Abstract
Background
This study examined relationships of extremes in neighborhood socioeconomic status with use of tobacco, alcohol, marijuana and other drugs. Hypotheses were (1) residence in disadvantaged neighborhoods would be positively associated with stress-related and higher-risk substance use patterns (e.g., drug use), and (2) residence in affluent neighborhoods would be positively associated with “healthy” substance use (e.g., drinking within recommended guidelines) and negatively associated with substance use patterns incompatible with a culture of health. Age was examined as a potential moderator.
Methods
Data were from nationally-representative samples of U.S. adults (N=14,531) from the 2000 and 2005 National Alcohol Surveys linked with indicators of neighborhood SES from the 2000 U.S. Decennial Census. Analyses included gender-stratified multivariate logistic regression using weights to adjust for sampling and non-response.
Results
As hypothesized, compared to middle-class neighborhoods, residence in disadvantaged neighborhoods was associated with higher odds of both men’s and women’s tobacco use and with women’s other drug use. Residence in affluent neighborhoods was associated with lower odds of men’s tobacco use and women’s marijuana use. The association of neighborhood SES with men’s tobacco use was modified by age, with the highest odds of daily tobacco use evident for all men in disadvantaged neighborhoods, as well as for younger men in middle-class neighborhoods. There were no significant associations of either alcohol outcome with neighborhood SES.
Conclusions
Increased risk of substance use for younger residents in both disadvantaged and middle-class neighborhoods and for older residents in disadvantaged neighborhoods suggest a need for targeted prevention interventions.
Keywords: neighborhood, tobacco, alcohol, substance use
1. INTRODUCTION
The importance of the neighborhood context for successful child and adolescent development has long been acknowledged (Bronfenbrenner, 1979), and studies of neighborhood effects on youth have proliferated over the past two decades (Leventhal and Brooks-Gunn, 2000). Neighborhood effects persist into adulthood, as the place one lives provides a context for both work and leisure, and many people develop important social relationships with neighbors. In the best cases, neighborhoods provide infrastructure and social structures that are positive resources for residents both young and old (Browning and Cagney, 2003; Robert, 1999; Wen et al., 2003); however, neighborhoods also can cause stress and tension (Cohen et al., 2003; Ewart and Suchday, 2002; Fitzpatrick and LaGory, 2000) or provide contextual cues and social norms promoting health risk behaviors such as alcohol or drug use (Ahern et al., 2008). For some, the combination of neighborhood stress and permissive social norms may result in tobacco, alcohol or other drug use to cope with increased anxiety and tension (Greeley and Oei, 1999; Moos et al., 1989). Neighborhood effects vary quite widely according to individual attributes, including the amount of time spent near home (Inagami et al., 2007). The current study examines effects of neighborhood socioeconomic status (SES) on substance use in a national sample of U.S. adults and examines variation by gender and age.
Studies of neighborhood effects on adult health outcomes suggest neighborhood SES is an important marker of a variety of contextual factors that impact health and behavior. Disadvantaged neighborhoods often suffer from illicit drug sales and proliferation of alcohol outlets including bars and liquor stores (Bluthenthal et al., 2008), as well as erosion of social controls of behaviors considered to be risky, antisocial or unconventional (Sampson and Groves, 1989; Wilson, 1987). Visible drug sales (Bradizza and Stasiewicz, 2003; Kadushin et al., 1998; Lambert et al., 2004), high alcohol outlet density (Bryden et al., 2012; Livingston et al., 2007; Theall et al., 2009) and social disorganization (Duncan et al., 2000; Esbensen and Huizinga, 1990; Hill and Angel, 2005; Lambert et al., 2004; Wilson et al., 2005) each contribute to substance use and associated problems. At the other end of the socioeconomic spectrum are more affluent areas. Residents of these areas often embrace health-related lifestyles (Cockerham et al., 1997; Ross, 2000). In contrast with neighborhood disadvantage, neighborhood affluence may be associated with certain types of light, recreational substance use patterns that are compatible with a sub-culture of health, such as moderate alcohol use.
Some studies show strong associations between neighborhood disadvantage and increased use of tobacco, alcohol or drugs (Boardman et al., 2001; Datta et al., 2006; Diez Roux et al., 2003; Giggs et al., 1989; Stimpson et al., 2007; Waitzman and Smith, 1998; Williams and Latkin, 2007). A recent review found that neighborhood SES was associated with both adult and adolescent substance use outcomes, with effects of neighborhood disadvantage noted more consistently in samples of adults (Karriker-Jaffe, 2011). There have only been a few studies conducted in the U.S. with national samples, as in the current study. Those suggest that neighborhood disadvantage is associated with recreational and illicit drug use (Ford and Beveridge, 2006; Hoffmann, 2002), heavy drinking (Karriker-Jaffe et al., 2012; Stimpson et al., 2007), and alcohol-related problems (Jones-Webb et al., 1997; Karriker-Jaffe et al., 2012). However, these national studies of neighborhood effects on drug outcomes often find differing results depending on the specific neighborhood measure employed. This was the case in the study by Hoffmann (2002), which documented a positive association between male joblessness in the neighborhood and adolescent drug use, as well as a negative association of the same outcome with neighborhood poverty. Findings also tend to vary by the particular outcome considered, such as in the study by Ford and Beverage (2006), which showed neighborhood disadvantage was associated with increased use of barbiturates and amphetamines, but not greater use of marijuana, cocaine, LSD or tranquilizers. The current study contributes to the extant literature by considering separate substance use outcomes in addition to alcohol, while using a Census-based composite measure of neighborhood socioeconomic status (SES) that allows differentiation of effects of affluent and disadvantaged (compared to middle-class) neighborhoods in a national sample of U.S. adults.
Characterization of neighborhoods in this manner is important, as there may be unique characteristics associated with conditions of advantage that are not captured by a mere absence of disadvantage (Robert, 1999). That is, there may be distinct benefits to residence in the most affluent areas that are not present in other non-poor, middle-class neighborhoods (Browning and Cagney, 2003). Thus, the two extremes in neighborhood socioeconomic conditions (i.e., disadvantage and affluence) may differ in their relationships with substance use outcomes. For example, there is evidence for adults that neighborhood affluence is associated with being an alcohol drinker (Galea et al., 2007a, 2007b) and regularly using alcohol (Chuang et al., 2005; Pollack et al., 2005), while neighborhood disadvantage is associated with abstinence from alcohol (Karriker-Jaffe et al., 2012). It remains unclear whether neighborhood affluence is associated (either positively or negatively) with problem drinking, although analyses using a subset of the data included in the present investigation suggest there may not be a strong association (Mulia and Karriker-Jaffe, 2012). Two analyses of data from New York City suggest higher neighborhood incomes (Galea et al., 2007b) and higher neighborhood education (Galea et al., 2007a) are associated with increased marijuana use, but effects on other drugs were not reported. It is unknown whether findings from prior research will replicate when national data on other drug use by adults is considered.
Thus, this study examines relationships of neighborhood SES with five substance use outcomes using data from two national samples of U.S. adults (analyzed together). The hypotheses are as follows: (1) compared to middle-class neighborhoods, residence in disadvantaged neighborhoods will be positively associated with stress-related and risky substance use patterns (daily tobacco use, monthly drunkenness, monthly use of marijuana and monthly use of other drugs), and (2) compared to middle-class neighborhoods, residence in affluent neighborhoods will be positively associated with “healthy” substance use (drinking within recommended guidelines), but negatively associated with substance use patterns incompatible with a culture of health (particularly daily tobacco use and monthly use of drugs other than marijuana).
Neighborhood effects may be more pronounced for younger adults, as they are more likely to engage in substance use than their older counterparts and they may be more involved in neighborhood-based social networks formed through school activities; however it also is possible that older adults may be more place-bound after retirement from formal employment and thus may be more strongly influenced by their residential environment (Bernard et al., 2007). As such, interactions with age also are assessed. As gender differences in relationships of substance use patterns with neighborhood SES have been suggested by other studies (Karriker-Jaffe et al., 2012; Karvonen and Rimpelä, 1996; Karvonen and Rimpelä, 1997; Matheson et al., 2011), we present gender-stratified models to highlight any differences in associations of these outcomes with neighborhood disadvantage and affluence. Finally, because some studies show neighborhood disadvantage is associated with both increased abstinence and increased heavy drinking and alcohol-related problems among some drinkers (Karriker-Jaffe et al., 2012), we conduct analyses of the alcohol outcomes in the full sample and in a restricted sample of past-year drinkers.
2. METHODS
2.1. Study design
2.1.1. Dataset
Survey data come from the 2000 and 2005 National Alcohol Surveys (NAS). Both cross-sectional surveys utilized computer-assisted telephone interviews with randomly-selected adults ages 18 and older. Each survey included oversamples of African-Americans, Hispanics, and residents from low-population states. For more details on methodology, please see Kerr et al. (2004) and Midanik and Greenfield (2003). The 2000 NAS included 7,613 respondents (58% response rate); the 2005 NAS included 6,919 respondents (56% response rate). Although lower than those of many face-to-face surveys, these response rates are typical of telephone surveys in a time of increasing barriers to random-digit dial studies in the U.S. (Midanik and Greenfield, 2002). Evidence suggests low response rates for telephone surveys may not bias estimates as much as low response rates for in-person studies, because most telephone sample losses are due to immediate hang-ups that occur prior to description of the study (Groves, 2006).
Survey data were matched with indicators of neighborhood SES from the 2000 Census (U.S. Census Bureau, 2002). Respondent addresses were matched with census geocodes by a commercial geocoding firm, and were found to be highly accurate when compared to the gold standard recommended by Krieger and colleagues (2001). Survey data then were linked via these geocodes to indicators of neighborhood SES at the census tract level. Census tracts effectively delineate social and structural determinants of health behaviors, including substance use (Cook et al., 1997; Karriker-Jaffe, 2011; Krieger et al., 2002). Approximately two-thirds (60%) of the sample had geocodes assigned based on the street address; the remainder had a geocode assigned based on the ZIP Code centroid. Preliminary analyses determined that the relationship between neighborhood SES and the outcomes did not vary significantly according to geocode precision (data available upon request). Regardless, all analyses adjusted for the precision of the geocode match.
2.1.2. Sample
The sample was 52.0% female, and the average age was 44.8 years (41.0% were under age 40). The majority (63.5%) were married or living with a partner. Most respondents (71.8%) were Caucasian, but 11.4% were African American, and 11.4% were Hispanic/Latino. Over half (57.6%) of the respondents had attended at least some college or technical school, and 66.8% were employed either full- or part-time. See Table 1 for detailed respondent characteristics by gender.
