Abstract
Purpose
To present the incidence, demographics, and clinical presentation of patients diagnosed with renal fibromuscular dysplasia (FMD) who underwent computed tomographic angiographic (CTA) for evaluation of living renal donor protocol.
Methods and materials
A retrospective review was performed from January 1, 2000, to December 31, 2011 on patients who underwent CTA for evaluation of living renal donor protocol. Two thousand six hundred and forty patients were identified and only those with a diagnosis of FMD by the radiology report underwent independent reader evaluation of the CTA for the presence of FMD and associated characteristics. In addition, the demographics, medical history, and presentation were reviewed using the electronic medical chart.
Results
Sixty-eight patients (2.6%; 59 female) with an average age of 52 ± 10 years were diagnosed with FMD according to the independent readers who evaluated the CTA. Unilateral FMD was observed in 46 patients (68%) and bilateral in 22 patients (32%). Three patients had aneurysms of the renal artery. The comorbidities included hypertension (n=21, 31%), dyslipidemia, (n=13, 19%), history of migraines (n=3, 4%), and history of smoking (n=14, 21%). No patients had diabetes mellitus, coronary artery disease, or family history of FMD. Twenty-one patients (31%) had a history of hypertension with 13 patients (62%) treated with antihypertensive medications.
Conclusion
The incidence of FMD in patients who underwent CTA for evaluation of living renal donor protocol is 2.6%.
Keywords: renal artery stenosis, fibromuscular dysplasia, hypertension
Introduction
The etiology of fibromuscular dysplasia (FMD) remains largely unknown. It is well recognized that the incidence is higher in women and the most common clinical presentation is hypertension. It is estimated that the incidence in the general population is 2% to 3% (1). The incidence of FMD in potential living renal donors is reported to be 4% to 6% (2–5). The purpose of the present study was to present the incidence of FMD in living renal donors undergoing computed tomographic angiograms (CTAs) of the abdomen and pelvis over an 11-year period. In addition, the patient demographics, CTA findings, and outcomes are presented.
Materials and Methods
Study Population
Institutional review board approval was obtained prior to conducting the study. From January 1, 2000, to December 31, 2011, the radiology information management system database was searched for an examination code of abdominal or pelvic CTA and a key phrase of potential renal donor. Cases of FMD were also searched using keywords of fibromuscular dysplasia, FMD, beaded, pearl, or string, in any and all combinations within the interpretation of the CTA. Patients with diagnosis of FMD were identified and the CTAs evaluated by independent readers as well as the demographics, comorbidities, and family history was reviewed.
Description of CTA Protocol
Over this time period, a variety of different multi-detector CT scanners were used to perform examinations, including the following: 4 multi-detector-row CT (MDCT) (Lightspeed QX/i; GE Medical Systems, Milwaukee, WI), 16 MDCT (Somatom Sensation 16; Siemens Medical Solutions, Forchheim, Germany), and more recently, 64 MDCT (Somatom Sensation 64; Siemens Medical Solutions) or 64 dual-source MDCT (Somatom Definition, Somatom Definition Flash; Siemens Medical Solutions) scanners. For example, the CTA parameters utilizing 4 MDCT included thickness of 1.25 mm, increment of 0.75 mm, field of view of 25 cm, rotation time of 0.8 sec, and scan delay of 18 sec after starting intravenous (IV) injection of 140 mL of iopamidol (300 mgI/mL), at an injection rate of 5 mL/sec using a mechanical power injector. CTA parameters utilizing state-of-the-art 64 MDCT scanners included thickness of 1.5 mm, increment of 0.8 mm, field of view of 25 cm, rotation time of 0.5 sec, collimation of 64 × 0.6, and scan delay triggered by automatic bolus tracking (CARE Bolus, Siemens Medical Solutions) following IV injection of 140 mL of iohexol (350 mgI/mL), at an injection rate of 5 mL/sec using a mechanical power injector. Contrast dosing was also adjusted based on patient weight. A combination of axial and multi-planar reconstructed images was used for interpretation.
A diagnosis of medial fibroplasia subtype of FMD was made based on the string of beads appearance, defined as alternating segments of concomitant stenoses and post-stenotic dilatation involving the renal artery. The study team independent of the original reading then reviewed only the CTAs, which were identified as having FMD. Unilateral or bilateral involvement of the renal artery with FMD was noted. Bilateral lesions were then further divided into which renal artery, right or left, had greater extent of involvement, taking into account both length and degree of beading. Length of involvement was measured on axial or coronal images from origin to distal point of beading. Degree of involvement was determined by visual inspection of the severity of beading in each artery. In addition, aneurysm and ectasia were noted. Aneurysm was defined as a focal vessel dilatation which was more than 2 times the proximal luminal diameter of the non-diseased renal artery, while ectasia was defined as less than or equal to 2 times the proximal luminal diameter of the non-diseased renal artery.
