Abstract
Objective
To describe parent perceptions of their child's hospital discharge and assess the relationship between these perceptions and hospital readmission.
Design
A prospective study of parents surveyed with questions adapted from the care transitions measure, an adult survey that assesses components of discharge care. Participant answers, scored on a 5-point Likert scale, were compared between children who did and did not experience a readmission using a Fisher's exact test and logistic regression that accounted for patient characteristics associated with increased readmission risk, including complex chronic condition and assistance with medical technology.
Setting
A tertiary-care children's hospital.
Participants: A total of 348 parents surveyed following their child's hospital discharge between March and October 2010.
Intervention
None.
Main Outcome Measure
Unplanned readmission within 30 days of discharge.
Results
There were 28 children (8.1%) who experienced a readmission. Children had a lower readmission rate (4.4 vs. 11.3%, P = 0.004) and lower adjusted readmission likelihood [odds ratio 0.2 (95% confidence interval 0.1, 0.6)] when their parents strongly agreed (n = 206) with the statement, ‘I felt that my child was healthy enough to leave the hospital’ from the index admission. Parent perceptions relating to care management responsibilities, medications, written discharge plan, warning signs and symptoms to watch for and primary care follow-up were not associated with readmission risk in multivariate analysis.
Conclusions
Parent perception of their child's health at discharge was associated with the risk of a subsequent, unplanned readmission. Addressing concerns with this perception prior to hospital discharge may help mitigate readmission risk in children.
Keywords: hospital discharge, readmission, care transition, quality of care, children
Background
It is important that hospitalized children are discharged safely and that their parents are prepared to leave the hospital with their child. Previous studies document the importance of discharge teaching, preparation and care coordination for families of hospitalized children, especially those with children with complex medical needs who have a high risk for readmission [1–8].
In the USA, the National Quality Forum (NQF) and Centers for Medicare and Medicaid Services (CMS) endorse measurement of the quality of hospital discharge care for adult patients with the care transitions measure [9–10]. The care transitions measure is a self-reported survey administered to patients after they leave the hospital. It measures the degree to which patients perceive their discharge care readiness, including medication use and self-management following discharge [11]. Care transitions measure scoring correlates with the success of hospital discharge and the need for readmission [12–15].
To our knowledge, there is no standardized assessment of discharge care for hospitalized children. In one prior study, care transitions measure scoring, when given to parents of children undergoing solid-organ transplantation, correlated with parent discharge readiness and the ability to cope with their child's health following discharge [16]. The relationship between a parent's perception of their child's discharge readiness and the likelihood of their child experiencing an unplanned readmission has not been assessed.
The roles of inpatient and outpatient care in preventing readmissions for children are currently under investigation. Some studies suggest that pediatric readmission may be an indicator of substandard care quality, whereas others do not [17–19]. To improve our understanding of the relationship of hospital discharge care and hospital readmission, the present study was conducted to (i) describe parent perceptions of their child's hospital discharge readiness and (ii) assess the correlation between those perceptions and the likelihood of readmission.
Methods
Study design, setting and patients
This is a prospective study of patients discharged from a freestanding children's hospital. The study was approved by the Children's Hospital Boston institutional review board. A 5% random sample of parents or legal guardians from a cohort of 11 910 hospitalized patients meeting the inclusion criteria who were discharged from the hospital every day from March to October 2010 were approached for study participation. The patients in the random sample had the same readmission rate, demographic, clinical and hospitalization characteristics as patients not selected for participation (data not shown) [20].
Patients who left the hospital against medical advice, who were transferred to another acute care facility at discharge or who died during their admission were not approached for interview [21]. Patients with malignancy were not approached because of their tendency to experience readmissions for scheduled treatment. Patients with medical and surgical admissions were included. Patients speaking all languages were included with the use of translation services for non-English speaking patients. Patients age ≥18 years admitted to the children's hospital were included because many have pediatric chronic health conditions that predispose them to experience readmission [22].
Parent perceptions of their child's hospital discharge
The items in the adult care transitions measure survey were used to measure perceptions of the pediatric hospital discharge [10, 13]. In the 6 months prior to participant enrollment, the adult care transitions measure item language was revised to permit the administration to parents of pediatric patients (Table 1). During this time, we performed 40 in-person cognitive interviews with parents of recently discharged children to revise the language of the items, to strike items that parents consistently did not understand how to answer and to add new items with discharge care constructs that the parents felt were important to assess. Item answers were contained within a 5-point Likert-scale (1 = strongly disagree, 2 = disagree, 3 = neither agree nor disagree, 4 = agree and 5 = strongly agree).
Table 1.
