Abstract
The objective of this study was to assess the impact of patient-provider race concordance on weight-related counseling among visits by obese patients. We hypothesized that race concordance would be positively associated with weight-related counseling. We used clinical encounter data obtained from the 2005–2007 National Ambulatory Medical Care Surveys (NAMCS). The sample size included 2,231 visits of black and white obese individuals (ages 20 and older) to their black and white physicians from the specialties of general/family practice and general internal medicine. Three outcome measures of weight-related counseling were explored: weight reduction, diet/nutrition, and exercise. Logistic regression was used to model the outcome variables of interest. Wald tests were used to statistically compare whether physicians of each race provided counseling at different rates for obese patients of different races. We did not observe a positive association between patient–physician race concordance and weight-related counseling. We found that visits by black obese patients to white doctors had a lower odds of exercise counseling as compared to visits by white obese patients to white doctors (odds ratio (OR) = 0.54; 95% confidence interval (CI): 0.31, 0.95), and visits by black obese patients to black physicians had lower odds of receiving weight-reduction counseling than visits among white obese patients seeing black physicians (OR = 0.34; 95% CI: 0.13, 0.90). Black obese patients receive less exercise counseling than white obese patients in visits to white physicians and may be less likely than white obese patients to receive weight-reduction counseling in visits to black physicians.
Introduction
Obesity—defined as a BMI greater than or equal to 30 kg/m2—is an important risk factor for mortality (1), is estimated to cost $147 billion annually (almost 10% of all medical spending), and is associated with annual medical costs which are 42% higher ($1429) than among healthy weight individuals (2). In the United States, blacks are disproportionately impacted by obesity; 44% of black adults are obese compared to 33% of white adults (3). Blacks are also at higher risk and experience a higher prevalence of the diseases associated with excess body weight compared to whites (e.g., type 2 diabetes) (4–6).
There is a growing body of evidence suggesting that obesity care is suboptimal. Most obese patients do not receive an obesity diagnosis when they visit their doctor (7). Research focused on patient-centered care (8) suggests that the quality of obesity care may be largely based on clinicians' ability to assess patients' attitudes regarding weight and body image, build rapport with patients, and counsel and facilitate patients' decisions to engage in weight-related behaviors such as diet and physical activity. Patient–physician communication and relationship problems may influence obesity care. For example, obese patients are more likely to report trying to lose weight or exercising regularly than nonobese patients, but physicians are less likely to perceive obese patients as engaging in those activities (9). Groups who are at higher risk for obesity are not more likely to receive exercise, diet, or weight-reduction counseling from their physician (7).
In 2003–2006, the proportion of obese adults told that they were overweight was significantly lower for blacks (62%) as compared with whites (69%) (10). Disproportionately poor communication between black patients and their physicians may contribute to suboptimal obesity care. One factor which may impact disparities in obesity care is race concordance between patients and clinicians (such as a black patient seeing a black doctor)—a question which has received increasing attention. Some studies have shown positive associations between race concordance and health-care processes and outcomes (8,11–17), while others have failed to show an association or have shown mixed results (18–20). Studies showing a positive association suggest that patients in race-concordant relationships with their physicians receive better quality of care (11,13,16), have longer visits and more participatory decision-making (8,13), more timely receipt of treatment (15), greater use of needed medical services (11), less delay in seeking care (11), more preventive care (14,18), and greater patient satisfaction with their provider and healthcare (8,12,17).
Despite the ample body of evidence identifying race/ethnicity as an important cultural barrier to the quality of the doctor–patient relationship (8,13,21–23), linking race concordance with better patient–physician communication and interpersonal care (8,16,24,25), and documenting racial disparities in prevalence and care for obesity (7,26,27), the impact of patient–doctor race concordance on obesity care has not been explored. An improved understanding of the relationship between patient-provider race concordance and obesity care among black obese individuals is critical to determine whether improved obesity care may result from concordant relationships, and if so, what the mechanism for improved care might be.
Another question is whether physician race in conjunction with patient race contribute to disparities in obesity care. In other words, do white physicians provide differential treatment to black and white obese patients? Similarly, do black physicians provide differential treatment to black and white obese patients? Despite known disparities in obesity care (7), and evidence documenting differences in health care based on physician race (8,11–17), we know of no research that examines whether disparities in obesity care differ by physician race.
The main purpose of this paper was to assess the impact of patient-provider race concordance on obesity care (defined as weight-related counseling) among non-Hispanic black and non-Hispanic white obese adults and their non-Hispanic black and non-Hispanic white physicians (hereafter referred to as “black” or “white”). Weight-related counseling was chosen since the clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults by the National Heart, Lung, and Blood Institute (28) and the U.S. Preventive Services Task Force (29) call for physicians to counsel their patients about weight loss and weight maintenance. We hypothesized that race concordance would be positively associated with weight-related counseling for obesity. We also hypothesized that the association of race concordance with weight-related counseling would be stronger among black obese patients than among white obese patients. A secondary purpose of this paper was to assess whether physicians of each race (white and black) provide differential care to white and black obese patients.
Methods and Procedures
Design
The study was a secondary analysis of a nationally representative cross-sectional survey of physician office visits.
Data
The data for this study was obtained from the 2005–2007 National Ambulatory Medical Care Surveys (NAMCS)—a nationally representative annual probability-sample survey of visits to office-based physicians in the United States conducted by the National Center for Health Statistics (30). The NAMCS uses a three-stage probability sampling procedure, with geographic primary sampling units as the first stage, physicians as the second stage, and visits to a sampled physician selected from a 1-week reporting period during the year as the third stage. Participating physicians are randomly selected from the master files of the American Medical Association and the American Osteopathic Association by specialty. Only patient visits to the offices of nonfederally employed physicians were included in the data. For each selected patient visit, data are collected concerning the specific clinical characteristics of the visit, including patient demographics, diagnoses (coded as International Classification of Diseases, Ninth Revision diagnostic codes), reason for visit, physician characteristics, visit characteristics, new or continued medications; diagnostic tests, and types of counseling ordered or provided; unweighted total visit response rate of 61.5% for 2005 (31), 59% for 2006 (32), and 61.6% for 2007 (33).
