Abstract
Background
Only a minority of individuals who have substance use disorders receives treatment, and those who do typically have more severe disorders. The current study examines the relationship of help-seeking with remission from alcohol and/or drug dependence and other outcomes.
Methods
Data from the Wave 1 (2001 – 2002) and Wave 2 (2004 – 2005) National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) were used to examine remission at Wave 2 among respondents who had past-year substance dependence disorders at Wave 1 (N=1,262). Multi-group structural equation modeling was used to compare individuals with (n = 356) and without (n = 906) prior help-seeking at Wave 1 on subsequent help-seeking and other factors that influence outcomes.
Results
Baseline help-seekers sought help at higher levels over the follow-up period (31% vs. 8%) and had lower rates of remission (50% vs. 68%), as compared with those without prior help-seeking, respectively. Among baseline help-seekers, there were stronger relationships between baseline stress and mental disorders and having sought help since baseline; age and past-year level of stress at follow-up; level of stress and health status at follow-up; and social support and mental disorders at follow-up. Among baseline non-help-seekers, there were stronger relationships between being female and past-year stress at follow-up, and between having sought help since baseline and physical health status at follow-up.
Conclusions
Findings extend our understanding of the factors associated with recovery from substance dependence, including “natural recovery,” use of services outside of addiction treatment, and gender differences in help-seeking and remission.
Keywords: help-seeking, treatment, substance dependence, remission, recovery, natural recovery
1. INTRODUCTION
Studies of individuals who are in remission from substance use disorders typically have been conducted with samples recruited from treatment settings, with the goal of understanding short- or long-term treatment outcomes. Yet only a minority of individuals with substance use disorders ever receives some form of treatment/services (Kessler et al., 1996; Wang et al., 2005). About one quarter of individuals with alcohol dependence receive treatment over their lifetime, whereas the rate is about 38% for those with drug dependence (Compton et al., 2007; Hasin et al., 2007). Rates of treatment use are even lower when examined for the past year. Findings from the National Survey on Drug Use and Health (NSDUH) show that among the general population, 10.8% of individuals with a past-year alcohol or drug use disorder received treatment from a “specialty” addiction treatment program (Substance Abuse and Mental Health Services Administration [SAMHSA], 2012). However, NSDUH and other cross-sectional surveys are unable to examine longitudinal patterns of help-seeking and remission over time.
Related to remission, which is determined by diagnostic criteria for a substance use disorder (Lopez-Quintero et al., 2011), is “recovery,” the components of which have been examined from the perspective of individuals who identify with this status. Using media-based recruitment, Laudet (2007) found that the predominant definition of “recovery” among a sample of 289 individuals, most of whom had participated in both formal drug treatment and 12-step groups, was strict abstinence from alcohol and drugs. In addition, most individuals in this sample described recovery as a process that results in an improved quality of life. Thus, although abstinence may be one component of recovery, a broader range of outcomes that addresses overall psychosocial functioning needs to be examined (Betty Ford Institute Consensus Panel, 2007; Laudet et al., 2009; White, 2007).
The aim of the current study was to examine the relationship of help-seeking with remission from substance dependence and other indicators of functioning among a longitudinal general population sample. We build upon a prior study that examined help-seeking among participants with alcohol and/or drug dependence disorders at Wave 1 in the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC; Grella et al., 2009). Individuals (N = 1,602) were classified into one of three groups: (1) received any help in the past year (14.7%); (2) perceived a need for help, but did not receive it (8.5%); or (3) had no perceived need for help and no help was received (76.8%). Factors that increased the receipt of help (retrospectively) included: older age, drug dependence (vs. alcohol only), longer time since the onset of dependence, co-occurring mood disorder, and more problems associated with use. Similarly, more problems associated with substance use increased the odds of perceiving a need for help, but not receiving it.
Using the same initial sample, the current study examines the longitudinal relationship of help-seeking with remission and other outcomes. The study is guided by a conceptual model developed by Moos (2007) on the personal and social resources that foster the process of remission from substance use disorders. Moos and Moos (2007) tested this conceptual model in a study of individuals (N = 346) who initiated help-seeking for alcohol-related problems and were subsequently followed-up over 16 years. They found that protective factors associated with social learning (self-efficacy), stress and coping theories (coping skills), behavioral economics (health and financial resources, 12-step resources), and social control theory (bonds with family, friends, coworkers) predicted better alcohol-related and psychosocial outcomes. Similarly, Laudet and White (2008) refer to the construct of “recovery capital” as assets or resources that may help an individual cope with stressors and sustain recovery, which may underlie “natural recovery” in the absence of treatment among some individuals (Granfield and Cloud, 2001).
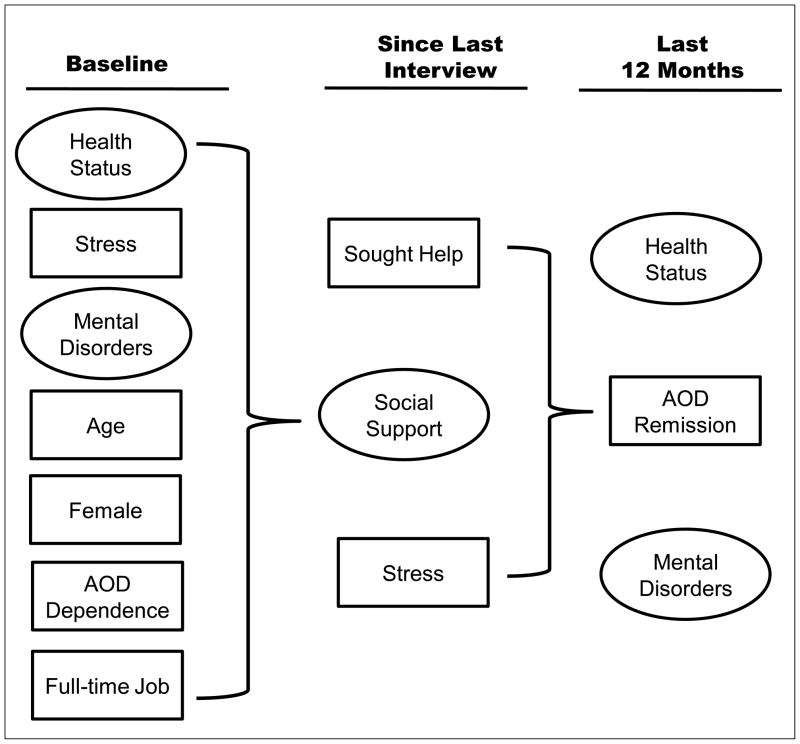
We used the longitudinal NESARC (Waves 1 and 2) study to test this conceptual model (shown in Figure 1). We incorporated variables that have prior empirical support (e.g., employment, stress, social support) to test their association with remission and other outcomes over the follow-up period using multi-group structural equation modeling. Consistent with prior research, we hypothesized that higher levels of social support and stress would be associated (in different directions) with remission and other health outcomes, although the effects of help-seeking, which is typically associated with higher levels of severity, would be indicative of lower likelihood of remission and poorer overall functioning.
