Abstract
INTRODUCTION
Polyethylene (PE) wear debris after total hip arthroplasty (THA) may cause formation of a soft tissue mass due to inflammatory reaction. To the best of our knowledge we report the first case in whom the diagnosis was made after examination of the hip, pelvis and lumbar spine with detailed radiological methods and the plain radiographs showed no signs of loosening of the THA.
PRESENTATION OF CASE
We report a 52 years-old woman who presented with a cyst causing sciatic irritation in her gluteal region due to wear debris after THA. Magnetic resonance imaging (MRI) was useful in detecting the cyst. Resolution of the cyst occured after subtotal cystectomy and revision of the acetabular components.
DISCUSSION
Although plain radiographs can show signs of the underlying pathology; such as osteolysis, loosening of the components and wear of the PE liner, they are unable to detect cystic lesions. Cystic lesions may be an early sign of wear debris.
CONCLUSION
This case shows us that sciatic neuropathy with no evidence of nerve root impingement on lumbar MRI in a patient with THA requires also examination of the hip and pelvis with detailed radiological methods, such as MRI, in addition to plain radiography. Removal of the source of debris via revision surgery following subtotal cystectomy leads to the resolution of the remaining portion of the cyst and also relief of the symptoms of sciatic nerve compression.
Keywords: Arthroplasty, Replacement, Hip, Prosthesis failure
1. Introduction
Symptomatic soft tissue masses due to wear debris are a rare complication after total hip arthroplasty (THA). Although intrapelvic cystic lesions secondary to THA wear debris have been well recognized there has been only one report including 3 patients with cysts surrounding the sciatic nerve in the extrapelvic region after THA in the English literature.1–16 Revision of the cemented arthroplasty was undertaken through a posterior approach and cystic mass was found overlying the greater trochanter area coincidentally. To the best of our knowledge we report the first case in whom the diagnosis was made after examination of the hip, pelvis and lumbar spine with detailed radiological methods whereas the plain radiographs showed no signs of loosening of the THA.
2. Case presentation
A 52-year-old female patient was examined in our department 7 years after implantation of bilateral total hip prostheses for severe symptomatic primary osteoarthritis. The implant in each hips consisted of an uncemented titanium alloy expanded acetabular shell (Protek AG, Bern, Switzerland) with a polyethylene (PE) liner and an uncemented titanium alloy femoral stem (Biomet, Warsaw, Indiana) with a 32-mm Co–Cr head. She underwent revision surgery of the left hip due to aseptic loosening. Because the acetabular components were stable, only the femoral stem was replaced. Recovery from the revision surgery was uneventful. Two years later, she was admitted to our hospital with complaints of pain in her left buttock, numbness in her thigh and an inability to walk without using canes on both sides. She had no history of acute trauma. A plain radiograph of her left hip showed a normal position of the THA, no suspicious opacities, and no radiolucencies. There was no eccentric location of the femoral head which indicates the wear of the acetabular liner (Fig. 1). Based on these findings no osteolysis and loosening of the components were considered. Her white blood cell count, C-reactive protein concentration, and erythrocyte sedimentation rate were within normal limits.
Fig. 1.
Anteroposterior radiograph 9 years after the index operation shows no eccentric location of the femoral head or osteolytic lesions of the femur and pelvis.
Magnetic resonance imaging (MRI) showed her lumbosacral region was normal, but a cystic lesion measuring 112 mm × 50 mm was present in her gluteal region. This lesion extended from the posterior aspect of the left hip joint to the gluteus maximus muscle (Fig. 2). An electromyogram (EMG) of her left lower leg was normal, and a technetium bone scan was negative. The cystic lesion was percutaneously aspirated under ultrasound guidance, with 60 ml of dark yellowish but nonpurulent fluid removed. Pathological examination of the aspirate revealed multiple macrophages and necrotic debris. Cultures of the fluid were negative.
Fig. 2.