For this study, individuals were considered obese if their BMI was ≥30 kg/m2 or if the checkbox for obesity was marked on the NAMCS abstraction form. Less than 3% of the sample had the obesity checkbox marked with no BMI available. The sample size for the analysis included 2,231 visits of black or white obese individuals (ages 20 and older) to their black or white physicians from the specialties of general/family practice and general internal medicine. We included only these specialties based on literature suggesting that they share common attitudes toward obesity management (34). Measures of patient height and body weight were obtained at the time of the sampled patient visit. If patient height and body weight were not measured at the visit, the abstractor or provider reviewed the patient chart for the last time height and weight were recorded (30).
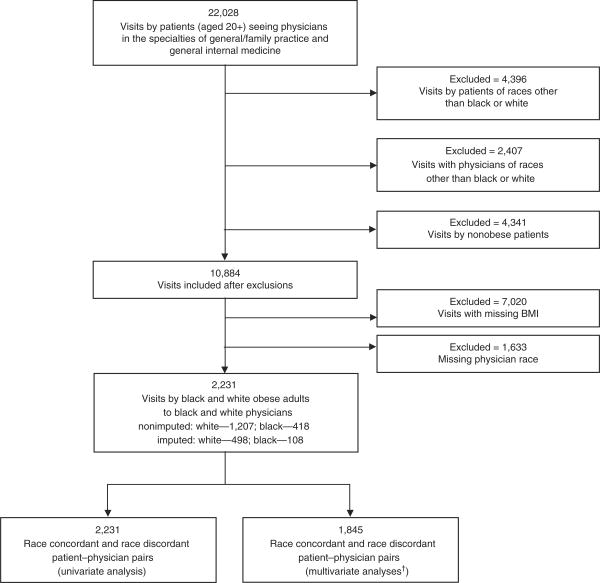
Item nonresponse within the NAMCS data for variables used to create the analytic sample reduced the sample size and potentially introduced bias. A discussion of the missing rates and analyses conducted to search for bias in the missing data is presented below. A flowchart identifying the inclusion and exclusion of study participants can be found in Figure 1.
Figure 1.
Flowchart for identification and inclusion of visits in study. †Lower n for pairs due to missing covariates.
Measures
Outcome variables
Three types of weight-related counseling were considered outcome measures for this analysis: weight-reduction counseling, diet/nutrition counseling, and exercise counseling. Visits by individuals were considered to have included diet/nutrition, exercise, or weight-reduction counseling if indicated via check box on the NAMCS encounter form. Diet/nutritional counseling included any topic related to the foods and/or beverages consumed by the patient as well as referrals to other health professionals, for example, dietitians and nutritionists. Exercise counseling included any topics related to the patient's physical conditioning or fitness as well as referrals to other health and fitness professionals. It did not include referrals for physical therapy. Weight-reduction counseling included any information given to the patient to assist in the goal of weight reduction as well as referrals to other health professionals for the purpose of weight reduction (33). Each outcome variable was examined as a separate, dichotomous outcome variable.
Independent variables
The primary independent variable of interest was patient-doctor race concordance defined as the following four categories: race-discordant white (white patient seeing a black physician), race-discordant black (black patient seeing a white physician), race-concordant white (white patient seeing a white physician) and race-concordant black (black patient seeing a black physician). We excluded Hispanic and Asian patients and physicians because the sample sizes for the race-concordant groups were too small to provide stable estimates on which to base inferences. Also, patients going to physicians of unknown race/ethnicity were excluded. Physician race/ethnicity was based on physician report. Patient race/ethnicity was based on physician report or from information in the medical record. Missing patient race/ethnicity was imputed by National Center for Health Statistics for 23.5% of records in our sample, but physician race was not imputed.
Covariates included: patient sociodemographic characteristics (gender, age, region, and health insurance), patient risk (comorbidity risk status), characteristics of the clinical encounter (visit type, seen before by practice, and length of the visit), and physician characteristics (gender and age). The physician characteristics were obtained from the restricted access NAMCS data file. Insurance was defined as private or nonprivate (Medicare, Medicaid, worker's compensation, self-pay, charity, other). The type of clinical visit was defined as preventive (e.g., routine or general exam), ongoing chronic problem, or acute problem. All covariates were included in the models based on the literature (7,35,36). We categorized patients according to their overall comorbidity risk status using the clinical guidelines forwarded by the National Heart, Lung, and Blood Institute for the identification, evaluation and treatment of obesity in adults (28). International Classification of Diseases, Ninth Revision diagnostic codes were used to identify patient comorbidities. Patients were classified as having a very high comorbidity risk if they had ischemic heart disease (410–414), diabetes (250), sleep apnea, (780.57) or other atherosclerotic diseases (peripheral arterial disease, 443.9; abdominal aortic aneurysm, 441; symptomatic carotid artery disease, 433.1); high risk if they had any one of the following: osteoarthritis (715), gallstones (574), stress incontinence (female 625.6; male 788.32), hyperlipidemia (272), hypertension (401–405), smoked cigarettes or were men aged 45 and older, or women aged 55 years or older; and lower risk if they were obese but had no other obesity-related risk factors.
Statistical analyses
χ2 tests were used to test differences in the frequency of weight-related counseling by patient–physician race group. Multivariate logistic regression was used to model the outcome variables of interest. A separate model was created for each outcome. To test our main study hypothesis, after estimating the models, we used a Wald test to statistically compare the coefficients of the black-concordant vs. black-discordant groups and white-concordant vs. white-discordant groups. To test our secondary hypothesis (10,26), we also used a Wald test to compare the coefficients of black patient/black physician vs. white patient/black physician pairs and white patient/white physician vs. black patient/white physician pairs. is tested whether physicians of each race provided counseling at different rates for patients of different races. When significant findings were obtained from the Wald test of coefficients, the model was rerun changing the reference category to obtain ORs for the significant relationship. As a sensitivity analysis, we conducted these analyses excluding visits for which race or ethnicity was imputed. These results are reported only where they differ from those using imputed data for race and ethnicity.
