Abstract
This study investigated the incidence and characteristics of poisoning fatalities and hospital admissions among indigenous Fijians and Indians in Viti Levu, Fiji. Individuals with a mechanism of injury classified as poisoning were identified using the Fiji injury surveillance in hospitals system, a population-based registry established for 12 months in Viti Levu, and analysed using population-based denominators. The mean annual rates of fatalities and hospitalisations were 2.3 and 26.0 per 100 000, respectively. Over two-thirds of poisonings occurred among people of Indian ethnicity. Most intentional poisoning admissions occurred among women (58.3%) and in 15–29-year-old individuals (73.8%). Unintentional poisoning admission rates were highest among Indian boys aged 0–14 years. While over 75% of events occurred at home, the substances involved were not systematically identified. The findings indicate the need for a strategy that addresses the differing contexts across age group, gender and ethnicity, and a lead agency responsible for implementing and monitoring its effectiveness.
Introduction
The global burden of poisoning is disproportionately borne by low and middle-income countries, influenced by many factors including greater exposure to hazardous products.1 Variations in the incidence of poisoning between and within countries also suggest the influence of socioculturally mediated factors, particularly among people of Asian ethnicity.2–5 In some rural Asian communities, poisoning is the commonest form of suicide, accounting for over 60% of all deaths.6 7 In Malaysia and Singapore, patients of Indian and Chinese ethnicity are disproportionately represented in poisoning statistics compared with other ethnic groups.3 8 9
Routinely reported poisoning statistics in Fiji are not usually disaggregated by ethnicity, but hospital-based studies in Fiji suggest that the Indian diaspora are overrepresented in hospitalisations and deaths due to poisoning in Fiji.10 11 The aim of this study was to investigate systematically the population-based incidence and demographic characteristics of poisoning resulting in death or hospital admission in Viti Levu, the largest island in Fiji. Viti Levu has a resident population of 650 640 (70% of the country's population), with indigenous Fijian and Indian people comprising 54.5% and 40.0% of the population, respectively.
Methods
The Fiji injury surveillance in hospitals system was established at all hospitals in Viti Levu for 12 months commencing 1 October 2005 as part of the Traffic-Related Injury in the Pacific (TRIP) project. This population-based registry, the development of which has been described previously,12 captured data on all deaths and hospital admissions for more than 12 h due to an acute injury or poisoning. Cases were identified from hospital accident and emergency registers, admission and post-mortem records. All poison-related deaths in Fiji are reported to the Police department and undergo postmortem examination.
This study focused on all records in the Fiji injury surveillance in hospitals database in which the mechanism of injury was classified as poisoning. Population-based incidence rates by sociodemographic characteristics were computed using denominator data from the Fiji census of 2007. The unique national hospital numbers were used to avoid double-counting of events.
Results
Fatalities
The 17 deaths (nine men) corresponded to an annual fatality rate of 2.3 per 100 000 population. All but one death was deemed intentional, most involving people of Indian ethnicity (n=13) and the age group 15–29 years (n=12). Most events (n=14) occurred at home or in a private compound. Five deaths occurred out of hospital, and 12 followed admission with an inhospital case fatality rate of 7.1% (12/169).
Non-fatal hospitalisations
The 157 non-fatal hospitalisations accounted for an annual rate of 24.1 per 100 000 population in Viti Levu. Poisonings deemed intentional, unintentional and of undetermined intent accounted for 53.5%, 43.9% and 2.5% of non-fatal events. The annual rate for intentional and unintentional poisoning was 12.9 and 10.6 per 100 000 population, respectively.
Female patients accounted for 58.3% of intentional poisonings and male patients accounted for 56.5% of unintentional events. While 73.8% of the intentional poisoning patients were in the 15–29 year age group, 40.6% of unintentional injury deaths occurred among children aged 14 years or less. The mean length of hospital stay was 2.6 days (median 2.0). Most poisoning events that resulted in non-fatal hospital admissions (93.6%) occurred at home or in a private compound.
Among the people who were admitted for poisoning, 107 (68.2%) were of Indian ethnicity, 47 (29.9%) were Fijian and three (1.9%) were of other ethnicities. The crude annual rate of non-fatal hospitalisations due to poisoning among Indians was three times that of Fijians (41.2 vs 13.3, per 100 000 population). Most non-fatal admissions among the Fijians were due to unintentional poisoning, while the majority of admissions and fatalities among Indians were due to intentional poisoning (table 1).
Table 1.
