Abstract
Objectives
To examine temporal trends in the US incidence of childhood asthma hospitalizations, inhospital mortality, mechanical ventilation use, and hospital charges between 2000 and 2009.
Study design
A serial, cross-sectional analysis of a nationally-representative sample of children hospitalized with acute asthma. The Kids Inpatient Database was used to identify children <18 years of age with asthma by International Classification of Diseases, Ninth Revision, Clinical Modification code 493.xx. Outcome Measures were asthma hospitalization incidence, in-hospital mortality, mechanical ventilation use, and hospital charges. We examined temporal trends of each outcome, accounting for sampling weights. Hospital charges were adjusted for inflation to 2009 US dollars.
Results
The four separated years (2000, 2003, 2006, and 2009) of national discharge data included 592 805 weighted discharges with asthma. Between 2000 and 2009, asthma hospitalization incidence decreased from 21.1 to 18.4 per 10 000 person-years among all US children (13% decrease; Ptrend<.001). Mortality declined significantly after adjusting for confounders (OR for comparison of 2009 with 2000, 0.37; 95%CI, 0.17-0.79). By contrast, there was an increase in mechanical ventilation use (0.8% to 1.0%; 28% increase; Ptrend<.001). Nationwide hospital charges also increased from $1.27 billion to $1.59 billion (26% increase; Ptrend<.001); this increase was driven by a rise in the geometric mean of hospital charges per discharge, from $5940 to $8410 (42% increase; Ptrend<.001).
Conclusions
Between 2000 and 2009, we found significant declines in asthma hospitalization and in-hospital mortality among US children. By contrast, mechanical ventilation use and hospital charges for asthma significantly increased over this same period.
Keywords: asthma, children, trends, hospitalization, mechanical ventilation, mortality, length of stay, hospital charge
Childhood asthma is a significant public health problem in the United States, with continued reports of rising prevalence.1-7 The most recent estimates indicated that asthma affected 9.6% (7.1 million) of US children in 2009.7 Asthma accounted for approximately 10.5 million missed days of school, 7.5 million outpatient visits, 640 000 emergency department visits, and 157 000 hospitalizations in 2007.7
Asthma hospitalizations represent a serious adverse outcome that is theoretically preventable with high-quality healthcare, patient education, and optimal management of asthma.8 Furthermore, hospitalizations are known to be an important driver of asthma-related direct healthcare costs.9-11 Although its public health burden is significant, prior research on childhood asthma has focused on asthma prevalence, incidence of ambulatory care visits and hospitalizations, and mortality.1, 2, 4, 6, 7 With the exception of one study of children with status asthmaticus within a local population,5 there have been no recent efforts to assess temporal trends in inpatient healthcare utilization for asthma, such as in-hospital use of mechanical ventilation and length of stay, and hospital charges of hospitalizations among US children.
In this context, we analyzed nationally-representative data to examine the temporal trends in childhood asthma hospitalizations in the US between 2000 and 2009,
METHODS
We performed a serial cross-sectional analysis of childhood hospitalizations in 2000, 2003, 2006, and 2009, using the Healthcare Cost and Utilization Project's (HCUP) Kids’ Inpatient Database (KID), compiled by the Agency for Healthcare Research and Quality (AHRQ).12 The KID was designed to report hospital use and outcomes for children and is the only all-payer inpatient care database for children in the US. The KID is a stratified sample of all pediatric discharges, defined as age 20 years or younger, from states that participate in HCUP. States that participate in HCUP provide discharge-level data on all inpatient discharges from all “community” hospitals (i.e., nonfederal, short-term, general, and specialty hospitals) in that state. KID contains a 10% stratified sample of uncomplicated in-hospital births and an 80% stratified sample of other cases. Discharges are weighted based on the sampling scheme to permit inferences for a nationally-representative population. In 2009, the KID contained information for 7.4 million weighted discharges from 4121 hospitals in 44 states; the states not in the KID 2009 were Alabama, Alaska, Delaware, Idaho, Mississippi, and North Dakota. The KID was available every three years beginning 1997. Because of significant changes in dataset sampling between 1997 and subsequent years, the present analysis used the KID in years 2000, 2003, 2006, and 2009. The KID has been used to study temporal trends in many different populations, and has been validated against the National Hospital Discharge Survey.13-15 Additional details of the KID can be found elsewhere.16 The institutional review board of Massachusetts General Hospital classified this analysis of de-identified data as exempt.
Hospital discharges for patients age 0 to 17 years, who had an International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) code for asthma (493.xx) in the primary diagnosis field, were eligible for our analyses. Patients were excluded from analysis if age was not documented.
Measurements
The KID contains information on patient characteristics, such as age, sex, race/ethnicity, primary insurance type (payer), discharge diagnoses and procedures, total charge for inpatient services, hospital length of stay, and disposition. To describe the socioeconomic status and burden of healthcare utilization, primary payer was included. Primary payer was grouped into public sources (Medicaid and Medicare), private payers, and other types. Additionally, race/ethnicity was categorized into white, black, Hispanic, and other. Diagnoses and procedures were available using ICD-9-CM and Clinical Classifications Software (CCS), a methodology developed by AHRQ to group ICD-9-CM codes into clinically sensible and mutually exclusive categories. High-risk medical condition was defined as at least one Pediatric Complex Chronic Condition, previously defined using ICD-9-CM codes in nine categories of illness (e.g., neuromuscular, cardiovascular, and respiratory).17
Hospital characteristics include US region, urban-rural status, teaching status, and designation as a children's hospital. Geographic regions (Northeast, South, Midwest, and West) were defined according to Census Bureau boundaries.18 Children's hospital designation was determined from the National Association of Children's Hospitals and Related Institutions classification criteria: non-children's hospital and children's hospital (children's general hospital, children's specialty hospital, and children's unit in general hospital).19
Outcome measures
The primary outcome measures were incidence of asthma hospitalization, in-hospital mortality, use of mechanical ventilation (non-invasive or invasive), and hospital charges. Other outcome measures of interest included in-hospital management such as length of stay, and direct medical cost. In-hospital mortality was defined as the number of deaths divided by total number of asthma discharges. Mechanical ventilation use was identified by using CCS code 216; non-invasive mechanical ventilation, such as bi-level/continuous positive airway pressure ventilation, was identified by ICD-9 procedure code 93.90. Total hospital charges reflected the total facility fees reported for each discharge record.
