Abstract
Although healthcare quality and patient safety have longstanding international attention, the target of reducing diagnostic errors has only recently gained prominence, even though numerous patients, families and professional caregivers have suffered from diagnostic mishaps for a long time. Similarly, patients have always been involved in their own care to some extent, but only recently have patients sought more opportunities for engagement and participation in healthcare improvements. This paper brings these two promising trends together, analysing strategies for patient involvement in reducing diagnostic errors in an individual's own care, in improving the healthcare delivery system's diagnostic safety, and in contributing to research and policy development on diagnosis-related issues.
Keywords: Patient safety, Diagnostic errors, Patient-centred care, Patient education, Communication
Introduction
Patient involvement in healthcare decisions is increasingly and internationally recognised as important for matching care to patient preferences and for improving the safety and quality of care.1–6 While evidence demonstrates beneficial effects of patient involvement on various processes and outcomes of care,7 8 few studies have addressed patient-targeted interventions during diagnosis to reduce error.9 10 Since diagnosis sets the stage for treatment, this oversight seems unusual. Additionally, diagnostic errors (not getting the right diagnosis in a timely fashion) commonly occur with dire human and economic consequences.11–14 Not surprisingly, three in five Americans (63%) are very or extremely concerned about diagnostic errors.15 Diagnostic error is particularly salient in stories seen through patient and family members’ eyes.16–20
Based on disease-specific studies, causes of diagnostic misadventures include problems that patients could potentially mitigate under some circumstances, but certainly not all. For example, in a retrospective study of patients who experienced delays in diagnosis for colorectal cancer, about one-third experienced an average of 5.3 diagnostic process breakdowns, including missed appointments for diagnostic tests without apparent provider awareness.21 Among 587 patients diagnosed with lung cancer, patients with missed opportunities experienced a significantly longer median time to diagnosis than controls (132 vs 19 days, respectively; p<0.001).22 Patient non-adherence to physician recommendations was present in 44% of patients with missed opportunities for diagnosis.22
Patient involvement in improving diagnostic safety is conceivable at multiple levels: one's own diagnostic processes and outcomes; the diagnostic delivery system; and research and policy related to diagnostic safety.23 This paper aims to synthesise background regarding patient involvement in the diagnostic process for each of these three levels, and suggests priorities for future efforts. To inform our synthesis, we reviewed international initiatives related to patient involvement in patient safety broadly, and conducted targeted literature searches in PubMed and PyschInfo using the basic logic: (‘patient involvement’ or ‘patient engagement’) and (‘patient safety’ or ‘diagnostic error’ or ‘diagnostic delay’) with variations to make the strategy more inclusive (eg, ‘involvement of patients’, ‘consumer’, ‘client’). We also drew substantially from five patient-centred sessions at the 2012 Diagnostic Errors in Medicine Conference that were designed to crystallise the experiences of patient and family representatives into lessons about potential patient involvement to reduce diagnostic errors.24 Finally, drawing on this synthesis and considering the unique aspects of diagnosis relative to treatment, we propose a framework for research design to evaluate personal and sociological factors associated with more or less involvement by patients during the diagnostic stage of care.
Unique aspects of the diagnostic stage of care
Diagnosis is the trouble-shooting stage of care that arises in response to symptoms of a problem or routine screening, while treatment involves formulating and implementing the care plan, after problem identification. Although distinction between the diagnostic stage and treatment stage blurs in cases of empirical treatment, the medical profession (and society more broadly) uses the two categories—diagnosis and treatment—because they differ conceptually and practically.
Most literature about patient involvement focuses on treatment for those already diagnosed with a particular condition. What makes the diagnosis stage and the possibility of error different compared with the treatment stage? How are these differences active for patients and providers? What are the implications for applying and adapting current approaches to patient involvement?23 25 Based on evolving input from the diagnostic error community, we have developed an initial list of relatively unique qualities of the diagnostic stage relevant to patient involvement in error prevention:
Role of reasoning: those interested in diagnostic error have concentrated on understanding the reasoning process of the diagnostician (eg, Systems 1 and Systems 2 typology of intuitive vs deliberate thinking), and the potential failure points due to cognitive heuristics and biases.26 27 To the extent that patients are involved in diagnosis, they also could be prone to the same biases.