Characteristics of non-fatal hospitalisations for poisoning by ethnicity
| No (%) of | |||
|---|---|---|---|
| Fijians (n=47) | Indians (n=107) | χ2 Value (p value) | |
| Gender | |||
| Male | 23 (48.9) | 50 (46.7) | 0.06 (0.800) |
| Female | 24 (51.1) | 57 (53.3) | |
| Age group, years | |||
| 0–14 | 14 (29.8) | 18 (16.8) | 12.90 (0.005) |
| 15–29 | 15 (31.9) | 65 (60.7) | |
| 30–44 | 10 (21.3) | 18 (16.8) | |
| ≥45 | 8 (17.0) | 6 (5.6) | |
| Intent | |||
| Unintentional | 35 (74.5) | 33 (30.8) | 25.45 (<0.001) |
| Intentional (self-harm) | 11 (23.4) | 71 (66.4) | |
| Undetermined intent | 1 (2.1) | 3 (2.8) | |
| Circumstance | |||
| Conflict situation | 12 (25.5) | 70 (65.4) | 26.54 (<0.001) |
| Leisure/play | 33 (70.2) | 28 (26.2) | |
| Other | 2 (4.2) | 9 (8.3) | |
| Alcohol use | |||
| Suspected/confirmed | 2 (4.3) | 4 (3.7) | 0.34 (0.842) |
| No | 40 (85.1) | 88 (82.2) | |
| Unknown | 5 (10.6) | 15 (14.0) | |
| Kava use | |||
| Suspected/confirmed | 2 (4.2) | 2 (1.9) | 0.88 (0.645) |
| No | 38 (80.9) | 86 (80.4) | |
| Unknown | 7 (14.9) | 19 (17.8) | |
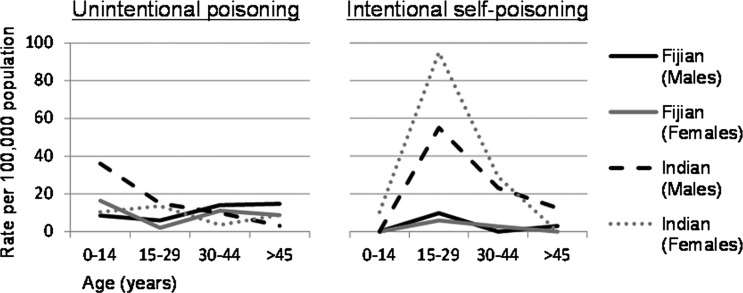
The context for unintentional poisoning events was commonly reported as ‘leisure or play’ (Fijians 94.3%, Indians 72.7%). Rates were highest among Indian boys aged 0–14 years (figure 1). The context for intentional poisoning events was most commonly reported as a conflict situation (Fijians 100%, Indians 93%). The age group most commonly involved was 15–29 years, with rates for women and men being considerably higher for Indians (116.6 and 70.0 per 100 000, respectively). Equivalent rates among Fijian women and men were 11.9 and 9.8 per 100 000, respectively.
Figure 1.
Ethnicity-based rates of non-fatal hospitalisations due to poisoning by intent.
Substances involved
Only a third of clinical records documented the substance involved in poisonings, a factor that did not differ significantly by age, gender, ethnicity, intent or outcome (fatal or non-fatal). Among intentional poisonings, the commonly documented substances were chemicals (41.2%), drugs (35.3%) and pesticides (23.5%). In unintentional poisonings, chemicals (69.6%), food (21.7%) and drugs (8.7%) comprised the common sources. The ‘chemicals’ involved were typically not defined further but kerosene and household cleaning products were identified as the agent in several (11) cases. Two cases were ascribed to ciguatera fish poisoning.
Discussion
This study adds to the relatively sparse published epidemiological information on poisoning in Pacific Islands by identifying a population-based profile of acute poisoning fatalities and hospital admissions in Viti Levu, Fiji. Over two-thirds of events in this predominantly Melanesian country occurred among people of Indian ethnicity. Rates of intentional poisoning were particularly high among Indian women aged 15–29 years, while unintentional poisoning rates were highest among Indian boys aged 0–14 years.