For all analyses, we used the patient visit survey weight provided in the NAMCS dataset. After inspection of the data, we determined that each patient saw a different doctor, so no clustering at the physician level was needed. Statistical analyses were performed using the STATA, version 9.2 software package (StataCorp LP, College Station, TX), using survey functions to adjust for the complex survey design.
Results
Characteristics of the study sample, patient–physician race concordance and outcome variables
Table 1 reports the characteristics of the study sample. A majority of visits in the study sample were by patients who were white (83%), female (57%), age 45 and older (74%), insured with private insurance (60%) and had a high or very high comorbidity risk status (65%). Among the physicians in the sample, 93% were white, 27% were female and 58% were under the age of 55. Roughly half of the clinical encounters were characterized as preventive or chronic (preventive, 17%; chronic 35%), most encounters were by patients who had been seen before by someone in the clinical practice (93%), although not necessarily by the current physician, and most clinical visits were 13 min or longer (74%).
Table 1. Characteristics of visits by non-Hispanic black and non-Hispanic white obese adults aged 20 and older to general/family practitioners or internal medicine physicians, National Ambulatory Medical care survey, 2005–2007.
| % (CI) | Missing (%) | |
|---|---|---|
| Patients | ||
| Sociodemographic characteristics | ||
| Race | ||
| White | 82.7 (77.4, 87.0) | 0.0 |
| Black | 17.3 (13.0, 22.6) | |
| Gender | ||
| Female | 56.7 (53.3, 60.0) | 0.0 |
| Male | 43.3 (40.0, 46.7) | |
| Age | ||
| 20–29 | 7.2 (5.8, 8.8) | 0.0 |
| 30–44 | 20.6 (18.1, 23.3) | |
| 45–64 | 46.8 (43.6, 50.0) | |
| 65+ | 25.5 (22.7, 28.5) | |
| Insurance | ||
| Private | 60.0 (55.6 64.3) | 3.5 |
| Nonprivate | 36.5 (32.3, 40.1) | |
| Region | ||
| Northeast | 13.6 (9.3, 19.5) | 0.0 |
| Midwest | 31.6 (22.9, 41.8) | |
| South | 37.3 (29.2, 46.1) | |
| West | 17.5 (12.0, 24.8) | |
| Comorbidity risk status | ||
| Very high risk | 16.5 (14.4, 18.8) | 8.4 |
| High risk | 49.3 (45.9, 52.8) | |
| Lower risk | 25.8 (22.3, 29.67) | |
| Physicians | ||
| Sociodemographic characteristics | ||
| Race | ||
| White | 92.6 (86.7, 96.0) | 0.0 |
| Black | 7.4 (4.0, 13.3) | |
| Gender | ||
| Female | 27.1 (20.5, 34.9) | 0.0 |
| Male | 72.9 (65.1, 79.5) | |
| Age | ||
| Under 55 | 58.1 (49.2, 66.5) | 1.7 |
| 55 and older | 41.6 (33.3, 50.5) | |
| Characteristics of clinical encounter | ||
| Visit type | ||
| Preventive | 17.3 (15.6, 20.5) | 1.6 |
| Chronic, ongoing | 34.9 (31.3, 38.6) | |
| Acute visit | 46.1 (42.6, 49.7) | |
| Seen before by anyone in practice: Yes | 93.1 (90.1, 94.8) | 0.0 |
| Time spent with doctor | ||
| 0–12 min | 18.7 (14.8, 23.6) | 0.0 |
| 13–24 min | 55.4 (50.6, 60.1) | |
| >24 min | 25.8 (22.0, 30.1) | |
| Patient–physician race concordance | ||
| Discordant white (white patient/black physician) | 1.9 (1.0, 3.9) | 0.0 |
| Discordant black (black patient/white physician) | 11.9 (8.9, 15.6) | |
| Concordant white (white patient/white physician) | 80.8 (74.7, 85.7) | |
| Concordant black (black patient/black physician) | 5.4 (2.7, 10.5) | |
| Visits with weight-related counseling | ||
| Weight reduction | 22.1 (18.1, 26.8) | 0.0 |
| Diet/nutrition | 29.8 (25.5, 34.3) | 0.0 |
| Exercise | 22.8 (18.9, 27.3) | 0.0 |
| Any weight-related counseling | 39.6 (35.0, 44.5) | 0.0 |
Individuals were considered to be obese if their BMI ≥30 kg/m2. Numbers may not sum to 100% due to rounding error. Patients were classified as having a very high comorbidity risk if they had ischemic heart disease (410–414), diabetes (250), sleep apnea (780.57) or other atherosclerotic diseases (peripheral arterial disease, 443.9; abdominal aortic aneurysm, 441; symptomatic carotid artery disease, 433.1); high risk if they had any one of the following: osteoarthritis (715), gallstones (574), stress incontinence (female 625.6; male 788.32), hyperlipidemia (272), hypertension (401–405), smoked cigarettes or were men aged 45 and older, or women aged 55 years or older; and lower risk if they were obese but had no other obesity-related risk factors.
CI, confidence interval.
Among patient–physician pairs, 2% were discordant white, 12% were discordant black, 81% were concordant white, and 5% were concordant black. In approximately one fifth of visits, patients received weight-reduction counseling (22%), in 30% of visits patients received diet/nutrition counseling, and in 23% of visits patients received exercise counseling. In almost 40% of visits, patients received at least one of the three types of weight-related counseling.
Frequency of weight-related counseling by patient-doctor race concordance
The frequency of each type of weight-related counseling (weight-reduction, diet/nutrition, and exercise) among race-concordant and race-discordant pairs is presented in Table 2. For weight-reduction counseling, the frequency of visits with counseling ranged from almost 12% among concordant black pairs to almost 26% among discordant white pairs. For diet/nutrition counseling, the frequency of visits with counseling ranged from almost 25% among discordant black pairs to almost 37% among concordant black pairs. For exercise counseling, the frequency of visits with counseling ranged from 15% among discordant black pairs to almost 30% among discordant white pairs.