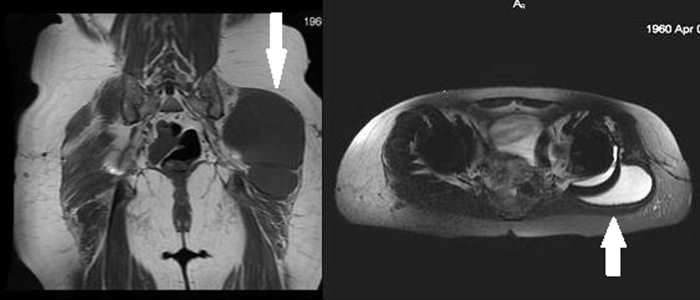
Axial and coronal pelvic MRI showing a cystic mass located in the extrapelvic region extending to the gluteus maximus muscle (white arrows).
The patient experienced apparent relief of hip symptoms after the aspiration. Three months later, however she presented with severe pain in her left buttock radiating to her lower leg. MRI of the left hip revealed recurrence of the cystic lesion indicating the need to excise the lesion. The hip was approached through a posterolateral incision. The cyst was observed to surround the sciatic nerve and was traced to the gluteus maximus muscle. Due to the close proximity of the cyst to the sciatic nerve and abundant soft tissue adhesions, the sciatic nerve could not be identified throughout its trajectory. Subtotal cystectomy was therefore performed. Excision of the cyst with capsulotomy revealed its connection with the joint space. On inspection of the PE and the femoral head, there was minor PE wear at the edge. Because the femoral and acetabular components were stable radiologically, the decision was made to replace only the PE liner. After extracting the liner, cracking of the acetabular shell was observed (Fig. 3). So the acetabular shell and PE were replaced with a hydroxyapatite coated acetabular component fixed with screws due to aseptic acetabular cup loosening. The femoral stem was stable, but the femoral head was exchanged. Histological analysis of the resected cyst showed foreign-body giant cells, along with abundant titanium deposits and PE particles. The patient's postoperative course was symptom free. One year follow-up MRI showed no recurrence of the cystic mass.
Fig. 3.

The picture shows the polyethylene wear at the edge of the liner (black arrow) and the crack pattern in the shell (red arrow).
3. Discussion
The biologic response to wear response is complex and incompletely understood. PE wear debris may cause the formation of a soft tissue mass due to inflammatory reaction.14 Wear debris may function as a foreign body, and be; phagocytosed by macrophages, resulting in a granulomatous reaction. Increases in inflammatory mediators, including interleukin (IL)-1, prostaglandin (PG)-E2 and IL-6 have ben reported to aggravate the inflammatory response.15,17 In this patient suboptimal support of the acetabular shell may have contributed to cystic lesion development due to increased formation of wear debris.
There have been several case reports describing the development of cystic lesions after THA due to PE wear debris.1–3 In nearly all cases, the main patient complaints were leg pain and inability to walk without aid.1,2,4 Symptoms were associated with the size and location of each cystic lesion, due to compression of the surrounding structures. Patients also reported neurological deficits, femoral vein thrombosis and urogenital and gastrointestinal symptoms.1,2,5–9 Most of these cystic lesions were located in the intrapelvic region.10–12 In contrast the cyst in our patient was in the extrapelvic region surrounding the sciatic nerve and extending to the gluteus maximus muscle, causing sciatic neuropathy. Fischer et al.2 described a patient with sciatic neuropathy following compression by an intrapelvic mass of wear debris. The first symptoms started 7 years after the index THA and the radiograph showed eccentric wear of acetabular liner and osteolytic lesions of the femur and pelvis but the diagnosis was delayed and the patient underwent a laminectomy without relief of symptoms before an abdominopelvic computed tomography scan revealed the mass. Two cases of Crawford et al.16 had received THA 12 years previously and the third case had undergone THA 18 years before. Plain radiographs of the three patients revealed loosening of the prosthesis. Nazarian and Zeni10 reported a case of a large intrapelvic cyst 15 years after substantial wear of the PE liner with radiological evidence of osteolysis. And also Fokter et al.1 decribed a patient who had femoral neuropathy secondary to wear debris 13 years after THA. The plain radiograph showed signs of prosthesis loosening. Osteolytic defects were filled with massive morsellized allograft bone. Nehme et al.11 presented a case of intrapelvic synovial cyst 3 years after THA without radiographic evidence of PE wear or osteolysis. Intra or extrapelvic cystic lesions without radiological evidence of prosthesis loosening may allow early diagnosis of problems related to PE wear. When component malalignment and osteolysis are present, a more extensive revision may be warranted.