Figure 1.
Conceptual model.
Note: AOD stands for alcohol or other drug
2. METHODS
2.1 NESARC study design
NESARC is an in-depth longitudinal epidemiological survey of a representative sample of the United States. The study methodology has been described in detail elsewhere (Grant et al., 2003, 2004). The target population of the NESARC was the civilian, non-institutional adult population of the United States residing in households as well as in group quarters (e.g., group homes, halfway houses). At Wave 1, face-to-face interviews were conducted with 43,093 respondents in 2001–2002 (response rate = 81%). African Americans, Hispanics, and young adults (ages 18–24 years) were over-sampled, with data adjusted for over-sampling and household- and person-level non-response. The weighted data were then adjusted to represent the U.S. civilian population based on the 2000 census. NESARC Wave 2 was conducted in 2004–2005 and had a response rate of 86.7% of those re-eligible for interview. Face-to-face interviews were conducted that contained parallel items to the baseline survey, as well as several additional modules.
2.2. Current study sample
The sample for this study (N = 1,262) includes all individuals in the NESARC Wave 1 sample who met criteria for past-year alcohol and/or drug dependence and who completed a follow-up interview in Wave 2. Thirty-eight percent of the sample was female; the mean age was 33 years (sd = 12.2). Thirty-two percent were married; the sample was 18% African-American, 61% Caucasian, and 20% Hispanic. Fifty-eight percent were employed full-time. Eighty-two percent had a high school diploma or GED or more (technical training, some college, college degree).
This sample was grouped on the basis of their response in the baseline survey to: Have you ever gone anywhere or seen anyone for a reason that was related in any way to use your use of [medicines/drugs or alcohol]. Responses comprise 12 forms of help/services, including specialty addiction treatment, 12-step groups, and other types of services1. Two groups were formed comprising individuals who had sought help from any source for either alcohol or drug problems (n = 356, 28.2%) and those who had not (n = 906, 71.8%).
2.3. Diagnostic assessment
The Alcohol Use Disorder and Associated Disabilities Interview Schedule – DSM-IV Version (AUDADIS-IV) was used to diagnose past-year alcohol or drug dependence at both Waves 1 and 2 (Grant and Hasin, 1991). The AUDADIS-IV includes an extensive list of symptom questions that separately operationalizes DSM-IV criteria for abuse and dependence on alcohol and 10 classes of illicit or prescription drugs. Consistent with the DSM-IV, AUDADIS-IV past-year dependence diagnoses required at least 3 of the 7 DSM-IV criteria for dependence to be met during the past year.
The AUDADIS-IV was also used to generate mental health diagnoses including: lifetime (at Wave 1) and past-year (at Wave 2) major depression, dysthymia, and generalized anxiety disorders. Mood and anxiety diagnoses in NESARC are consistent with the DSM-IV criteria for “primary” or independent diagnosis, meaning those mental disorders that were substance-induced due to a general medical condition or entirely accounted for by bereavement were excluded (Grant et al., 2004). Numerous studies conducted with clinical and general population samples have demonstrated good-to-excellent reliability and validity of the AUDADIS-IV diagnoses (Grant et al., 2003).
2.4. Variables
2.4.1. Baseline (Wave 1)
Demographics
Baseline demographic indicators included age in years at entry into the study and gender (male = 0, female = 1). Employment status was indicated by whether he/she had a full-time job (no = 0, yes = 1). Other demographics (i.e., education, marital status, and ethnicity) were not significant predictors of the outcomes of the study and were dropped for model parsimony.
Physical health
Health status was represented by a latent variable comprising 5 items taken from the SF-12 Health Survey - Physical Functioning Scales (Ware et al., 1996). One item assessed self-reported appraisal of participants’ overall physical health status (scaled 1–5), two items asked participants to assess their ability to perform various daily activities (scaled 1–3), and two items asked participants to assess how much time and to what extent health problems had limited their activities in the past 4 weeks (scaled 1–5).
Stress
Respondents were asked whether they had experienced any of 12 types of stressful life events relating to health, social, job, or legal situations during the 12 months preceding the Wave 2 interview, scored as yes/no (Dawson et al., 2005). A summative score of positive responses was created (coefficient alpha = 0.81).
Mental disorders
Three conditions were used as indicators of mental disorders, based on diagnoses using the AUDADIS: major depression, dysthymia, and generalized anxiety.
Degree of dependency ranged from 1–7 and indicated the severity of dependence in terms of the number of substance-dependence disorders reported at baseline. The scale ranged from 1–7, with 1 = one substance of dependence (alcohol or drug); 2 = 2 drugs or 1 drug and alcohol dependence, etc. The modal value was 1 (91.6%); 6.7% had a score of 2, .87% had a 3, and less than 1% had values greater than 3.
2.4.2. Since last interview
Help-seeking was assessed at Wave 2 in the same manner as at baseline, with reference to the period since the baseline interview.
Social support was assessed at Wave 2 by the Interpersonal Support Evaluation List–12 (Cohen et al., 1985), which measures respondents’ perceptions of the social resources available to them (Ruan et al., 2008). Four parcels were randomly created from the 12 items (coefficient alpha = .83). Items were scaled from 1–4 (1 = definitely false, 2 = probably false, 3 = probably true, 4 = definitely true). Items were rescaled when necessary so that high responses meant better social support. Parcels were created to avoid too many indicators in the model. Parceling is acceptable when the coefficient alpha is high (Yuan et al., 1997).