Table 1.
| Men (N=6,709) | Women (N=7,822) | |
|---|---|---|
| Married/partnered ** | 69.5 | 57.9 |
| Age ** | ||
| 18–29 years | 22.0 | 20.5 |
| 30–39 years | 21.5 | 19.4 |
| 40–49 years | 21.1 | 20.5 |
| 50–59 years | 17.6 | 17.6 |
| 60 years and older | 17.8 | 22.0 |
| Race/ethnicity ** | ||
| Caucasian | 71.3 | 72.2 |
| African American | 10.6 | 12.2 |
| Hispanic/Latino | 12.1 | 10.8 |
| Other race/ethnicity | 6.0 | 4.8 |
| Education ** | ||
| Less than high school | 12.7 | 12.3 |
| High school graduate | 29.1 | 30.6 |
| Some college | 24.8 | 28.5 |
| College graduate | 33.4 | 28.6 |
| Employment status ** | ||
| Employed | 75.1 | 59.0 |
| Unemployed | 4.0 | 4.0 |
| Not in workforce | 20.9 | 37.0 |
| Income ** | ||
| < $10,000 | 7.2 | 11.6 |
| $10,001–20,000 | 10.7 | 12.9 |
| $20,001–40,000 | 23.0 | 22.9 |
| $40,001–60,000 | 16.4 | 14.9 |
| $60,001–80,000 | 12.8 | 9.6 |
| > $80,000 | 19.6 | 12.6 |
| Missing income | 10.3 | 15.5 |
| Urban neighborhood | 60.2 | 59.5 |
| Neighborhood SES | ||
| Disadvantaged | 23.8 | 25.3 |
| Middle-class | 50.6 | 51.0 |
| Affluent | 25.6 | 23.7 |
| Daily tobacco use ** | 28.3 | 21.1 |
| Drinking within guidelines ** | 67.4 | 77.8 |
| Monthly drunkenness ** | 11.1 | 3.6 |
| Monthly marijuana use ** | 5.7 | 2.6 |
| Monthly other drug use | 3.3 | 3.6 |
Weighted percentages.
Significant gender differences assessed using bivariate F-tests.
p<.05.
p<.01.
2.2. Measures
2.2.1. Neighborhood SES
Neighborhood SES was based on composite indicators of socioeconomic disadvantage and affluence defined across three dimensions (income, educational capital and employment opportunities) using easily-interpretable, socially-relevant markers of extremes in SES (Krieger et al., 2002; Wagle, 2002; Wilson, 1987). Neighborhood disadvantage was defined using U.S. Census data on the proportions of adults without a high school diploma, males who were unemployed or not in the labor force, people with incomes below poverty, families with incomes below 50% of the U.S. median, and households without access to a car. Neighborhood affluence was defined using U.S. Census data on the proportions of families with incomes above 150% the U.S. median, households with income from secondary sources such as rent or dividends, adults over age 25 with a 4-year college degree, and adults over age 15 in management and professional occupations. The composite measures were validated in a prior study utilizing data from a subset of cases from the current sample using factor analysis and reliability assessment (Karriker-Jaffe and Kaskutas, 2009). In the current sample, each measure had high reliability (Cronbach’s alphas=.89 for disadvantage and .91 for affluence), and disadvantage was highly correlated with percent receiving public assistance (r=.73, p<.01) and proportion working class (r=.60, p<.01), while affluence was negatively correlated with these measures (r= −.53, p<.01, and r= −.89, p<.01, respectively).
Disadvantaged neighborhoods were those in the top quartile on the disadvantage composite; affluent neighborhoods were those in the top quartile on the affluence composite. Thus, 24.6% of respondents lived in disadvantaged neighborhoods and another 24.6% lived in affluent neighborhoods. Other than a small group of neighborhoods high on both disadvantage and affluence (0.8%, which were excluded), all other neighborhoods were classified as middle-class (reference group). Median household income averaged $27,868 in the sample’s disadvantaged neighborhoods and $68,630 in the affluent neighborhoods, both of which were significantly different than the median income in middle-class neighborhoods ($42,746). The national median income was $41,994 in 1999 (U.S. Census Bureau, 2002). Median housing value averaged $89,048 in disadvantaged neighborhoods and $229,883 in affluent neighborhoods, both of which were significantly different than middle-class neighborhoods ($110,497). The national median housing value was $119,600 in 1999 (U.S. Census Bureau, 2002).
2.2.2. Outcomes
Substance use outcomes were based on the past 12 months. Daily tobacco use included smoking or using other tobacco “daily or nearly daily.” Drinking within guidelines was a dichotomous variable indicating whether respondents had remained within the U.S. National Institute on Alcohol Abuse and Alcoholism’s (National Institute on Alcohol Abuse and Alcoholism, 2005) gender-specific, low-risk guidelines for daily and weekly drinking. Recommended limits for men are no more than 4 drinks per day and 14 drinks per week; limits for women are no more than 3 drinks per day and 7 drinks per week. Monthly drunkenness was a dichotomous measure indicating whether respondents drank enough to feel drunk at least once a month. Frequency of drunkenness is a strong predictor of alcohol-related problems (Midanik, 1999). In this sample, monthly drunkenness was more strongly correlated with past-year alcohol problems (r=.53 with dependence symptoms and r=.48 with negative consequences of drinking, both p<.01) than was a measure of less frequent drunkenness (i.e., got drunk more than once in past year, with r=.49 with dependence symptoms and r=.40 with negative consequences of drinking, both p<.01). Monthly marijuana use was a dichotomous measure indicating using marijuana at least “once every month or two.” Monthly illicit drug use was a dichotomous indicator of using cocaine, amphetamines or methamphetamines, heroin, tranquilizers, painkillers, hallucinogens, or prescription drugs “not as prescribed by a doctor” at least “once every month or two.” In the current sample, monthly drug use measures each were more strongly associated with past-year drug problems (r=.31 for marijuana and r=.22 for other drugs, both p<.01) than an indicator of use at least once in the past year (r=.27 for marijuana and r=.05 for other drugs, both p<.01). Both monthly drug use measures included a majority of respondents who reported using the substance on a weekly basis or more (61.1% of monthly marijuana users and 55.1% of monthly users of other drugs).
2.2.3. Control variables
Basic multivariate analyses adjusted for age (18–29 years, 30–39 years, 40–49 years, and 50–59 years, with 60 years and over as reference), race/ethnicity (African American, Hispanic/Latino, and other race/ethnicity, with Caucasian as reference), marital status (married or partnered, with single/divorced/widowed as reference), education (less than high school, high school graduate, and some college, with college graduate as reference), employment status (unemployed and not in workforce, with employed as reference), total household income before taxes (five variables starting with “less than $10,000,” with “more than $80,000/year” as reference, with an additional indicator of missing income). In models containing neighborhood SES, it is important to control for individual SES as it is a likely confounder of any observed associations between neighborhood SES and behavior (Karriker-Jaffe et al., 2012); neighborhood and individual SES also have independent effects on health (Robert, 1999). Multivariate models also included indicators of urbanicity (more than 90% of tract residents living in an urban area or urbanized cluster), geocoding precision (whether geocode was based on ZIP code match or street address) and survey year.
In addition to these demographic controls, additional variables that might confound or mediate relationships between neighborhood SES and outcomes were included in final multivariate models. These included sense of coherence, measured with a 4-item scale indicating a positive outlook and orientation to the world as a manageable and meaningful place (Eriksson and Lindström, 2005), and which has protective effects on mortality (Wainwright et al., 2008) and substance use and related problems (Midanik and Zabkiewicz, 2009; Wainwright et al., 2008); current levels of distress, measured with an 8-item scale based on the Center for Epidemiologic Studies’ Depression Scale (Radloff, 1977; Roberts, 1980), and which is associated with past-year substance use (Boardman et al., 2001; Graham et al., 2007; McGue et al., 1997; Mulia et al., 2008; Palfai et al., 2007; Stasiewicz and Maisto, 1993); family history of alcohol problems and heavy drinking in teens, to represent biological and behavioral propensity for substance use (Dawson et al., 2008, 1992; Prescott and Kendler, 1999); and region of residence, to indicate cultural norms around drinking as defined by Kerr (2010).
2.3. Data analysis
Associations between neighborhood SES (both disadvantage and affluence) and substance use were examined using gender-stratified unadjusted and adjusted logistic regression models. Adjusted models progressed from basic demographic controls to the larger set of possible confounding and mediating variables. Overall contribution of neighborhood SES to each model was assessed using an omnibus F-test (design-adjusted Wald test). Multivariate models for alcohol outcomes were repeated for past-year drinkers (n=9,971). Fully-adjusted moderation models assessed interactions between neighborhood SES (both disadvantage and affluence) with age using a dichotomous indicator (under age 40 vs. age 40 and over). Analyses were conducted using Stata (Stata Corp., 2009) to accommodate weights adjusting for sampling and non-response. Survey year was used as the weighting stratum in order to approximate the age, sex and race/ethnicity distributions of the U.S. population at the time each survey was conducted. Weights were normalized to each survey’s sample size; respondents thus were weighted to represent the average person during the respective year of data collection. Preliminary analyses suggested associations between neighborhood SES and outcomes did not vary by survey year (data available upon request).
2.4. Human subjects protection
The current secondary data analysis was reviewed by the Institutional Review Boards of the Public Health Institute, Oakland, CA, and the University of California, Berkeley, and found to be exempt because no personally-identifying data were used.
3. RESULTS
3.1. Descriptive statistics
Respondents living in the sample’s three types of neighborhoods showed important demographic differences. Compared to residents of the middle-class neighborhoods, respondents in disadvantaged neighborhoods were significantly more likely to be under 40 years of age (46.2% disadvantaged vs. 39.5% middle-class vs. 38.6% affluent neighborhoods, F(1.98, 28573)=18.20, p<0.01), less likely to be living with a partner or spouse (53.8% disadvantaged vs. 66.8% middle-class vs. 67.0% affluent neighborhoods, F(1.99, 28699)=71.43, p<0.01), less likely to be white (48.4% disadvantaged vs. 79.1% middle-class vs. 80.7% affluent neighborhoods, F(5.44, 78315)=193.11, p<0.01), more likely to have dropped out of high school (23.1% disadvantaged vs. 10.9% middle-class vs. 5.2% affluent neighborhoods, F(5.95, 85233)=159.28, p<0.01), and less likely to be employed (61.2% disadvantaged vs. 67.9% middle-class vs. 70.2% affluent neighborhoods, F(3.90, 55937)=17.49, p<0.01).