Table 2. Frequency of weight-related counseling among visits by race-concordant and race-discordant patient–physician pairs, % (confidence interval) (n = 2,231), National Ambulatory Medical Care Survey, 2005–2007.
| Race of | N | Weight reduction | Diet/nutrition | Exercise | |
|---|---|---|---|---|---|
| Patient | Physician | ||||
| Black | White | 318 | 19.7 (14.5, 26.3) | 24.3 (17.0, 33.5) | 15.0 (9.7, 22.3) |
| Black | Black | 208 | 11.8 (4.0, 29.4) | 36.5 (22.7, 52.9) | 25.8 (11.2, 48.8) |
| White | Black | 57 | 25.5 (12.3, 45.6) | 32.9 (15.0, 57.6) | 29.4 (12.1, 55.7) |
| White | White | 1,648 | 23.1 (18.5, 28.4) | 30.0 (25.4, 35.1) | 23.6 (19.4, 28.4) |
| P value | 0.28 | 0.46 | 0.33 |
P values are based on χ2 tests comparing rates between patient–physician race categories within each type of weight-related counseling.
The rates of weight-related counseling were not statistically different among any of the patient–physician race categories (P = 0.28 for weight-reduction counseling, P = 0.46 diet/nutrition counseling, and P = 0.33 for exercise counseling), providing no evidence of differences in weight-related counseling among any of the patient–physician race categories.
Adjusted association between weight-related counseling and patient–physician race concordance
Table 3 presents the adjusted associations between each type of weight-related counseling and patient–physician race concordance: weight reduction (first column), diet/nutrition (second column) and exercise (third column).
Table 3. Adjusted odds ratios (ORs) for weight-related counseling by patient–physician race concordance classification (n of pairs = 1,845), National Ambulatory Medical Care Survey, 2005–2007.
| Weight reduction counseling | Diet/nutrition counseling | Exercise counseling | ||
|---|---|---|---|---|
|
| ||||
| Race of | OR (95% CI) | OR (95% CI) | OR (95% CI) | |
| Patient | Physician | |||
| Black | White | 1.15 (0.72, 1.85) | 0.69 (0.39, 1.24) | 0.54 (0.31, 0.95)† |
| Black | Black | 0.49 (0.15, 1.61) | 1.25 (0.69, 2.27) | 1.02 (0.38, 2.70) |
| White | Black | 1.45 (0.61, 3.40) | 1.15 (0.61, 2.33) | 1.99 (0.81, 4.89) |
| White | White | 1.00 (Reference) | 1.00 (Reference) | 1.00 (Reference) |
| 1,845 | 1,845 | 1,845 | ||
CI, confidence interval.
Odds ratios are adjusted for: patient sociodemographic characteristics (gender, age, region, and health insurance), patient risk (comorbidity risk status), characteristics of the clinical encounter (visit type, seen before by practice, and length of the visit), and physician characteristics (gender, and age).
P value < 0.05.
After adjustment for potential confounders, visits by black patients seeing white doctors had a lower odds of including exercise counseling as compared to visits by white patients seeing white doctors (OR = 0.54; 95% CI: 0.31, 0.95). We observed no association between race concordance and weight-reduction or diet/nutrition counseling. However, the weight-reduction model indicated that visits by black obese patients seeing black physicians had significantly lower odds of including weight-reduction counseling than visits by white obese patients seeing black physicians (OR = 0.34; 95% CI: 0.13, 0.90). No other significant associations were observed.
Other significant predictors (P < 0.05) in all three models of weight-related counseling models included: patient's age, comorbidity risk status, visit type, and visit length. In the weight-reduction model and the diet/nutrition counseling model, visits by patients in the Northeast region had significantly higher odds of including weight-related counseling than in the other regions. Point estimates and CIs for the full models, including all covariates variables, can be found in the Supplementary Appendix online.
A model was run where the outcome variable was any counseling (data not shown). No significant findings related to race concordance were found. The results of the weight-reduction model using only unimputed data for race and ethnicity were substantially similar to those using imputed data. However, the finding that visits by black obese patients seeing black physicians had lower odds of including weight-reduction counseling than visits by white obese patients seeing black physicians did not reach statistical significance (P = 0.088).
Discussion
This paper is among the first to examine the relationship between patient-provider race concordance and obesity care. Despite prior research suggesting greater use of needed medical services among race-concordant pairs (11), we did not find support for our hypothesis that race concordance would be positively associated with obesity care. With respect to the hypothesis that white and black physicians treat their white and black obese patients differently, we found only one effect that was significant in both the main analysis and in sensitivity analysis: visits by black patients to white doctors were less likely to include exercise counseling as compared to visits by white patients to white doctors. We also found that visits by black obese patients to black doctors were less likely to include weight-reduction counseling than visits by white obese patients to black doctors, although this finding may be more tenuous as it did not reach statistical significance in the sensitivity analysis without the imputed patient race/ethnicity data. These findings suggest that visits by black patients include less exercise counseling than visits by white patients when they see white doctors and less weight-reduction counseling than white patients when they see black doctors. In this sample, patient–physician race concordance does not appear to have a positive impact on weight-related counseling for visits among black obese patients. We also evaluated a model to predict any weight-related counseling and found no differences by concordance status for either black or white patients.
There are several potential reasons why black obese patients might receive less obesity care than white obese patients. Several studies suggest that physicians hold more negative perceptions about likelihood of adherence, engagement in risk behaviors, and social resources available to black patients (37). The low rates of weight-reduction counseling among black patients seeing black physicians may also reject black physicians' efforts to be culturally sensitive to their black patients. Several studies have shown differences in body image and perceptions of overweight and obesity status between blacks and whites (38,39). It could also be the case that physicians may not be aware that blacks, as compared to whites, are disproportionately impacted by obesity (3). Physicians may lack sensitivity to underlying levels of obesity risk in the adult population. The similarly low rate of weight-related counseling among black and white physicians could additionally reflect inadequate usage of clinical obesity guidelines; in other words physicians may generally not get adequate training or have adequate resources to provide weight-related counseling to their obese patients, regardless of their race. It could also reflect physicians' belief that their advice will have little effect on patient behavior (40,41), that patients are not interested or ready for treatment (40,42–44), and that obesity is the responsibility of the patient (45).