Statistical Analysis
Categorical variables were expressed as ratios and percentages. Continuous variables were expressed as mean ± standard deviation (SD) or median (range). SAS version 9 (SAS Institute Inc., Cary, North Carolina) was used for all statistical analyses.
Results
Patient Characteristics
As part of a renal donor protocol, 2,640 patients underwent CTAs of the abdomen and pelvis. Sixty-eight (2.6%) patients with an average age of 52 ± 10 years (59 [87%] women) were diagnosed with FMD according to CTA report (Table 1). The cardiovascular risk factors included hypertension (n=21, 31%), dyslipidemia, (n=13, 19%), history of smoking (n=14, 21%), and history of migraines (n=3, 4%). Five patients (7%) had a history of oral contraceptives (OCPs) and/or hormone replacement therapy use and 8 patients (12%) used nonsteroidal anti-inflammatory drugs (NSAIDs). The mean body mass index was 27 ± 4 kg/m2. There were no patients with a history of diabetes mellitus or coronary artery disease. One patient (68-year-old) was a smoker and had peripheral arterial disease with history of dyslipidemia requiring a statin at the time of diagnosis with FMD. Fifteen patients (22%) had a family history of coronary artery disease; however, no patients had a family history of FMD. Five patients (7%) had a family history of polycystic kidney disease.
Table 1.
Study Group Demographics
| Study variable | Study group N (%) |
|---|---|
| N | 68 |
| Women (%) | 59 (87%) |
| Mean age at diagnosis (years old) | 52 ± 10 |
| BMI | 27 ± 4 |
| White | 57 (84%) |
| Risk Factors (%) | |
| Hypertension | 21 (31%) |
| Dyslipidemia | 13 (19%) |
| Peripheral arterial disease | 1 (1%) |
| Statin usage | 5 (7%) |
| Smoking (current or past) | 14 (21%) |
| Diabetes | 0 (0%) |
| Stroke | 0 (0%) |
| Coronary artery disease | 0 (0%) |
| Chronic renal insufficiency | 0 (0%) |
| Carotid disease | 0 (0%) |
| Family history of coronary artery disease | 15 (22%) |
| Chronic renal insufficiency | 0 (0%) |
| NSAIDs | 8 (12%) |
| Estrogen use (OCPs or HRT) | 5 (7%) |
| Migraines | 3 (4%) |
Abbreviations: BMI, body mass index; HRT, hormone replacement therapy; NSAIDs, nonsteroidal anti-inflammatory drugs; OCPs, oral contraceptives.
CTA Characteristics of Renal FMD Lesions
The FMD characteristics according to the CTA findings are listed in table 2. Unilateral disease was observed in 46 patients (68%) with the right renal artery being involved in 36 patients and the left in 10. Twenty-two patients (32%) had bilateral renal artery FMD involvement with greater involvement on the right side in 9 patients (41%), left side in 3 (14%), and equal amount involving the bilateral renal arteries in 11 (50%). Three patients (4%) had extrarenal involvement of FMD with 2 involving the superior mesenteric artery and 1 the external iliac arteries bilaterally. Three patients (4%) had five aneurysms of the renal artery, with 1 patient having multiple aneurysms with 2 on the left and 1 on the right (Fig. 1).
Table 2.
CT characterization of FMD
Renal Artery Stenosis (RAS) Location
| Unilateral FMD | 46 (68%) |
|
| |
| Left sided FMD | 10 (14%) |
| Right sided FMD | 36 (53%) |
|
| |
| Bilateral FMD | 22 (32%) |
|
| |
| Right renal artery predominant | 8 (36%) |
| Left renal artery predominant | 3 (14%) |
| Equivocal involvement | 11 (50%) |
|
| |
| Aneurysms | 3 (4%) |
Abbreviation: FMD, fibromuscular dysplasia.
Figure 1.