We were unable to perform a total cystectomy in our patient due to abundant soft tissue adhesions and the close proximity of the cyst to the sciatic nerve. Follow-up radiological examination showed that the remaining portion of the cyst resolved after exchange of the acetabular shell and polyethylene liner. Similar resolutions of remaining cystic portions after subtotal cystectomy and revision of the components have been described.2,13
The design of the titanium alloy expanded acetabular shell would likely affect the degree of PE liner wear.14 Expanded acetabular shells with multiple holes were reported to be unable to support PE liners sufficiently and could increase the amount of wear debris due to suboptimal locking and micromotion at the nonarticular interface.1 In addition, our patient underwent the index operation at a young age with higher demands in daily life, which have contributed to PE liner wear. Highly crosslinked PE would be a good option for this patient because highly crosslinked PE liners substantially reduce overall wear and wear rates.18
Catastrophic acetabular component breakage of the expansion cup secondary to severe liner wear and acetabular osteolysis is well described in the literature.19–21 The expansion acetabular component consists of six titanium lobes connected at the pole. Each of these lobes has three rows of antirotation spikes on its convex side. The inner surface is threaded to capture the PE insert. When the insert is screwed in place, the cup expands and mechanical stability is achieved by means of purchase of the sharp antirotation spikes on the bony acetabulum. The metal back is provided with a porous surface to promote bone ingrowth. Since the expansion cup is not rigid, it can match the elasticity of the iliac bone, minimizing the relative movement between the implant and the pelvis.19 Fatigue fracture is favoured by this typical structure, elasticity, and thinness of the expansion cup.19 In our case the operation was performed by the senior orthopaedic surgeon and overturning to expand the cup was avoided. No signs of a production or material failure was observed in the revision surgery. The accelerated wear led to complete PE wear-through and direct contact between the metallic head and the titanium lobe of the acetabular shell, which was weakened and which ultimately cracked. We believe that cracking was an indicator of future catastrophic failure.
Although plain radiographs can show signs of the underlying pathology; such as osteolysis, loosening of the components and wear of the PE liner, plain radiographs alone are unable to detect cystic lesions. There are also cases similar to ours without signs of osteolysis and loosening of the components.11,15 Examination by ultrasound (US), computed tomography (CT), MRI and/or arthrography may assist in diagnosis, preoperative planning and management of follow-up. US is usually the first modality used to demonstrate the nature of a palpable mass and its relationship to adjacent structures.14 Both CT and MRI are reliable methods of radiological diagnosis, delimitating the mass and revealing its walls and fluid content. These modalities can help to distinguish among cysts, neoplasms, hematomas and aneurysms. MRI can also show the communication between the cystic lesion and the articular cavity minimizing the need for arthrography.14
4. Conclusion
This case shows us that sciatic neuropathy with no evidence of nerve root impingement on lumbar MRI in a patient with THA requires also examination of the hip and pelvis with detailed radiological methods, such as US, CT or MRI, in addition to plain radiography. An extrapelvic location of a cyst secondary to wear debris in a patient without radiological findings of the loosening of the THA is even a sign of early damage of the acetabular liner and shell. Awareness on the part of nonorthopaedic physicians may also aid in prompt diagnosis and prevent the delay in the diagnosis of wear debris. In such situations revision surgery is more easy due to the nonexistance of osteolysis and there is no need for bone grafting in most cases. Removal of the source of debris via revision surgery with a posterior approach following subtotal cystectomy may lead to the resolution of the remaining portion of the cyst and also relief of the symptoms of sciatic nerve compression. We believe the findings of our case should be useful for a broad spectrum of medical specialities, including orthopaedics, neurology, neurosurgery, radiology and general surgery.