Adaptation of the adult care transitions measure survey items for use in children
| Pediatric care transition measure survey itemsa | Adult care transition measure survey items |
|---|---|
| 1. I had all the information I needed to be able to take care of my child when we left the hospital. | 1. When I left the hospital, I had all the information I needed to be able to take care of myself. |
| 2. I had a good understanding of what would make my child's health condition better or worse when we left the hospital. | 2. When I left the hospital, I had a good understanding of my health condition and what makes it better or worse. |
| 3. I understood which warning signs and symptoms meant I should call one or more of my child's healthcare providers right away when we left the hospital. | 3. When I left the hospital, I clearly understood the warning signs and symptoms I should watch for to monitor my health condition. |
| 4. I had a good understanding of the things that I was responsible for in managing my child's health when we left the hospital. | 4. When I left the hospital, I had a good understanding of the things I was responsible for in managing my health. |
| 5. I understood how to manage my child's health over the weeks after going home when we left the hospital. | 5. When I left the hospital, I clearly understood how to manage my health. |
| 6. I understood who to call if I had questions or concerns about my child's health at home when we left the hospital. 7. I felt comfortable contacting my child's primary care physician for help if my child's health worsened after leaving the hospital. 8. I had the transportation I needed to take my child to health appointments scheduled for after we left the hospital. |
6. When I left the hospital, I was confident that I knew what to do to manage my health. 7. When I left the hospital, I was confident I could actually do the things I needed to do to take care of my health. 8. Before I left the hospital, the staff and I agreed about clear health goals for me and how these would be reached. |
| 9. I felt that my child was healthy enough to leave the hospital. | |
| 10. I had an easily understood written plan that described how my child's healthcare needs were going to be met when we left the hospital. | 9. When I left the hospital, I had a readable and easily understood written plan that described how all of my healthcare needs were going to be met. |
| 11. I had an easily understood written list of the appointments or tests my child needed to complete within the weeks after going home when we left the hospital. | 10. When I left the hospital, I had a readable and easily understood written list of the appointments or tests I needed to complete within the next several weeks. |
| 12. The hospital staff took my preferences into account in deciding where my child's healthcare needs would be provided once we left the hospital. | 11. The hospital staff took my preferences and those of my family or caregiver into account in deciding where my healthcare needs would be met when I left the hospital. |
| 13. The hospital staff took my preferences into account in deciding how my child's healthcare needs would be met once we left the hospital. | 12. The hospital staff took my preferences and those of my family or caregiver into account in deciding what my healthcare needs would be when I left the hospital. |
| 14. I had a good understanding as to why my child had to take each of his/her medications when we left the hospital. | 13. When I left the hospital, I clearly understood the purpose for taking each of my medications. |
| 15. I had a good understanding of how often and how much of each medication my child needed to take when we left the hospital. | 14. When I left the hospital, I clearly understood how to take each of my medications, including how much I should take and when. |
| 16. I had a good understanding of the major side effects of each of my child's medications when we left the hospital. | 15. When I left the hospital, I clearly understood the possible side effects of each of my medications. |
| 17. I had a good understanding of how to use my child's medical equipment and supplies when we left the hospital. |
aWe performed 40 in-person cognitive interviews with parents of recently discharged children to revise the language of the adult Care Transition items, to strike items that parents consistently did not understand how to answer and to add new items with discharge care constructs that the parents felt were important to assess.
The same interviewer (W.K.) surveyed parents by phone to capture perceptions of their child's hospital discharge. This interviewer was not involved in the care of enrolled patients. Consistent with methods of prior care transitions measure studies, we approached parents to complete the survey starting 48 h after their child's hospitals discharge with multiple daily attempts to contact the parents. We considered surveying parents while their child was still in the hospital. We decided not to use that method to avoid the possibility of biasing inpatient care delivery and readmission risk (e.g. while in the hospital, a parent may have expressed that their child was not healthy enough to be discharged in the survey and so the child remained in a hospital for a few more days and the child's readmission risk declined). The phone interview script was strictly followed to avoid coercion or leading the interviewee's responses.
Main outcome measure
The main outcome measure was unplanned readmission within 30 days. We identified and excluded readmissions for a planned surgical operation by reviewing the physician's admitting note for each readmission. Planned operations were those that were scheduled in advance for a non-emergent medical issue. Thirty-day readmissions are publically reported by CMS, endorsed by NQF and have been used in prior adult care transitions measure studies [9, 12–15].