The use of a quality-assured injury surveillance database12 that captured serious poisoning events resulting in hospital admission or death provided the opportunity to obtain population-based estimates in this setting and identify subgroups at increased risk of poisoning. When interpreting findings, however, it is important to acknowledge that access to healthcare could influence presentations, and the study was not designed to identify assessments by primary care providers or traditional healers. The study is also limited by the lack of detailed information on the context of these events and systematically coded data on the substances involved. In the third of cases in which this information was available, the minimum dataset available did not characterise the types of ‘chemicals’ or ‘drugs’ involved. Consistent with many developing countries, pesticides and drugs were commonly implicated in intentional poisoning.2 13 The study focused on Viti Levu where over 70% of the population resides, and the epidemiology of poisoning was not considered likely to be substantially different in other parts of Fiji. However, the relatively small study population could lead to a degree of imprecision in the estimates derived.
The rate of attempted suicide by poisoning in a previous hospital-based study in Fiji2 was twice that estimated in our study (25.9 compared with 12.9 per 100 000). This difference is likely to be due to the exclusion of patients admitted for less than 12 h and the inclusion of the entire population of Viti Levu in the present study. The higher rate of poisoning deemed intentional, with women aged 15–29 years being at highest risk, is a pattern observed in many low and middle-income countries including Ethiopia,14 Iran,9 15 India,13 16 Nepal17 18 and Malaysia.3
While the absolute numbers of deaths were low and crude mortality rates were difficult to compare due to different demographic structures, the inhospital case fatality rate in Viti Levu (7.1%) is similar to findings in Ethiopia (8.6%),14 but higher than those reported from Iran (1.3–2.3%)15 19 and Nepal (5%).17 However, higher case fatality rates have been reported from India (12.8–15%).13 16
The ethnic differences identified in our study are consistent with previous case series from Fiji,2 10 11 and the observation of elevated rates of suicide among the Indian diaspora in other countries.2–5 8 11 While the context is likely to be complex, a range of sociocultural and behavioural factors have been postulated, including the high social mobility, breakdown in the extended family system and rapid cultural transformation as well as impulsivity, aggression and easy accessibility to agents such as pesticides.5 11
The findings of this study indicate the need for careful explorations of the physical and sociocultural environments in which these events occur. Aspects that may differ among age group, gender and ethnic lines that require particular attention in an overarching poison control strategy include the exposure to hazardous substances during the developmentally vulnerable childhood period, exposure to conflict and violence, practices relating to help seeking and access to supportive services in the context of mental health concerns.
Poison information centres that provide information to heathcare workers and the community, and maintain contacts with industry for exchange of information on chemical products, can save lives and reduce healthcare costs.20 While such centres have also been shown to reduce morbidity and mortality in some low and middle-income countries,20 establishing and maintaining these can be difficult in the context of scarce resources and competing public health priorities. In Fiji, where there is increasing investment in strengthening the health information system, systematically collecting and reporting data on poisoning events could help prioritise appropriate poison control strategies.
What is already known on the subject.
Poisoning is an important cause of death and hospitalisation, particularly in low and middle-income countries.
What this study adds.
Over two-thirds of poisoning-related deaths and hospitalisations in this predominantly Melanesian country occur among the minority Indian population.
Socioculturally mediated factors need to be taken in to account when identifying culturally relevant preventive strategies that address unintentional poisoning among children and intentional poisoning particularly among young women aged 15–29 years.
Acknowledgments
The authors gratefully acknowledge the support of the Permanent Secretary of Health, Dr Lepani Waqatakirewa and the Fiji Ministry of Health staff at national, divisional and subdivisional levels, the doctors and nurses in the surveillance hospitals and the final year medical students of 2005–6 at the Fiji School of Medicine who assisted with data collection, and the wider TRIP Project team including Professors Sitaleki Finau and Rod Jackson, Drs Aumea Herman and Robyn McIntyre, Asilika Naisaki, Mabel Taoi, Ramneek Gounder, Litia Vuniduvu and Nola Vanualailai.
Footnotes
Contributors: All authors provided substantial contributions to the conception and design, acquisition of data, analysis and interpretation of data and in writing the final version of the manuscript for publication.
Funding: This study was funded by an international collaborative research grant from The Wellcome Trust (UK) (grant no GR071671MA) and the Health Research Council of New Zealand (grant no 04/498). The funders had no involvement in the study design, collection, analysis and interpretation of the study data, the writing of the manuscript or the decision to submit the manuscript for publication. Views and/or conclusions in this article are those of the authors and may not reflect the position of The Wellcome Trust or Health Research Council of New Zealand.
Competing interests: None.