Avoidance of uncertainty: people often feel distress under conditions of uncertainty, with anxiety decreasing after diagnosis.28 Knowledge asymmetries between patient and doctor foster collusion that the diagnosis is right once made, instead of just a working diagnosis.
Inadequate feedback dynamic: significant delays in seeing problems with diagnosis create challenges for a system of feedback and learning about breakdowns, especially for patients encountering numerous doctors and disconnected care sites during the diagnostic process.
Physician centrality and resultant deference by others: nurses, technicians and others who ‘touch’ the patient may see signs of deterioration or patterns that are diagnostic, but they have been socialised and legally required to operate within ‘scope of practice’ which typically excludes diagnosis. Therefore, they may not easily speak up about problems with diagnosis. Patients may follow suit.
Patient inexperience with the diagnostic process: while patients have expertise in their own experience of symptoms, they typically have minimal knowledge about their diagnostic journey to an unknown destination. The patient does not necessarily know what information is valuable for diagnosis, or when to be concerned that diagnosis is off track.
The role of the patient: improving their own diagnosis
Barriers that patients face
While each patient and situation has unique aspects, patients often find barriers to productive involvement in their diagnostic journey, in cases when involvement is feasible. A persistent challenge facing many patients is suboptimal communication with their physicians and, related to this, the ‘(im)balance of power’ between physicians and patients. Despite consensus about the importance of patient autonomy—and, in turn, the resulting efforts to enhance physician–patient communication, shared decision making, and patient-centred care—evidence suggests specific hurdles. In one recent qualitative study, focus groups of primary care patients described hierarchical relationships with physicians, characterised by less-than-candid conversations and information exchanges.29 Patients described physicians as ‘authoritarian’. Moreover, even though participants in this study had above average levels of education, and had often sought information from outside sources, either to verify or to make sense of the discussion with their doctor, they were still reluctant to ask questions during their visits for fear of ‘second guessing’ or being perceived as difficult or contrary by their physicians. In other instances, patients and their families may face too many choices without enough physician guidance or coordination.
Related to communication and coordination is the barrier of health literacy. While patient understanding can be improved with clearer communication by providers (using plain language and avoiding medical jargon), communication alone does not provide for a full understanding of medical complexities.29 Assimilation of medical information (eg, possible conditions; rationale for diagnostic tests; insurance considerations) is a daunting task for patients, yet it is essential for becoming an informed consumer.
Several Diagnostic Errors in Medicine conference sessions resulted in a list of common challenges experienced by patients and families during delayed, missed and erroneous diagnoses, whether in the hospital or over the course of numerous outpatient visits (box 1).
Box 1. Challenges experienced by patients and their families during the diagnostic journey.
Patients and families sometimes:
Fear complaining, being seen as difficult
Feel powerless for many reasons (sick, scared, social status)
Do not always take own problems seriously enough
Are unsure about basics of the health system or involvement opportunities
Have difficulty dealing with inexperienced doctors who are trying to appear experienced in the problem
Are unsure how to get ‘the supervisor’ when issues are not resolved at frontline
Healthcare professionals sometimes:
Dismiss patients’ complaints and knowledge
Do not listen to concerns about serious symptoms or deteriorations
Give psychiatric, alcoholic or drug abuse diagnoses incorrectly during undiagnosed phase
Health systems sometimes exhibit:
Disjointed care: lack of coordination and teamwork
Breakdown in communication
Lack of information passed along to patient
Test results not reviewed closely or followed up
No disclosure or apology after diagnostic errors
Source: Synthesis generated by authors from the Diagnostic Errors In Medicine Conference24
What can patients do today to improve diagnosis?