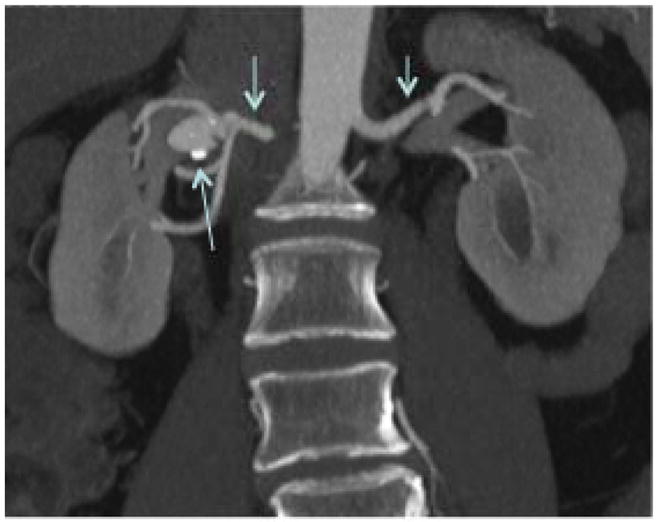
CT Angiogram showing a renal artery aneurysm with FMD changes (arrows).
Hypertension
Twenty-one patients (31%) had a history of hypertension with 13 patients (62%) treated with antihypertensive medications. Eleven of the 22 patients (50%) with bilateral FMD had hypertension. Of the 46 patients with unilateral disease, 10 (22%) were hypertensive.
Discussion
In the present study, based on CTA results, a 2.6% incidence of renal artery FMD in renal donor patients was observed. As expected, the majority of the patients (87%) were women. The average age of the patients was 52 years. Patients presented with bilateral FMD approximately one third of the time with the majority of the patients having right-sided involvement. Three patients had renal artery aneurysms. Three patients presented with extrarenal FMD involving the external iliac artery or superior mesenteric artery. The majority of the patients were asymptomatic with approximately one third (21 patients) having a history of hypertension. Patients who had bilateral renal artery FMD had a higher incidence of hypertension.
There are three types of FMD: intimal, medial, and adventitial. The majority of the FMD is the medial form typically described as the classic “string of beads sign” that has been observed in 65% to 90% of FMD lesions (6, 7). The string of beads finding is easily detected using CTA (8). Several studies have compared DSA and CTA for detection of renal artery stenosis (RAS) and have showed slightly lower sensitivities and specificities for CTA ranging from 88% to 100% and 97% to 99%, respectively (9–12). In the present study, the incidence of FMD was 2.6% by CTA compared to 2% to 6.6% in DSA studies (2, 5). The difference in incidence is likely a reflection of the imaging modality used for detection.
The major advantages of CTA when compared to DSA are that it is noninvasive and offers anatomical visualization of other parts of the body including the mesenteric vessels (8). Mild changes of FMD were most likely less conspicuous by CTA especially using a 4 MDCT scanner with IV injection of 140 mL of iodinated contrast media (300 mgI/mL) than the current state of the art 64 MDCT CTA with IV injection of 140 mL of iodinated contrast media (350 mgI/mL). It is reasonable to speculate that the moderate to severe changes of FMD should have been visualized with CTA when utilizing a 4 MDCT scanner with IV injection of 140 mL of contrast media (300 mgI/mL).
As expected, the majority of the patients were women. With respect to the average age of the patient, much of the previous literature details renal FMD affecting patients between 15–50 (1, 6). In the present study, 49 patients (72%) were older than 50 years of age. These data suggest renal FMD might have a higher prevalence in an older population than previously thought and has been supported by observations from other studies (1, 2, 13).
In the present study, approximately one-third of the patients had bilateral FMD. This is lower than other studies that have reported bilateral disease involvement in 39% to 64% of patients using CTA or DSA analysis (2–5). FMD can involve the extrarenal blood vessels. In the present study, FMD was observed in the superior mesenteric artery and external iliac arteries consistent with other studies (1). A minority of patients (4%) had renal artery aneurysm that is slightly lower than reported incidences of 8% to 9.8% consistent with other studies (1–5). None of the patients had renal artery dissection or renal artery occlusion.
Hypertension was the main clinical presentation consistent with other studies (15). Patients with bilateral disease had a greater incidence of hypertension (50%) compared to unilateral disease (22%). None of the patients had refractory hypertension or chronic kidney disease. This is consistent with other studies that have found that most renal FMD lesions have no presenting symptoms related to hypertension (1, 6).
There are some limitations in the current study. This study is based on living renal donors that may be a healthier population than the general population. In addition, only the reports of the CTA were reviewed and not all CTAs were reviewed for the presence of FMD. Therefore extrapolation of the data to the general population may be unreliable. Another limitation is that renal FMD was not confirmed in all patients with an angiogram. Therefore, the incidence and extent of renal FMD maybe under diagnosed.