As cost data were not available in the early part of the study period, we calculated direct medical costs using hospital-specific cost/charge ratios for 2009 hospitalizations only. Cost information was obtained from the hospital accounting reports collected by the Centers for Medicare and Medicaid Services. Because of incomplete hospital cost/charge ratios data (missing data in less than 10% of eligible cases), cases without hospital-specific cost/charge ratios were excluded and data were appropriately reweighted to analyzed cost, following HCUP recommendations.12
Statistical analyses
We examined changes in the weighted estimate of all outcomes in 2000, 2003, 2006, and 2009. We calculated hospitalization incidence rates using population estimates obtained from the US Census Bureau.20 Incidence rates were expressed as the number of estimated hospitalizations per 10 000 children of the corresponding age group. Cochran–Armitage testing was used to test for trend in incidence rates.
To facilitate direct comparisons between years for hospital charges, we converted all charges to 2009 US dollars using the medical care component of the Consumer Price Index.21 Because hospital charges were not normally distributed, we calculated the weighted geometric mean and median of charges.22 The geometric mean is the average of the logarithmic values of a data set, which is then converted back to a base-ten number; it is less influenced by extreme values than the arithmetic mean. We estimated total charges as a weighted sum of case-level charges. We performed linear regression for models of log-transformed charges to test temporal trends.
To examine temporal trends of in-hospital mortality and mechanical ventilation use, we fit two analytical models. First, we developed an unadjusted model that included only calendar year as the independent variable. Second, we examined the independent association between calendar year and each outcome using multivariable logistic regression. We adjusted for both patient-level variables (i.e., age, sex, race/ethnicity, primary payer, and high-risk medical conditions) and hospital-level characteristics (region, urban and rural distinction, hospital teaching status, and children's hospital designation).
We then conducted a series of stratification analyses to assess the consistency of temporal trend in each primary outcome among age groups (0-4, 5-11, and 12-17 years), according to the National Asthma Education and Prevention Program guidelines.8 Additionally, to address the possibility that diagnostic transfer may partially explain the temporal trend in hospitalization rates, we examined temporal trends for pneumonia (CCS code 122), bronchiolitis (ICD-9-CM code 466.1), bronchitis (ICD-9-CM code 466.0), and wheezing (ICD-9-CM codes 519.8 or 786.07) in the primary diagnosis field.
All analyses used SAS-callable SUDAAN, version 11.0 (Research Triangle Institute, Research Triangle Park, NC) to obtain nationally-representative estimates weighted by AHRQ-specified discharge values in compliance with the HCUP analysis recommendations.12 Two-sided P<.05 was considered statistically significant; all data were reported with standard errors or 95% confidence intervals (CIs).
RESULTS
We identified a total of 354 259 patient discharges of childhood asthma in the US, which corresponded to a weighted estimate of 592 805 discharges across the four datasets (2000, 2003, 2006, and 2009). Asthma accounted for 2.3% (95%CI, 2.2%-2.4%) of all hospitalizations for children <18 years.
The patient and hospital characteristics of the hospitalized children with asthma in the four 1-year periods are shown in Table I. In more recent years, the hospitalized children were less likely to be white; and more likely to be Hispanic. The children were more likely to be insured by Medicaid or Medicare, and to have high-risk medical conditions (from 4.0% in 2000 to 5.2% in 2009; 30% increase; Ptrend<.001). Over the study period, children with asthma also had a higher frequency of admission to children's hospitals (34% in 2000 to 43% in 2009; 28% increase; Ptrend<.001).
Table I.
Patient and Hospital Characteristics of Childhood Asthma Hospitalizations; 2000-2009*
| 2000 | 2003 | 2006 | 2009 | P for Trend | |
|---|---|---|---|---|---|
| Unweighted sample, No. | 81 057 | 97 418 | 83 167 | 92 617 | |
| Weighted sample, No. | 152 149 | 165 755 | 137 729 | 137 172 | |
| Patient | |||||
| Age (year) | |||||
| 0-4 | 52.9 (0.4) | 55.7 (0.4) | 54.0 (0.4) | 51.2 (0.4) | <.001 |
| 5-11 | 32.4 (0.4) | 30.1 (0.3) | 33.1 (0.3) | 36.2 (0.3) | <.001 |
| 11-17 | 14.7 (0.3) | 13.7 (0.2) | 12.9 (0.2) | 12.6 (0.2) | <.001 |
| Male sex | 62.5 (0.2) | 62.3 (0.2) | 62.4 (0.2) | 62.9 (0.2) | .08 |
| Race or ethnic group† | |||||
| White | 35.0 (1.2) | 28.3 (1.0) | 28.3 (1.0) | 31.0 (1.2) | .002 |
| Black | 28.8 (1.6) | 24.1 (1.3) | 24.7 (1.3) | 28.5 (1.6) | .88 |
| Hispanic | 16.0 (1.1) | 16.1 (1.2) | 17.4 (1.1) | 19.0 (1.1) | .003 |
| Other | 6.1 (0.6) | 6.1 (0.6) | 6.1 (0.5) | 7.7 (0.5) | .01 |
| Type of health insurance† | |||||
| Public | 44.2 (0.9) | 48.6 (0.9) | 51.1 (0.8) | 55.5 (1.0) | <.001 |
| Private | 48.0 (1.0) | 43.4 (1.0) | 40.1 (0.9) | 37.2 (0.9) | <.001 |
| Other | 7.7 (0.4) | 8.0 (0.8) | 8.4 (0.5) | 7.3 (0.5) | .58 |
| Any high-risk condition‡ | 4.0 (0.2) | 4.7 (0.2) | 4.7 (0.2) | 5.2 (0.2) | <.001 |
| Hospital | |||||
| Region | |||||
| Northeast | 24.2 (2.4) | 23.9 (1.9) | 24.3 (2.0) | 25.1 (2.8) | .60 |
| Midwest | 13.6 (1.7) | 20.1 (1.8) | 20.3 (1.9) | 19.0 (2.0) | .005 |
| South | 40.1 (2.5) | 38.5 (2.1) | 37.9 (2.3) | 37.4 (2.4) | .09 |
| West | 21.3 (2.2) | 17.5 (1.7) | 17.5 (1.7) | 18.5 (1.9) | .06 |
| Location/teaching status | |||||
| Rural | 15.0 (0.9) | 14.6 (0.9) | 11.5 (0.7) | 11.0 (0.7) | .004 |
| Urban non-teaching | 29.4 (1.7) | 30.1 (1.6) | 27.6 (1.6) | 27.8 (1.7) | .20 |
| Urban teaching | 55.6 (2.2) | 54.8 (1.9) | 60.1 (1.9) | 61.2 (2.1) | .001 |
| Hospital designation | <.001 | ||||
| Children's hospital | 33.9 (2.9) | 32.2 (2.4) | 40.2 (2.5) | 43.3 (2.8) | |
| Non-children's hospital | 66.1 (2.9) | 67,8 (2.4) | 59.8 (2.5) | 56.7 (2.8) |
Data are expressed as % (standard error) otherwise indicated.