Conflict of interest
None declared.
Funding
None.
Ethical approval
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editor-in chief of this journal on request.
Author contributions
Murat Mert wrote the manuscript. Study design was done by Yusuf Öztürkmen. Images and network were designed by Ethem A. Ünkar and Sinan Erdoğan. Onat Üzümcügil supervised the study.
Footnotes
This is an open-access article distributed under the terms of the Creative Commons Attribution-NonCommercial-No Derivative Works License, which permits non-commercial use, distribution, and reproduction in any medium, provided the original author and source are credited.
References
- 1.Fokter S.K., Repse-Fokter A., Takac I. Case report: femoral neuropathy secondary to total hip arthroplasty wear debris. Clinical Orthopaedics and Related Research. 2009;467:3032–3035. doi: 10.1007/s11999-009-0894-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fischer S.R., Christ D.J., Roehr B.A. Sciatic neuropathy secondary to total hip arthroplasty wear debris. Journal of Arthroplasty. 1999;14(6):771–774. doi: 10.1016/s0883-5403(99)90237-1. [DOI] [PubMed] [Google Scholar]
- 3.Lin K.H., Lo N.N. Failure of polyethylene in total hip arthroplasty presenting as a pelvic mass. Journal of Arthroplasty. 2009;24(7) doi: 10.1016/j.arth.2008.06.029. 1144.e13–5. [DOI] [PubMed] [Google Scholar]
- 4.Skiadas V., Koutoulidis V., Plotas A. An atypical case of noninfected iliopsoas bursitis – MRI findings. Journal of Radiology Case Reports. 2009;3(10):15–18. doi: 10.3941/jrcr.v3i10.326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Beksac B., Tozun R., Baktiroglu S., Sener N., Gonzalez Della Valle A. Extravascular compression of the femoral vein due to wear debris induced iliopsoas bursitis: a rare cause of leg swelling after total hip arthroplasty. Journal of Arthroplasty. 2007;2(3):453–456. doi: 10.1016/j.arth.2006.04.002. [DOI] [PubMed] [Google Scholar]
- 6.Regis D., Sandri A., Costa A., Bartolozzi P., Mazzilli G. Recurrent femoral deep vein thrombosis: rare complication of a pelvic mass induced by polyethylene wear debris following total hip arthroplasty. A case report. Thrombosis Research. 2008;121(4):593–595. doi: 10.1016/j.thromres.2007.05.024. [DOI] [PubMed] [Google Scholar]
- 7.Lax-Pérez R., Salinas-Gilabert J.E., Lajara-Marco F., Lax-Pérez A., Corraliza-Zamorano A., García-Gálvez A. Thrombosis of the superficial femoral vein due to psoas bursitis secondary to particle disease in total hip arthroplasty. Acta Ortopaedica Mexicana. 2011;25(3):180–183. [PubMed] [Google Scholar]
- 8.Hananouchi T., Saito M., Nakamura N., Yamamoto T., Yonenobu K. Huge pelvis mass secondary to wear debris causing ureteral obstruction. Journal of Arthroplasty. 2005;20(7):946–949. doi: 10.1016/j.arth.2004.11.005. [DOI] [PubMed] [Google Scholar]
- 9.Hattrup S.J., Bryan R.S., Gaffey T.A., Stanhope C.R. Pelvic mass causing vesical compression after total hip arthroplasty. Case report. Clinical Orthopaedics and Related Research. 1988;227(2):184–189. [PubMed] [Google Scholar]
- 10.Nazarian D.G., Zeni J.A.J.R. Management of a pelvic mass following a worn uncemented total hip arthroplasty. Journal of Arthroplasty. 2012;27(2) doi: 10.1016/j.arth.2011.03.023. 323.e17–20. [DOI] [PubMed] [Google Scholar]