Stress was assessed in the same manner at Wave 2 as baseline, with reference to the prior 12 months (Ruan et al., 2008).
2.4.3. Follow-up (Wave 2)
Physical Health was assessed in the same manner as it was assessed at baseline. Mental Health Disorders consisted of diagnoses of past-year major depression, dysthymia, and generalized anxiety. Remission was defined as no longer meeting DSM-IV criteria for an alcohol or drug dependence disorder (past 12 months) at the Wave 2 assessment.
2.5. Analyses
2.5.1. General approach
Help-seekers (HS) and non-help-seekers (NHS) were analyzed separately and then contrasted in multi-sample models. The analyses were performed using the EQS structural equations program (Bentler, 2006). Goodness-of-fit of the models was assessed with the maximum-likelihood χ2, the Comparative Fit Index (CFI), the Satorra-Bentler χ2(S -B χ2), the Robust Comparative Fit Index (RCFI), and the root mean squared error of approximation (RMSEA; Bentler, 2006; Bentler and Dudgeon, 1996; Hu and Bentler, 1999). The Robust S-B χ2 was used in addition to the maximum likelihood χ2 because it is more appropriate when the data depart from multivariate normality. Mardia’s normalized multivariate kurtosis estimate was high in both groups (z-statistic= 48.04 [help-seekers], 127.47 [non-help-seekers]) (Bentler and Dudgeon, 1996). The CFI and RCFI range from 0 to 1 and reflect the improvement in fit of a hypothesized model over a model of complete independence among the measured variables. The RCFI adjusts for sample size; values at .95 or greater are desirable for both the CFI and RCFI, indicating that the hypothesized model reproduces 95% or more of the covariation in the data (Hu and Bentler, 1999). The RMSEA is a measure of fit per degrees of freedom, controlling for sample size, and values less than .06 indicate a relatively good fit between the hypothesized model and the observed data (Hu and Bentler, 1999).
Two types of models were compared: (1) confirmatory factor models with no time-ordering and (2) path models. Confirmatory factor analyses examined the correlations among all of the variables in the model, assessing the adequacy of the measurement models for the latent variables within each sample. Then, separate and initially identical predictive structural equation path models were tested in which baseline predictors included gender (female), age in years, employment status (full time job), physical health, stress, and mental disorders. These items predicted the intermediate variables assessed 2 years later (since the last interview) of help-seeking, social support, and stress. In turn, these variables predicted physical health, mental disorders, and remission in the last 12 months. Additional significant predictors of the variables assessed in the last 12 months were added from the baseline variables if they were suggested by the LaGrange Multiplier (LM) test (Chou and Bentler, 1990). Correlations (covariances) that were significant among the predictive background variables and among the outcome variables were retained in these models if they were significant. Nonsignificant paths and correlations in the path models were trimmed gradually, following the model-evaluation procedure of MacCallum (1986).
2.5.2. Multiple group models
We used multiple group assessment techniques to (1) contrast the correlations in the confirmatory models from the two datasets, compare the factor structures, and assess whether there were differences in the latent means of the two groups and (2) compare the parameters in the path models. In both types of models, hypotheses of cross-sample equality were tested, starting with an unrestricted model in which no assumptions were made about the comparability of various parameters across the groups under scrutiny. We then tested more restrictive hypotheses through the use of equality constraints that equated the factor loadings and then the correlations (or path coefficients) among the constructs in the model for the two groups. The plausibility of the equality constraints was determined with the goodness-of-fit indexes described above, chi-square difference tests, and results of the LM test. In the context of a multiple-group analysis, the LM test provides information concerning which equality constraints are not reasonable and should be released to improve the fit of the model. Due to the numerous comparisons in these large models, especially the comparison of correlations between the two groups, a χ2 value of 5.02 was used as the criterion for significance (1 df, p < .025, Z- score equivalent= 1.96) to avoid capitalizing on relatively small chance differences.
3. RESULTS
3.1. Preliminary confirmatory analysis
The initial confirmatory factor models had an excellent fit in both groups: HS: ML χ2 = 370.82, 275 df; CFI = .98, RMSEA = .03; S-B χ2 = 327.74, 275 df; RCFI = .98; RMSEA = .02. NHS: ML χ2= 495.43, 275 df; CFI = .97, RMSEA = .03; S-B χ2 = 407.14, 275 df; RCFI = .97; RMSEA = .02. Table 1 reports summary statistics for each group as well as the factor loadings in the two groups. Table 2 reports the correlations among the variables.
Table 1.
Means or percentages, standard deviations, ranges and factor loadings of measured variables in the Confirmatory Factor Analysis for 1262 individuals with past-year alcohol and/or drug dependence at Wave 1in the National Epidemiologic Survey on Alcohol and Related Conditions.
