio L., Consiglio R. Congenital and spontaneous acquired lumbar hernias. (Clinical contribution: three cases) Policlinico Chir. 1965;72:366–380. [PubMed] [Google Scholar]
- 4.Ponka J.L. WB Saunders; Philadelphia: 1980. Hernias of the Abdominal Wall. [Google Scholar]
- 5.Teo K.A., Burns E., Garcea G., Abela J.E., McKay C.J. Incarcerated small bowel within a spontaneous lumbar hernia. Hernia. 2010;14:539–541. doi: 10.1007/s10029-009-0581-3. [DOI] [PubMed] [Google Scholar]
- 6.Delabrousse E., Sarlieve P., Rodiere E., Michalakis D., Boulahdour Z., Kastler B. Large bowel obstruction secondary to lumbar hernia following latissimus dorsi flap. Journal de Radiologie. 2005;86:167–169. doi: 10.1016/s0221-0363(05)81338-1. [DOI] [PubMed] [Google Scholar]
- 7.Salimbeni G. Lumbar hernia after latissimus dorsi flap dissection. Plastic and Reconstructive Surgery. 2000;105:1572. doi: 10.1097/00006534-200004040-00065. [DOI] [PubMed] [Google Scholar]
- 8.Salameh J.R., Salloum E.J. Lumbar incisional hernias: diagnostic and management dilemma. Journal of the Society of Laparoendoscopic Surgeons. 2004;8:391–394. [PMC free article] [PubMed] [Google Scholar]
- 9.Mismar A., Al-Ardah M., Albsoul N., Younes N. Underlay mesh repair for spontaneous lumbar hernia. International Journal of Surgery Case Reports. 2013;4:534–536. doi: 10.1016/j.ijscr.2013.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Heniford B.T., Iannitti D.A., Gagner M. Laparoscopic inferior and superior lumbar hernia repair. Archives of Surgery. 1997;132:1141–1144. doi: 10.1001/archsurg.1997.01430340095017. [DOI] [PubMed] [Google Scholar]
- 11.Baker M.E., Weinerth J.L., Andriani R.T., Cohan R.H., Dunnick N.R. Lumbar hernia: diagnosis by CT. American Journal of Roentgenology. 1987;148:565–567. doi: 10.2214/ajr.148.3.565. [DOI] [PubMed] [Google Scholar]
- 12.Moreno-Egea A., Baena E.G., Calle M.C., Martinez J.A., Albasini J.L. Controversies in the current management of lumbar hernias. Archives of Surgery. 2007;142:82–88. doi: 10.1001/archsurg.142.1.82. [DOI] [PubMed] [Google Scholar]
- 13.Sharma A., Panse R., Khullar R., Soni V., Baijal M., Chowbey P.K. Laparoscopic transabdominal extraperitoneal repair of lumbar hernia. Journal of Minimal Access Surgery. 2005;1:70–73. doi: 10.4103/0972-9941.16530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zhou X., Nve J.O., Chen G. Lumbar hernia: clinical analysis of 11 cases. Hernia. 2004;8:260–263. doi: 10.1007/s10029-004-0230-9. [DOI] [PubMed] [Google Scholar]
- 15.Bickel A., Haj M., Eitan A. Laparoscopic management of lumbar hernia. Surgical Endoscopy. 1997;11:1129–1130. doi: 10.1007/s004649900547. [DOI] [PubMed] [Google Scholar]
- 16.Cavallaro G., Sadighi A., Miceli M., Burza A., Carbone G., Cavallaro A. Primary lumbar hernia repair: the open approach. European Surgical Research. 2007;39:88–92. doi: 10.1159/000099155. [DOI] [PubMed] [Google Scholar]
- 17.Garg C.P., Sharma P., Patel G., Malik P. Sutureless meshplasty in lumbar hernia. Surgical Innovation. 2011;18:285–288. doi: 10.1177/1553350610397214. [DOI] [PubMed] [Google Scholar]
- 18.Zhou X., Zhang J., Hu H. Kugel patch repair of superior lumbar hernias. Hernia. 2013 doi: 10.1007/s10029-013-1056-0. [DOI] [PubMed] [Google Scholar]