Consistent with the trend of patients being more proactive and involved in their own healthcare,30 becoming a more knowledgeable consumer may reduce the risk of diagnostic error.31 Patients may become more informed through second opinions or the internet, but the vastness of the internet also poses a risk for information overload, contradictory information, misinformation from unreliable/unverified sources, or misuse of the information to self-diagnose instead of seeking professional help. Using these resources is becoming easier with the recent availability of clinical diagnosis support systems32–34; these systems give patients access to validated diagnosis search algorithms that dramatically outperform non-specific ‘Google’-based searches.34 35
Improving communication is another intervention target to improve diagnosis. New communication strategies focus on healthcare providers and patients/families. For example, the Speak Up programme, promoted by the Joint Commission, invites bidirectional discussion, welcomes questions, and empowers everyone involved in patient care to challenge assumptions or report questionable decisions without reprimand.36
These efforts focus largely on reducing medical errors in managing and treating health problems, but some of the same principles can be applied to improving diagnosis. The Diagnostic Errors in Medicine conference participants expanded and embellished Graber's strategies whereby the patient can assist the physician in reaching an accurate diagnosis (box 2).37 Among these, several communication-based recommendations—telling one's story well, being a good historian, and keeping good records—have also been identified by experts who value the ‘patient history’ as a critical component of proper diagnosis.34 38 The Informed Medical Decisions Foundation developed a worksheet for patients titled, ‘I wish I had asked that!’39 In addition, Graedon and Graedon offer a list of key questions that patients might pose to their providers in an effort to think more critically about potential diagnoses (box 3).18
Box 2. Patient/family tactics for preventing and detecting diagnostic errors.
Tell your story well (careful communication)
Be a good historian (attention to timing detail)
Be a good record keeper (attention to documentation)
Be an informed consumer (awareness)
Facilitate communication and coordination among different people involved in care
Ensure test results are known
Ensure follow-up (do not assume no news is good news)
Encourage your doctors to think broadly
Understand uncertainly in diagnosis (assume you have a ‘working diagnosis’ that may change)
Sources: Adapted in part from Graber,37 and synthesis generated by authors from the Diagnostic Errors in Medicine Conference24
Box 3. Questions to ask your provider to reduce diagnostic problems.
What are my primary concerns and symptoms?
How confident are you about the diagnosis?
What further tests might be helpful to improve your confidence?
Will the tests you are proposing change the treatment plan?
Are there findings/symptoms that do not fit your diagnosis?
What else could it be?
Can you facilitate a second opinion by providing me with my medical records?
When should I expect to see my test results?
What resources can you recommend for me to learn more about diagnosis?
Source: Graedon and Graedon18
Other approaches for involving patients in healthcare decisions regarding treatment might also be applicable when patients first meet with their providers, seeking diagnosis. For example, educational training efforts to improve physician–patient communication often focus on the physician, but can materials be developed to help train patients to initiate questions and communicate more effectively? Can educators and advocacy groups develop simulation exercises—that is, immersive experiences that help familiarise patients and their families with the healthcare system? How can health coaches or patient facilitators help patients become engaged effectively in the diagnostic process?
Why should patients want to become part of the process?
To be sure, patient engagement in health-related decisions requires time and effort on the part of patients and family members.40 We have described it here as a potential path to reduce diagnostic errors, but patient involvement and enhanced physician–patient communication can potentially yield other benefits as well. For example, in a 2007 survey of more than 15 000 households, Hibbard and Cunningham found that ‘activated patients’ who were engaged in their health reported having fewer delays in seeking medical care.41 Two-way communication provides physicians with feedback and improves clinical reasoning,42 regardless of whether the patient provides confirmatory information (in support of the physician's hypothesis) or contradictory information (that may require reconsidering the current hypothesis).
The role of the patient: improving the diagnostic delivery system
Reporting diagnostic errors
Healthcare organisations use many different tools to discover patient safety problems, but the instruments currently in use are generally ineffective in capturing diagnostic errors.43 Patients can therefore play a critical role in bringing these to light by reporting diagnostic errors, stimulating the organisation to study these incidents and consider improvements.6 44 The Agency for Healthcare Research and Quality is developing a new national reporting portal for all patients and caregivers. A Canadian study post paediatric hospital admission found that patients and their families are willing and able to report valid safety concerns, and that very few of these (less than 3% in this study) had been identified by the hospitals’ own safety-monitoring programme.45 Similar findings have been reported from Japan,46 Sweden47 and the USA.48 49 Patients are also able to report diagnostic errors in ambulatory settings; a recent survey of primary care patients found that 13% had experienced a diagnostic error.20 Studies of the factors that facilitate and hinder feedback are needed to improve reporting in the future,50 with special attention to diagnostic problems.