In the present study, a 2.6% incidence of FMD in patients who underwent renal donor CTA evaluation was observed. The average age of the patient was 52 years old and nearly 90% were women. One third of the patients had bilateral disease and often, patients were asymptomatic.
Acknowledgments
This work was funded by a R01HL098967 (SM) from the National Heart, Lung, And Blood Institute.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Olin JW, Froehlich J, Gu X, et al. The United States Registry for Fibromuscular Dysplasia: Results in the First 447 Patients. Circulation. 2012;125:3182–3190. doi: 10.1161/CIRCULATIONAHA.112.091223. [DOI] [PubMed] [Google Scholar]
- 2.Cragg AH, Smith TP, Thompson BH, et al. Incidental fibromuscular dysplasia in potential renal donors: long-term clinical follow-up. Radiology. 1989;172:145–147. doi: 10.1148/radiology.172.1.2662248. [DOI] [PubMed] [Google Scholar]
- 3.Blondin D, Lanzman R, Schellhammer F, et al. Fibromuscular dysplasia in living renal donors: still a challenge to computed tomographic angiography. Eur J of Rad. 2010;75:67–71. doi: 10.1016/j.ejrad.2009.03.014. [DOI] [PubMed] [Google Scholar]
- 4.Neymark E, LaBerge JM, Hirose R, et al. Arteriographic detection of renovascular disease in potential renal donors: incidence and effect on donor surgery. Radiology. 2000;214:755–760. doi: 10.1148/radiology.214.3.r00mr18755. [DOI] [PubMed] [Google Scholar]
- 5.Andreoni KA, Weeks SM, Gerber DA, et al. Incidence of donor renal fibromuscular dysplasia: does it justify routine angiography? Transplantation. 2002;73:1112–1116. doi: 10.1097/00007890-200204150-00018. [DOI] [PubMed] [Google Scholar]
- 6.Safian RD, Textor SC. Renal-artery stenosis. N Engl J Med. 2001;344:431–442. doi: 10.1056/NEJM200102083440607. [DOI] [PubMed] [Google Scholar]
- 7.Stanley JC, Gewertz BL, Bove EL, Sottiurai V, Fry WJ. Arterial fibrodysplasia. Histopathologic character and current etiologic concepts. Arch of Sur. 1975;110:561–566. doi: 10.1001/archsurg.1975.01360110107018. [DOI] [PubMed] [Google Scholar]
- 8.Sabharwal R, Vladica P, Coleman P. Multidetector spiral CT renal angiography in the diagnosis of renal artery fibromuscular dysplasia. Eur J of Rad. 2007;61:520–527. doi: 10.1016/j.ejrad.2006.10.005. [DOI] [PubMed] [Google Scholar]
- 9.Kim TS, Chung JW, Park JH, Kim SH, Yeon KM, Han MC. Renal artery evaluation: comparison of spiral CT angiography to intra-arterial DSA. J of Vasc Interv Radiol. 1998;9:553–559. doi: 10.1016/s1051-0443(98)70320-3. [DOI] [PubMed] [Google Scholar]
- 10.Galanski M, Prokop M, Chavan A, Schaefer C, Jandeleit K, Nischelsky JE. Renal artery stenoses: spiral CT angiography. Radiology. 1993;189:185–192. doi: 10.1148/radiology.189.1.8372191. [DOI] [PubMed] [Google Scholar]
- 11.Rubin GD, Dake MD, Napel S, et al. Spiral CT of renal artery stenosis: comparison of three-dimensional rendering techniques. Radiology. 1994;190:181–189. doi: 10.1148/radiology.190.1.8259402. [DOI] [PubMed] [Google Scholar]
- 12.Beregi JP, Elkohen M, Deklunder G, Artaud D, Coullet JM, Wattinne L. Helical CT angiography compared with arteriography in the detection of renal artery stenosis. AJR. 1996;167:495–501. doi: 10.2214/ajr.167.2.8686635. [DOI] [PubMed] [Google Scholar]
- 13.Pascual A, Bush HS, Copley JB. Renal fibromuscular dysplasia in elderly persons. Am J Kid Dis. 2005;45:e63–e66. doi: 10.1053/j.ajkd.2005.01.039. [DOI] [PubMed] [Google Scholar]
- 14.Kincaid OW, Davis GD, Hallermann FJ, Hunt JC. Fibromuscular dysplasia of the renal arteries. Arteriographic features, classification, and observations on natural history of the disease. AJR. 1968;104:271–282. [PubMed] [Google Scholar]