Percentages are not equal 100 because of missing data.
High-risk medical condition was defined as at least 1 complex medical condition, previously defined using ICD-9-CM codes in 9 categories of illness (i.e., neuromuscular, cardiovascular, respiratory, renal, gastrointestinal, hematology or immunologic, metabolic, malignancy, and other congenital or genetic defect disorders).
Temporal trends in incidence of childhood asthma hospitalizations
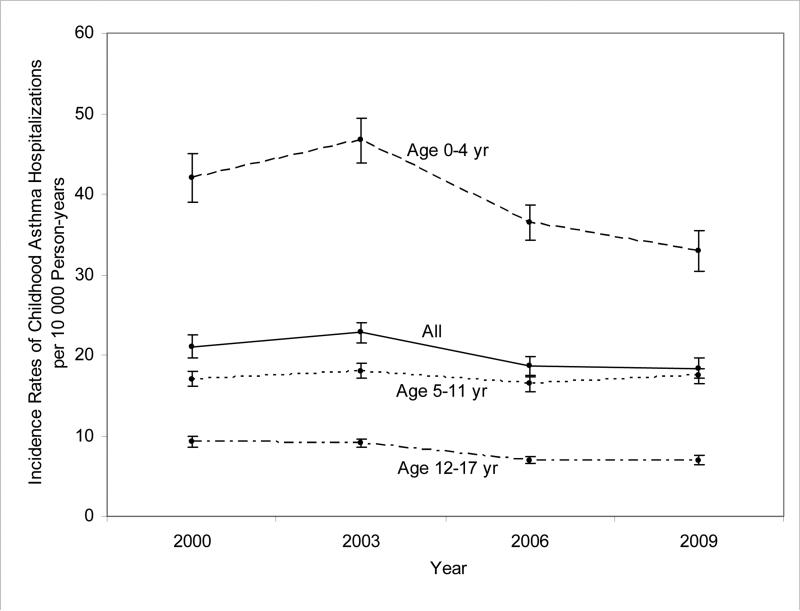
Between 2000 and 2009, there was a decrease in the incidence of asthma hospitalization, from 21.1 (95%CI, 19.6-22.5) to 18.4 (95%CI, 17.1-19.7) per 10 000 person-years (13% decrease; Ptrend<.001; Figure 1). The decreasing temporal trend in asthma hospitalizations persisted among the youngest (0-4 years) and the oldest (12-17 years) age groups (both Ptrend<.001). Incidence of hospitalization was highest among the youngest group.
Figure 1.
Incidence Rates of US Asthma Hospitalizations per 10 000 Children, According to Age Group, 2000-2009.
Between 2000 and 2009, there was a significant decline in the incidence rate of asthma hospitalization among overall US children (13% decrease; Ptrend<.001), the 0- to 4-year-old age group (21% decrease; Ptrend<.001), and the 12- to 17-year-old age group (25% decrease; Ptrend<.001). The incidence rate among the 5- to 11-year-old age group did not change significantly (Ptrend=.31).
Temporal trends in healthcare utilization and in-hospital mortality
Between 2000 and 2009, unadjusted in-hospital mortality decreased significantly (0.06% in 2000 to 0.02% in 2009; unadjusted OR for comparison of 2009 with 2000, 0.44; 95%CI, 0.21-0.90; P=.009; Table II). Similarly, multivariable-adjusted mortality declined significantly (adjusted OR, 0.37; 95%CI, 0.17-0.79; P=.006; Table III available at www.jpeds.com). The older age groups (age 5-11 years and 11-17 years) had higher in-hospital mortality, compared with the youngest age group (age 0-4 years).
Table II.
In-hospital Mortality, Health Care Use, and Hospital Charges for Childhood Asthma Hospitalizations; 2000-2009
| 2000 (N = 152 149) | 2003 (N = 165 755) | 2006 (N = 137 729) | 2009 (N = 137 172) | P for Trend | |
|---|---|---|---|---|---|
| Primary outcomes | |||||
| In-hospital death, weighted No. | 84 | 22 | 36 | 33 | |
| In-hospital mortality, % (95% CI) | 0.06 (0.03-0.10) | 0.01 (0.01-0.02) | 0.03 (0.02-0.04) | 0.02 (0.02-0.04) | .009 |
| Mechanical ventilation | |||||
| Weighted No. | 1211 | 1235 | 988 | 1397 | |
| % (95% CI) | 0.80 (0.67-0.94) | 0.75 (0.65-0.85) | 0.72 (0.62-0.83) | 1.02 (0.89-1.17) | <.001 |
| Hospital charges | |||||
| Total Charge (95% CI) (billions) | 1.27 (1.19-1.34) | 1.59 (1.50-1.68) | 1.40 (1.32-1.48) | 1.59 (1.49-1.70) | |
| Charges per discharge Geometric mean (95% CI) | 5938 (5673-6203) | 6879 (6583-7174) | 7448 (7102-7793) | 8406 (7941-8870) | <.001 |
| Median (IQR) | 5640 (3572-9339) | 6537 (4099-10 827) | 7130 (4529-11 763) | 8109 (5089-13 436) | |
| Secondary outcomes | |||||
| Total inpatient days (95% CI), d (thousands) | 364 (356-371) | 390 (384-398) | 310 (304-315) | 305 (299-310) | |
| Length of stay Geometric mean (95% CI), d | 2.0 (2.0-2.0) | 2.0 (1.9-2.0) | 1.9 (1.9-1.9) | 1.9 (1.8-1.9) | <.001 |
| Median (IQR), d | 1.5 (1.0-2.5) | 1.5 (1.0-2.4) | 1.4 (1.0-2.3) | 1.4 (1.0-2.2) |
CI, confidence interval; IQR, interquartile range
All charges are expressed as 2009 US dollars.
Table III.