- 11.Nehme A., Oakes D.A., Marcheix B., Gomez-Brouchet A., Puget J. Compressive intrapelvic synovial cysts: an early complication of an HA-coated cup. Clinical Orthopaedics and Related Research. 2005;430(1):232–236. [PubMed] [Google Scholar]
- 12.Liman J., von Gottberg P., Bähr W., Kermer P. Femoral nerve palsy caused by ileopectineal bursitis after total hip replacement: a case report. Journal of Medical Case Reports. 2011;18(5):190. doi: 10.1186/1752-1947-5-190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Leigh W., O’Grady P., Lawson E.M., Hung N.A., Theis J.C., Matheson J. Pelvic pseudotumor: an unusual presentation of an extra-articular granuloma in a well-fixed total hip arthroplasty. Journal of Arthroplasty. 2008;23(6):934–938. doi: 10.1016/j.arth.2007.08.003. [DOI] [PubMed] [Google Scholar]
- 14.Jacobs J.J., Shanbhag A., Glant T.T., Black J., Galante J.O. Wear debris in total joint replacements. Journal of the American Academy of Orthopaedic Surgeons. 1994;2(4):212–220. doi: 10.5435/00124635-199407000-00004. [DOI] [PubMed] [Google Scholar]
- 15.Gruber F.W., Böck A., Trattnig S., Lintner F., Ritschl P. Cystic lesion of the groin due to metallosis: a rare long-term complication of metal-on-metal total hip arthroplasty. Journal of Arthroplasty. 2007;22(6):923–927. doi: 10.1016/j.arth.2006.10.002. [DOI] [PubMed] [Google Scholar]
- 16.Crawford J.R., Van Rensburg L., Marx C. Compression of the sciatic nevre by wear debris following total hip replacement: a report of three cases. Journal of Bone and Joint Surgery British Volume. 2003;85(8):1178–1180. doi: 10.1302/0301-620x.85b8.13638. [DOI] [PubMed] [Google Scholar]
- 17.Crawford R., Sabokbar A., Wulke A., Murray D.W., Athanasou N.A. Expansion of an osteoarthritic cyst associated with wear debris. A case report. Journal of Bone Joint Surgery British Volume. 1998;80(6):990–993. doi: 10.1302/0301-620x.80b6.8905. [DOI] [PubMed] [Google Scholar]
- 18.Mall N.A., Nunley R.M., Zhu J.J., Maloney W.J., Barrack R.L., Clohisy J.C. The incidence of acetabular osteolysis in young patients with conventional versus highly crosslinked polyethylene. Clinical Orthopaedics and Related Research. 2011;469:372–381. doi: 10.1007/s11999-010-1518-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mariconda M., Silvestro A., Mansueto G., Marinó D. Complete polyethylene wear-through and secondary breakage of the expansion cup in a ceramic–polyethylene total hip arthroplasty. Archives of Orthopaedic Trauma and Surgery. 2010;130:61–64. doi: 10.1007/s00402-009-0843-7. [DOI] [PubMed] [Google Scholar]
- 20.Chotai P., Shon W.Y., Han S.B., Yoon Y.C., Park Y.H., Siddaraju V.M. Catastrophic rupture of a CLS Spotorno acetabular expansion cup in a metal–polyethylene total hip arthroplasty: a case reprt. Journal of Bone and Joint Surgery British Volume. 2012;94(Suppl. 25) [Google Scholar]
- 21.Kim Y.G., Kim S.Y., Kim S.J., Park B.C., Kim P.T., Ihn J.C. The use of cementless expansion acetabular component and an alumina–poyethylene bearing in total hip arthroplasty for osteonecrosis. Journal of Bone Joint Surgery British Volume. 2005;87:776–780. doi: 10.1302/0301-620X.87B6.15380. [DOI] [PubMed] [Google Scholar]