Differences between men and women in prevalence of daily tobacco use, drinking within guidelines, monthly drunkenness and regular marijuana use were statistically significant (Table 1). Men reported higher rates of most outcomes, with the exception of drinking within recommended guidelines, which was more prevalent among women.
3.2. Bivariate models
Bivariate models showed neighborhood SES was significantly associated with daily tobacco use (F(2, 14429)=26.36, p<0.01), drinking within guidelines (F(2, 14447)=8.85, p<0.01), and regular marijuana use (F(2, 14434)=3.36, p<0.05) for men, and with daily tobacco use (F(2, 14415)=17.12, p<0.01), drinking within guidelines (F(2, 14387)=15.77, p<0.01), regular marijuana use (F(2, 14436)=3.77, p<0.05) and regular other drug use (F(2, 14461)=8.79, p<0.01) for women. Residence in disadvantaged (vs. middle-class) neighborhoods was associated with significantly higher odds of daily tobacco use, drinking within guidelines and regular marijuana use for men (Table 2), as well as with marginally higher odds of daily tobacco use and significantly higher odds of drinking within guidelines and regular other drug use for women (Table 3). Residence in affluent (vs. middle-class) neighborhoods was associated with significantly lower odds of daily tobacco use, drinking within guidelines and regular other drug use (marginally significant) for men, as well as with lower odds of daily tobacco use, drinking within guidelines, regular marijuana use and regular other drug use (marginally significant) for women.
Table 2.
Relationship between neighborhood socioeconomic status and substance use outcomes among U.S. men
| Daily tobacco use | Drinking within guidelines | Monthly drunkenness | Monthly marijuana use | Monthly other drug use | |
|---|---|---|---|---|---|
| Bivariate models | OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) |
|
| |||||
| Neighborhood SES a | |||||
| Disadvantaged | 1.19 (1.02, 1.38)* | 1.20(1.04, 1.39)* | 0.89 (0.71, 1.11) | 1.49 (1.10, 2.02)** | 0.98 (0.67, 1.43) |
| Affluent | 0.60 (0.50, 0.71)** | 0.83 (0.72, 0.97)* | 1.06 (0.84, 1.33) | 1.12 (0.80, 1.57) | 0.67 (0.44, 1.04)† |
|
| |||||
| Multivariate models b | OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) |
|
| |||||
| Married/partnered | 0.95 (0.81, 1.11) | 1.37 (1.18, 1.59)** | 0.54 (0.44, 0.68)** | 0.75 (0.55, 1.01) † | 0.75 (0.52, 1.08) |
| Age c | |||||
| 18–29 years | 3.23 (2.45, 4.27)** | 0.11 (0.08, 0.15)** | 22.39 (12.29, 40.79)** | 24.56 (10.35, 58.28)** | 1.93 (1.02, 3.67)* |
| 30–39 years | 3.26 (2.46, 4.30)** | 0.16 (0.12, 0.22)** | 10.11 (5.47, 18.66)** | 17.34 (7.12, 42.24)** | 1.08 (0.52, 2.23) |
| 40–49 years | 3.31 (2.52, 4.34)** | 0.29 (0.21, 0.39)** | 7.29 (3.93, 13.51)** | 11.28 (4.66, 27.29)** | 1.62 (0.83, 3.16) |
| 50–59 years | 2.54 (1.93, 3.35)** | 0.46 (0.34, 0.63)** | 3.67 (1.91, 7.04)** | 7.09 (2.83, 17.72)** | 1.66 (0.88, 3.13) |
| Race/ethnicity d | |||||
| African American | 0.56 (0.45, 0.69)** | 2.52 (1.99, 3.19)** | 0.61 (0.43, 0.85)** | 1.15 (0.77, 1.73) | 1.42 (0.85, 2.37) |
| Hispanic/Latino | 0.42 (0.34, 0.53)** | 1.13 (0.93, 1.37) | 0.73 (0.55, 0.97)* | 0.63 (0.40, 1.00) † | 0.71 (0.43, 1.18) |
| Other race/ethnicity | 1.08 (0.80, 1.46) | 1.97 (1.40, 2.76)** | 0.70 (0.43, 1.14) | 1.51 (0.91, 2.52) | 1.43 (0.77, 2.67) |
| Education e | |||||
| Less than high school | 3.01 (2.36, 3.85)** | 1.12 (0.87, 1.43) | 0.98 (0.68, 1.41) | 2.16 (1.32, 3.52)** | 2.18 (1.22, 3.90)** |
| High school graduate | 3.44 (2.01, 2.96)** | 0.94 (0.78, 1.13) | 0.85 (0.64, 1.12) | 1.73 (1.14, 2.62)** | 2.01 (1.21, 3.33)** |
| Some college | 2.21 (1.81, 2.68)** | 0.77 (0.64, 0.92)** | 1.19 (0.92, 1.56) | 1.65 (1.12, 2.44)** | 1.58 (0.94, 2.64) † |
| Employment status f | |||||
| Unemployed | 1.15 (0.84, 1.57) | 0.98 (0.70, 1.39) | 1.00 (0.63, 1.60) | 2.33 (1.50, 3.64)** | 1.51 (0.76, 3.00) |
| Not in workforce | 1.23 (1.00, 1.52) † | 1.27 (1.00, 1.60)* | 0.88 (0.63, 1.23) | 2.00 (1.37, 2.93)** | 1.91 (1.18, 3.08)** |
| Income g | |||||
| < $10,000 | 1.30 (0.94, 1.79) | 1.42 (1.03, 1.95)* | 1.05 (0.68, 1.63) | 1.33 (0.76, 2.33) | 1.68 (0.85, 3.33) |
| $10,001–20,000 | 1.37 (1.03, 1.83)* | 1.81 (1.36, 2.40)** | 1.08 (0.71, 1.64) | 1.61 (0.92, 2.81) † | 1.55 (0.81, 2.99) |
| $20,001–40,000 | 1.48 (1.17, 1.89)** | 1.31 (1.05, 1.63)* | 1.01 (0.72, 1.41) | 1.03 (0.63, 1.68) | 1.30 (0.71, 2.38) |
| $40,001–60,000 | 1.31 (1.02, 1.68)* | 1.08 (0.86, 1.36) | 1.11 (0.78, 1.57) | 1.14 (0.69, 1.88) | 0.93 (0.49, 1.78) |
| $60,001–80,000 | 1.14 (0.87, 1.49) | 1.14 (0.90, 1.44) | 0.95 (0.65, 1.38) | 0.91 (0.52, 1.60) | 1.33 (0.65, 2.70) |
| Missing income | 1.10 (0.82, 1.48) | 1.63 (1.21, 2.18)** | 0.55 (0.35, 0.88)* | 1.28 (0.72, 2.26) | 0.92 (0.41, 2.05) |
| Urban neighborhood | 0.94 (0.81, 1.09) | 0.96 (0.83, 1.12) | 1.09 (0.87, 1.37) | 1.37 (1.00, 1.89)* | 1.04 (0.72, 1.51) |
| Neighborhood SES a | |||||
| Disadvantaged | 1.26 (1.06, 1.49)** | 1.16 (0.98, 1.38) † | 0.81 (0.64, 1.04) | 1.10 (0.78, 1.54) | 0.75 (0.49, 1.15) |
| Affluent | 0.81 (0.67, 0.98)* | 0.86 (0.72, 1.02) † | 1.06 (0.81, 1.37) | 1.25 (0.88, 1.78) | 0.81 (0.51, 1.27) |
| Obs (Wtd. N) | 6,487 (6,773) | 6,505 (6,788) | 6,427 (6,756) | 6,492 (6,770) | 6,526 (6,805) |
OR, odds ratio. CI, confidence interval. Obs, number of observations. Wtd. N, weighted sample size.
Middle-class neighborhood is reference.
Models also controlled for survey year and precision of geocode.
60 and older is reference.
White is reference.
College graduate is reference.
Employed is reference.
Over $80,000 is reference.
p < .10
p<.05.
p<.01
Table 3.