Patient clinical and demographic characteristics
We analyzed pediatric chronic diagnoses, obtained from the patient's inpatient medical record, which may influence a patient's discharge care and readmission likelihood, using Feudtner's complex chronic condition (CCC) groupings [23, 24]. CCCs represent defined International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM) code groupings of pediatric respiratory, renal, gastrointestinal, metabolic, hematologic, congenital or genetic defect, malignancy, cardiovascular and neuromuscular diagnoses that (i) are expected to last longer than 12 months and (ii) involve either several different organ systems or one organ system severely enough to require specialty pediatric care and hospitalization. We also assessed the use of durable medical equipment (e.g. gastrostomy tube, oxygen) following discharge because children using it have an increased risk of readmission [24, 25]. We also assessed the patients' demographic characteristics of age, gender, race/ethnicity (Hispanic, non-Hispanic black, non-Hispanic white and other) and insurance type (public vs. non-public). Age was analyzed continuously and in categories that have correlated with readmission risk in prior studies [22, 23]. Parent demographic characteristics were not assessed.
Index hospitalization characteristics
We also examined the length of hospital stay and discharge disposition [discharged to home, to home with home nursing or to another healthcare facility (e.g. rehabilitation hospital, long-term care facility)] of each patient's index hospitalization.
Statistical analysis
In bivariate analyses, we used Fisher's exact tests to assess whether the care transitions measure answers differed between readmitted and non-readmitted patients. We analyzed the survey answers categorically; we compared the answer ‘strongly agree’ vs. the remaining answers because some hospitals might set ‘strongly agree’ as the optimal target for all patients. In clinical practice, it may be difficult to use the answers to the survey items in the care transition measure as ‘predictors’ of a subsequent readmission. However, in a post hoc multivariate analysis, we used logistic regression to assess which survey items remained significantly associated with readmission in the setting of patient characteristics, such as a CCC, that are known to influence readmission risk. Covariates with a P value of ≤ 0.1 in bivariate analyses were entered in the models and maintained if their P value remained ≤ 0.1. P values of ≤0.05 were considered statistically significant. Stata (version 11) was used for all analyses.
Results
We approached 613 parents of discharged children. Three hundred and forty-eight (57%) of them completed the survey a median of 5 days (interquartile range 4–7 days) from the discharge of their child's prior admission. No patients who we succeeded in contacting refused the interview. There was no situation where multiple patients from the same family were surveyed. Twenty-eight children (8.1%) experienced an unplanned 30-day readmission. All parents of readmitted children were surveyed prior to their child's readmission. No child enrolled in the study experienced multiple readmissions during the study period. Twelve readmissions (42.9%) were for the exact same medical problem or for a problem within the same organ system as the index admission. Ten readmissions (35.7%) were for post-operative medical problems following an index admission for a surgical operation or procedure. Six readmissions (21.4%) were for a non-surgical problem within a different organ system than the index admission.
Patient demographic, clinical and hospitalization characteristics
The mean age of participating children was 8.5 years [standard deviation (SD) 7.5]; 69.0% were non-Hispanic white, 53.4% were male and 20.1% used public insurance. The demographic characteristics did not significantly differ between readmitted and non-readmitted children (Table 2).
Table 2.
Demographic, clinical and hospital characteristics of patients readmitted and not readmitted within 30 days
| Characteristic | Readmitted within 30 days of an index hospital discharge |
P value* | |
|---|---|---|---|
| Yes (n = 28) | No (n = 320) | ||
| Patient demographic characteristics | |||
| Mean age (standard deviation) | 8.1 (10.4) | 8.6 (7.3) | 0.77 |
| Age in categories (%) | |||
| Neonate (0–30 days) | 0.0 | 0.9 | 0.27 |
| Infancy (31–365 days) | 17.9 | 15.6 | |
| Early childhood (1–4 years) | 42.9 | 24.1 | |
| Late childhood (5–12 years) | 14.3 | 30.0 | |
| Adolescence (13–18 years) | 17.9 | 21.6 | |
| Adulthood (>18 years) | 7.1 | 7.8 | |
| Male (%) | 71.4 | 53.4 | 0.08 |
| Race/ethnicity (%) | |||
| Non-Hispanic White | 64.3 | 69.4 | 0.17 |
| Non-Hispanic Black | 14.3 | 8.1 | |
| Hispanic | 17.9 | 8.8 | |
| Other | 3.6 | 5.6 | |
| Missing | 0.0 | 8.1 | |
| Primary insurance: public (%) | 28.6 | 19.4 | 0.32 |
| Patient clinical characteristics | |||
| Mean no. of CCCs (standard deviation) | 0.4 (0.7) | 0.3 (0.6) | 0.36 |
| Any CCCa (%) | 35.7 | 25.3 | 0.26 |
| Neuromuscular | 14.3 | 6.3 | 0.12 |
| Cardiovascular | 7.1 | 10.0 | 1.0 |
| Other congenital or genetic defect | 7.1 | 5.9 | 0.68 |
| Respiratory | 3.6 | 2.8 | 0.57 |
| Gastrointestinal | 3.6 | 2.2 | 0.49 |
| Renal | 3.6 | 1.9 | 0.45 |
| Metabolic | 3.6 | 0.6 | 0.22 |
| Hematologic or immunologic | 0.0 | 2.2 | 1.0 |
| Use of durable medical equipment (%) | 51.9 | 30.2 | 0.03 |
| Index hospitalization characteristics | |||
| Mean length of hospital stay in days (standard deviation) | 4.6 (6.0) | 2.2 (3.8) | 0.002 |
| Discharge disposition (%) | |||
| Home | 82.1 | 94.7 | 0.02 |
| Home with home health care | 17.9 | 5.3 | |
aPatients may have more than one complex chronic condition.