Unadjusted and Multivariable Models of In-hospital Mortality and Use of Mechanical Ventilation among Childhood Asthma Hospitalizations; 2000-2009
| In-hospital Mortality | Use of Mechanical Ventilation | |||
|---|---|---|---|---|
| Variable | Unadjusted model | Multivariable model | Unadjusted model | Multivariable model |
| Calendar year | ||||
| 2000 | Reference | Reference | Reference | Reference |
| 2003 | 0.24 (0.11-0.55) | 0.22 (0.09-0.52) | 0.94 (0.78-1.13) | 0.97 (0.79-1.17) |
| 2006 | 0.48 (0.24-0.97) | 0.40 (0.19-0.87) | 0.90 (0.74-1.10) | 0.86 (0.70-1.33) |
| 2009 | 0.44 (0.21-0.90) | 0.37 (0.17-0.79) | 1.28 (1.06-1.55) | 1.09 (0.89-1.33) |
| Age (year) | ||||
| 0-4 | – | Reference | – | Reference |
| 5-11 | – | 2.18 (1.06-4.49) | – | 1.49 (1.33-1.67) |
| 11-17 | – | 6.16 (3.08-12.35) | – | 3.01 (2.64-3.43) |
| Male sex (vs. female) | – | 0.78 (0.52-1.17) | – | 1.00 (0.92-1.09) |
| Race or ethnic group | ||||
| White | – | Reference | – | Reference |
| Black | – | 0.68 (0.35-1.32) | – | 1.02 (0.86-1.21) |
| Hispanic | – | 0.80 (0.37-1.73) | – | 0.82 (0.69-0.97) |
| Other | – | 0.67 (0.26-1.69) | – | 1.23 (1.02-1.48) |
| Type of health insurance | ||||
| Public | – | 0.63 (0.29-1.37) | – | 1.02 (0.85-1.22) |
| Private | – | 0.81 (0.37-1.78) | – | 0.99 (0.83-1.18) |
| Other | – | Reference | – | Reference |
| Any high-risk condition* | – | 7.28 (4.26-12.42) | – | 4.36 (3.85-4.93) |
| Region | ||||
| Northeast | – | Reference | – | Reference |
| Midwest | – | 4.37 (1.71-11.14) | – | 0.82 (0.57-1.19) |
| South | – | 1.47 (0.76-2.83) | – | 0.83 (0.66-1.05) |
| West | – | 1.38 (0.68-2.81) | – | 0.91 (0.69-1.19) |
| Location/teaching status | ||||
| Rural | – | Reference | – | Reference |
| Urban non-teaching | – | 0.44 (0.09-2.21) | – | 1.93 (1.24-3.00) |
| Urban teaching | – | 1.90 (0.66-5.45) | – | 4.86 (3.85-4.93) |
| Hospital designation | ||||
| Children's hospital | – | 2.05 (1.03-4.10) | – | 2.02 (1.65-2.48) |
| Non-children's hospital | – | Reference | – | Reference |
Data are expressed as odds ratio (95% confidence interval) unless otherwise indicated.
High-risk medical condition was defined as at least 1 complex medical condition, previously defined using ICD-9-CM codes in 9 categories of illness (i.e., neuromuscular, cardiovascular, respiratory, renal, gastrointestinal, hematology or immunologic, metabolic, malignancy, and other congenital or genetic defect disorders).
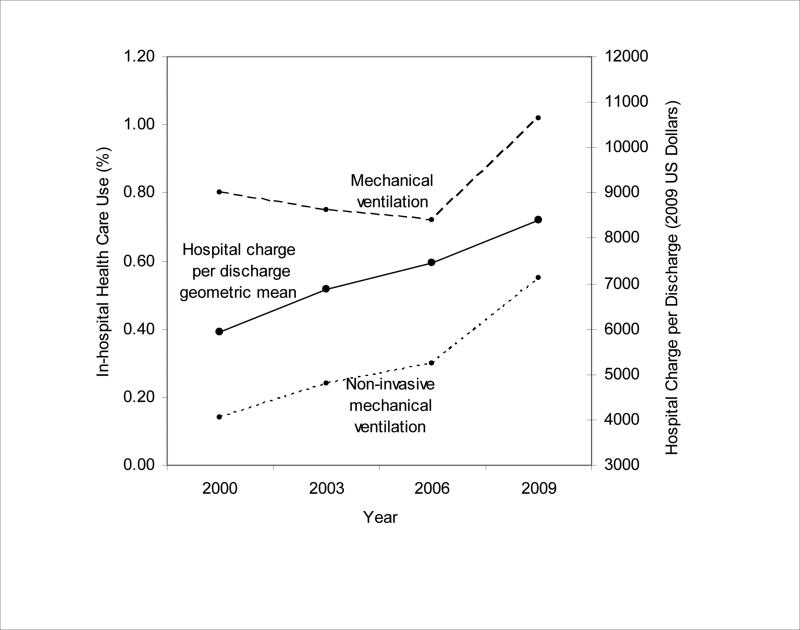
Unlike the mortality data, the rate of children with asthma who underwent mechanical ventilation over the study period increased significantly (unadjusted OR for comparison of 2009 with 2000, 1.28; 95%CI, 1.06-1.55; P<.001; Table II and Figure 2). Likewise, use of non-invasive mechanical ventilation increased significantly (unadjusted OR, 4.10; 95%CI, 2.83-5.96; P<.001). The increasing temporal trends in use of overall mechanical ventilation and non-invasive mechanical ventilation persisted across all age groups (all Ptrend≤.01; Table IV available at www.jpeds.com). By contrast, the temporal trend of the overall mechanical ventilation use became non-significant after adjustment for covariates, such as high-risk medical condition (adjusted OR for comparison of 2009 with 2000, 1.09; 95%CI, 0.89-1.33; P=.40; Table III). Presence of high-risk medical conditions was significantly associated with use of mechanical ventilation (adjusted OR, 4.36; 95%CI, 3.85-4.93; P<.001).
Figure 2.
In-hospital Health Care Utilization and Hospital Charges for Childhood Asthma Hospitalizations, 2000-2009.
Between 2000 and 2009, use of mechanical ventilation increased (28% increase; Ptrend<.001); use of non-invasive mechanical ventilation also increased (292% increase; Ptrend<.001). The geometric mean of hospital charges per case increased significantly (42% increase; Ptrend<.001), adjusted for inflation.
Table IV.