Besides providing important information back to the healthcare system, feedback from patients about diagnostic errors would help physicians as well. Developing clinical expertise depends on obtaining frequent, meaningful and direct feedback on performance. With autopsy rates markedly decreased, feedback on diagnosis is lacking. Feedback from patients on diagnostic errors could help fill this gap, and is thought to be essential for physicians to improve their internal calibration and reduce overconfidence.42 51
Direct involvement in delivery system
Hospitals and ambulatory practices are increasingly using patient advisory groups to provide feedback and advice on current performance.52 Similarly, input from patients through surveys is now expected and required in most healthcare settings. A new opportunity for a patient to improve the safety of healthcare and avoid diagnostic errors is to help another patient. The wisdom of someone who has already experienced a medical error makes ‘patient advocate’ programmes invaluable to patients who have taken advantage of such services.53 These three pathways reflect the growing trend for healthcare providers to utilise the patient's perspective and involvement to improve quality, safety, timeliness and value of their own healthcare delivery systems.
Acting as the safety net
An ideal healthcare system would excel at communication and care coordination. Although this remains the goal, failures in these two dimensions comprise the leading system-related causes of diagnostic error.54 By keeping copies of test results, discharge summaries, consultations and progress notes, and making these available to all of the physicians involved in the diagnostic process, patients and their families can effectively improve the diagnostic process by serving as the fail-safe backup for jobs that rightfully should be performed by their healthcare practices and organisations.26
The role of the patient: improving research and policy regarding diagnostic safety
At a recent Diagnostic Errors in Medicine conference,24 15 patients, family members and their representatives participated throughout the meeting at the podium, presenting, asking questions, making comments and developing strategies for next steps for advocacy, research and policy. The participants included patients/family members with no organisational affiliations and those who run or participate in patient safety and research organisations. The group and others will continue to contribute their thinking to the emerging Society to Improve Diagnosis in Medicine (SIDM).55 With a growing emphasis on stakeholder participation (eg, US-based Patient-Centered Outcomes Research Institute (http://www.pcori.org)), the research community is offering more opportunities for patient and family involvement. Although policymakers traditionally have valued active citizen involvement, they have more recently engaged patients and their representatives in healthcare improvement reforms and research.7 56–58
Targeting active relevant policy and research areas
Multiple national leverage points exist in diagnosis. Several contemporary initiatives illustrate the opportunity and challenge.
The ‘patient centred medical home’ (PCMH) is becoming a reality in many locations.59 What makes PCMH a policy imperative is the anticipation that emergency room utilisation will fall and hospital readmissions will decrease. However, patients often do not know how to optimally use their ‘medical home’, and do not take advantage of newer services like expanded office hours and telephone visits. As researchers evaluate PCMH, and policymakers set up incentives for this care approach, they are likely to benefit from input from patients about ways to maximise the likelihood for PCMH to be part of the solution to diagnostic errors.
Personal health records could improve the diagnostic process, and despite their great interest in these tools when interviewed, patients are adopting the technology slowly.60 61 The under-utilisation seems to reflect, as one of many issues, a classic illustration of limited early diffusion of innovation.62
Finally, the recently launched Patient-Centered Outcomes Research Institute offers an opportunity for patients to become personally involved in research directed specifically at problems of most interest to patients and their families. For example, what do we need to understand about the health system and doctors responses to different types of involvement and communication during diagnosis (eg, Boxes 2 and 3, and others from ‘The Take Charge Patient’ based on 200 interviews with patients, families and healthcare professionals)?17 How do we measure diagnostic error in a patient-centred way? What are the effects of malpractice policy on patient involvement in improving diagnosis?