Relationship between neighborhood socioeconomic status and substance use outcomes among U.S. women
| Daily tobacco use | Drinking within guidelines | Monthly drunkenness | Monthly marijuana use | Monthly other drug use | |
|---|---|---|---|---|---|
| Bivariate models | OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) |
|
| |||||
| Neighborhood SES a | |||||
| Disadvantaged | 1.16 (0.99, 1.35)† | 1.34 (1.12, 1.59)** | 0.88 (0.61, 1.27) | 0.91 (0.60, 1.38) | 1.61 (1.14, 2.26)** |
| Affluent | 0.63 (0.51, 0.76)** | 0.76 (0.64, 0.90)** | 0.89 (0.59, 1.34) | 0.40 (0.21, 0.78)** | 0.68 (0.43, 1.06)† |
|
| |||||
| Multivariate models b | OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) |
|
| |||||
| Married/partnered | 0.74 (0.63, 0.88)** | 1.33 (1.13, 1.58)** | 0.42 (0.29, 0.60)** | 0.71 (0.45, 1.12) | 0.70 (0.49, 1.01) † |
| Age c | |||||
| 18–29 years | 2.60 (2.00, 3.40)** | 0.15 (0.11, 0.20)** | 64.74 (24.52, 170.93)** | 184.06 (24.15, 1403.06)** | 2.15 (1.26, 3.66)** |
| 30–39 years | 3.42 (2.60, 4.51)** | 0.25 (0.19, 0.34)** | 17.74 (6.36, 49.48)** | 73.71 (9.44, 575.79)** | 1.47 (0.78, 2.77) |
| 40–49 years | 2.90 (2.23, 3.78)** | 0.40 (0.30, 0.54)** | 22.70 (8.44, 61.02)** | 64.80 (8.23, 509.99)** | 1.54 (0.84, 2.83) |
| 50–59 years | 2.69 (2.07, 3.50)** | 0.69 (0.51, 0.97)* | 7.29 (2.52, 21.08)** | 34.81 (4.26, 284.33)** | 2.33 (1.36, 3.98)** |
| Race/ethnicity d | |||||
| African American | 0.49 (0.40, 0.61)** | 3.17 (2.50, 4.02)** | 0.56 (0.35, 0.90)* | 0.57 (0.34, 0.93)* | 0.95 (0.61, 1.49) |
| Hispanic/Latino | 0.29 (0.21, 0.39)** | 1.78 (1.39, 2.29)** | 0.34 (0.20, 0.58)** | 0.37 (0.21, 0.67)** | 0.62 (0.30, 1.29) |
| Other race/ethnicity | 0.72 (0.50, 1.05) † | 2.05 (1.27, 3.31)** | 0.47 (0.21, 1.03) † | 1.36 (0.57, 3.23) | 1.07 (0.54, 2.10) |
| Education e | |||||
| Less than high school | 3.51 (2.65, 4.63)** | 1.92 (1.40, 2.64)** | 1.54 (0.88, 2.70) | 2.34 (1.18, 4.64)* | 1.64 (0.93, 2.87) † |
| High school graduate | 2.66 (2.12, 3.33)** | 1.34 (1.09, 1.66)** | 0.77 (0.48, 1.22) | 0.86 (0.45, 1.64) | 1.03 (0.64, 1.67) |
| Some college | 2.37 (1.91, 2.95)** | 0.93 (0.76, 1.13) | 1.22 (0.74, 1.72) | 1.72 (0.93, 3.17) † | 1.75 (1.09, 2.79)* |
| Employment status f | |||||
| Unemployed | 1.36 (0.97, 1.90) † | 1.28 (0.81, 2.01) | 1.05 (0.51, 2.16) | 1.39 (0.69, 2.81) | 0.41 (0.18, 0.94)* |
| Not in workforce | 0.96 (0.81, 1.15) | 1.49 (1.23, 1.81)** | 0.78 (0.49, 1.24) | 0.85 (0.51, 1.42) | 1.45 (0.99, 2.11) † |
| Income g | |||||
| < $10,000 | 1.39 (0.97, 2.00) † | 1.45 (1.01, 2.08)* | 0.99 (0.47, 2.06) | 5.47 (1.38, 21.76)* | 0.90 (0.37, 2.22) |
| $10,001–20,000 | 1.44 (1.01, 2.05)* | 1.53 (1.10, 2.13)* | 1.14 (0.58, 2.24) | 5.12 (1.30, 20.06)* | 0.90 (0.38, 2.13) |
| $20,001–40,000 | 1.57 (1.14, 2.17)** | 1.57 (1.19, 2.08)** | 0.60 (0.32, 1.13) | 3.56 (0.96, 13.16) † | 0.78 (0.34, 1.76) |
| $40,001–60,000 | 1.14 (0.81, 1.59) | 1.50 (1.12, 2.00)** | 0.90 (0.49, 1.67) | 2.96 (0.74, 11.88) | 1.24 (0.55, 2.81) |
| $60,001–80,000 | 0.82 (0.56, 1.20) | 1.29 (0.95, 1.75) | 0.84 (0.40, 1.78) | 4.12 (1.06, 16.07)* | 0.71 (0.29, 1.75) |
| Missing income | 0.88 (0.62, 1.26) | 2.02 (1.44, 2.81)** | 0.61 (0.28, 1.77) | 1.66 (0.40, 6.87) | 0.53 (0.23, 1.26) |
| Urban neighborhood | 0.93 (0.79, 1.09) | 0.86 (0.73, 1.03) † | 0.98 (0.68, 1.40) | 1.03 (0.63, 1.69) | 0.96 (0.66, 1.39) |
| Neighborhood SES a | |||||
| Disadvantaged | 1.24 (1.03, 1.47)* | 1.07 (0.89, 1.31) | 0.77 (0.51, 1.19) | 0.74 (0.48, 1.15) | 1.54 (1.05, 2.26)* |
| Affluent | 0.81 (0.65, 1.00)* | 0.89 (0.73, 1.09) | 0.80 (0.51, 1.27) | 0.43 (0.21, 0.89)* | 0.66 (0.38, 1.14) |
| Obs (Wtd. N) | 7,477 (7,258) | 7,451 (7,242) | 7,406 (7,190) | 7,497 (7,263) | 7,522 (7,301) |
OR, odds ratio. CI, confidence interval. Obs, number of observations. Wtd. N, weighted sample size.
Middle-class neighborhood is reference.
Models also controlled for survey year and precision of geocode.
60 and older is reference.
White is reference.
College graduate is reference.
Employed is reference.
Over $80,000 is reference.
p < .10
p < .05.
p < .01
3.3. Multivariate models
Some associations were attenuated upon adjustment for individual-level control variables (Tables 2 and 3). In multivariate models, neighborhood SES remained significantly associated with daily tobacco use (F(2, 14306)=7.90, p<0.01) and drinking within guidelines (F(2, 14324)=4.15, p<0.05) for men, and with daily tobacco use (F(2, 14183)=6.25, p<0.01), regular marijuana use (F(2, 14203)=2.92, p=0.05) and regular other drug use (F(2, 14228)=5.64, p<0.01) for women. For men, residence in disadvantaged (vs. middle-class) neighborhoods was associated with higher odds of tobacco use and drinking within recommended guidelines (marginally significant). For women, neighborhood disadvantage was associated with higher odds of both tobacco and other drug use. Residence in affluent (vs. middle-class) neighborhoods was associated with significantly lower odds of tobacco use and drinking within recommended guidelines (marginally significant) for men and with lower odds of both tobacco and marijuana use for women.
When the male sample was limited to past-year drinkers (full models not shown), there were no significant associations between neighborhood SES with either drinking within recommended guidelines (F(2, 14396)=0.56, p>0.10) or monthly drunkenness (F(2, 14385)=0.86, p>0.10). For past-year female drinkers, there also were no significant associations of neighborhood SES with either drinking within recommended guidelines (F(2, 14325)=0.44, p>0.10) or monthly drunkenness (F(2, 14332)=0.39, p>0.10).
Further adjustment for additional confounders or possible mediators of effects of neighborhood SES on outcomes did not substantively change the pattern of findings (Tables 4 and 5). Significant associations remained for neighborhood SES with men’s tobacco use (F(2, 14009)=8.11, p<0.01) and with women’s tobacco use (F(2, 13845)=5.35, p<0.01), marijuana use (F(2, 13863)=3.41, p<0.05) and other drug use (F(2, 13811)=3.61, p<0.05). Neighborhood disadvantage increased odds of men’s tobacco use, women’s tobacco use, and women’s other drug use (marginally so). Neighborhood affluence decreased odds of men’s tobacco use and women’s marijuana use. The protective effect of neighborhood affluence on women’s tobacco use was reduced to non-significance in the further-adjusted models, although the odds ratios for the multivariate models were similar in magnitude.
Table 4.
Relationship between neighborhood socioeconomic status and substance use outcomes among U.S. men further adjusted for additional confounders and possible mediatorsa
| Daily tobacco use | Drinking within guidelines | Monthly drunkenness | Monthly marijuana use | Monthly other drug use | |
|---|---|---|---|---|---|
| Married/partnered | 0.96 (0.82, 1.14) | 1.33 (1.13, 1.57)** | 0.54 (0.43, 0.69)** | 0.76 (0.56, 1.03) † | 0.88 (0.60, 1.28) |
| Age b | |||||
| 18–29 years | 2.87 (2.14, 3.86)** | 0.11 (0.08, 0.15)** | 17.25 (9.40, 31.67)** | 19.63 (7.93, 48.60)** | 1.32 (0.66, 2.65) |
| 30–39 years | 2.87 (2.14, 3.86)** | 0.18 (0.13, 0.24)** | 7.04 (3.78, 13.12)** | 13.34 (5.20, 34.18)** | 0.74 (0.34, 1.60) |
| 40–49 years | 3.00 (2.25, 4.00)** | 0.33 (0.24, 0.46)** | 5.04 (2.71, 9.35)** | 7.83 (3.08, 19.92)** | 1.06 (0.53, 2.10) |
| 50–59 years | 2.31 (1.73, 3.10)** | 0.53 (0.38, 0.74)** | 2.80 (1.43, 5.48)** | 5.92 (2.23, 15.76)** | 1.22 (0.61, 2.44) |
| Race/ethnicity c | |||||
| African American | 0.59 (0.48, 0.74)** | 2.12 (1.65, 2.73)** | 0.83 (0.58, 1.18) | 1.53 (1.00, 2.35) † | 1.65 (0.97, 2.81) † |
| Hispanic/Latino | 0.43 (0.34, 0.55)** | 1.05 (0.85, 1.29) | 0.77 (0.56, 1.05) † | 0.60 (0.37, 0.99)* | 0.67 (0.40, 1.14) |
| Other race/ethnicity | 1.11 (0.81, 1.52) | 1.93 (1.34, 2.76)** | 0.72 (0.46, 1.14) | 1.36 (0.81, 2.29) | 1.30 (0.67, 2.53) |
| Education d | |||||
| Less than high school | 2.77 (2.15, 3.58)** | 1.44 (1.11, 1.87)* | 0.76 (0.51, 1.14) | 1.69 (1.02, 2.81)* | 2.06 (1.13, 3.76)* |
| High school graduate | 2.31 (1.88, 2.82)** | 1.09 (0.89, 1.33) | 0.67 (0.50, 0.91)* | 1.52 (0.98, 2.37) † | 1.93 (1.12, 3.33)* |
| Some college | 2.07 (1.69, 2.53)** | 0.89 (0.73, 1.08) | 0.99 (0.74, 1.30) | 1.41 (0.94, 2.12) | 1.63 (0.95, 2.79) † |
| Employment status e | |||||
| Unemployed | 1.07 (0.77, 1.50) | 1.05 (0.74, 1.49) | 0.81 (0.48, 1.37) | 2.15 (1.37, 3.38)** | 1.08 (0.54, 2.16) |
| Not in workforce | 1.23 (0.99, 1.53) † | 1.37 (1.08, 1.73)* | 0.82 (0.59, 1.15) | 2.00 (1.35, 2.97)** | 1.72 (1.03, 2.87)* |
| Income f | |||||
| < $10,000 | 1.39 (1.00, 1.94) † | 1.24 (0.89, 1.74) | 1.18 (0.74, 1.88) | 1.34 (0.75, 2.42) | 1.29 (0.62, 2.68) |
| $10,001–20,000 | 1.38 (1.03, 1.86)* | 1.80 (1.33, 2.43)** | 1.05 (0.68, 1.63) | 1.50 (0.85, 2.63) | 1.19 (0.60, 2.38) |
| $20,001–40,000 | 1.55 (1.21, 1.99)** | 1.24 (0.98, 1.57) † | 1.07 (0.75, 1.53) | 1.04 (0.62, 1.72) | 1.13 (0.60, 2.13) |
| $40,001–60,000 | 1.39 (1.08, 1.80)** | 1.10 (0.86, 1.40) | 1.14 (0.78, 1.66) | 1.01 (0.59, 1.73) | 0.80 (0.41, 1.57) |
| $60,001–80,000 | 1.17 (0.89, 1.55) | 1.11 (0.86, 1.43) | 0.98 (0.65, 1.46) | 0.95 (0.53, 1.72) | 1.22 (0.58, 2.56) |
| Missing income | 1.23 (0.91, 1.68) | 1.37 (1.00, 1.88) † | 0.65 (0.40, 1.07) † | 1.56 (0.86, 2.83) | 0.89 (0.38, 2.05) |
| Sense of coherence | 1.00 (0.90, 1.11) | 0.95 (0.85, 1.07) | 0.85 (0.72, 1.00)* | 0.93 (0.76, 1.14) | 0.83 (0.65, 1.06) |
| Depression | 1.10 (1.00, 1.21) † | 0.91 (0.83, 1.00)* | 1.16 (1.01, 1.33)* | 1.29 (1.05, 1.58)* | 1.79 (1.39, 2.31)** |
| Family history of alcohol problems | 1.24 (1.08, 1.43)** | 0.78 (0.68, 0.90)** | 1.19 (0.96, 1.47) | 1.72 (1.28, 2.31)** | 1.89 (1.30, 2.75)** |
| Heavy drinking in teens | 1.88 (1.63, 2.17)** | 0.28 (0.24, 0.33)** | 4.15 (3.32, 5.19)** | 3.38 (2.53, 4.51)** | 2.12 (1.47, 3.07)** |
| Urban neighborhood | 0.98 (0.83, 1.14) | 1.00 (0.85, 1.17) | 1.02 (0.80, 1.30) | 1.43 (1.02, 1.99)* | 1.12 (0.75, 1.69) |
| Neighborhood SES g | |||||
| Disadvantaged | 1.27 (1.06, 1.51)** | 1.16 (0.97, 1.39) | 0.84 (0.65, 1.09) | 1.05 (0.74, 1.50) | 0.68 (0.44, 1.04) † |
| Affluent | 0.79 (0.65, 0.97)* | 0.91 (0.75, 1.09) | 1.09 (0.83, 1.44) | 1.25 (0.87, 1.79) | 0.88 (0.55, 1.40) |
| Obs (Wtd. N) | 6,190 (6,464) | 6,198 (6,470) | 6,189 (6,462) | 6,194 (6,462) | 6,526 (6,805) |
OR, odds ratio. CI, confidence interval. Obs, number of observations. Wtd. N, weighted sample size.