| Latent and Measured Variables (range) | Help seekers Mean (S. D.)/% | Non-help seekers Mean (S. D.)/% | Help Seekers Factor Loadings | Non-help seekers Factor Loadings |
|---|---|---|---|---|
| Baseline | ||||
| Physical Health | ||||
| Current health assessment (1–5) | 3.28 (1.17) | 3.72 (1.08) | .64 | .56 |
| Moderate activities (1–3) | 2.66 (0.64) | 2.85 (0.45) | .78 | .79 |
| Climbing several flights of stairs (1–3) | 2.63 (0.66) | 2.81 (0.51) | .72 | .74 |
| Accomplished less due to health (1–5) | 3.98 (1.32) | 4.42 (1.02) | .78 | .68 |
| Limited in kind of work could do (1–5) | 4.08 (1.35) | 4.61 (0.92) | .80 | .78 |
| Stress | 3.88 (2.46) | 3.06 (2.21) | __ | __ |
| Mental Disorders (lifetime) | ||||
| Major depression | 54% | 34% | .58 | .59 |
| Dysthymia | 21% | 9% | .73 | .51 |
| Generalized anxiety | 16% | 9% | .58 | .51 |
| Age (years) | 37.0 (12.1) | 31.38 (11.95) | __ | __ |
| Female | 33% | 40% | __ | __ |
| AOD Dependence | 1.23 (0.66) | 1.07 (0.30) | __ | __ |
| Has a full-time job | 55% | 60% | __ | __ |
| Since last interview | ||||
| Sought help | 31% | 8% | __ | __ |
| Social Support | ||||
| Support1 | 3.39 (0.65) | 3.52 (0.57) | .81 | .75 |
| Support2 | 3.29 (0.65) | 3.44 (0.61) | .79 | .74 |
| Support3 | 3.43 (0.60) | 3.61 (0.52) | .82 | .76 |
| Support4 | 3.40 (0.65) | 3.55 (0.56) | .87 | .76 |
| Stress | 3.24 (2.57) | 2.57 (2.25) | __ | __ |
| Last 12 months | ||||
| Physical Health | ||||
| Current health assessment | 3.36 (1.17) | 3.69 (1.06) | .67 | .61 |
| Moderate activities (1–3) | 2.62 (0.78) | 2.80 (0.53) | .74 | .72 |
| Climbing several flights of stairs (1–3) | 2.57 (0.74) | 2.77 (0.55) | .81 | .73 |
| Accomplished less due to health (1–5) | 3.84 (1.30) | 4.21 (1.09) | .68 | .65 |
| Limited in kind of work could do (1–5) | 4.00 (1.31) | 4.44 (1.01) | .80 | .78 |
| AOD Remission | 50.3% | 67.8% | __ | __ |
| Mental Disorders (past-year) | ||||
| Major depression | 25% | 15% | .57 | .70 |
| Dysthymia | 4% | 2% | .39 | .35 |
| Generalized anxiety | 11% | 6% | .58 | .41 |
Note: Factor loadings are standardized; all factor loadings significant, p ≤ .001.
Help seekers N = 356, non help-seekers N = 906.
Table 2.
Correlations among model constructs for 1262 participants with past-year alcohol and/or drug dependence at Wave 1 in the National Epidemiologic Survey on Alcohol and Related Conditions.
| Variables | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Baseline | |||||||||||||
| 1. Physical Health | -- | .01 | −.30c | −.35c | −.06 | −.11 | .42c | −.07 | .22c | −.01 | .74c | .08 | −.19b |
| 2. Stress | −.12c | -- | .22c | −.24c | .10 | .21c | −.09 | .21c | −.03 | .39c | −.02 | −.10 | .26c |
| 3. Mental Disorders | −.43c | .29c | -- | .10 | .34c | .18b | −.14a | .24c | −.21c | .22c | −.31c | −.14a | .58c |
| 4. Age | −.32c | −25c | .20c | -- | −.01 | −.14b | −.14b | .02 | −.13b | −.29c | −.45c | −.06 | −.01 |
| 5. Female | −.12c | .10b | .30c | .03 | -- | .13b | −.10a | −.01 | .01 | .06 | −.11a | .12a | .18b |
| 6. AOD Dependence | −.09b | .15c | .23c | −.09a | .00 | -- | −.12a | .06 | .06 | .12a | −.04 | .02 | .02 |
| 7. Has full-time job | .24c | −.14c | −.14c | .08a | −.12c | −.07a | -- | −.14b | .05 | −.07 | .37c | −.01 | −.17b |
| Since last interview | |||||||||||||
| 8. Sought Help | −.03 | .02 | .07 | .01 | −.05 | .08a | −.02 | -- | −.20c | .20c | −.04 | −.31c | .39c |
| 9. Social Support | .23c | −.05 | −.34c | −.18a | −.07 | .04 | .10b | −.05 | -- | −.15b | .25c | .24c | −.54c |
| 10. Stress | −.08a | .41c | .17c | −.22c | .15c | .13c | −.08a | .13c | −.08a | -- | −.09 | −.21c | .33c |
| Last 12 months | |||||||||||||
| 11. Physical Health | .77c | −.11b | −.33c | −.35c | −.17c | −.09b | .21c | −.13c | .30c | −.11b | -- | .14b | −.21b |
| 12. AOD Remission | .05 | −.04 | −.09a | −.04 | .05 | −.08a | −.03 | −.18c | .13c | −.13c | .10b | -- | −.37c |
| 13. Mental Disorders | −.13b | .20c | .55c | −.04 | .26c | .09a | −.06 | .21c | −.22c | .27c | −.22c | −.22c | -- |
Note: help seekers at baseline above diagonal (N = 356), non help-seekers at baseline below the diagonal (N = 906); Correlations that are significantly different in the 2 groups are in boldface type.
p ≤ .05,
p ≤ .01,
p ≤ .001.
3.2. Multiple group comparison of the factor structure and correlations among the variables
Although model fit continued to be excellent after the imposition of equality constraints on the measurement model, one constraint was reported as untenable and was dropped from the analysis. This was the equality constraint on the factor loading of the lifetime dysthymia indicator on the baseline mental disorders latent variable (.73 in the HS group vs. .51 in the NHS group). When we contrasted the correlations among the variables by constraining the correlations to equality between the groups, only 5 out of the 78 correlations were significantly different using the criterion of χ2 = 5.02 for the univariate test statistic. These included the correlations between baseline stress and help-seeking since last interview (.21 HS, .02 NHS, χ2= 6.13), baseline mental disorders and social support (−.21 HS, −.34 NHS, χ2 = 6.33), age and having a full-time job (−.14 HS, .08 NHS, χ2 = 5.46), help seeking since last interview and physical health last 12 months (−.04 HS, −.13 NHS, χ2 = 7.69), and mental disorders in the last 12 months and social support (−.54 HS, −.22 NHS, χ2 = 8.23).
3.3. Latent means comparison
Once an invariant factor structure was confirmed as described above, we also assessed whether there were significant group differences in the means of the latent constructs in the model as well as demographic differences. Table 3 reports the Z-scores for the latent means comparisons. The NHS group reported better health at Waves 1 and 2 and the HS group reported more mental disorders and stress at both time periods. The HS were significantly older, less likely to be female, and had a greater degree of dependency at baseline. The HS were more likely to have sought further help since their last interview and were less likely to report social support. Members of the NHS group were more likely to be classified as in remission from any alcohol or other drug dependence. There was no difference in whether they had a full-time job.