*P values were obtained from Fisher's exact tests and t-test for categorical and continuous data, respectively.
Ninety-one (26.2%) of children had at ≥1 CCC and 109 (31.9%) used durable medical equipment. Children experiencing readmission had a higher percentage of durable medical equipment use (51.9 vs. 30.2%, P = 0.03) (Table 2). Children experiencing readmission had a longer length of stay during their index admission than children without a readmission [mean 4.6 days (SD 6.0) vs. 2.2 days (SD 3.8), P = 0.007]. A higher percentage of children experiencing readmission were discharged to home with home nursing services (17.9 vs. 5.3%, P = 0.02) (Table 2).
Parent perceptions of their child's hospital discharge
In general, the vast majority of parents had favorable perceptions of their child's hospital discharge (Supplementary data, Appendix Table). For example, 95.1% of parents felt they had all the information they needed to take of their child when they left the hospital, 97.9% understood which warning signs and symptoms meant they should call their child's healthcare providers right away and 100% had a good understanding of why their child had to take each of his/her medications.
Bivariate analysis of parent perceptions of their child's hospital discharge and readmission likelihood
Three of the survey items were significantly associated (P≤0.05) with readmission likelihood in bivariate analysis. These items are described below.
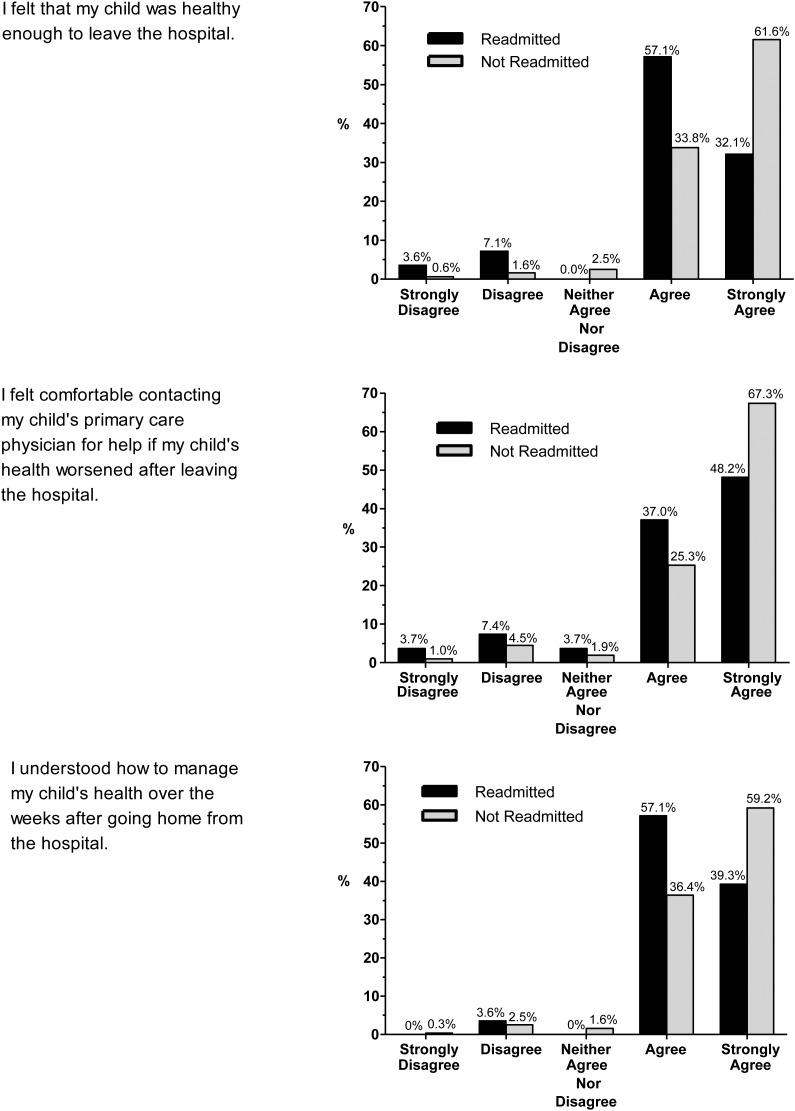
Child health at discharge
Parents of readmitted children were less likely to strongly agree with the statement, ‘I felt that my child was healthy enough to leave the hospital’ (32.1 vs. 61.7%) (Fig. 1). The 30-day readmission rate for children whose parents did not strongly agree with this perception (n = 206) was significantly higher than children whose parents strongly agreed with it [11.3 vs. 4.4%; odds ratio (OR) of readmission = 3.4 (95% confidence interval (CI) 1.5–7.7)].