These results, like previous research (7), indicate that despite clinical guidelines suggesting that clinicians screen all adult patients for obesity and offer intensive counseling to promote sustained weight loss for obese adults, rates of weight-related counseling are low, regardless of patient race/ethnicity (29). Although studies fail to document disparities in weight-related counseling, factors that contribute to suboptimal rates of weight-related counseling may differ for black and white patients. We hypothesized that race concordance might be one such factor among black patients, but our study suggests this is not the case. Future work should examine similarities and differences in the contribution of patient, clinician, and health system factors to low levels of weight-related counseling among patients of different ethnic groups.
Our finding of low rates of weight-related counseling may be a reflection of general physician stigma toward obesity that has been documented (34,46) as well as lower physician respect toward patients with a higher BMI (47). Also, consistent with past studies, we found that other factors influence weight-related counseling such as patient's gender, age, and comorbidity risk status as well as characteristics of the clinical encounter (e.g., type of visit, time spent with the doctor) (7). Like previous studies (10,26), our results suggest less weight-related counseling in visits by black patients than in visits by white patients.
Improving rates of weight-related counseling in primary care settings is an important strategy to promote behavior change in obese patients. There is a growing body of evidence suggesting that patients who are told by their physician that they are overweight are more likely to lose weight relative to those who are not told (48,49), that patients who are counseled about their weight or weight-related behaviors are more likely to report working on those areas (50–53), and that patients who are advised by their physician to modify their behavior are generally more confident and motivated to engage in lifestyle modifications (e.g., dietary changes, increased physical activity) (51,54,55).
The mechanism through which race concordance has been primarily associated with positive patient–physician interaction is through perceptions of similarity (56–58). Patient's preference for health care providers of their same race/ethnicity (59) may also be in response to well documented unequal treatment in heath care by race/ethnicity (60). In addition to race/ethnicity, there are several other shared identities between the patient and their physician which may also impact obesity care. Therefore, future research could examine the impact of other shared characteristics, including patient–physician gender concordance on obesity care. Previous research on gender concordance and quality of care has found, for example, that preventive screening rates were higher among women seeing female doctors (61). Future work could also explore why the patterns we observed between race concordance and weight-related counseling differ by the type of counseling.
There are several limitations to this analysis worth noting. First, that we don't observe an effect in some of the race-concordant groups could be because our sample size, especially for white patients seeing black physicians, is too small. Second, unmeasured patient or physician factors may have affected our findings. Examples include patient familiarity with their physician, patient and physician attitudes toward race/ethnicity and preferred communication styles. Third, the data rely on physician reports (which cannot be objectively verified), and which may lead to an underestimation of weight-related counseling given evidence suggesting that physicians underreport behavioral counseling (62). However, recent research validating the NAMCS indicates that it is highly specific, suggesting that if physicians report having delivered a service, there is a high likelihood that it was given (63); even if a physician reporting bias existed, it would be unlikely to differ by race concordance in the patient–physician relationship. Weight-related counseling could also be underestimated if physicians provided weight-related counseling to their obese patients but did not document it in the medical chart as it is typically not reimbursed by insurance companies (64). However, it is unlikely that underreporting of weight-related counseling would vary by doctor–patient race concordance. Nonetheless, to address this potential limitation, we controlled for patient insurance type in the analysis given that reimbursement for weight-related counseling may differ by type of health insurance. Fourth, patient race ethnicity is based upon the physician's report or abstraction from the medical record by office staff or a federal abstractor. It is unknown to what extent patient race/ethnicity is based on the physician's (or potentially even the office staff's) perception of the patient's race/ethnicity as compared to the physician or office staff having asked the patient about their own perception. A physician's perception of a patient's race/ethnicity may differ from the patient's own perception; however, it is likely that physicians' perceptions of patients' race/ethnicity influence their own communication behaviors and decision-making. Fifth, because the NAMCS is a visit-based survey, obese patients who see their physician more often may have received weight-reduction counseling at a clinical encounter not captured by the survey. Sixth, patients were considered to have received weight-related counseling if it was “ordered or provided” at the clinical encounter. In the case of ordered services, it was not possible to know whether the patient actually received them. It is also not possible to know the quality of counseling services provided or ordered. Seventh, we are unable to determine from the data whether patients had health insurance coverage for weight-reduction counseling. However, we controlled for respondents' health insurance status as a crude proxy for access to obesity-related services. Eighth, we controlled for the length of the clinical visit based on literature which suggested that race concordance is associated with longer clinical encounters (8); however, weight-related counseling may be associated with longer visit times which could lead to overcontrolling and thus bias the estimates of our outcome variables toward the null. We did run the models excluding length of visit (data not shown) and the estimates did not change significantly. Ninth, we would have ideally included other measures in our risk status variable, such as physical inactivity, but those data were not available in the 2005–2007 NAMCS.
Finally, missing data creates the potential for bias in the analysis. Among the 10,884 visits that met the inclusion criteria for the study or had missing data on inclusion criteria, whether a patient was obese could not be determined for 64% of the visits and physician race and ethnicity was missing for an additional 15% of the visits. In addition, as stated above, patient race/ethnicity was imputed for 23.5% of the sample. To look for bias due to each of these areas of missing data, we conducted the following analyses. First, as described above, we conducted all analyses with and without imputed patient race/ethnicity. Second, to look for bias in cases with missing concordance as a whole, we compared the rate of each type of weight-related counseling in visits with known concordance status to those with missing concordance status. We found no significant relationship between missing concordance status and receipt of any type of weight-related counseling. To assess whether bias might exist in the multivariate models, we repeated our logistic regression models using concordance (missing vs. not missing) as the dependent variable and the weight-related counseling variables as the independent variables of interest. Again, no type of weight-related counseling predicted whether concordance was missing. These analyses were also conducted using only cases with unimputed race, and similar results were found.