Models also controlled for survey year, precision of geocode and region of country.
60 and older is reference.
White is reference.
College graduate is reference.
Employed is reference.
Over $80,000 is reference.
Middle-class neighborhood is reference.
p<.10
p<.05.
p<.01
Table 5.
Relationship between neighborhood socioeconomic status and substance use outcomes among U.S. women further adjusted for additional confounders and possible mediatorsa
| Daily tobacco use | Drinking within guidelines | Monthly drunkenness | Monthly marijuana use | Monthly other drug use | |
|---|---|---|---|---|---|
| Married/partnered | 0.78 (0.66, 0.92)** | 1.36 (1.14, 1.63)** | 0.40 (0.27, 0.59)** | 0.74 (0.45, 1.22) | 0.76 (0.53, 1.10) |
| Age b | |||||
| 18–29 years | 1.97 (1.49, 2.63)** | 0.21 (0.15, 0.28)** | 41.61 (14.85, 116.61)** | 91.98 (11.91, 710.13)** | 1.57 (0.91, 2.71) |
| 30–39 years | 2.55 (1.90, 3.43)** | 0.40 (0.29, 0.55)** | 10.55 (3.57, 31.14)** | 33.74 (4.30, 264.93)** | 1.15 (0.61, 2.18) |
| 40–49 years | 2.12 (1.60, 2.81)** | 0.60 (0.44, 0.83)** | 13.18 (4.61, 37.72)** | 31.74 (3.87, 260.13)** | 1.04 (0.54, 2.01) |
| 50–59 years | 2.37 (1.80, 3.12)** | 0.91 (0.65, 1.26) | 5.63 (1.81, 17.49)** | 20.31 (2.42, 170.58)** | 1.90 (1.09, 3.31)* |
| Race/ethnicity c | |||||
| African American | 0.55 (0.44, 0.68)** | 2.42 (1.89, 3.11)** | 0.72 (0.43, 1.19) | 0.79 (0.45, 1.37) | 1.06 (0.67, 1.68) |
| Hispanic/Latino | 0.35 (0.25, 0.48)** | 1.53 (1.17, 2.01)** | 0.51 (0.30, 0.88)* | 0.47 (0.24, 0.90)* | 0.62 (0.30, 1.27) |
| Other race/ethnicity | 0.75 (0.51, 1.10) | 1.86 (1.16, 3.00)** | 0.48 (0.21, 1.11) † | 1.28 (0.52, 3.12) | 0.89 (0.43, 1.87) |
| Education d | |||||
| Less than high school | 3.37 (2.52, 4.51)** | 1.88 (1.36, 2.61)** | 1.32 (0.71, 2.46) | 2.05 (0.93, 4.48) † | 1.47 (0.83, 2.63) |
| High school graduate | 2.56 (2.02, 3.24)** | 1.39 (1.11, 1.75)** | 0.76 (0.48, 1.22) | 0.73 (0.35, 1.50) | 0.97 (0.60, 1.58) |
| Some college | 2.30 (1.84, 2.88)** | 0.94 (0.76, 1.16) | 1.10 (0.70, 1.73) | 1.54 (0.80, 3.00) | 1.63 (1.00, 2.64) † |
| Employment status e | |||||
| Unemployed | 1.25 (0.87, 1.79) | 1.45 (0.90, 2.33) | 0.74 (0.33, 1.66) | 1.39 (0.64, 2.99) | 0.39 (0.16, 0.92)* |
| Not in workforce | 0.94 (0.78, 1.14) | 1.58 (1.28, 1.94)** | 0.75 (0.46, 1.21) | 0.77 (0.44, 1.34) | 1.32 (0.89, 1.96) |
| Income f | |||||
| < $10,000 | 1.22 (0.83, 1.80) | 1.61 (1.11, 2.33)* | 0.77 (0.36, 1.63) | 3.68 (0.93, 14.64) † | 0.71 (0.28, 1.79) |
| $10,001–20,000 | 1.33 (0.91, 1.94) | 1.58 (1.12, 2.23)* | 1.01 (0.49, 2.08) | 3.60 (0.87, 14.89) † | 0.75 (0.31, 1.82) |
| $20,001–40,000 | 1.53 (1.09, 2.15)* | 1.65 (1.23, 2.22)** | 0.55 (0.28, 1.06) † | 2.92 (0.76, 11.15) | 0.73 (0.32, 1.66) |
| $40,001–60,000 | 1.14 (0.80, 1.63) | 1.56 (1.13, 2.14)* | 0.84 (0.45, 1.59) | 1.97 (0.40, 9.62) | 1.28 (0.55, 2.94) |
| $60,001–80,000 | 0.76 (0.51, 1.15) | 1.40 (1.00, 1.95) † | 0.76 (0.34, 1.67) | 2.76 (0.70, 10.94) | 0.74 (0.30, 1.83) |
| Missing income | 0.93 (0.64, 1.36) | 1.88 (1.32, 2.67)** | 0.55 (0.24, 1.28) | 1.34 (0.32, 5.70) | 0.50 (0.21, 1.21) |
| Sense of coherence | 0.83 (0.74, 0.93)** | 0.99 (0.87, 1.13) | 0.82 (0.63, 1.06) | 0.77 (0.56, 1.06) † | 0.69 (0.54, 0.88)** |
| Depression | 1.14 (1.02, 1.27)* | 1.05 (0.95, 1.17) | 1.06 (0.84, 1.33) | 1.21 (0.89, 1.64) | 1.24 (0.94, 1.63) |
| Family history of alcohol problems | 1.63 (1.39, 1.91)** | 0.77 (0.65, 0.91)** | 1.27 (0.88, 1.82) | 1.47 (0.83, 2.59) | 1.13 (0.79, 1.60) |
| Heavy drinking in teens | 2.20 (1.81, 2.66)** | 0.23 (0.19, 0.28)** | 3.57 (2.50, 5.11)** | 3.67 (2.34, 5.77)** | 1.33 (0.85, 2.09) |
| Urban neighborhood | 0.95 (0.81, 1.13) | 0.88 (0.73, 1.06) | 1.05 (0.70, 1.56) | 1.07 (0.64, 1.77) | 1.01 (0.69, 1.48) |
| Neighborhood SES g | |||||
| Disadvantaged | 1.26 (1.04, 1.52)* | 1.01 (0.81, 1.25) | 0.75 (0.47, 1.17) | 0.69 (0.44, 1.08) | 1.42 (0.95, 2.11) † |
| Affluent | 0.83 (0.66, 1.05) | 0.87 (0.70, 1.07) | 0.87 (0.54, 1.41) | 0.37 (0.16, 0.85)* | 0.69 (0.39, 1.21) |
| Obs (Wtd. N) | 7,139 (6,900) | 7,112 (6,883) | 7,112 (6,878) | 7,137 (6,904) | 7,171 (6,927) |
OR, odds ratio. CI, confidence interval. Obs, number of observations. Wtd. N, weighted sample size.
Models also controlled for survey year, precision of geocode and region of country.
60 and older is reference.
White is reference.
College graduate is reference.
Employed is reference.
Over $80,000 is reference.