Use of Mechanical Ventilation in Childhood Asthma Hospitalizations, According to Age Group; 2000-2009
| Use of mechanical ventilation, % (95% CI) |
||||||
|---|---|---|---|---|---|---|
| Weighted sample, No. | 2000 | 2003 | 2006 | 2009 | P for Trend | |
| All childhood asthma Overall mechanical ventilation | 137 172 | 0.80 (0.67-0.94) | 0.75 (0.65-0.85) | 0.72 (0.62-0.83) | 1.02 (0.89-1.17) | <.001 |
| Non-invasive ventilation | 1776 | 0.14 (0.09-0.20) | 0.24 (0.18-0.34) | 0.30 (0.23-0.39) | 0.55 (0.45-0.69) | <.001 |
| Subgroup | ||||||
| Age 0 to 4 year Overall mechanical ventilation | 70 235 | 0.51 (0.42-0.61) | 0.58 (0.50-0.58) | 0.52 (0.44-0.62) | 0.68 (0.57-0.81) | .01 |
| Non-invasive ventilation | 515 | 0.07 (0.04-0.11) | 0.16 (0.11-0.23) | 0.14 (0.10-0.20) | 0.30 (0.22-0.41) | <.001 |
| Age 5 to 11 year Overall mechanical ventilation | 49 671 | 0.87 (0.67-1.13) | 0.66 (0.55-0.79) | 0.72 (0.60-0.88) | 1.07 (0.91-1.26) | <.001 |
| Non-invasive ventilation | 685 | 0.18 (0.11-0.29) | 0.24 (0.16-0.36) | 0.35 (0.26-0.47) | 0.63 (0.51-0.78) | <.001 |
| Age 12 to 17 year Overall mechanical ventilation | 17 266 | 1.66 (1.35-2.03) | 1.61 (1.33-1.95) | 1.52 (1.22-1.90) | 2.25 (1.92-2.63) | .002 |
| Non-invasive ventilation | 576 | 0.28 (0.16-0.47) | 0.60 (0.40-0.90) | 0.82 (0.59-1.14) | 1.35 (1.08-1.69) | <.001 |
CI, confidence interval
Temporal trends in hospital charges for asthma
Between 2000 and 2009, the total hospital charges for asthma hospitalization increased from approximately $1.27 billion (95%CI, $1.19-$1.34 billion) to $1.59 billion (95%CI, $1.49-$1.70 billion) nationally, adjusted for inflation (26% increase; Ptrend<.001; Table II). The geometric mean of hospital charges per discharge increased from $5938 (95%CI, $5673-$6203) to $8406 (95%CI, $7941-$8870; 42% increase; Ptrend<.001; Figure 2). The increasing temporal trends in hospital charge per discharge were present in all age groups (all Ptrend<.001; Table V available at www.jpeds.com). By contrast, the length of stay decreased significantly over the study period (2.0 days in 2000 and 1.9 days in 2009; Ptrend<.001). In 2009, the total direct cost of asthma hospitalizations was $502 million (95% CI, $477-$527 million) nationally (Table VI; available at www.jpeds.com). Children 0-4 years of age accounted for nearly half of this annual cost.
Table V.
Hospital Charges per Discharge for Childhood Asthma Hospitalizations, According to Age Group; 2000-2009
| Hospital charge per discharge, $ |
||||||
|---|---|---|---|---|---|---|
| Weighted sample, No. | 2000 | 2003 | 2006 | 2009 | P for Trend | |
| Age 0 to 4 year Geometric mean (95% CI) | 70 235 | 5508 (5260-5755) | 6432 (6152-6712) | 6871 (6521-7180) | 7720 (7230-8160) | <.001 |
| Median (IQR) | 5253 (3388-8564) | 6140 (3861-10 090) | 6630 (4213-10 762) | 7487 (4754-12 168) | ||
| Age 5 to 11 year Geometric mean (95% CI) | 49 671 | 6286 (5994-6568) | 7268 (6957-7579) | 7903 (7527-8280) | 8886 (8413-9359) | <.001 |
| Median (IQR) | 5966 (3762-9976) | 6837 (4339-11 373) | 7585 (4850-12 451) | 8553 (5348-14 235) | ||
| Age 12 to 17 year Geometric mean (95% CI) | 17 266 | 6878 (6536-7220) | 7999 (7598-8399) | 8968 (8463-9473) | 10121 (9496-10746) | <.001 |
| Median (IQR) | 6552 (4049-10 847) | 7477 (4703-12 783) | 8522 (5293-14 460) | 9750 (5937-16 387) | ||
IQR, interquartile range.
All charges are expressed as 2009 US dollars.
Table VI.
Total and Mean Direct Cost for Childhood Asthma Hospitalizations, According to Age Group; 2009
| Weighted sample, No. | Total Direct Cost (95% CI), $ (Millions) | Cost per Hospitalization, $ | ||
|---|---|---|---|---|
| Geometric mean (95% CI) | Median (IQR) | |||
| All childhood asthma | 137 172 | 502 (477-527) | 2780 (2675-2885) | 2650 (1794-4111) |
| Subgroup | ||||
| Age 0 to 4 year | 70 235 | 230 (220-240) | 2544 (2457-2632) | 2459 (1679-3734) |
| Age 5 to 11 year | 49 671 | 193 (182-203) | 2947 (2827-3065) | 2787 (1889-4386) |
| Age 12 to 17 year | 17 266 | 79 (74-85) | 3379 (3200-3557) | 3190 (2107-5077) |
CI, confidence interval; IQR, interquartile range
DISCUSSION
Using a large database of US pediatric hospitalizations between 2000 and 2009, we found that the burden of asthma as measured by hospitalization rates and in-hospital mortality decreased significantly. In conjunction with these declines, we observed a marked increase in use of mechanical ventilation and hospital charges across all age groups. Other notable temporal trends during this 10-year period included increasing patients with high-risk medical conditions, and more frequent hospitalization to children's hospitals. These findings were consistent with a previous study of children with status asthmaticus in New Jersey that reported lower hospitalization rates, greater ICU use, and higher costs between 1992 and 2006.5 The KID provides a nationally-representative sample that better addresses the public health burden and healthcare utilizations of asthma in US children.