In searching for bias among visits with missing BMI, we noted that if observations with missing BMI followed a similar distribution to those with BMI, ∼46% of those with missing BMI would be obese. However, we hypothesized that height and body weight might be more likely to be recorded if a patient were obese. We, therefore, examined the percent of each type of weight-related counseling within visits by obese patients, nonobese patients, and for visits among patients with unknown obesity status. Compared to known obese patients, rates of all types of counseling were significantly lower among visits by nonobese patients and among visits by patients with unknown obesity status. Compared to nonobese patients, rates of counseling among visits by patients with unknown obesity status were neither significantly different nor significantly lower. These results suggest that bias from missing BMI is less likely since patients with unknown BMI are more similar to nonobese patients, who were excluded from the analysis. An alternative explanation is that in visits by obese patients where the physician does not measure height and weight, leading to missing BMI in the dataset, the physician may be less likely to provide counseling. If these visits are distributed differentially across patient-doctor race groups, this could lead to bias in the analysis. However, height and weight may be missing from the data set for a variety of reasons, including those related to abstraction of the data in addition to the failure of the physician to obtain height and weight at the visit. We also examined whether missing BMI data differed systematically for our primary dependent variable (doctor–patient race concordance) and found no statistically significant differences.
Although our analyses were unable to uncover bias due to missing data, we recognize that, as in all studies with high rates of missing or imputed data, the potential for bias still exists.
Our data suggest that black obese patients receive less exercise counseling than white obese patients in visits to white physicians and may be less likely than white obese patients to receive weight-reduction counseling in visits to black physicians. Further research is needed to understand how to improve counseling, particularly for black obese patients.
Supplementary Material
Acknowledgments
S.N.B., A.E.S., and L.A.C. conceived the study and developed the hypotheses. S.N.B. analyzed the data. All authors contributed to the interpretation of study findings. S.N.B. drafted the manuscript and all authors contributed to the final draft. S.N.B. is the guarantor. This work was supported by two grants from the National Heart, Lung, and Blood Institute (1K01HL096409 and K24HL083113). The findings and conclusions in this paper are those of the authors and do not necessarily reflect the views of the Centers for Disease Control and Prevention.
Footnotes
Supplementary Material: Supplementary material is linked to the online version of the paper at http://www.nature.com/oby
Disclosure: The authors declared no conflict of interest.
References
- 1.Flegal KM, Graubard BI, Williamson DF, Gail MH. Cause-specific excess deaths associated with underweight, overweight, and obesity. JAMA. 2007;298:2028–2037. doi: 10.1001/jama.298.17.2028. [DOI] [PubMed] [Google Scholar]
- 2.Finkelstein EA, Trogdon JG, Cohen JW, Dietz W. Annual medical spending attributable to obesity: payer-and service-specific estimates. Health Aff (Millwood) 2009;28:w822–w831. doi: 10.1377/hlthaff.28.5.w822. [DOI] [PubMed] [Google Scholar]
- 3.Flegal KM, Carroll MD, Ogden CL, Curtin LR. Prevalence and trends in obesity among US adults, 1999-2008. JAMA. 2010;303:235–241. doi: 10.1001/jama.2009.2014. [DOI] [PubMed] [Google Scholar]
- 4.Hajjar I, Kotchen TA. Trends in prevalence, awareness, treatment, and control of hypertension in the United States, 1988-2000. JAMA. 2003;290:199–206. doi: 10.1001/jama.290.2.199. [DOI] [PubMed] [Google Scholar]
- 5.Brancati FL, Whelton PK, Kuller LH, Klag MJ. Diabetes mellitus, race, and socioeconomic status. A population-based study. Ann Epidemiol. 1996;6:67–73. doi: 10.1016/1047-2797(95)00095-x. [DOI] [PubMed] [Google Scholar]
- 6.Centers for Disease Control and Prevention (CDC) Prevalence of diabetes and impaired fasting glucose in adults--United States, 1999–2000. MMWR Morb Mortal Wkly Rep. 2003;52:833–837. [PubMed] [Google Scholar]
- 7.Bleich SN, Pickett-Blakely O, Cooper LA. Physician practice patterns of obesity diagnosis and weight-related counseling. Patient Educ Couns. 2011;82:123–9. doi: 10.1016/j.pec.2010.02.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cooper LA, Roter DL, Johnson RL, et al. Patient-centered communication, ratings of care, and concordance of patient and physician race. Ann Intern Med. 2003;139:907–915. doi: 10.7326/0003-4819-139-11-200312020-00009. [DOI] [PubMed] [Google Scholar]
- 9.Bleich SN, Huizinga MM, Beach MC, Cooper LA. Patient use of weight-management activities: a comparison of patient and physician assessments. Patient Educ Couns. 2010;79:344–350. doi: 10.1016/j.pec.2010.01.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Agency for Healthcare Quality and Research. National Healthcare Disparities Report. Agency for Healthcare Quality and Research; Rockville: 2009. [Google Scholar]
- 11.LaVeist TA, Nuru-Jeter A, Jones KE. The association of doctor-patient race concordance with health services utilization. J Public Health Policy. 2003;24:312–323. [PubMed] [Google Scholar]
- 12.LaVeist TA, Carroll T. Race of physician and satisfaction with care among African-American patients. J Natl Med Assoc. 2002;94:937–943. [PMC free article] [PubMed] [Google Scholar]
- 13.Cooper-Patrick L, Gallo JJ, Gonzales JJ, et al. Race, gender, and partnership in the patient–physician relationship. JAMA. 1999;282:583–589. doi: 10.1001/jama.282.6.583. [DOI] [PubMed] [Google Scholar]
- 14.Lasser KE, Mintzer IL, Lambert A, Cabral H, Bor DH. Missed appointment rates in primary care: the importance of site of care. J Health Care Poor Underserved. 2005;16:475–486. doi: 10.1353/hpu.2005.0054. [DOI] [PubMed] [Google Scholar]
- 15.King WD, Wong MD, Shapiro MF, Landon BE, Cunningham WE. Does racial concordance between HIV-positive patients and their physicians affect the time to receipt of protease inhibitors? J Gen Intern Med. 2004;19:1146–1153. doi: 10.1111/j.1525-1497.2004.30443.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Saha S, Komaromy M, Koepsell TD, Bindman AB. Patient–physician racial concordance and the perceived quality and use of health care. Arch Intern Med. 1999;159:997–1004. doi: 10.1001/archinte.159.9.997. [DOI] [PubMed] [Google Scholar]
- 17.Laveist TA, Nuru-Jeter A. Is doctor-patient race concordance associated with greater satisfaction with care? J Health Soc Behav. 2002;43:296–306. [PubMed] [Google Scholar]
- 18.Saha S, Arbelaez JJ, Cooper LA. Patient–physician relationships and racial disparities in the quality of health care. Am J Public Health. 2003;93:1713–1719. doi: 10.2105/ajph.93.10.1713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Meghani SH, Brooks JM, Gipson-Jones T, et al. Patient-provider race-concordance: does it matter in improving minority patients' health outcomes? Ethn Health. 2009;14:107–130. doi: 10.1080/13557850802227031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Strumpf EC. Racial/ethnic disparities in primary care: the role of physician-patient concordance. Social Science Research Network. 2010 Working paper series. no. 1655959 < http://papers.ssrn.com/sol3/papers.cfm?abstract_id=1655959>.