Middle-class neighborhood is reference.
p<.10
p<.05.
p<.01
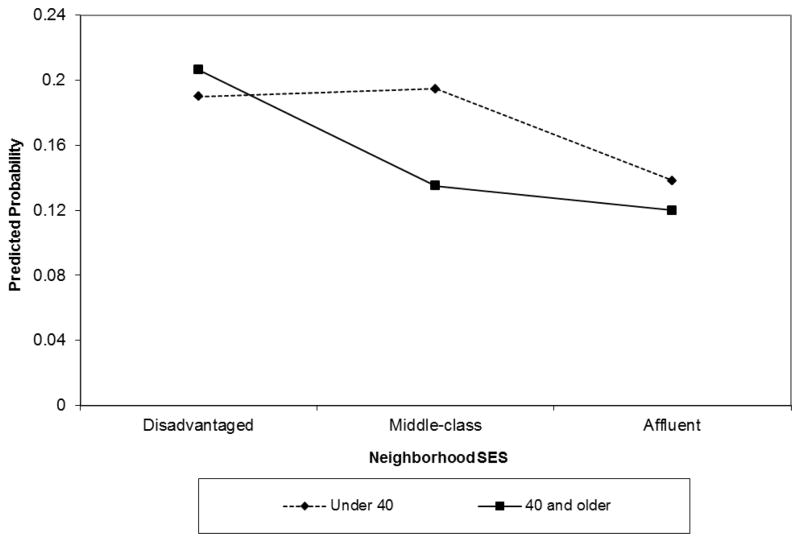
3.4. Modification by age
Omnibus F-tests from a second set of fully-adjusted models (not shown) identified a significant interaction of neighborhood SES with age for men’s tobacco use (F(2, 14371)=5.79, p<0.01). There was an elevated risk of tobacco use for younger men (under age 40) in both disadvantaged and middle-class neighborhoods and for older men (ages 40 and older) only in disadvantaged neighborhoods (Figure 1).
Figure 1.
Interaction of Neighborhood SES and Age for Men’s Daily Tobacco Use
In the full sample, there also was a significant interaction of neighborhood SES with age for women’s drinking within recommended guidelines (F(2, 13973)=3.23, p<0.05), which reflected reduced probability of drinking within guidelines for older women in affluent neighborhoods, as well as slightly increased probability of drinking within guidelines for younger women in affluent neighborhoods. The interaction was not significant when limited to past-year female drinkers (F(2, 14156)=1.15, p>0.10).
4. DISCUSSION
The hypotheses were partially supported, with more evidence compatible with the disadvantage hypothesis than the affluence hypothesis. Specifically, compared to middle-class neighborhoods, residence in disadvantaged neighborhoods was positively associated with one of the stress-related behaviors (daily tobacco use by both men and women) and with one of the more risky substance use outcomes (regular use of other drugs by women). There were no significant associations of neighborhood disadvantage with either monthly drunkenness or regular marijuana use for men or women, however. As hypothesized, residence in affluent neighborhoods was negatively associated with substance use patterns incompatible with more conventional norms and a health culture (particularly less daily tobacco use, but also less regular marijuana use by women). However, the hypothesized associations of neighborhood affluence with the alcohol outcomes were not significant for either the full sample or the sub-sample of past-year drinkers. Additionally, other than robust results for tobacco, findings varied by gender, with associations between disadvantage and higher odds of other drug use and between affluence and reduced odds of regular marijuana use emerging only for women. The association between neighborhood SES and tobacco use for men was further modified by age, with protective effects of residence in middle-class neighborhoods only evident for older adults.
With some exceptions (see, for example, Diez Roux et al., 2003), most studies of neighborhood SES and tobacco use have focused on disadvantage, without considering effects of concentrated affluence. The gradient effect of neighborhood SES on tobacco outcomes observed in the current data thus extends findings from other studies using localized samples of adults in the U.S. (Ross, 2000; Tseng et al., 2001) and other countries (Duncan et al., 1999; Shohaimi et al., 2003), which have documented an association between neighborhood disadvantage and increased smoking. Increased tobacco use in disadvantaged neighborhoods may be partially due to the density of tobacco outlets (Henriksen et al., 2008), which may contribute to social norms supporting tobacco use and promote tobacco as a relatively low-cost stress-reduction strategy. As in a study of young adults in four U.S. cities (Diez Roux et al., 2003), in these national data, residence in affluent neighborhoods was associated with a further reduction in daily tobacco use above that observed in middle-class (vs. disadvantaged) neighborhoods. Examination of mediators of effects of both neighborhood affluence and disadvantage on tobacco use would help confirm hypothesized differences in norms supporting healthy lifestyles. The moderation effect for men uncovered differential relationships between neighborhood SES and tobacco use by age, and other studies suggest neighborhood effects on smoking vary by race/ethnicity (Diez Roux et al., 2003; Kandula et al., 2009; Nowlin and Colder, 2007; Tseng et al., 2001). Future studies should examine which groups are at increased risk in disadvantaged and middle-class neighborhoods and identify protective factors that could be targets of intervention.
In this national sample there was a protective effect of neighborhood affluence on reduced marijuana use by women, but there was no association between neighborhood disadvantage and marijuana use for either men or women in adjusted models. This is counter to findings from a New York City sample (Galea et al., 2007a, 2007b), and it suggests that their reported positive associations between neighborhood affluence and recent marijuana use could be unique to large urban areas. Along those lines, the current multivariate models showed neighborhood urbanicity was significantly associated with increased marijuana use by men, but not by women. Although only statistically significant for women in multivariate models, the direction of associations of neighborhood SES with regular marijuana use differed for men and women. Additional investigations could provide valuable insight into social norms and attitudes toward marijuana use that may differ by gender and neighborhood SES, and also by urbanicity. These norms also may vary by region, as marijuana use was reported significantly more often by men in New England and the Pacific (compared to the Dry South; data available on request).
These data also produced somewhat unexpected results for regular use of drugs other than marijuana. There was a significant association between neighborhood disadvantage and other drug use for women. In contrast to findings from prior studies using local U.S. samples (Boardman et al., 2001; Williams and Latkin, 2007), in this national dataset, there was no significant relationship between neighborhood SES and regular non-marijuana drug use for men. There may be a “downward drift” of heavy substance users into disadvantaged neighborhoods over time (Buu et al., 2007) that could contribute to these findings, but it is not clear why this effect would be more pronounced for women than men. As documented in the fully-adjusted models, the increased odds of other drug use by women in disadvantaged neighborhoods was only slightly reduced after controlling for indicators of early substance use and genetic vulnerability to substance use, each of which may contribute to neighborhood selection as an adult. Replication of these results in other datasets would be informative.
Overall, there were no notable effects of neighborhood SES on the drinking outcomes. For both men and women, the strongest correlates of monthly drunkenness were age (inverse association) and heavy drinking as a teenager. One hypothesis was that stress-related behaviors, including frequent drunkenness, would be associated with neighborhood disadvantage. Alcohol may only be used to reduce stress by those individuals who drink to improve their emotional states or who expect alcohol to relieve stress or other negative emotions (Greeley and Oei, 1999). Thus, it would be informative to investigate individual differences in vulnerabilities to neighborhood stress that might contribute to increased alcohol (or other drug) use in disadvantaged neighborhoods. The second hypothesis was that neighborhood affluence would be positively associated with drinking within recommended guidelines (a relatively healthy alcohol use pattern) and negatively associated with frequent drunkenness (posited to be incompatible with a healthy or conventional lifestyle), but the data did not support this. A study from New York City suggests neighborhood-level norms about drunkenness are related to drinking patterns (Ahern et al., 2008). Future studies examining whether norms vary by neighborhood SES would be able to provide an alternative test of this hypothesis.
Limitations of this study should be noted. First, analyses cannot account for length of neighborhood residence, and the data are cross-sectional. A recent longitudinal study demonstrated that men diagnosed as alcohol dependent were significantly more likely to move to disadvantaged neighborhoods over time (Buu et al., 2007), and this neighborhood selection pattern presumably would be similar, or perhaps even more acute, for heavy drug users. A recent critical literature review documented that relationships between neighborhood socioeconomic status and substance use outcomes do not differ markedly for cross-sectional and longitudinal studies (Karriker-Jaffe, 2011), but longitudinal studies of neighborhood effects on adults could provide more nuanced understanding of the interplay between individuals and their neighborhood environments over time. Another limitation pertains to the relatively low response rate of this and other recent U.S. telephone surveys (Midanik and Greenfield, 2002). Alternative methods for recruiting and engaging nationally-representative samples for both cross-sectional and longitudinal studies of health behaviors are needed. Despite these limitations, the very large, nationally-representative sample of U.S. adults derived from the two National Alcohol Surveys is unique and provided statistical power necessary to examine effects of neighborhood SES on relatively rare substance use outcomes. The current examination of effects of neighborhood affluence, as well as disadvantage, also fills a critical gap in the extant literature.
Findings have implications for prevention of substance use. Environmental and community systems prevention focuses on individuals and their environments by altering social, cultural, economic and physical contexts to shift conditions away from those that promote substance use to those that support health (Holder, 1998). In addition to affecting targeted individuals at a given time, these approaches also potentially benefit individuals who later enter the improved environment (Rose, 1985; Thomas, 2007). This study provides some evidence that environmental interventions targeting both disadvantaged and middle-class neighborhoods may help prevent substance use. In particular, in middle-class neighborhoods (the majority of U.S. neighborhoods), there are unmet needs in terms of anti-smoking messages directed to younger men. Further, older women in affluent neighborhoods also may need to be reached with information about recommended drinking guidelines, particularly because recent efforts to implement screening and brief intervention for alcohol problems in primary care settings suggest this intervention may be less effective for women than men (Kaner et al., 2009). Thus, it may be beneficial to develop targeted interventions to serve these higher-risk populations in neighborhoods where they live.
Acknowledgments
Role of Funding Source
National Institute on Alcohol Abuse and Alcoholism (NIAAA) provided funding that supported this study. The NIAAA had no further role in study design; in the collection, analysis or interpretation of data; in the writing of the report; or in the decision to submit the paper for publication. The content is solely the responsibility of the author and does not necessarily represent the official views of the NIAAA or the National Institutes of Health.
I would like to thank Drs. Sarah Zemore, Nina Mulia and Jason Bond for their helpful feedback throughout this study. National Institute on Alcohol Abuse and Alcoholism (NIAAA) provided funding for the National Alcohol Surveys (P30 AA05595, T. Greenfield, PI), post-doctoral research fellowship (T32 AA00724, L. Kaskutas, PI) and research grant (R21 AA019175, K.J. Karriker-Jaffe, PI) that supported this study.
Footnotes
Contributors
Dr. Karriker-Jaffe designed the study, undertook the statistical analysis and wrote the manuscript.