Ethics approval: Ethics approval was provided by the Fiji National Research Ethics Review Committee.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.World Health Organisation Poisoning prevention and management. 2011. www.who.int/ipcs/poisons/en/ (accessed 13.12.2011). [Google Scholar]
- 2.Aghanwa HS. Attempted suicide by drug overdose and by poison-ingestion methods seen at the main general hospital in the Fiji islands: a comparative study. Gen Hosp Psychiatry 2001;23:266–71 [DOI] [PubMed] [Google Scholar]
- 3.Fathelrahman AI, Ab Rahman AF, Zain ZM, et al. Factors associated with adult poisoning in northern Malaysia: a case–control study. Hum Exp Toxicol 2006;25:167–73 [DOI] [PubMed] [Google Scholar]
- 4.Bhui K, McKenzie K, Rasul F. Rates, risk factors & methods of self harm among minority ethnic groups in the UK: a systematic review. BMC Public Health 2007;7:336–49 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.van Spijker BAJ, Graafsma T, Dullaart HIA, et al. Impulsive but fatal self-poisoning with pesticides among South Asians in Nickerie, Suriname. Crisis 2009;30:102–5 [DOI] [PubMed] [Google Scholar]
- 6.Somasundaram DJ, Rajadurai S. War and suicide in northern Sri Lanka. Acta Psychiatr Scand 1995;91:1–4 [DOI] [PubMed] [Google Scholar]
- 7.Joseph A, Abraham S, Muliyil JP, et al. Evaluation of suicide rates in rural India using verbal autopsies 1994–9. BMJ 2003;326:1121–2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wai BH, Hong C, Heok KE. Suicidal behavior among young people in Singapore. Gen Hosp Psychiatry 1999;21:128–33 [DOI] [PubMed] [Google Scholar]
- 9.Azizi BH, Zulkifli HI, Kasim MS. Risk factors for accidental poisoning in urban Malaysian children. Ann Trop Paediatr 1993;13:183–8 [DOI] [PubMed] [Google Scholar]
- 10.Pridmore S, Lawler A, Couper D. Hanging and poisoning autopsies in Fiji. Aust NZ J Psychiatry 1996;30:685–7 [DOI] [PubMed] [Google Scholar]
- 11.Aghanwa HS. The characteristics of suicide attempters admitted to the main general hospital in Fiji Islands. J Psychosom Res 2000;9:439–45 [DOI] [PubMed] [Google Scholar]
- 12.Wainiqolo I, Kafoa B, MaCaig E, et al. Development and piloting of the Fiji Injury Surveillance in Hospitals System (TRIP Project-1). Injury. Published Online First: 16 November 2011. doi:10.1016/j.injury.2011.10.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jaiprakash H, Sarala N, Venkatarathnamma PN, et al. Analysis of different types of poisoning in a tertiary care hospital in rural South India. Food Chem Toxicol 2011;49:248–50 [DOI] [PubMed] [Google Scholar]
- 14.Desalew M, Aklilu A, Amanuel A, et al. Pattern of acute adult poisoning at Tikur Anbessa specialized teaching hospital, a retrospective study, Ethiopia. Hum Exp Toxicol 2011;30:523–7 [DOI] [PubMed] [Google Scholar]
- 15.Ahmadi A, Pakravan N, Ghazizadeh Z. Pattern of acute food, drug, and chemical poisoning in Sari City, Northern Iran. Hum Exp Toxicol 2010;29:731–8 [DOI] [PubMed] [Google Scholar]
- 16.Singh B, Unnikrishnan B. A profile of acute poisoning at Mangalore (South India). J Clin Forensic Med 2006;13:112–16 [DOI] [PubMed] [Google Scholar]
- 17.Paudyal BP. Poisoning: pattern and profile of admitted cases in a hospital in central Nepal. J Nepal Med Assoc 2005;44:92–6 [PubMed] [Google Scholar]
- 18.Thapa SR, Lama PK, Karki N, et al. Pattern of poisoning cases in Emergency Department of Kathmandu Medical College Teaching Hospital. Kathmandu Univ Med J 2008;6:209–13 [PubMed] [Google Scholar]
- 19.Islambulchilar M, Islambulchilar Z, Kargar-Maher MH. Acute adult poisoning cases admitted to a university hospital in Tabriz, Iran. Hum Exp Toxicol 2008;28:185–90 [DOI] [PubMed] [Google Scholar]
- 20.Peden M, Oyegbite K, Ozanne-Smith J, et al., eds World report on child injury prevention. Geneva: World Health Organization, 2008 [PubMed] [Google Scholar]