- 21.McKinlay JB, Potter DA, Feldman HA. Non-medical influences on medical decision-making. Soc Sci Med. 1996;42:769–776. doi: 10.1016/0277-9536(95)00342-8. [DOI] [PubMed] [Google Scholar]
- 22.Levy DR. White doctors and black patients: influence of race on the doctor-patient relationship. Pediatrics. 1985;75:639–643. [PubMed] [Google Scholar]
- 23.Kaplan SH, Gandek B, Greenfield S, Rogers W, Ware JE. Patient and visit characteristics related to physicians' participatory decision-making style. Results from the Medical Outcomes Study. Med Care. 1995;33:1176–1187. doi: 10.1097/00005650-199512000-00002. [DOI] [PubMed] [Google Scholar]
- 24.Malat J. Social distance and patients' rating of healthcare providers. J Health Soc Behav. 2001;42:360–372. [PubMed] [Google Scholar]
- 25.van Wieringen JC, Harmsen JA, Bruijnzeels MA. Intercultural communication in general practice. Eur J Public Health. 2002;12:63–68. doi: 10.1093/eurpub/12.1.63. [DOI] [PubMed] [Google Scholar]
- 26.Agency for Healthcare Quality and Research. National Healthcare Disparities Report. Agency for Healthcare Quality and Research; Rockville: 2008. [Google Scholar]
- 27.Ogden CL, Carroll MD, Curtin LR, et al. Prevalence of overweight and obesity in the United States, 1999-2004. JAMA. 2006;295:1549–1555. doi: 10.1001/jama.295.13.1549. [DOI] [PubMed] [Google Scholar]
- 28.North American Association for the Study of Obesity (NAASO) and the National Heart Lung and Blood Institute. Clinical Guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults —The Evidence Report. National Institutes of Health. Obes Res. 1998;6(Suppl 2):51S–209S. [PubMed] [Google Scholar]
- 29.US Preventive Services Task Force. Screening for obesity in adults: recommendations and rationale. Ann Intern Med. 2003;139:930–932. doi: 10.7326/0003-4819-139-11-200312020-00012. [DOI] [PubMed] [Google Scholar]
- 30.National Center for Health Statistics. 2005 NAMCS Micro-data file documentation. 2006 < ftp://ftp.cdc.gov/pub/Health_Statistics/NCHS/Dataset_Documentation/NAMCS/doc05.pdf>.
- 31.Cherry DK, Woodwell DA, Rechtsteiner EA. Advance data from vital and health statistics no 387. National Center for Health Statistics; Hyattsville, MD: 2007. National Ambulatory Medical Care Survey: 2005 Summary. [PubMed] [Google Scholar]
- 32.Cherry DK, Hing E, Woodwell DA, Rechtsteiner EA. National Health Statistics Reports no 3. National Center for Health Statistics; Hyattsville, MD: 2008. National Ambulatory Medical Care Survey: 2006 summary. [PubMed] [Google Scholar]
- 33.National Center for Health Statistics. [Accessed 18 June 2010];2007 NAMCS micro-data file documentation. 2007 < ftp://ftp.cdc.gov/pub/Health_Statistics/NCHS/Dataset_Documentation/NAMCS/doc07.pdf>.
- 34.Kristeller JL, Hoerr RA. Physician attitudes toward managing obesity: differences among six specialty groups. Prev Med. 1997;26:542–549. doi: 10.1006/pmed.1997.0171. [DOI] [PubMed] [Google Scholar]
- 35.Bleich SN, Clark JM, Goodwin SM, Huizinga MM, Weiner JP. Variation in provider identification of obesity by individual- and neighborhood-level characteristics among an insured population. J Obes. 2010;2010:1–7. doi: 10.1155/2010/637829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Schmittdiel J, Grumbach K, Selby JV, Quesenberry CP., Jr Effect of physician and patient gender concordance on patient satisfaction and preventive care practices. J Gen Intern Med. 2000;15:761–769. doi: 10.1046/j.1525-1497.2000.91156.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.van Ryn M, Burgess D, Malat J, Griffin J. Physicians' perceptions of patients' social and behavioral characteristics and race disparities in treatment recommendations for men with coronary artery disease. Am J Public Health. 2006;96:351–357. doi: 10.2105/AJPH.2004.041806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Dorsey RR, Eberhardt MS, Ogden CL. Racial/ethnic differences in weight perception. Obesity (Silver Spring) 2009;17:790–795. doi: 10.1038/oby.2008.603. [DOI] [PubMed] [Google Scholar]
- 39.Bennett GG, Wolin KY. Satisfied or unaware? Racial differences in perceived weight status. Int J Behav Nutr Phys Act. 2006;3:40. doi: 10.1186/1479-5868-3-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kushner RF. Barriers to providing nutrition counseling by physicians: a survey of primary care practitioners. Prev Med. 1995;24:546–552. doi: 10.1006/pmed.1995.1087. [DOI] [PubMed] [Google Scholar]
- 41.Laws RA, Jayasinghe UW, Harris MF, et al. Community Health SNAP Project Team Explaining the variation in the management of lifestyle risk factors in primary health care: a multilevel cross sectional study. BMC Public Health. 2009;9:165. doi: 10.1186/1471-2458-9-165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Timmerman GM, Reifsnider E, Allan JD. Weight management practices among primary care providers. J Am Acad Nurse Pract. 2000;12:113–116. doi: 10.1111/j.1745-7599.2000.tb00289.x. [DOI] [PubMed] [Google Scholar]