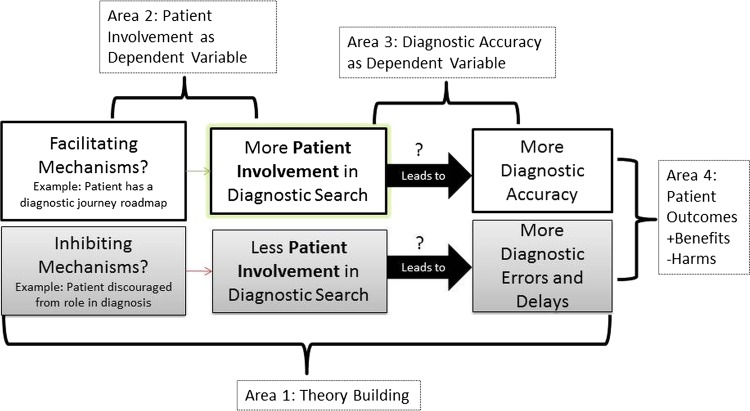
Patient involvement and diagnostic safety in tandem: research framework
Studying patient involvement and diagnostic error requires research in four priority areas. First, we need a theory to guide diagnostic error prevention, with a primary focus on patient involvement in care, recognising informal caregiver involvement as well. The scope of such theory-based research includes defining terminology and hypothesised relationships such as those shown in figure 1. Patient involvement is in the middle of a causal sequence with some factors influencing patient involvement level, and then, in turn, patient involvement becoming the independent variable in predicting variation in diagnostic safety. Refining this initial theory would require qualitative, experimental and quantitative observational research and further theory building. Mounting evidence supports that social relationships and associations have a strong effect on health, and available conceptual models of important linkages from macro-social to psychological and biologic processes could be overlaid with the patient's journey through the diagnostic process.63–65 Second, we need research exploring factors encouraging and inhibiting patient involvement in diagnosis. What increases involvement and what decreases it? What exactly counts as involvement in the diagnostic search? Third, we envision projects testing whether more patient involvement leads to better diagnostic performance, and under what circumstances. Fourth, and critically, we need research that evaluates the effects of involvement on the endpoints of patient and economic outcomes, including unintended adverse effects (eg, unnecessary testing). While the diagram is highly stylised and simplified, its depiction of relationships among major research areas could enable iterative learning and application of previous findings on patient involvement in safety and quality improvement broadly. Further consideration of ways that diagnosis resembles or differs from other areas of medical practice is important in developing a strategy to study patient involvement in improving diagnostic safety.
Figure 1.
Simplified schematic of priority research areas.
Conclusion
Diagnostic errors mete out a high cost to patients and their families, and to professional caregivers.66 We have proposed engaging healthcare consumers at three levels to improve diagnostic processes and decisions: a role in a patient's own care to the extent feasible, a contribution of advising and providing feedback to the delivery system, and more globally, a crucial voice for informing policy and research agendas. Patients are now being encouraged to take a more proactive role in their own care and safety, and programmes such as the PCMH and personal health records give them the opportunity to do so. To the extent that patients want this involvement, the opportunity exists for developing patient-oriented strategies to reduce diagnostic errors, and improve the safety and quality of healthcare in general. Many efforts are underway to support consumer involvement in the healthcare arena (eg, the Society for Participatory Medicine, movements like ‘Let Patients Help’67) and others are directing their supportive suggestions to the diagnostic slice of medicine (eg, books written and organisations formed by those who have experienced diagnostic errors).16–19 67 Bringing attention to diagnostic safety and understanding its particular challenges to patient participation is new territory for some, but well trod by many others who have experienced problems and hope that the lessons they have learned will help other patients, the delivery system and policymakers.16 67 68 It is time for the research field to direct its attention to the intersection of diagnostic safety and patient involvement.
Footnotes
Contributors: KMM, CLB and MLG each made substantial contributions to the conception and design of the article, drafting the article, and final approval of the version to be published.