Figure 1.
Parent perceptions of their child's health and discharge planning that differed between patients readmitted and not readmitted within 30 days. This figure presents the answers to the three parent perceptions that were significantly (P < 0.05) different between children readmitted and not readmitted. The percent distribution of answers on the 5-point Likert scale is shown for each perception.
Comfort contacting the child's primary care physician
Parents of readmitted children were less likely to strongly agree with the statement, ‘I felt comfortable contacting my child's primary care physician for help if my child's health worsened after leaving the hospital’ than parents of children who were not readmitted (48.1 vs. 67.3%) (Fig. 1). The 30-day readmission rate for children whose parents did not strongly agree with this perception (n = 223) was significantly higher than those whose parents strongly agreed with it [12.1 vs. 5.8%; OR 2.2 (95% CI 1.0–4.9)].
Understanding how to manage the child's health
Parents of readmitted children were less likely to strongly agree with the statement, ‘I understood how to manage my child's health over the weeks after going home’ than parents of those who were not readmitted (39.3 vs. 59.2%) (Fig. 1). The 30-day readmission rate for children whose parents did not strongly agree with this perception (n = 198) was significantly higher than those whose parents who strongly agreed with it [11.6 vs. 5.6%; OR 2.2 (95% CI 1.0–4.9)].
Multivariate analysis of parent perceptions of their child's hospital discharge and readmission likelihood
In multivariate analysis, parent perceptions of their child's health at hospital discharge was the only survey item that remained significantly associated with the likelihood of 30-day unplanned readmission after controlling for patient demographic, clinical and hospitalization characteristics (Table 3). The adjusted OR of readmission for children whose parents strongly agreed with that statement was 0.2 (95% CI 0.1, 0.6). Parents' comfort contacting their child's primary care physician and their understanding of how to manage their child's health following discharge were not associated (P > 1.0) with readmission likelihood in multivariate analysis.
Table 3.
Multivariate analysis of the likelihood of 30-day readmission
| Covariate | 30-day unplanned readmission |
P value | |
|---|---|---|---|
| OR | 95% CI | ||
| Parent perception of their child's hospital discharge | |||
| ‘I felt that my child was healthy enough to leave the hospital’. | 0.2a | 0.1, 0.6 | 0.002 |
| ‘I felt comfortable contacting my child's primary care physician for help if my child's health worsened after leaving the hospital’. | 0.8a | 0.3, 2.2 | 0.6 |
| ‘I understood how to manage my child's health over the weeks after going home’. | 0.7a | 0.1, 4.1 | 0.7 |
| Child demographic characteristics | |||
| Male gender | 2.5 | 1.0, 6.5 | 0.06 |
| Age at admission (in years) | 1.0b | 1.0, 1.1 | 0.71 |
| Private vs. public insurance | 1.4 | 0.4, 4.7 | 0.56 |
| Hispanic | 4.1c | 0.7, 22.5 | 0.1 |
| Non-Hispanic Black | 2.7c | 0.6, 11.2 | 0.4 |
| Other race/ethnicity | 0.5c | 0.1, 2.7 | 0.6 |
| Child clinical characteristics | |||
| Use of home nursing | 2.6 | 0.9, 7.4 | 0.07 |
| Use of durable medical equipment | 1.5 | 0.5, 4.2 | 0.47 |
| Complex chronic condition | 1.4 | 0.5, 3.9 | 0.54 |
| Child hospitalization characteristics | |||
| Length of stay of index hospitalization (in days) | 1.2 | 1.0, 1.3 | 0.008 |
| Discharge to home | 0.6 | 0.1, 3.4 | 0.54 |
aShown are the odds of admission for children whose parents strongly agreed with the perception.
bShown are the odds of admission for a 1-year increase in age at admission.
cNon-Hispanic white is the reference group.