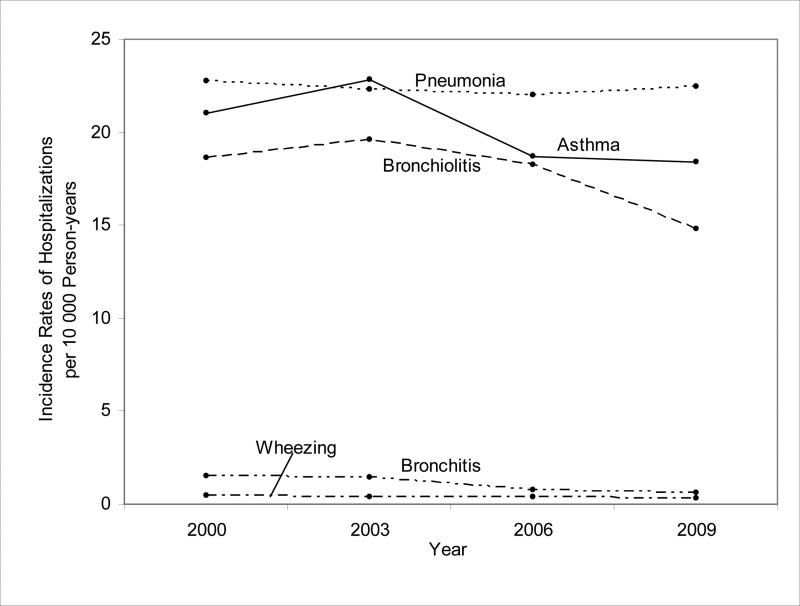
Although a previous study reported a non-significant annual decrease in the incidence of childhood asthma hospitalizations from 1991 through 2006 using the National Hospital Discharge Survey,1 we found a significant 13% decrease nationally between 2000 and 2009. The reasons for the decreasing temporal trend are unclear and likely multifactorial. The decrease in hospitalization rates could reflect decreases in the frequency of asthma exacerbations and their severity.6 Alternatively, non-biological factors, such as changes in asthma education, evidence-based therapy, access to ambulatory healthcare, and criteria for hospitalizations, may have contributed.23, 24 Another possible explanation for the decreasing hospitalization rates is diagnostic transfer (ie, a change in labeling of respiratory condition in children over time). If diagnostic-coding variations during the study period substantially influenced the decrease in asthma hospitalization rates, we would expect a compensatory increase in hospitalization rates for other lower respiratory tract diseases. However, the observed decline in hospitalization rates for asthma was mirrored by decreases in those for pneumonia, bronchiolitis, bronchitis, and wheezing between 2000 and 2009 (all Ptrend<.001; Figure 3 available at www.jpeds.com), which argues against the idea that diagnostic transfer accounts for the welcome decrease in asthma hospitalization rates.
Figure 3.
Incidence Rates of Asthma, Pneumonia, Bronchiolitis, Bronchitis, and Wheezing Hospitalizations per 10 000 Children; 2000-2009.
For all disease groups, a decreasing trend in incidence of hospitalization was seen across all study years (Ptrend<.001).
The data also showed more than a two-fold decrease in adjusted in-hospital mortality among US children with asthma; the mortality finding occurred despite an increase in children with high-risk medical conditions. This promising temporal trend also has many possible contributing factors. Decline in mortality may reflect availability and utilization of healthcare, access to and appropriate use of medication and prevention strategies, and severity of disease. Alternatively, the improvement in survival may have been driven by change in coding practice, with fewer severe cases of asthma being recognized and coded in more recent years. Arguing against this are the observed decline in asthma hospitalization rate and rise in the proportion of children with comorbidity. The significant reductions in mortality were large and consistent with the recent surveillance efforts using National Vital Statistic System, further supporting the validity of these findings.1, 6, 7
The increased use of mechanical ventilation including non-invasive ventilation raises the possibility that advanced respiratory support was being performed at an earlier phase on less critically ill patients with asthma,25 which may have led to a reduction in mortality rates. Additionally, an increasing proportion of hospitalizations in children's hospitals may reflect an improvement of regional systems of healthcare for critically ill children, similar to neonatal intensive care and trauma care, contributing to the decline in mortality through increased coordination of care.26, 27 Furthermore, the dissemination of national asthma management guidelines in 1997 and of updates in 2002 and 2007, which highlight the central role of inflammation and preventive management, might have contributed to decreased asthma-related mortality.1, 8 Indeed, a recent cross-sectional study of US children's hospitals using Children's Asthma Care measure data showed high compliances.28 Furthermore, an analysis using the National Health and Nutrition Examination Survey demonstrated the increase in use of preventive asthma medications, such as inhaled corticosteroids, among US children with asthma during the same period.29 However, many children with asthma and their caregivers do not use preventive medications or have written instructions for handling acute asthma and for adjustment of medication before exposures.30 The observed temporal trends to date allow optimism that adverse outcomes can be prevented and the burden reduced. However, the large remaining burden of asthma suggests the need for sustained efforts for children with asthma.
The promising temporal trends in the incidence of hospitalization and in-hospital mortality contrast sharply with our findings that charges related to asthma hospitalization increased over time, even after adjusting for inflation. Despite the public health burden of asthma, there have been no recent studies examining temporal trends in hospital charges or direct cost among US children with asthma. Furthermore, there is a wide range in the national estimates of direct cost of asthma hospitalization that are available from the literature ranging from $186 million to $2.1 billion, depending on the study methodology and time period.31-35 Nevertheless, we observed a 26% increase in national charges from $1.3 billion in 2000 to $1.6 billion in 2009. This increase was driven by increases in the average hospital charge per case-day, because the volume of hospitalizations declined and the length of stay slightly decreased during the study period. Reasons for increasing hospital charges per case are likely multifactorial. The population of asthma may be similar in severity but their inpatient use may be increasing. Alternatively, the noticeable rise in the proportion of childhood asthma hospitalizations with high-risk medical conditions might lead to more intensive resource use, such as non-invasive and invasive respiratory support. Indeed, the attenuation of the temporal trends in mechanical ventilation use after adjustment for high-risk medical conditions suggests an important contribution of this variable to more intensive resource use. Additionally, despite the favorable temporal trend in some clinical outcomes (e.g., in-hospital mortality), the literature demonstrated significant practice variations and gaps between accepted best practices for acute asthma care and actual care delivered (i.e., important differences in process measures).23, 36, 37 The latter findings might contribute to the increasing financial burden.
Our study can better inform systems of care for children with asthma. At the health system level, the increasing financial burden should facilitate studies to evaluate its determinants and identify systems to achieve more cost-effective approaches to improve outcomes of children with asthma. At the individual provider and community level, despite the presence of an existing gap between evidence-based guidelines and actual care delivered, clinical studies and pilot programs have demonstrated that increased provider adherence to the National Asthma Education and Prevention Program guidelines can be achieved and is effective in decreasing asthma adverse events.23, 38-40 Future research should focus on knowledge translation strategies to address the important care gaps that remain.
Our study has several potential limitations. First, the KID contains discharge-level records and not patient-level records. Thus, we are unable to detect multiple hospitalizations for each patient. It is possible that a proportion of patients might have been hospitalized multiple times in the same year. In this case, because mortality events are not recurrent, the number of deaths should not change. Second, we used an administrative database of discharge-level data, without clinical information beyond that captured in ICD-9-CM codes. We might have underestimated or overestimated the frequency of asthma hospitalization and misdiagnosed with lower respiratory tract infections, such as bronchitis and pneumonia.41 However, we have conducted sensitivity analyses to address this issue, and it is difficult to postulate that diagnostic substitution explains the observed trend. Third, the KID data do not include some helpful clinical covariates, such as the child's history of asthma and their pre-hospitalization level of severity and control. Thus, as with any observational study, the observed trends may be confounded by these factors. Lastly, hospital billing practices might change over time accounting for the reported increase in mechanical ventilation use and hospital charge for childhood asthma.