Competing interests: None.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Patient Experience Network (NHS) 2006–2013; http://www.institute.nhs.uk/share_and_network/pen/publications.html (accessed 24 Jan 2013)
- 2.Davis RE, Jacklin R, Sevdalis N, et al. Patient involvement in patient safety: what factors influence patient participation and engagement? Health Expect 2007;10:259–67 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.O'Connor AM, Stacey D, Rovner D, et al. Decision aids for people facing health treatment or screening decisions. Cochrane Database Syst Rev 2001;(3) Diagnostic Error in Medicine:CD001431. [DOI] [PubMed] [Google Scholar]
- 4.O'Connor AM, Wennberg JE, Legare F, et al. Toward the ‘tipping point’: decision aids and informed patient choice. Health Aff (Millwood) 2007;26:716–25 [DOI] [PubMed] [Google Scholar]
- 5.Vincent CA, Coulter A. Patient safety: what about the patient? Qual Saf Health Care 2002;11:76–80 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ward JK, Armitage G. Can patients report patient safety incidents in a hospital setting? A systematic review. BMJ Qual Saf 2012;21:685–99 [DOI] [PubMed] [Google Scholar]
- 7.Olsen LA, Saunders RS, McGinnis JM. eds. Patients charting the course: citizen engagement and the learning health system: workshop summary. Washington, DC: The National Academies Press, 2011 [PubMed] [Google Scholar]
- 8.Barry MJ, Edgman-Levitan S. Shared decision making—pinnacle of patient-centered care. N Engl J Med 2012;366:780–1 [DOI] [PubMed] [Google Scholar]
- 9.McDonald KM, Matesic B, Contopoulos-Ioannidis DG, et al. Patient safety strategies targeted at diagnostic errors: a systematic review. Ann Intern Med 2013;158 [DOI] [PubMed] [Google Scholar]
- 10.Singh H, Graber ML, Kissam SM, et al. System-related interventions to reduce diagnostic errors: a narrative review. BMJ Qual Saf 2012;21:160–70 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Phillips RL, Jr, Bartholomew LA, Dovey SM, et al. Learning from malpractice claims about negligent, adverse events in primary care in the United States. Qual Saf Health Care 2004;13:121–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Schiff GD, Kim S, Abrams R, et al. Diagnosing diagnosis errors: lessons from a multi-institutional collaborative project. In: Henriksen K, Battles JB, Marks ES, Lewin DI. eds. Advances in patient safety: from research to implementation (Volume 2: Concepts and methodology). Rockville, MD: Agency for Healthcare Research and Quality, 2005 [PubMed] [Google Scholar]
- 13.Selbst SM, Baghdassarian A. Pediatric emergency medicine: legal briefs. Pediatr Emerg Care 2011;27:1213–15 [DOI] [PubMed] [Google Scholar]
- 14.Shojania KG, Burton EC, McDonald KM, et al. Changes in rates of autopsy-detected diagnostic errors over time: a systematic review. JAMA 2003;289:2849–56 [DOI] [PubMed] [Google Scholar]
- 15.Americans are concerned about hospital-based medical and surgical errors Wall Street Journal Online's Health Industry Edition. 20 July 2004
- 16.Brook I. My voice: a physician's personal experience with throat cancer. Charleston, SC: BookSurge Publishing, 2009 [Google Scholar]
- 17.Ehrenclou M. The take-charge patient: how you can get the best medical care. Santa Monica, CA: Lemon Grove Press, 2012 [Google Scholar]
- 18.Graedon J, Graedon T. Top screwups doctors make and how to avoid them. New York: Harmony, 2011 [Google Scholar]
- 19.King S. Josie's story: a mother's inspiring crusade to make medical care safe. New York: Atlantic Monthly Press, 2009 [Google Scholar]
- 20.Kistler CE, Walter LC, Mitchell CM, et al. Patient perceptions of mistakes in ambulatory care. Arch Intern Med 2010;170:1480–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Singh H, Daci K, Petersen LA, et al. Missed opportunities to initiate endoscopic evaluation for colorectal cancer diagnosis. Am J Gastroenterol 2009;104:2543–54 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Singh H, Hirani K, Kadiyala H, et al. Characteristics and predictors of missed opportunities in lung cancer diagnosis: an electronic health record-based study. J Clin Oncol 2010;28:3307–15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Carman KL, Dardess P, Maurer M, et al. Patient and family engagement: a framework for understanding the elements and developing interventions and policies. Health Aff (Millwood) 2013;32:223–31 [DOI] [PubMed] [Google Scholar]