Discussion
This study suggests that parents' perception of their child's hospital discharge is associated with the likelihood of unplanned 30-day readmission. In bivariate analysis, readmission likelihood was associated with parent perceptions of their child's health at hospital discharge, their comfort contacting their child's primary care physician for help and their understanding of how to manage their child's health. Parent perception of their child's health was the only perception that remained significantly associated with readmission after controlling for other patient characteristics that influenced readmission risk.
The perceptions of hospital discharge that are associated with readmission may be different for children than adults. In adult studies, the care transitions measure perceptions that correlate the most with readmission are patients' understanding of their medications, health management and healthcare needs following discharge [26]. Although parent perceptions of these discharge attributes were not associated with child readmission risk in multivariate analysis, the importance of the attributes should not be discounted. The generalizability of our results is limited by the small, single tertiary-care center design with nearly uniformly positive perceptions of hospitals discharge. The discharge process, and parent perceptions of it, may be different at other hospitals. A larger, more adequately powered, multi-institutional study is needed to determine whether the components of discharge care that influence the need for readmission are truly different for children than adults.
In the present study, parent perception of their child's health at discharge was the most strongly correlated with readmission risk. Most inpatient clinicians probably feel that they adequately address the health of hospitalized children prior to discharge. Yet, some parents in our study had concerns about their child's health at discharge even through they had already been discharged home. It is unknown whether some parents had concerns about their child's health prior to hospital discharge and if they expressed their concerns to the inpatient providers. Disparate opinions of discharge readiness between adult patients and their inpatient providers have been reported [27, 28].
Answering the survey could have prompted some parents to realize that their child, in retrospect, was actually not healthy enough to be discharged. These parents may not have had this perception during or before hospital discharge [29]. Although not assessed in this study, some parents may have assessed their child's health differently prior to discharge because they were rushed or eager to leave the hospital [30]. Some providers may have had difficulty assessing the health of children with complex illness at discharge because these children might not be able to return to a ‘normal’ baseline state of health [31, 32].
There was a small percentage of parents with unfavorable perceptions of their child's hospital discharge. In a post hoc analysis, we analyzed the readmission likelihood for children of these parents. Children whose parents disagreed or strongly disagreed with the statement, ‘I felt that my child was healthy enough to leave the hospital’ had an adjusted OR of readmission of 4.7 (95% CI 1.0, 21.9). Although it could be difficult to analyze the care transition measure as a predictor of readmission, some hospitals may prefer to target and minimize unfavorable perceptions of their hospital discharge before their patients leave the hospital.
This study has several limitations. Although the readmission rate and patient characteristics of the children enrolled into the study were not different from the non-responders or the children not approached for enrollment (data not shown), the discharge experience of the non-responders or the non-enrollees could have been different. Our recruitment period, March–October 2010, did not include the full winter respiratory illness season when readmission risk and parent perceptions of their child's hospital discharge may be different. Readmission rates may be different in other types of hospitals, such as non-children's hospitals, that care for fewer children with complex, chronic illnesses. We were unable to measure readmissions to a different hospital. We did not assess parent attributes (e.g. age, gender and education) that could have influenced their hospital discharge perceptions or their child's readmission risk.
Despite these limitations, this study suggests that parents' perception of their child's hospital discharge is associated with readmission likelihood. The NQF has endorsed a set of 11 distinct components designed to prepare patients for discharge [33]. The use of the survey items in the present study, or similar ones adapted from the adult care transitions measure, may be helpful to standardize this assessment in children prior to hospital discharge and to help identify which children are at risk for readmission. Although assessment of a child's health may be considered an existing, standard component of discharge care, we must ensure that this assessment is done well. All families must be presented with an equal opportunity to voice their perceptions of their child's health and, if necessary, address concerns with that perception prior to hospital discharge. Family involvement in initiatives to improve pediatric discharge care delivery will assure that the process is responsive to family needs and that it reaches maximum effectiveness to ensure successful care transitions for children.
Supplementary material
Supplementary material is available at INTQHC Journal online.
Funding
This work was supported by the Children's Hospital Integrated Care Organization (CHICO). Dr. Berry was supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development career development award K23 HD058092.