Using a nationally-representative database of US pediatric hospitalizations between 2000 and 2009, we found significant declines in the incidence of asthma hospitalizations and in-hospital mortality among these asthma-related hospitalizations. These temporal trends indicate that, on a national level, earlier progress in reducing the impact of these serious asthma outcomes has continued. In contrast to these declines, use of mechanical ventilation and hospital charges for asthma hospitalizations increased markedly. Although we demonstrated the promising temporal trends in childhood asthma outcomes, the large asthma burden and continued adverse outcomes present an ongoing public health challenge. To achieve further improvement in clinical outcomes, clinicians and health service researchers need continued efforts to bridge the care gaps. Furthermore, understanding the expenditures of asthma hospitalization may assist policy makers and program administrators in their assessment of more cost-effective approaches to the management of childhood asthma.
Acknowledgments
K.H. and Y.T. were supported, in part, by St. Luke's Life Science Institute (Tokyo, Japan). C.C. was supported by the National Institutes of Health (U01 AI-87881). C.C. provided asthma-related consultation for Genentech, GSK, Merck, Novartis, and Pfizer.
Abbreviations
- AHRQ
Agency for Healthcare Research and Quality
- CCS
Clinical Classifications Software
- HCUP
Healthcare Cost and Utilization Project
- ICD-9-CM
International Classification of Diseases, Ninth Revision, Clinical Modification
- KID
Kids’ Inpatient Database
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
The other authors declare no conflicts of interest.
REFERENCES
- 1.Akinbami LJ, Moorman JE, Garbe PL, Sondik EJ. Status of childhood asthma in the United States, 1980-2007. Pediatrics. 2009;123(Suppl 3):S131–45. doi: 10.1542/peds.2008-2233C. [DOI] [PubMed] [Google Scholar]
- 2.Akinbami LJ, Schoendorf KC. Trends in childhood asthma: prevalence, health care utilization, and mortality. Pediatrics. 2002;110:315–22. doi: 10.1542/peds.110.2.315. [DOI] [PubMed] [Google Scholar]
- 3.Newacheck PW, Halfon N. Prevalence, impact, and trends in childhood disability due to asthma. Arch Pediatr Adolesc Med. 2000;154:287–93. doi: 10.1001/archpedi.154.3.287. [DOI] [PubMed] [Google Scholar]
- 4.American Lung Association [2013 January 15];Trends in asthma morbidity and mortality. 2012 Available from http://www.lung.org/finding-cures/our-research/epidemiology-and-statistics-rpts.html.
- 5.Hartman ME, Linde-Zwirble WT, Angus DC, Watson RS. Trends in admissions for pediatric status asthmaticus in New Jersey over a 15-year period. Pediatrics. 2010;126:e904–11. doi: 10.1542/peds.2009-3239. [DOI] [PubMed] [Google Scholar]
- 6.Centers for Disease Control and Prevention National surveillance of asthma: United States, 2001-2010.] Available from http://www.cdc.gov/asthma/asthmadata.htm.
- 7.Akinbami LJ, Moorman JE, Liu X. Asthma prevalence, health care use, and mortality: United States, 2005-2009. Natl Health Stat Report. 2011:1–14. [PubMed] [Google Scholar]
- 8.Expert Panel Report 3 (EPR-3): Guidelines for the diagnosis and management of asthma-summary report 2007. J Allergy Clin Immunol. 2007;120:S94–138. doi: 10.1016/j.jaci.2007.09.043. [DOI] [PubMed] [Google Scholar]
- 9.Barnett SB, Nurmagambetov TA. Costs of asthma in the United States: 2002-2007. J Allergy Clin Immunol. 2011;127:145–52. doi: 10.1016/j.jaci.2010.10.020. [DOI] [PubMed] [Google Scholar]
- 10.Lozano P, Sullivan SD, Smith DH, Weiss KB. The economic burden of asthma in US children: estimates from the National Medical Expenditure Survey. J Allergy Clin Immunol. 1999;104:957–63. doi: 10.1016/s0091-6749(99)70075-8. [DOI] [PubMed] [Google Scholar]
- 11.Bahadori K, Doyle-Waters MM, Marra C, Lynd L, Alasaly K, Swiston J, et al. Economic burden of asthma: a systematic review. BMC Pulm Med. 2009;9:24. doi: 10.1186/1471-2466-9-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Healthcare and Cost Utilization Project . Kids’ Inpatient Database, 2009. Agency for Healthcare Research and Quality; Rockville, MD: 2011. [Google Scholar]
- 13.Lee GE, Lorch SA, Sheffler-Collins S, Kronman MP, Shah SS. National hospitalization trends for pediatric pneumonia and associated complications. Pediatrics. 2010;126:204–13. doi: 10.1542/peds.2009-3109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Simon TD, Berry J, Feudtner C, Stone BL, Sheng X, Bratton SL, et al. Children with complex chronic conditions in inpatient hospital settings in the United States. Pediatrics. 2010;126:647–55. doi: 10.1542/peds.2009-3266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.HUCP Kids’ Inpatient Database Comparision Report. Healthcare Cost and Utilization Project. Agency for Healthcare Research and Quality; Available from http://www.hcupus.ahrq.gov/db/nation/kid/kidrelatedreports.jsp. [Google Scholar]
- 16.KID Related Reports. Healthcare Cost and Utilization Project. Agency for Healthcare Research and Quality; Rockville, MD: Available from http://www.hcupus.ahrq.gov/kidoverview.jsp. [Google Scholar]
- 17.Feudtner C, Hays RM, Haynes G, Geyer JR, Neff JM, Koepsell TD. Deaths attributed to pediatric complex chronic conditions: national trends and implications for supportive care services. Pediatrics. 2001;107:E99. doi: 10.1542/peds.107.6.e99. [DOI] [PubMed] [Google Scholar]
- 18.United States Bureau of the Census Census regions and divisions of the United States. Available from http://www.census.gov/geo/www/us_regdiv.pdf.