Table 3.
Z-scores in 2-group means comparisons among help-seeking (N = 356) and non-help-seeking (N = 906) participants with past-year alcohol and/or drug dependence at Wave 1 in the National Epidemiologic Survey on Alcohol and Related Conditions.
| Variable | Help seekers vs. non-help-seekers* |
|---|---|
| Baseline | Z-scores |
| 1. Physical Health | 6.76c |
| 2. Stress | −5.44c |
| 3. Mental Disorders | −6.30c |
| 4. Age | −7.45c |
| 5. Female | 2.20a |
| 6. AOD Dependence | −4.60c |
| 7. Full-time job | 1.60 |
| Since last interview | |
| 8. Sought Help | −8.96c |
| 9. Social Support | 4.57c |
| 10. Stress | −4.27c |
| Last 12 months | |
| 11. Physical Health | 5.72c |
| 12. AOD Remission | 5.69c |
| 13. Mental Disorders | −4.00c |
Note: Positive score indicates higher scores for non-help-seekers. Negative scores indicate higher scores for help-seekers.
p ≤ .05,
p ≤ .01,
p ≤ .001
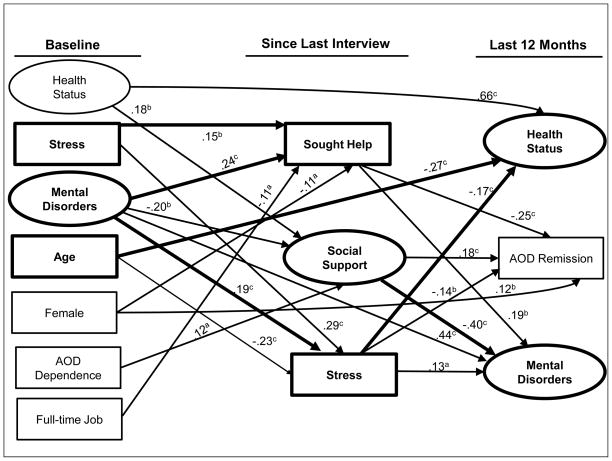
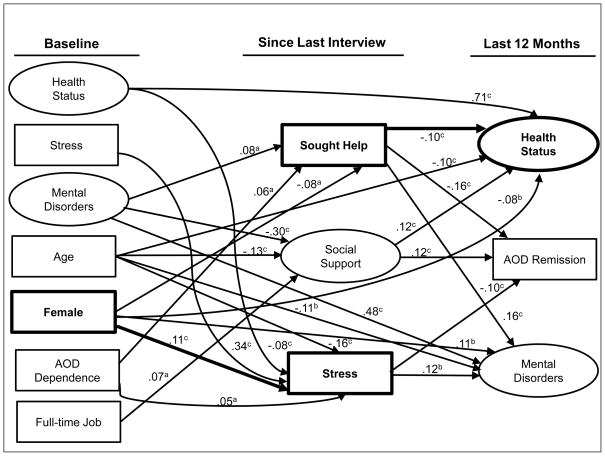
3.4. Path analysis
Figures 2 and 3 depict the results of the predictive path analyses after model trimming for individuals with and without prior help-seeking at baseline (respectively). Both models had excellent fit statistics: HS: ML χ2 = 444.31, 321 df; CFI = .97, RMSEA = .03; S-B χ2 = 397.12, 321 df; RCFI = .98; RMSEA = .03. NHS: ML χ2= 578.29, 310 df; CFI = .97, RMSEA = .03; S-B χ2 = 479.86, 310 df; RCFI = .96; RMSEA = .03. The equality of regression paths across the two samples was tested with constrained models similar to those reported above.
Figure 2.
Path model for 356 individuals in the National Epidemiologic Survey on Alcohol and Related Conditions with past-year substance dependence and prior help-seeking at baseline.
Note: AOD stands for alcohol or other drug. Bolded lines indicate path relations between variables that differed in the multi-group analysis. a p ≤ .05, b = p ≤ .01; c = p ≤ .001
Figure 3.
Path model for 906 individuals in the National Epidemiologic Survey on Alcohol and Related Conditions with past-year substance dependence and no prior help-seeking at baseline.
Note: AOD stands for alcohol or other drug. Bolded lines indicate path relations between variables that differed in the multi-group analysis. a p ≤ .05, b = p ≤ .01; c = p ≤ .001
There were eight paths that were significantly different in strength between the two models (see Table 4). In six of these, relationships were stronger in the help-seeker model. These include the paths between: (1) baseline stress and having sought help since the last interview; (2) baseline mental disorders and having sought help, (3) baseline mental disorders and level of stress since last interview; (4) age at baseline and past-year health status; (5) stress since last interview and past-year health status; and (6) social support and mental disorders in the past year. In two instances, the pathways were stronger in the model of non-help-seekers: between (1) female and past-year stress, and (2) having sought help since last interview and physical health in past year.
Table 4.
Significantly different paths in 2-group assessment among help-seeking (N = 356) and non-help-seeking (N = 906) participants with alcohol and/or drug dependence in the National Epidemiologic Survey on Alcohol and Related Conditions.
| Regression path between: | χ2 | Regression coefficient in HS | Regression coefficient in NHS |
|---|---|---|---|
| 1. Baseline Stress and sought help SLI | 5.39a | .15 | NA |
| 2. Baseline Mental Disorders and sought help SLI | 6.74a | .24 | .08 |
| 3. Baseline Mental Disorders and Stress SLI | 8.76b | .19 | NA |
| 4. Age and Health last 12 months | 7.76a | −.27 | −.10 |
| 5. Female and Stress SLI | 6.30a | NA | .11 |
| 6. Sought help SLI and Health last 12 months | 12.13c | NA | −.10 |
| 7. Stress SLI and Health last 12 months | 5.71a | −.17 | NA |
| 8. Social Support and Mental Disorders last 12 months | 9.12b | −.40 | NA |
Note: SLI stands for since last interview, HS for help-seekers, NHS for non-help-seekers, NA for not applicable or not significant in the model.
p ≤ .05,
p ≤ .01,
p ≤ .001, two-tailed tests.