Supplementary Material
References
- 1.Affleck G, Tennen H, Rowe J, et al. Effects of formal support on mothers' adaptation to the hospital-to-home transition of high-risk infants: the benefits and costs of helping. Child Dev. 1989;60:488–501. doi: 10.1111/j.1467-8624.1989.tb02730.x. doi:10.2307/1130993. [DOI] [PubMed] [Google Scholar]
- 2.Kenner C, Lott JW. Parent transition after discharge from the NICU. Neonatal Netw. 1990;9:31–7. [PubMed] [Google Scholar]
- 3.Sheikh L, O'Brien M, McCluskey-Fawcett K. Parent preparation for the NICU-to-home transition: staff and parent perceptions. Child Health Care. 1993;22:227–39. doi: 10.1207/s15326888chc2203_5. doi:10.1207/s15326888chc2203_5. [DOI] [PubMed] [Google Scholar]
- 4.Smith VC, Young S, Pursley DM, et al. Are families prepared for discharge from the NICU? J Perinatol. 2009;29:623–9. doi: 10.1038/jp.2009.58. doi:10.1038/jp.2009.58. [DOI] [PubMed] [Google Scholar]
- 5.Sneath N. Discharge teaching in the NICU: are parents prepared? An integrative review of parents' perceptions. Neonatal Netw. 2009;28:237–46. doi: 10.1891/0730-0832.28.4.237. doi:10.1891/0730-0832.28.4.237. [DOI] [PubMed] [Google Scholar]
- 6.Weiss M, Johnson NL, Malin S, et al. Readiness for discharge in parents of hospitalized children. J Pediatr Nurs. 2008;23:282–95. doi: 10.1016/j.pedn.2007.10.005. doi:10.1016/j.pedn.2007.10.005. [DOI] [PubMed] [Google Scholar]
- 7.Klitzner TS, Rabbitt LA, Chang RK. Benefits of care coordination for children with complex disease: a pilot medical home project in a resident teaching clinic. J Pediatr. 2010;156:1006–10. doi: 10.1016/j.jpeds.2009.12.012. doi:10.1016/j.jpeds.2009.12.012. [DOI] [PubMed] [Google Scholar]
- 8.Wong DL. Transition from hospital to home for children with complex medical care. J Pediatr Oncol Nurs. 1991;8:3–9. doi: 10.1177/104345429100800102. doi:10.1177/104345429100800102. [DOI] [PubMed] [Google Scholar]
- 9.National Quality Forum. 3-Item care transition measure (CTM-3) http://www.qualityforum.org/MeasureDetails.aspx?Actid=0&SubmissionId=466#k=Care+Transitions. (4 April 2012, date last accessed)
- 10.Coleman EA. The care transitions program http://www.caretransitions.org/
- 11.Department of Health and Human Services. Improving quality of care for medicare patients: accountable care organizations. 2012. http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/sharedsavingsprogram/Downloads/ACO_Quality_Factsheet_ICN907407.pdf. (3 August 2013, date last accessed)
- 12.Coleman EA, Parry C, Chalmers S, et al. The care transitions intervention: results of a randomized controlled trial. Arch Intern Med. 2006;166:1822–8. doi: 10.1001/archinte.166.17.1822. doi:10.1001/archinte.166.17.1822. [DOI] [PubMed] [Google Scholar]
- 13.Coleman EA, Smith JD, Frank JC, et al. Development and testing of a measure designed to assess the quality of care transitions. Int J Integr Care. 2002;2:e02. doi: 10.5334/ijic.60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Coleman EA, Smith JD, Frank JC, et al. Preparing patients and caregivers to participate in care delivered across settings: the Care Transitions Intervention. J Am Geriatr Soc. 2004;52:1817–25. doi: 10.1111/j.1532-5415.2004.52504.x. doi:10.1111/j.1532-5415.2004.52504.x. [DOI] [PubMed] [Google Scholar]
- 15.Weiss M, Yakusheva O, Bobay K. Nurse and patient perceptions of discharge readiness in relation to postdischarge utilization. Med Care. 0000;48:482–6. doi: 10.1097/MLR.0b013e3181d5feae. doi:10.1097/MLR.0b013e3181d5feae. [DOI] [PubMed] [Google Scholar]
- 16.Lerret SM, Weiss ME. How ready are they? Parents of pediatric solid organ transplant recipients and the transition from hospital to home following transplant. Pediatr Transplant. 2011;15:606–16. doi: 10.1111/j.1399-3046.2011.01536.x. [DOI] [PubMed] [Google Scholar]
- 17.Sobota A, Graham DA, Neufeld EJ, et al. Thirty-day readmission rates following hospitalization for pediatric sickle cell crisis at freestanding children's hospitals: risk factors and hospital variation. Pediatr Blood Cancer. 2012;58:61–5. doi: 10.1002/pbc.23221. doi:10.1002/pbc.23221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Feudtner C, Pati S, Goodman DM, et al. State-level child health system performance and the likelihood of readmission to children's hospitals. J Pediatr. 2010;157:98–102 e1. doi: 10.1016/j.jpeds.2010.01.049. doi:10.1016/j.jpeds.2010.01.049. [DOI] [PubMed] [Google Scholar]
- 19.Morse RB, Hall M, Fieldston ES, et al. Hospital-level compliance with asthma care quality measures at children's hospitals and subsequent asthma-related outcomes. JAMA. 2011;306:1454–60. doi: 10.1001/jama.2011.1385. doi:10.1001/jama.2011.1385. [DOI] [PubMed] [Google Scholar]
- 20.Berry JG, Hall M, Hall DE, et al. Inpatient growth and resource use in 28 children's hospitals: a longitudinal, multi-institutional study. J Pediatr. 2013;167:170–77. doi: 10.1001/jamapediatrics.2013.432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Centers for Medicare & Medicaid Services. Medicare Hospital Quality Chartbook. Yale New Haven Health System Corporation Center for Outcomes Research and Evaluation. 2010.