- 19.The National Association of Children's Hospitals and Related Institutions classification criteria. National Association of Children's Hospitals and Related Institutions; [2012 Nov 28]. Available from http://www.childrenshospitals.net. [Google Scholar]
- 20.US Census Bereau Population estimates. Available from http://www.census.gov/popest/
- 21.Consumer Price Index. United States Department of Labor, Bureau of Labor Statistics. Available from http://www.bls.gov/cpi/home.htm.
- 22.Lagu T, Rothberg MB, Shieh MS, Pekow PS, Steingrub JS, Lindenauer PK. Hospitalizations, costs, and outcomes of severe sepsis in the United States 2003 to 2007. Crit Care Med. 2012;40:754–61. doi: 10.1097/CCM.0b013e318232db65. [DOI] [PubMed] [Google Scholar]
- 23.Tsai CL, Sullivan AF, Gordon JA, Kaushal R, Magid DJ, Blumenthal D, et al. Quality of care for acute asthma in 63 US emergency departments. J Allergy Clin Immunol. 2009;123:354–61. doi: 10.1016/j.jaci.2008.10.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Russo MJ, McConnochie KM, McBride JT, Szilagyi PG, Brooks AM, Roghmann KJ. Increase in admission threshold explains stable asthma hospitalization rates. Pediatrics. 1999;104:454–62. doi: 10.1542/peds.104.3.454. [DOI] [PubMed] [Google Scholar]
- 25.Thill PJ, McGuire JK, Baden HP, Green TP, Checchia PA. Noninvasive positive-pressure ventilation in children with lower airway obstruction. Pediatr Crit Care Med. 2004;5:337–42. doi: 10.1097/01.pcc.0000128670.36435.83. [DOI] [PubMed] [Google Scholar]
- 26.Nathens AB, Jurkovich GJ, Cummings P, Rivara FP, Maier RV. The effect of organized systems of trauma care on motor vehicle crash mortality. JAMA. 2000;283:1990–4. doi: 10.1001/jama.283.15.1990. [DOI] [PubMed] [Google Scholar]
- 27.Rautava L, Lehtonen L, Peltola M, Korvenranta E, Korvenranta H, Linna M, et al. The effect of birth in secondary- or tertiary-level hospitals in Finland on mortality in very preterm infants: a birth-register study. Pediatrics. 2007;119:e257–63. doi: 10.1542/peds.2006-1964. [DOI] [PubMed] [Google Scholar]
- 28.Morse RB, Hall M, Fieldston ES, McGwire G, Anspacher M, Sills MR, et al. Hospital-level compliance with asthma care quality measures at children's hospitals and subsequent asthma-related outcomes. JAMA. 2011;306:1454–60. doi: 10.1001/jama.2011.1385. [DOI] [PubMed] [Google Scholar]
- 29.Kit BK, Simon AE, Ogden CL, Akinbami LJ. Trends in preventive asthma medication use among children and adolescents, 1988-2008. Pediatrics. 2012;129:62–9. doi: 10.1542/peds.2011-1513. [DOI] [PubMed] [Google Scholar]
- 30.Diette GB, Skinner EA, Nguyen TT, Markson L, Clark BD, Wu AW. Comparison of quality of care by specialist and generalist physicians as usual source of asthma care for children. Pediatrics. 2001;108:432–7. doi: 10.1542/peds.108.2.432. [DOI] [PubMed] [Google Scholar]
- 31.Weiss KB, Gergen PJ, Hodgson TA. An economic evaluation of asthma in the United States. N Engl J Med. 1992;326:862–6. doi: 10.1056/NEJM199203263261304. [DOI] [PubMed] [Google Scholar]
- 32.Kamble S, Bharmal M. Incremental direct expenditure of treating asthma in the United States. J Asthma. 2009;46:73–80. doi: 10.1080/02770900802503107. [DOI] [PubMed] [Google Scholar]
- 33.Weiss KB, Sullivan SD, Lyttle CS. Trends in the cost of illness for asthma in the United States, 1985-1994. J Allergy Clin Immunol. 2000;106:493–9. doi: 10.1067/mai.2000.109426. [DOI] [PubMed] [Google Scholar]
- 34.Smith DH, Malone DC, Lawson KA, Okamoto LJ, Battista C, Saunders WB. A national estimate of the economic costs of asthma. Am J Respir Crit Care Med. 1997;156:787–93. doi: 10.1164/ajrccm.156.3.9611072. [DOI] [PubMed] [Google Scholar]
- 35.Halfon N, Newacheck PW. Trends in the hospitalization for acute childhood asthma, 1970-84. Am J Public Health. 1986;76:1308–11. doi: 10.2105/ajph.76.11.1308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Scribano PV, Lerer T, Kennedy D, Cloutier MM. Provider adherence to a clinical practice guideline for acute asthma in a pediatric emergency department. Acad Emerg Med. 2001;8:1147–52. doi: 10.1111/j.1553-2712.2001.tb01131.x. [DOI] [PubMed] [Google Scholar]
- 37.McDermott MF, Grant EN, Turner-Roan K, Li T, Weiss KB. Asthma care practices in Chicago-area emergency departments. Chicago Asthma Surveillance Initiative Project Team. Chest. 1999;116:167S–73S. doi: 10.1378/chest.116.suppl_2.167s. [DOI] [PubMed] [Google Scholar]
- 38.Cloutier MM, Hall CB, Wakefield DB, Bailit H. Use of asthma guidelines by primary care providers to reduce hospitalizations and emergency department visits in poor, minority, urban children. J Pediatr. 2005;146:591–7. doi: 10.1016/j.jpeds.2004.12.017. [DOI] [PubMed] [Google Scholar]
- 39.Kattan M, Crain EF, Steinbach S, Visness CM, Walter M, Stout JW, et al. A randomized clinical trial of clinician feedback to improve quality of care for inner-city children with asthma. Pediatrics. 2006;117:e1095–103. doi: 10.1542/peds.2005-2160. [DOI] [PubMed] [Google Scholar]
- 40.Sullivan SD, Weiss KB, Lynn H, Mitchell H, Kattan M, Gergen PJ, et al. The cost-effectiveness of an inner-city asthma intervention for children. J Allergy Clin Immunol. 2002;110:576–81. doi: 10.1067/mai.2002.128009. [DOI] [PubMed] [Google Scholar]
- 41.Mansbach JM, Espinola JA, Macias CG, Ruhlen ME, Sullivan AF, Camargo CA., Jr Variability in the diagnostic labeling of nonbacterial lower respiratory tract infections: a multicenter study of children who presented to the emergency department. Pediatrics. 2009;123:e573–81. doi: 10.1542/peds.2008-1675. [DOI] [PubMed] [Google Scholar]