4. DISCUSSION
This study addresses a gap identified in a recent systematic review of prospective cohort studies of remission from substance use disorders, which concludes that the evidence base on remission is “very thin” and is particularly lacking in studies with general population samples (Calabria et al., 2010, p. 745). Moreover, the current study’s focus on remission from alcohol and/or drug dependence differentiates it from prior studies with NESARC that have identified correlates of both abstinent and non-abstinent recovery from alcohol dependence (Dawson and Grant, 2005, Dawson et al., 2006a, 2012).
The findings from the multi-group path model comparison showed generally similar dynamics in the influences on remission and other outcomes across groups with and without prior help-seeking at baseline, consistent with the study conceptual model. Social support and life stressors are important covariates with remission, but in opposite ways. Higher exposure to life stressors was associated with poorer mental and physical health and less remission at follow-up, whereas more social support was associated with better mental and physical health and a higher likelihood of remission. Thus, the study findings confirm that lower severity of both substance use and mental health disorders and more resources (i.e., employment and social support) are critical factors for recovery, whether within the context of help-seeking or not.
In addition, greater severity of disorders is the strongest factor associated with help-seeking. Other research has shown that recovery from alcohol dependence in the absence of treatment is common among the general population (Sobell et al., 1996), and is more prevalent among individuals with less severe disorders (Cunningham et al., 2000; Smart, 2007). Prior retrospective research with NESARC showed that transitional life events associated with school, employment, marital or parental status, were associated with recovery from alcohol dependence, regardless of treatment participation (Dawson et al., 2006b). Studies of individuals with drug disorders have also identified critical life events as a catalyst for change in the absence of treatment (Waldorf, 1987).
Individuals with prior help-seeking at baseline continued to have higher rates of help-seeking over the follow-up period. A combination of multiple problems, stressors, and limited social support appears to propel individuals to continue to seek help. Yet the poorer overall mental and physical health status and lower rates of remission among help-seekers suggests that addiction treatment faces a perceptional problem by virtue of its association with individuals who have the most severe and persistent disorders. Indeed, a prior longitudinal study conducted with NESARC found that the strongest barrier to seeking help for substance dependence, among those who believed that they needed help but had not received it, was pessimistic attitudes about the value of treatment (Mojtabai and Crum, 2013). The current study suggests that individuals with substance use disorders may seek help when other options to change are no longer viable, and when problem severity reaches a critical threshold.
In this regard, the current study encompassed a broad range of treatment and other types of services/help that individuals utilize for substance dependence, in addition to specialty rehabilitation and outpatient treatment programs1. Given the overall low rates of use of specialty addiction treatment, as discussed previously (SAMHSA, 2012), the study findings highlight the importance of broadening the scope of services and other forms of assistance for individuals with substance use problems. Moreover, the focus on services integration that has been emphasized in policy reports (Institute of Medicine, 2006) and is embedded in the Affordable Care Act (i.e., health care reform), suggests fruitful areas of outreach, screening, and brief interventions and cross-systems integration for individuals with substance dependence disorders in non-treatment settings.
Another robust finding across groups was the lower likelihood of help-seeking among women in the general population. Although women have generally higher rates of health services utilization (Verbrugge, 1985), even after controlling for health status and symptom severity (Green and Pope, 1999), they are less likely to seek help for substance abuse problems (Greenfield et al., 2007). Women with substance use problems encounter unique barriers, as compared with other forms of health services use. These may include factors such as greater stigma, less access to insurance coverage for addiction treatment, less family or other support for seeking treatment, concerns about jeopardizing custody of children or parental rights, and more family-related demands that hinder treatment participation (Grella, 2009; Grella and Joshi, 1999; Haller et al., 2003; Jessup et al., 2003). Women who had sought help were more likely to have multiple substance dependencies, comorbid mental health problems, and lower rates of employment, characteristics that have been well established in studies of clinical samples (Brady et al., 2009). However, women who had a history of help-seeking at baseline were more likely to be in remission at follow-up, a seeming contradiction with their higher levels of problem severity. Non-help-seeking women also had poorer mental and physical health, as well as higher levels of stress, which also led to an indirect negative effect of being female on remission mediated through stress.
Several limitations need to be considered in interpretation of study findings. Although we examined multiple outcomes, we lacked a measure of overall quality of life (Laudet et al., 2009) as well as a measure of self-perception as being “in recovery.” Thus our findings are more indicative of behavioral changes that are commonly associated with recovery from substance use disorders. Further, this secondary analysis of national survey data has the usual advantages (e.g., representative sample) and disadvantages (limited measures) associated with these large-scale surveys. The main study grouping variable of help-seeking is also limited in that we lack confirmation of the types of services that were actually provided to individuals in the settings where they sought help. This may be particularly true in hospital emergency rooms, which are unlikely to provide screening and/or referral for addiction treatment. Because of temporal overlap between variables assessed at Wave 2 that pertain to both potential mediators (e.g., stress, social support) and outcomes, we cannot assume causality from the study findings. Lastly, although the NESARC Wave 2 had an overall follow-up rate of approximately 87%, there was some selective study attrition, as the follow-up sample had a higher proportion of baseline help-seekers.
In conclusion, longitudinal studies of recovery from substance use disorders need to capture inputs across multiple service systems, including “informal” care, as well as examine remission among individuals who never receive treatment or other services. Integration of addiction, mental health, and physical health services is critical to addressing individuals with multiple problems who are most likely to seek treatment, but such integration will only reach the most severe patients who access these services. Strategies to engage non-help-seekers need to be embedded in alternative systems and approaches that may increase their access to resources that facilitate remission and eventual recovery from substance dependence.
Supplementary Material
Acknowledgments
Role of Funding Source
Dr. Christine E. Grella was supported by the National Institute on Drug Abuse grant P30-DA016383-07 and Dr. Judith A. Stein was supported by P01-DA01070-37.
The funding agency had no further role in study design; in the collection, analysis and interpretation of data; in the writing of the report; or in the decision to submit the paper for publication. The opinions expressed in this paper are the authors’ and do not necessarily represent the views of the funding agency.
The authors thank Elizabeth Teshome of UCLA for her assistance in preparation of this paper.