- 22.Berry JG, Hall DE, Kuo DZ, et al. Hospital utilization and characteristics of patients experiencing recurrent readmissions within children's hospitals. JAMA. 2011;305:682–90. doi: 10.1001/jama.2011.122. doi:10.1001/jama.2011.122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Feudtner C, Levin JE, Srivastava R, et al. How well can hospital readmission be predicted in a cohort of hospitalized children? A retrospective, multicenter study. Pediatrics. 2009;123:286–93. doi: 10.1542/peds.2007-3395. doi:10.1542/peds.2007-3395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Berry JG, Hall DE, Kuo DZ, et al. Hospital utilization and characteristics of patients experiencing recurrent readmissions within children's hospitals. JAMA. 2011;305:682–90. doi: 10.1001/jama.2011.122. doi:10.1001/jama.2011.122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Berry JG, Graham DA, Graham RJ, et al. Predictors of clinical outcomes and hospital resource use of children after tracheotomy. Pediatrics. 2009;124:563–72. doi: 10.1542/peds.2008-3491. doi:10.1542/peds.2008-3491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Parry C, Mahoney E, Chalmers SA, et al. Assessing the quality of transitional care: further applications of the care transitions measure. Med Care. 2008;46:317–22. doi: 10.1097/MLR.0b013e3181589bdc. doi:10.1097/MLR.0b013e3181589bdc. [DOI] [PubMed] [Google Scholar]
- 27.Reiley P, Pike A, Phipps M, et al. Learning from patients: a discharge planning improvement project. Jt Comm J Qual Improv. 1996;22:311–22. doi: 10.1016/s1070-3241(16)30235-8. [DOI] [PubMed] [Google Scholar]
- 28.Bernstein HH, Spino C, Finch S, et al. Decision-making for postpartum discharge of 4300 mothers and their healthy infants: the Life Around Newborn Discharge study. Pediatrics. 2007;120:e391–400. doi: 10.1542/peds.2006-3389. doi:10.1542/peds.2006-3389. [DOI] [PubMed] [Google Scholar]
- 29.Bernstein HH, Spino C, Baker A, et al. Postpartum discharge: do varying perceptions of readiness impact health outcomes? Ambul Pediatr. 2002;2:388–95. doi: 10.1367/1539-4409(2002)002<0388:pddvpo>2.0.co;2. doi:10.1367/1539-4409(2002)002<0388:PDDVPO>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 30.Jack BW. Project RED: reengineering the hospital discharge process. Slide Presentation from the AHRQ 2009 Annual Conference (Text Version); Rockville, MD: Agency for Healthcare Research and Quality; 2009. http://www.ahrq.gov/about/annualconf09/jack.htm. cited 2011] (29 March 2011, date last accessed. [Google Scholar]
- 31.Iezzoni LI. Going beyond disease to address disability. N Engl J Med. 2006;355:976–9. doi: 10.1056/NEJMp068093. doi:10.1056/NEJMp068093. [DOI] [PubMed] [Google Scholar]
- 32.Thyen U, Kuhlthau K, Perrin JM. Employment, child care, and mental health of mothers caring for children assisted by technology. Pediatrics. 1999;103:1235–42. doi: 10.1542/peds.103.6.1235. doi:10.1542/peds.103.6.1235. [DOI] [PubMed] [Google Scholar]
- 33.Jack B, Greenwald J, Forsythe S, et al. Developing the tools to administer a comprehensive hospital discharge program: the ReEngineered Discharge (RED) Program. Agency for Healthcare Research and Quality. 2008. [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.