- 24.Diagnostic Errors in Medicine, Program Booklet, 5th International Conference, 11–14 November 2012 http://www.hopkinscme.edu/pdfs/80028747.pdf (accessed 27 Jan 2013) [Google Scholar]
- 25.Hibbard JH, Greene J. What the evidence shows about patient activation: better health outcomes and care experiences; fewer data on costs. Health Aff (Millwood) 2013;32:207–14 [DOI] [PubMed] [Google Scholar]
- 26.Graber ML, Kissam S, Payne VL, et al. Cognitive interventions to reduce diagnostic error: a narrative review. BMJ Qual Saf 2012;21:535–57 [DOI] [PubMed] [Google Scholar]
- 27.Rajkomar A, Dhaliwal G. Improving diagnostic reasoning to improve patient safety. Permanente J 2011;15:68–73 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Flory N, Lang EV. Distress in the radiology waiting room. Radiology 2011;260:166–73 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Frosch DL, May SG, Rendle KA, et al. Authoritarian physicians and patients’ fear of being labeled ‘difficult’ among key obstacles to shared decision making. Health Aff (Millwood) 2012;31:1030–8 [DOI] [PubMed] [Google Scholar]
- 30.Boyer CA, Lutfey KE. Examining critical health policy issues within and beyond the clinical encounter: patient-provider relationships and help-seeking behaviors. J Health Soc Behav 2010;51(Suppl) Diagnostic Error in Medicine:S80–93 [DOI] [PubMed] [Google Scholar]
- 31.Lindsay S, Vrijhoef HJM. Introduction—a sociological focus on ‘expert patients’. Health Sociol Rev 2009;18:139–44 [Google Scholar]
- 32.Faust O, Acharya UR, Tamura T. Formal design methods for reliable computer-aided diagnosis: a review. IEEE Rev Biomed Eng 2012;5:15–28 [DOI] [PubMed] [Google Scholar]
- 33.Graber ML, Wachter RM, Cassel CK. Bringing diagnosis into the quality and safety equations. JAMA 2012;308:1211–12 [DOI] [PubMed] [Google Scholar]
- 34.Sanders L. Every patient tells a story: medical mysteries and the art of diagnosis. New York, NY: Broadway Books, 2009 [Google Scholar]
- 35.Dragusin R, Petcu P, Lioma C, et al. FindZebra: a search engine for rare diseases. Int J Med Inform 2013;82:528–38 [DOI] [PubMed] [Google Scholar]
- 36.The Joint Commission: Facts about Speak Up Initiatives. http://www.jointcommission.org/assets/1/18/Facts_Speak_Up.pdf (accessed 13 May 2013)
- 37.Graber ML. Family centered patient advocacy training. Chapter 9: steering clear of diagnostic errors. State Wantagh, NY: PULSE of NY, 2007 [Google Scholar]
- 38.Art of Diagnosis: Second Opinion. http://secondopinion-tv.org/episode/art-diagnosis1/24/13.
- 39.I Wish I Had Asked That! A worksheet for patients Informed medical decisions foundation web site. http://informedmedicaldecisions.org/2012/12/11/i-wish-i-had-asked-that-a-worksheet-for-patients (accessed 28 Jan 2013)
- 40.Vicarelli MG, Bronzini M. From the ‘expert patient’ to ‘expert family’: a feasibility study on family learning for people with long-term conditions in Italy. Health Sociol Rev 2009;18:182–93 [Google Scholar]
- 41.Hibbard JH, Cunningham PJ. How engaged are consumers in their health and health care, and why does it matter? HSC Research Brief 2008;(8) Diagnostic Error in Medicine:1–9 [PubMed] [Google Scholar]
- 42.Schiff GD. Minimizing diagnostic error: the importance of follow-up and feedback. Am J Med 2008;121(5 Suppl) Diagnostic Error in Medicine:S38–42 [DOI] [PubMed] [Google Scholar]
- 43.Levtzion-Korach O, Frankel A, Alcalai H, et al. Integrating incident data from five reporting systems to assess patient safety: making sense of the elephant. Jt Comm J Qual Patient Saf 2010;36:402–10 [DOI] [PubMed] [Google Scholar]
- 44.Millman EA, Pronovost PJ, Makary MA, et al. Patient-assisted incident reporting: including the patient in patient safety. J Patient Saf 2011;7:106–8 [DOI] [PubMed] [Google Scholar]