Footnotes
Supplementary material can be found by accessing the online version of this paper at http://dx.doi.org and by entering doi:...
Frequencies for types of help received at NESARC Wave 1 and Wave 2 for the study sample are shown can be found by accessing the online version of this paper at http://dx.doi.org and by entering doi:...
Contributors
CEG designed the study and wrote the first and final drafts of the paper, JAS conducted statistical analyses and collaborated in writing the paper. Both authors contributed to and have approved the final manuscript.
Conflict of Interest
Neither of the authors has a conflict of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Bentler PM. EQS 6 Structural Equations Program Manual. Multivariate Software, Inc; Encino, CA: 2006. [Google Scholar]
- Bentler PM, Dudgeon P. Covariance structure analysis: statistical practice, theory, and directions. Annu Rev Psychol. 1996;47:563–592. doi: 10.1146/annurev.psych.47.1.563. [DOI] [PubMed] [Google Scholar]
- Betty Ford Institute Consensus Panel. What is recovery? A working definition from the Betty Ford Institute. J Subst Abuse Treat. 2007;33:221–228. doi: 10.1016/j.jsat.2007.06.001. [DOI] [PubMed] [Google Scholar]
- Brady KT, Back SE, Greenfield SF, editors. Women & Addiction: A Comprehensive Handbook. Guildford Press; New York: 2009. [Google Scholar]
- Calabria B, Degenhardt L, Briegleb C, Vos T, Hall W, Lynskey M, Callaghan B, Rana U, McLaren J. Systematic review of prospective studies investigating “remission” from amphetamine, cannabis, cocaine or opioid dependence. Addict Behav. 2010;35:741–749. doi: 10.1016/j.addbeh.2010.03.019. [DOI] [PubMed] [Google Scholar]
- Chou C, Bentler PM. Model modification in covariance structure modeling: a comparison among likelihood ratio, Lagrange multiplier, and Wald tests. Multivariate Behav Res. 1990;25:115–136. doi: 10.1207/s15327906mbr2501_13. [DOI] [PubMed] [Google Scholar]
- Cohen S, Mermelstein R, Kamarck T, Hoberman HM. Measuring the functional components of social support. In: Sarason IG, Sarason BR, editors. Social Support: Theory, Research, and Applications. Martinus Nijhoff; Seattle: 1985. pp. 73–94. [Google Scholar]
- Compton WM, Thomas YF, Stinson FS, Grant BF. Prevalence, correlates, disability, and comorbidity of DSM-IV drug abuse and dependence in the United States. Arch Gen Psychiatry. 2007;64:566–576. doi: 10.1001/archpsyc.64.5.566. [DOI] [PubMed] [Google Scholar]
- Cunningham JA, Lin E, Ross HE, Walsh GW. Factors associated with untreated remissions from alcohol abuse or dependence. Addict Behav. 2000;25:317–321. doi: 10.1016/s0306-4603(98)00130-0. [DOI] [PubMed] [Google Scholar]
- Dawson DA, Goldstein RB, Ruan WJ, Grant BF. Correlates of recovery from alcohol dependence: a prospective study over a 3-year follow-up interval. Alcohol Clin Exp Res. 2012;36:1268–1277. doi: 10.1111/j.1530-0277.2011.01729.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dawson DA, Grant BF, Ruan WJ. The association between stress and drinking: modifying effects of gender and vulnerability. Alcohol Alcohol. 2005;40:453–460. doi: 10.1093/alcalc/agh176. [DOI] [PubMed] [Google Scholar]
- Dawson DA, Grant BF. Recovery from DSM-IV alcohol dependence: United States, 2001–2002. Addiction. 2005;100:281–292. doi: 10.1111/j.1360-0443.2004.00964.x. [DOI] [PubMed] [Google Scholar]
- Dawson DA, Grant BF, Stinson FS, Chou PS. Estimating the effect of help-seeking on achieving recovery from alcohol dependence. Addiction. 2006a;101:824–834. doi: 10.1111/j.1360-0443.2006.01433.x. [DOI] [PubMed] [Google Scholar]
- Dawson DA, Grant BF, Stinson FS, Chou PS. Maturing out of alcohol dependence: the impact of transitional life events. J Stud Alcohol. 2006b;67:195–203. doi: 10.15288/jsa.2006.67.195. [DOI] [PubMed] [Google Scholar]
- Granfield R, Cloud W. Social context and “natural recovery”: the role of social capital in the resolution of drug-associated problems. Subst Use Misuse. 2001;36:1543–1570. doi: 10.1081/ja-100106963. [DOI] [PubMed] [Google Scholar]
- Grant BF, Dawson DA, Stinson FS, Chou PS, Kay W, Pickering R. The Alcohol Use Disorder and Associated Disabilities Interview Schedule-IV (AUDADIS-IV): reliability of alcohol consumption, tobacco use, family history of depression and psychiatric diagnostic modules in a general population sample. Drug Alcohol Depend. 2003;71:7–16. doi: 10.1016/s0376-8716(03)00070-x. [DOI] [PubMed] [Google Scholar]
- Grant BF, Hasin DS. The Alcohol Use Disorders and Associated Disabilities Interview Schedule. National Institute on Alcohol and Alcoholism; Rockville, MD: 1991. [Google Scholar]
- Grant BF, Stinson FS, Dawson DA, Chou SP, Dufour MC, Compton W, Kaplan K. Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry. 2004;61:807–816. doi: 10.1001/archpsyc.61.8.807. [DOI] [PubMed] [Google Scholar]
- Green CA, Pope CR. Gender, psychosocial factors and the use of medical services: a longitudinal analysis. Soc Sci Med. 1999;48:1363–1372. doi: 10.1016/s0277-9536(98)00440-7. [DOI] [PubMed] [Google Scholar]
- Greenfield SF, Brooks AJ, Gordon SM, Green CA, Kropp F, McHugh RK, Lincoln M, Hien D, Miele GM. Substance abuse treatment entry retention, and outcome in women: a review of the literature. Drug Alcohol Depend. 2007;86:1–21. doi: 10.1016/j.drugalcdep.2006.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grella CE. Treatment seeking and utilization among women with substance use disorders. In: Brady KT, Back SE, Greenfield SF, editors. Women and Addiction: A Comprehensive Handbook. Guilford Publication; New York: 2009. pp. 307–322. [Google Scholar]
- Grella CE, Joshi V. Gender differences in drug treatment careers among clients in the national Drug Abuse Treatment Outcome Study. Am J Drug Alcohol Abuse. 1999;25:385–406. doi: 10.1081/ada-100101868. [DOI] [PubMed] [Google Scholar]