Conflict of Interest
Dr. Karriker-Jaffe declares she has no conflicts of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Ahern J, Galea S, Hubbard A, Midanik L, Syme SL. “Culture of Drinking” and individual problems with alcohol use. Am J Epidemiol. 2008;167:1041–1049. doi: 10.1093/aje/kwn022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernard P, Charafeddine R, Frohlich KL, Daniel M, Kestens Y, Potvin L. Health inequalities and place: a theoretical conception of neighborhood. Soc Sci Med. 2007;65:1839–1852. doi: 10.1016/j.socscimed.2007.05.037. [DOI] [PubMed] [Google Scholar]
- Bluthenthal RN, Cohen DA, Farley TA, Scribner R, Beighley C, Schonlau M, Robinson PL. Alcohol availability and neighborhood characteristics in Los Angeles, California and Southern Louisiana. J Urban Health. 2008;85:191–205. doi: 10.1007/s11524-008-9255-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boardman JD, Finch BK, Ellison CG, Williams DR, Jackson JS. Neighborhood disadvantage, stress, and drug use among adults. J Health Soc Behav. 2001;42:151–165. [PubMed] [Google Scholar]
- Bradizza CM, Stasiewicz PR. Qualitative analysis of high-risk drug and alcohol use situations among severly mentally ill substance abusers. Addict Behav. 2003;28:157–168. doi: 10.1016/s0306-4603(01)00272-6. [DOI] [PubMed] [Google Scholar]
- Bronfenbrenner U. The Ecology of Human Development: Experiments by Nature and Design. Harvard University Press; Cambridge, MA: 1979. [Google Scholar]
- Browning CR, Cagney KA. Moving beyond poverty: neighborhood structure, social processes, and health. J Health Soc Behav. 2003;44:552–571. [PubMed] [Google Scholar]
- Bryden A, Roberts B, McKee M, Petticrew M. A systematic review of the influence on alcohol use of community level availablity and marketing of alcohol. Health Place. 2012;18:349–357. doi: 10.1016/j.healthplace.2011.11.003. [DOI] [PubMed] [Google Scholar]
- Buu A, Mansour M, Wang J, Refior SK, Fitzgerald HE, Zucker RA. Alcoholism effects on social migration and neighborhood effects on alcoholism over the course of 12 years. Alcohol Clin Exp Res. 2007;31:1545–1551. doi: 10.1111/j.1530-0277.2007.00449.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chuang YC, Ennett ST, Bauman KE, Foshee VA. Neighborhood influences on adolescent cigarette and alcohol use: mediating effects through parent and peer behaviors. J Health Soc Behav. 2005;46:187–204. doi: 10.1177/002214650504600205. [DOI] [PubMed] [Google Scholar]
- Cockerham WC, Rütten A, Abel T. Conceptualizing contemporary health lifestyles: moving beyond Weber. Sociolog Q. 1997;38:321–342. [Google Scholar]
- Cohen DA, Farley TA, Mason K. Why is poverty unhealthy? Social and physical mediators. Soc Sci Med. 2003;57:1631–1641. doi: 10.1016/s0277-9536(03)00015-7. [DOI] [PubMed] [Google Scholar]
- Cook TD, Shagle SC, Degirmencioglu SM. Capturing social process for testing mediational models of neighborhood effects. In: Brooks-Gunn J, Duncan GJ, Aber JL, editors. Neighborhood Poverty: Policy Implications in Studying Neighborhoods. Russell Sage Foundation; New York: 1997. pp. 94–119. [Google Scholar]
- Datta GD, Subramanian SV, Colditz GA, Kawachi I, Palmer JR, Rosenberg L. Individual, neighborhood, and state-level predictors of smoking among US Black women: a multilevel analysis. Soc Sci Med. 2006;63:1034–1044. doi: 10.1016/j.socscimed.2006.03.010. [DOI] [PubMed] [Google Scholar]
- Dawson DA, Goldstein RB, Chou SP, Ruan WJ, Grant BF. Age at first drink and the first incident of adult-onset DSM-IV alcohol use disorders. Alcohol Clin Exp Res. 2008;32:2149–2160. doi: 10.1111/j.1530-0277.2008.00806.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dawson DA, Harford TC, Grant BF. Family history as a predictor of alcohol dependence. Alcohol Clin Exp Res. 1992;16:572–575. doi: 10.1111/j.1530-0277.1992.tb01419.x. [DOI] [PubMed] [Google Scholar]
- Diez Roux AV, Stein Merkin S, Hannan P, Jacobs DR, Kiefe CI. Area characteristics, individual-level socioeconomic indicators, and smoking in young adults. Am J Epidemiol. 2003;157:315–326. doi: 10.1093/aje/kwf207. [DOI] [PubMed] [Google Scholar]
- Duncan C, Jones K, Moon G. Smoking and deprivation: are there neighbourhood effects? Soc Sci Med. 1999;48:497–505. doi: 10.1016/s0277-9536(98)00360-8. [DOI] [PubMed] [Google Scholar]
- Duncan SC, Duncan TE, Strycker LA. Risk and protective factors influencing adolescent problem behavior: a multivariate latent growth curve analysis. Ann Behav Med. 2000;22:103–109. doi: 10.1007/BF02895772. [DOI] [PubMed] [Google Scholar]
- Eriksson M, Lindström B. Validity of Antonovsky’s sense of coherence scale: a systematic review. J Epidemiol Community Health. 2005;59:460–466. doi: 10.1136/jech.2003.018085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Esbensen FA, Huizinga D. Community structure and drug use: from a social disorganization perspective. Justice Q. 1990;7:691–709. [Google Scholar]
- Ewart CK, Suchday S. Discovering how urban poverty and violence affect health: development and validation of a neighborhood stress index. Health Psychol. 2002;21:254–262. doi: 10.1037//0278-6133.21.3.254. [DOI] [PubMed] [Google Scholar]
- Fitzpatrick K, LaGory M. Unhealthy Places: The Ecology of Risk in the Urban Landscape. Routledge; New York: 2000. [Google Scholar]
- Ford JM, Beveridge AA. Varieties of substance use and visible drug problems: individual and neighborhood factors. J Drug Issues. 2006;36:377–392. [Google Scholar]
- Galea S, Ahern J, Tracy M, Rudenstine S, Vlahov D. Education inequality and use of cigarettes, alcohol, and marijuana. Drug Alcohol Depend. 2007a;90:S4–S15. doi: 10.1016/j.drugalcdep.2006.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galea S, Ahern J, Tracy M, Vlahov D. Neighborhood income and income distribution and the use of cigarettes, alcohol and marijuana. Am J Prev Med. 2007b;32:S195–S202. doi: 10.1016/j.amepre.2007.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giggs J, Bean P, Whynes D, Wilkinson C. Class A drug users: prevalence and characteristics in Greater Nottingham. Br J Addict. 1989;84:1473–1480. doi: 10.1111/j.1360-0443.1989.tb03929.x. [DOI] [PubMed] [Google Scholar]
- Graham K, Massak A, Demers A, Rehm J. Does the association between alcohol consumption and depression depend on how they are measured? Alcohol Clin Exp Res. 2007;31:78–88. doi: 10.1111/j.1530-0277.2006.00274.x. [DOI] [PubMed] [Google Scholar]
- Greeley J, Oei T. Alcohol and tension reduction. In: Leonard KE, Blane HT, editors. Psychological Theories of Drinking and Alcoholism. The Guilford Press; New York, NY: 1999. pp. 14–53. [Google Scholar]
- Groves RM. Nonresponse rates and nonresponse bias in household surveys. Public Opin Q. 2006;70:646–675. [Google Scholar]
- Henriksen L, Feighery EC, Schleicher NC, Cowling DW, Kline RS, Fortmann SP. Is adolescent smoking related to the density and proximity of tobacco outlets and retail cigarette advertising near schools? Prev Med. 2008;47:210–214. doi: 10.1016/j.ypmed.2008.04.008. [DOI] [PubMed] [Google Scholar]
- Hill TD, Angel RJ. Neighborhood disorder, psychological distress, and heavy drinking. Soc Sci Med. 2005;61:965–975. doi: 10.1016/j.socscimed.2004.12.027. [DOI] [PubMed] [Google Scholar]
- Hoffmann JP. The community context of family structure and adolescent drug use. J Marriage Family. 2002;64:314–330. [Google Scholar]
- Holder HD. Alcohol and the Community: A Systems Approach to Prevention. Cambridge University Press; Cambridge, MA: 1998. [Google Scholar]
- Inagami S, Cohen DA, Finch BK. Non-residential neighborhood exposures suppress neighborhood effects on self-rated health. Soc Sci Med. 2007;65:1779–1791. doi: 10.1016/j.socscimed.2007.05.051. [DOI] [PubMed] [Google Scholar]
- Jones-Webb R, Snowden LR, Herd D, Short B, Hannan P. Alcohol-related problems among black, Hispanic, and white men: the contribution of neighborhood poverty. J Stud Alcohol. 1997;58:539–545. doi: 10.15288/jsa.1997.58.539. [DOI] [PubMed] [Google Scholar]
- Kadushin C, Reber E, Saxe L, Livert D. The substance use system: social and neighborhood environments associated with substance use and misuse. Subst Use Misuse. 1998;33:1681–1710. doi: 10.3109/10826089809058950. [DOI] [PubMed] [Google Scholar]
- Kandula NR, Wen M, Jacobs EA, Lauderdale DS. Association between neighborhood context and smoking prevalence among Asian Americans. Am J Public Health. 2009;99:885–892. doi: 10.2105/AJPH.2007.131854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaner EFS, Dickinson HO, Beyer FR, Campbell F, Schlesinger C, Heather N, Saunders JB, Burnand B, Pienaar ED. [Accessed: 2013-01-29];Effectiveness of brief alcohol interventions in primary care populations (Review) 2009 (4) doi: 10.1002/14651858.CD004148.pub3. Archived by WebCite® at http://www.webcitation.org/6E2l80uaL]. Cochrane Database System. Rev. p. 91. [DOI] [PubMed]
- Karriker-Jaffe KJ. Areas of disadvantage: a systematic review of effects of area-level socioeconomic status on substance use. Drug Alcohol Rev. 2011;30:84–95. doi: 10.1111/j.1465-3362.2010.00191.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karriker-Jaffe KJ, Kaskutas LA. Neighborhood socioeconomic context of alcohol use: a measurement validation study. Alcohol Clin Exp Res. 2009;33:190A, S1. [Google Scholar]
- Karriker-Jaffe KJ, Zemore SE, Mulia N, Jones-Webb RJ, Bond J, Greenfield TK. Neighborhood disadvantage and adult alcohol outcomes: differential risk by race and gender. J Stud Alcohol Drugs. 2012;73:865–873. doi: 10.15288/jsad.2012.73.865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karvonen S, Rimpelä A. Socio-regional context as a determinant of adolescents’ health behaviour in Finland. Soc Sci Med. 1996;43:1467–1474. doi: 10.1016/0277-9536(96)00044-5. [DOI] [PubMed] [Google Scholar]