- 45.Pear R. New system for patients to report medical mistakes. The New York Times 22 September 2012
- 46.Hasegawa T, Fujita S, Seto K, et al. Patients’ identification and reporting of unsafe events at six hospitals in Japan. Jt Comm J Qual Patient Safety 2011;37:502–8 [DOI] [PubMed] [Google Scholar]
- 47.Ohrn A, Elfstrom J, Liedgren C, et al. Reporting of sentinel events in Swedish hospitals: a comparison of severe adverse events reported by patients and providers. Jt Comm J Qual Patient Safety 2011;37:495–501 [DOI] [PubMed] [Google Scholar]
- 48.Fowler FJ, Jr, Epstein A, Weingart SN, et al. Adverse events during hospitalization: results of a patient survey. Jt Comm J Qual Patient Safety 2008;34:583–90 [DOI] [PubMed] [Google Scholar]
- 49.Weingart SN, Pagovich O, Sands DZ, et al. What can hospitalized patients tell us about adverse events? Learning from patient-reported incidents. J Gen Intern Med 2005;20:830–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Davis RE, Sevdalis N, Jacklin R, et al. An examination of opportunities for the active patient in improving patient safety. J Patient Saf 2012;8:36–43 [DOI] [PubMed] [Google Scholar]
- 51.Berner ES, Graber ML. Overconfidence as a cause of diagnostic error in medicine. Am J Med 2008;121(5 Suppl) Diagnostic Error in Medicine:S2–23 [DOI] [PubMed] [Google Scholar]
- 52.White K. Engaging patients to improve the healthcare experience. Healthc Financ Manage 2012;66:84–8 [PubMed] [Google Scholar]
- 53.Corina I, Shapiro E. Family centered patient advocacy—a training manual. New York: PULSE of NY, 2009. http://www.pulseofny.org/Tools.html (accessed 24 January 2013) [Google Scholar]
- 54.Graber ML, Franklin N, Gordon R. Diagnostic error in internal medicine. Arch Intern Med 2005;165: 1493–9 [DOI] [PubMed] [Google Scholar]
- 55.Society to Improve Diagnosis in Medicine. http://www.improvediagnosis.org/ (accessed 13 May 2013)
- 56.Boote J, Telford R, Cooper C. Consumer involvement in health research: a review and research agenda. Health Policy 2002;61:213–36 [DOI] [PubMed] [Google Scholar]
- 57.Helfand M, Tunis S, Whitlock EP, et al. A CTSA agenda to advance methods for comparative effectiveness research. Clin Transl Sci 2011;4:188–98 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Selby JV, Beal AC, Frank L. The Patient-Centered Outcomes Research Institute (PCORI) national priorities for research and initial research agenda. JAMA 2012;307:1583–4 [DOI] [PubMed] [Google Scholar]
- 59.Jackson GL, Powers BJ, Chatterjee R, et al. The patient-centered medical home: a systematic review. Ann Intern Med 2012 [DOI] [PubMed] [Google Scholar]
- 60.Archer N, Fevrier-Thomas U, Lokker C, et al. Personal health records: a scoping review. J Am Med Inform Assoc 2011;18:515–22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Patel VN, Abramson E, Edwards AM, et al. Consumer attitudes toward personal health records in a beacon community. Am J Manag Care 2011;17:e104–120 [PubMed] [Google Scholar]
- 62.Emani S, Yamin CK, Peters E, et al. Patient perceptions of a personal health record: a test of the diffusion of innovation model. J Med Internet Res 2012;14:e150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Berkman LF, Glass T, Brissette I, et al. From social integration to health: Durkheim in the new millennium. Soc Sci Med 2000;51:843–57 [DOI] [PubMed] [Google Scholar]
- 64.Eisenberg JM. Sociologic influences on decision-making by clinicians. Ann Intern Med 1979;90:957–64 [DOI] [PubMed] [Google Scholar]
- 65.Longtin Y, Sax H, Leape LL, et al. Patient participation: current knowledge and applicability to patient safety. Mayo Clinic Proc 2010;85:53–62 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Wu AW. Medical error: the second victim. The doctor who makes the mistake needs help too. BMJ 2000;320: 726–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Let Patients Help TED Talk. http://epatientdave.com/videos/ (accessed 27 Jan 2013)
- 68.Rory Staunton Foundation. http://www.rorystaunton.com/index.php (accessed 27 Jan 2013)