- Grella CE, Karno MP, Warda US, Moore AA, Niv N. Perceptions of need and help received for substance dependence in a national probability survey. Psychiatr Serv. 2009;60:1068–1074. doi: 10.1176/appi.ps.60.8.1068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haller DL, Miles DR, Dawson KS. Factors influencing treatment enrollment by pregnant substance abusers. Am J Drug Alcohol Abuse. 2003;29:117–131. doi: 10.1081/ada-120018842. [DOI] [PubMed] [Google Scholar]
- Hasin DS, Stinson FS, Ogburn E, Grant BF. Prevalence, correlates, disability, and comorbidity of DSM-IV alcohol abuse and dependence in the United States. Arch Gen Psychiatry. 2007;64:830–842. doi: 10.1001/archpsyc.64.7.830. [DOI] [PubMed] [Google Scholar]
- Hu LT, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Equ Modeling. 1999;6:1–55. [Google Scholar]
- Institute of Medicine. Improving the Quality of Health Care for Mental and Substance-Use Conditions. National Academy Press; Washington, DC: 2006. [Google Scholar]
- Jessup MA, Humphreys JC, Brindis CD, Kathryn AL. Extrinsic barriers to substance abuse treatment among pregnant drug dependent women. J Drug Issues. 2003;33:285–304. [Google Scholar]
- Kessler RC, Nelson CB, McGonagle KA, Edlund MJ, Frank RG, Leaf PJ. The epidemiology of co-occurring addictive and mental disorders: implications for prevention and service utilization. Am J Orthopsychiatry. 1996;66:17–31. doi: 10.1037/h0080151. [DOI] [PubMed] [Google Scholar]
- Laudet AB. What does recovery mean to you? Lessons from the recovery experience for research and practice. J Subst Abuse Treat. 2007;33:243–256. doi: 10.1016/j.jsat.2007.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laudet AB, White WL. Recovery capital as prospective predictor of sustained recovery, life satisfaction, and stress among former poly-substance users. Subst Use Misuse. 2008;43:27–54. doi: 10.1080/10826080701681473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laudet AB, Becker JB, White WL. Don’t wanna go through that madness no more: quality of life satisfaction as predictor of sustained remission from illicit drug misuse. Subst Use Misuse. 2009;44:227–252. doi: 10.1080/10826080802714462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lopez-Quintero C, Hasin DS, de Los Cobos JP, Pines A, Wang S, Grant BF, Blanco C. Probability and predictors of remission from life-time nicotine, alcohol, cannabis or cocaine dependence: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Addiction. 2011;106:657–669. doi: 10.1111/j.1360-0443.2010.03194.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacCallum R. Specification searches in covariance structure modeling. Psychol Bull. 1986;100:107–120. [Google Scholar]
- Mojtabai R, Crum RM. Perceived unmet need for alcohol and drug use treatments and future use of services: results from a longitudinal study. Drug Alcohol Depend. 2013;127:59–64. doi: 10.1016/j.drugalcdep.2012.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moos RH. Theory-based processes that promote the remission of substance use disorders. Clin Psychol Rev. 2007;27:537–551. doi: 10.1016/j.cpr.2006.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moos RH, Moos BS. Protective resources and long-term recovery from alcohol use disorders. Drug Alcohol Depend. 2007;86:46–54. doi: 10.1016/j.drugalcdep.2006.04.015. [DOI] [PubMed] [Google Scholar]
- Ruan WJ, Goldstein RB, Chou SP, Smith SM, Saha TD, Pickering RP, Dawson DA, Huang B, Stinson FS, Grant BF. Alcohol use disorder and associated disabilities interview schedule-IV (AUDADIS-IV): reliability of new psychiatric diagnostic modules and risk factors in a general population sample. Drug Alcohol Depend. 2008;92:27–36. doi: 10.1016/j.drugalcdep.2007.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smart RG. Natural recovery or recovery without treatment from alcohol and drug problems as seen from survey data. In: Klingemann H, Sobell LC, editors. Promoting Self-Change from Addictive Behaviors: Practical Implications for Policy, Prevention, and Treatment. Springer; New York: 2007. pp. 59–71. [Google Scholar]
- Sobell LC, Cunningham JA, Sobell MB. Recovery from alcohol problems with and without treatment: prevalence in two population surveys. Am J Public Health. 1996;86:966–972. doi: 10.2105/ajph.86.7.966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration [SAMHSA] Results from the 2011 National Survey on Drug Use and Health: Summary of National Findings. NSDUH Series H-44, HHS Publication No SMA-12–4713. 2012 Retrieved December 18, 2012, from: http://www.samhsa.gov/data/NSDUH/2k11Results/NSDUHresults2011.pdf.
- Verbrugge LM. Gender and health: an update on hypotheses and evidence. J Health Soc Behav. 1985;26:156–182. [PubMed] [Google Scholar]
- Waldorf D. Natural recovery from opiate addiction: some social-psychological processes of untreated recovery. J Drug Issues. 1983:237–247. [Google Scholar]
- Wang PS, Lane M, Olfson M, Pincus HA, Wells KB, Kessler RC. Twelvemonth use of mental health services in the United States. Arch Gen Psychiatry. 2005;62:629–640. doi: 10.1001/archpsyc.62.6.629. [DOI] [PubMed] [Google Scholar]
- Ware JE, Kosinski M, Keller SD. A 12-item short-form health survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34:220–233. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- White WL. Addiction recovery: its definition and conceptual boundaries. J Subst Abuse Treat. 2007;33:229–241. doi: 10.1016/j.jsat.2007.04.015. [DOI] [PubMed] [Google Scholar]
- Yuan KH, Bentler PM, Kano Y. On averaging variables in a confirmatory factor analysis model. Behaviormetrika. 1997;24:71–83. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.