- 43.Hoppé R, Ogden J. Practice nurses' beliefs about obesity and weight related interventions in primary care. Int J Obes Relat Metab Disord. 1997;21:141–146. doi: 10.1038/sj.ijo.0800379. [DOI] [PubMed] [Google Scholar]
- 44.Epstein L, Ogden J. A qualitative study of GPs' views of treating obesity. Br J Gen Pract. 2005;55:750–754. [PMC free article] [PubMed] [Google Scholar]
- 45.Hash RB, Munna RK, Vogel RL, Bason JJ. Does physician weight affect perception of health advice? Prev Med. 2003;36:41–44. doi: 10.1006/pmed.2002.1124. [DOI] [PubMed] [Google Scholar]
- 46.Price JH, Desmond SM, Krol RA, Snyder FF, O'Connell JK. Family practice physicians' beliefs, attitudes, and practices regarding obesity. Am J Prev Med. 1987;3:339–345. [PubMed] [Google Scholar]
- 47.Huizinga MM, Cooper LA, Bleich SN, Clark JM, Beach MC. Physician respect for patients with obesity. J Gen Intern Med. 2009;24:1236–1239. doi: 10.1007/s11606-009-1104-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Levy BT, Williamson PS. Patient perceptions and weight loss of obese adults. J Fam Pract. 1988;27:285–290. [PubMed] [Google Scholar]
- 49.Kant AK, Miner P. Physician advice about being overweight: association with self-reported weight loss, dietary, and physical activity behaviors of US adolescents in the National Health and Nutrition Examination Survey, 1999-2002. Pediatrics. 2007;119:e142–e147. doi: 10.1542/peds.2006-1116. [DOI] [PubMed] [Google Scholar]
- 50.Calfas KJ, Sallis JF, Oldenburg B, Ffrench M. Mediators of change in physical activity following an intervention in primary care: PACE. Prev Med. 1997;26:297–304. doi: 10.1006/pmed.1997.0141. [DOI] [PubMed] [Google Scholar]
- 51.Galuska DA, Will JC, Serdula MK, Ford ES. Are health care professionals advising obese patients to lose weight? JAMA. 1999;282:1576–1578. doi: 10.1001/jama.282.16.1576. [DOI] [PubMed] [Google Scholar]
- 52.Sciamanna CN, Tate DF, Lang W, Wing RR. Who reports receiving advice to lose weight? Results from a multistate survey. Arch Intern Med. 2000;160:2334–2339. doi: 10.1001/archinte.160.15.2334. [DOI] [PubMed] [Google Scholar]
- 53.Loureiro ML, Nayga RM., Jr Obesity, weight loss, and physician's advice. Soc Sci Med. 2006;62:2458–2468. doi: 10.1016/j.socscimed.2005.11.011. [DOI] [PubMed] [Google Scholar]
- 54.Huang J, Yu H, Marin E, et al. Physicians' weight loss counseling in two public hospital primary care clinics. Acad Med. 2004;79:156–161. doi: 10.1097/00001888-200402000-00012. [DOI] [PubMed] [Google Scholar]
- 55.Kreuter MW, Chheda SG, Bull FC. How does physician advice influence patient behavior? Evidence for a priming effect. Arch Fam Med. 2000;9:426–433. doi: 10.1001/archfami.9.5.426. [DOI] [PubMed] [Google Scholar]
- 56.Bissell P, May CR, Noyce PR. From compliance to concordance: barriers to accomplishing a re-framed model of health care interactions. Soc Sci Med. 2004;58:851–862. doi: 10.1016/s0277-9536(03)00259-4. [DOI] [PubMed] [Google Scholar]
- 57.Burgess DJ, Fu SS, van Ryn M. Why do providers contribute to disparities and what can be done about it? J Gen Intern Med. 2004;19:1154–1159. doi: 10.1111/j.1525-1497.2004.30227.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Street RL, Jr, O'Malley KJ, Cooper LA, Haidet P. Understanding concordance in patient–physician relationships: personal and ethnic dimensions of shared identity. Ann Fam Med. 2008;6:198–205. doi: 10.1370/afm.821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Saha S, Taggart SH, Komaromy M, Bindman AB. Do patients choose physicians of their own race? Health Aff (Millwood) 2000;19:76–83. doi: 10.1377/hlthaff.19.4.76. [DOI] [PubMed] [Google Scholar]
- 60.Smedley B, Stith A, Nelson A, editors. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. National Academy Press; Washington DC: 2002. [PubMed] [Google Scholar]
- 61.Franks P, Bertakis KD. Physician gender, patient gender, and primary care. J Womens Health (Larchmt) 2003;12:73–80. doi: 10.1089/154099903321154167. [DOI] [PubMed] [Google Scholar]
- 62.Stange KC, Zyzanski SJ, Smith TF, et al. How valid are medical records and patient questionnaires for physician profiling and health services research? A comparison with direct observation of patients visits. Med Care. 1998;36:851–867. doi: 10.1097/00005650-199806000-00009. [DOI] [PubMed] [Google Scholar]
- 63.Gilchrist VJ, Stange KC, Flocke SA, McCord G, Bourguet CC. A comparison of the National Ambulatory Medical Care Survey (NAMCS) measurement approach with direct observation of outpatient visits. Med Care. 2004;42:276–280. doi: 10.1097/01.mlr.0000114916.95639.af. [DOI] [PubMed] [Google Scholar]
- 64.Lee JS, Sheer JL, Lopez N, Rosenbaum S. Coverage of obesity treatment: a state-by-state analysis of Medicaid and state insurance laws. Public Health Rep. 2010;125:596–604. doi: 10.1177/003335491012500415. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.