- Karvonen S, Rimpelä AH. Urban small area variation in adolescents’ health behaviour. Soc Sci Med. 1997;45:1089–1098. doi: 10.1016/s0277-9536(97)00036-1. [DOI] [PubMed] [Google Scholar]
- Kerr WC. Categorizing US state drinking practices and consumption trends. Int J Environ Res Public Health. 2010;7:269–283. doi: 10.3390/ijerph7010269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kerr WC, Greenfield TK, Bond J, Ye Y, Rehm J. Age, period and cohort influences on beer, wine and spirits consumption trends in the US National Surveys. Addiction. 2004;99:1111–1120. doi: 10.1111/j.1360-0443.2004.00820.x. [DOI] [PubMed] [Google Scholar]
- Krieger N, Chen JT, Waterman PD, Soobader MJ, Subramanian SV, Carson R. Geocoding and monitoring of US socioeconomic inequalities in mortality and cancer incidence: does the choice of area-based measure and geographic level matter? Am J Epidemiol. 2002;156:471–482. doi: 10.1093/aje/kwf068. [DOI] [PubMed] [Google Scholar]
- Krieger N, Waterman P, Lemieux K, Zierler S, Hogan JW. On the wrong side of the tracts? Evaluating the accuracy of geocoding in public health research. Am J Public Health. 2001;91:1114–1116. doi: 10.2105/ajph.91.7.1114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lambert SF, Brown TL, Phillips CM, Ialongo NS. The relationship between perceptions of neighborhood characteristics and substance use among urban African American adolescents. Am J Community Psychol. 2004;34:205–218. doi: 10.1007/s10464-004-7415-3. [DOI] [PubMed] [Google Scholar]
- Leventhal T, Brooks-Gunn J. The neighborhoods they live in: the effects of neighborhood residence on child and adolescent outcomes. Psychol Bull. 2000;126:309–337. doi: 10.1037/0033-2909.126.2.309. [DOI] [PubMed] [Google Scholar]
- Livingston M, Chikritzhs T, Room R. Changing the density of alcohol outlets to reduce alcohol-related problems. Drug Alcohol Rev. 2007;26:557–566. doi: 10.1080/09595230701499191. [DOI] [PubMed] [Google Scholar]
- Matheson FI, White HL, Moineddin R, Dunn JR, Glazier RH. Drinking in context: the influence of gender and neighbourhood deprivation on alcohol consumption. J Epidemiol Community Health. 2011;66:e4. doi: 10.1136/jech.2010.112441. [DOI] [PubMed] [Google Scholar]
- McGue M, Slutske W, Taylor J, Iacono WG. Personality and substance use disorders: I. effects of gender and alcoholism subtype. Alcohol Clin Exp Res. 1997;21:513–520. [PubMed] [Google Scholar]
- Midanik L. Drunkenness, feeling the effects, and 5+ measures. Addiction. 1999;94:887–897. doi: 10.1046/j.1360-0443.1999.94688711.x. [DOI] [PubMed] [Google Scholar]
- Midanik LT, Greenfield TK. Telephone Versus In-person Interviews for Alcohol Use: Results of the Year 2000 National Alcohol Survey. American Public Health Association; Philadelphia, PA: 2002. Nov 11–14, [Google Scholar]
- Midanik LT, Greenfield TK. Defining “current drinkers” in national surveys: results of the 2000 National Alcohol Survey. Addiction. 2003;98:517–522. doi: 10.1046/j.1360-0443.2003.00344.x. [DOI] [PubMed] [Google Scholar]
- Midanik LT, Zabkiewicz D. Indicators of sense of coherence and alcohol-related problems: the 2000 U.S. National Alcohol Survey. Subst Use Misuse. 2009;44:357–373. doi: 10.1080/10826080802347511. [DOI] [PubMed] [Google Scholar]
- Moos RH, Fenn CB, Billings AG, Moos BS. Assessing life stressors and social resources: applications to alcoholic patients. J Subst Abuse. 1989;1:135–152. doi: 10.1016/s0899-3289(88)80017-8. [DOI] [PubMed] [Google Scholar]
- Mulia N, Karriker-Jaffe KJ. Interactive influences of neighborhood and individual socioeconomic status on alcohol consumption and problems. Alcohol Alcohol. 2012;47:178–186. doi: 10.1093/alcalc/agr168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mulia N, Schmidt L, Bond J, Jacobs L, Korcha R. Stress, social support and problem drinking among women in poverty. Addiction. 2008;103:1283–1293. doi: 10.1111/j.1360-0443.2008.02234.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Institute on Alcohol Abuse and Alcoholism. NIH Publication No 07-3769. National Institute on Alcohol Abuse and Alcoholism; Rockville, MD: 2005. [accessed 12/11/09]. Helping Patients Who Drink Too Much: A Clinician’s Guide. Updated 2005 Edition. [ http://pubs.niaaa.nih.gov/publications/Practitioner/CliniciansGuide2005/guide.pdf. [Google Scholar]
- Nowlin PR, Colder CR. The role of ethnicity and neighborhood poverty on the relationship between parenting and adolescent cigarette use. Nicotine Tob Res. 2007;9:545–556. doi: 10.1080/14622200701239613. [DOI] [PubMed] [Google Scholar]
- Palfai TP, Cheng DM, Samet JH, Kraemer KL, Roberts MS, Saitz R. Depressive symptoms and subsequent alcohol use and problems: a prospective study of medical inpatients with unhealthy alcohol use. J Stud Alcohol Drugs. 2007;68:673–680. doi: 10.15288/jsad.2007.68.673. [DOI] [PubMed] [Google Scholar]
- Pollack CE, Cubbin C, Ahn D, Winkleby M. Neighbourhood deprivation and alcohol consumption: does the availability of alcohol play a role? Int J Epidemiol. 2005;34:772–780. doi: 10.1093/ije/dyi026. [DOI] [PubMed] [Google Scholar]
- Prescott CA, Kendler KS. Age at first drink and risk for alcoholism: a noncausal association. Alcohol Clin Exp Res. 1999;23:101–107. [PubMed] [Google Scholar]
- Radloff LS. The CES-D Scale: a self-report depression scale for research in the general population. Appl Psychol Measure. 1977;1:385–401. [Google Scholar]
- Robert SA. Socioeconomic position and health: the independent contribution of community socioeconomic context. Annu Rev Sociol. 1999;25:489–516. [Google Scholar]
- Roberts RE. Reliability of the CES-D scale in different ethnic settings. Psychiatry Res. 1980;2:125–134. doi: 10.1016/0165-1781(80)90069-4. [DOI] [PubMed] [Google Scholar]
- Rose G. Sick individuals and sick populations. Int J Epidemiol. 1985;14:31–38. doi: 10.1093/ije/14.1.32. [DOI] [PubMed] [Google Scholar]
- Ross CE. Walking, exercising, and smoking: does neighborhood matter? Soc Sci Med. 2000;51:265–274. doi: 10.1016/s0277-9536(99)00451-7. [DOI] [PubMed] [Google Scholar]
- Sampson RJ, Groves WB. Community structure and crime: testing social disorganization theory. Am J Sociol. 1989;94:774–802. [Google Scholar]
- Shohaimi S, Luben R, Wareham N, Day N, Bingham S, Welch A, Oakes S, Khaw KT. Residential area deprivation predicts smoking habit independently of individual educational level and occupational social class. A cross sectional study in the Norfolk cohort of the European Investigation into Cancer (EPIC-Norfolk) J Epidemiol Community Health. 2003;57:270–276. doi: 10.1136/jech.57.4.270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stasiewicz PR, Maisto SA. Two-factor avoidance theory: the role of negative affect in the maintenance of substance use and substance use disorder. Behav Ther. 1993;24:337–356. [Google Scholar]
- Stata Corp. Stata Statistical Software: Release 11.0. Stata Corporation; College Station, TX: 2009. [Google Scholar]
- Stimpson JP, Ju H, Raji MA, Eschbach K. Neighborhood deprivation and health risk behaviors in NHANES III. Am J Health Behav. 2007;31:215–222. doi: 10.5555/ajhb.2007.31.2.215. [DOI] [PubMed] [Google Scholar]
- Theall KP, Scribner R, Cohen D, Bluthenthal RN, Schonlau M, Lynch S, Farley TA. The neighborhood alcohol environment and alcohol-related morbidity (doi: 10.1093/alcalc/agp042) Alcohol Alcohol. 2009;44:491–499. doi: 10.1093/alcalc/agp042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomas YF. The social epidemiology of drug abuse. Am J Prev Med. 2007;32:S141–S146. doi: 10.1016/j.amepre.2007.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tseng M, Yeatts K, Millikan R, Newman B. Area-level characteristics and smoking in women. Am J Public Health. 2001;91:1847–1850. doi: 10.2105/ajph.91.11.1847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Census Bureau. Census 2000 Summary File 3—United States. Public Information Office, U.S. Census Bureau; Washington, DC: 2002. [Accessed: 2013-01-10]. Archived by WebCite® at http://www.webcitation.org/6DZgPzvaf. [Google Scholar]
- Wagle U. Rethinking poverty: definition and measurement. Intl Soc Sci J. 2002;54:155–165. [Google Scholar]
- Wainwright NWJ, Surtees PG, Welch AA, Luben RN, Khaw KT, Bingham SA. Sense of coherence, lifestyle choices and mortality. J Epidemiol Community Health. 2008;62:829–831. doi: 10.1136/jech.2007.066464. [DOI] [PubMed] [Google Scholar]
- Waitzman NJ, Smith KR. Phantom of the area: poverty-area residence and mortality in the United States. Am J Public Health. 1998;88:973–976. doi: 10.2105/ajph.88.6.973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wen M, Browning CR, Cagney KA. Poverty, affluence, and income inequality: neighborhood economic structure and its implications for health. Soc Sci Med. 2003;57:843–860. doi: 10.1016/s0277-9536(02)00457-4. [DOI] [PubMed] [Google Scholar]
- Williams CT, Latkin CA. Neighborhood socioeconomic status, personal network attributes, and use of heroin and cocaine. Am J Prev Med. 2007;32:S203–S210. doi: 10.1016/j.amepre.2007.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson N, Syme SL, Boyce WT, Battistich VA, Selvin S. Adolescent alcohol, tobacco, and marijuana use: the influence of neighborhood disorder and hope. Am J Health Promot. 2005;20:11–19. doi: 10.4278/0890-1171-20.1.11. [DOI] [PubMed] [Google Scholar]
- Wilson WJ. The Truly Disadvantaged: The Inner City, The Underclass and Public Policy. University of Chicago Press; Chicago: 1987. [Google Scholar]