Abstract
Our prior research focused on parental treatment acceptability (TA) and preferences (TP) for preventive dental treatments for young Hispanic children. We adapted the interview for administration to parents of young African American children.
Objective
In a sample of African American parents, determine parental TA and TP for 5 dental treatments to prevent early childhood caries.
Methods
Interviewed 48 parents/caregivers of African American children attending Head Start, assessing TA and TP for 3 treatments for children: toothbrushing with fluoride toothpaste (TB), fluoride varnish (FV), and xylitol in food (XF); and 2 treatments for mothers: xylitol gum (XG) and chlorhexidine (CHX) rinse. The interview included verbal information, illustrated treatment cards, photos/video clips, and samples. Parents provided TA of each treatment (1–5 scale), TP between each of 10 pairs of the 5 treatments, and open-ended reasons for their preferences. TP were summed (0–4) to create overall preference.
Results
All treatments were acceptable (means 4.4–4.9). TB was more acceptable than FV and XF (p<0.05). Summed TP revealed a strong preference for TB (mean 3.1) above other treatments (all p<0.01). Primary reasons for preferring TB were: promotes healthy habits; child-focused; and effectiveness.
Conclusions
All treatments were acceptable, however, parents/guardians strongly preferred TB. Parents’ emphasis on healthy habits and child-focused treatment supports efforts for oral health education programs in early childhood settings. Some parents expressed concerns about FV, XF, and CHX. Results may be useful in planning prevention programs for young children in African American communities.
Keywords: oral health, acceptability of healthcare, pediatric dentistry, preventive dental treatments, African American
INTRODUCTION
Early childhood caries (ECC), defined as the presence of 1 or more decayed, missing, or filled tooth surface in a child under the age of six years old (1), is the most common, chronic disease of childhood and it is largely preventable (2). Efforts to reduce ECC prevalence have focused on providing early preventive care. However, despite reduction in caries rates in older children, rates among children from minority and low-income families have increased (3), indicating that more effective approaches are needed.
ECC reduction has been a public health priority and the federal government and many states have expended considerable resources to address this issue. State child health insurance programs, implemented in 1997 by many states and the federal government, for example, resulted in a decrease in the number of children who lacked dental insurance from 29% to 20% (4). Unfortunately, despite this positive outcome, under-utilization of available dental care resources remains unnecessarily high in minority and low-income communities (5).
Barriers to utilizing accessible oral health care may include: caregivers’ lack of knowledge regarding treatment availability, difficulty in making and keeping appointments, and providers’ lack of cultural competence in health systems. Additionally, cultural norms may negatively influence the acceptability of health care treatments and may vary across racial and ethnic populations. Thus, understanding the acceptability of preventive dental treatments for young children from low-income and minority populations may play an important role in improving their care utilization and oral health outcomes.
Few studies have explored acceptability of preventive oral health treatments for children. Most have examined preferences for varying characteristics such as flavor, color, or type of a particular treatment such as fluoride varnish (6) or xylitol in food (7). However, these findings represent preferences for treatments already received; participants have already found them acceptable because they agreed to receive the treatment. Very little research has examined acceptability and preferences among different treatments at the broader community level, among participants who may or may not wish to receive the treatments. Most studies assessing acceptability and preferences independently of actual treatment evaluation tended to focus on restorative caries treatments for children, including restoration versus monitoring (8) and type of restorative material preferred (9).
Our prior study explored parent/guardian acceptability and preferences for preventive treatments for young Hispanic children (10). Five treatments were assessed – fluoride varnish (FV), toothbrushing with fluoride toothpaste (TB), xylitol in food (XF), all for children, and two treatments for mothers, xylitol gum (XG) and chlorhexidine rinse (CHX). Parents/guardians reported that all the treatments were highly acceptable for their children; however, they expressed significant preferences for FV and TB, compared to the three other treatments. Acceptability and preference for these treatments have not been explored within other racial and ethnic groups at high risk for ECC. Because parents are the decision makers for their children’s dental care, an increased understanding of parental preferences for treatments that would benefit children could inform efforts to increase utilization of available treatments. Thus, the purpose of this study was to extend our prior research with Hispanic parents/guardians (10) to evaluate caregiver (parent/guardian) acceptability and preferences for FV, TB, FX, XG, and CHX treatments, known to prevent ECC, and to explore the reasons for those preferences in a sample of parents of African American children. These treatments were chosen because they are low-cost, appropriate for young children or mothers, and they represent home-based and office-based options.
METHODS
The study took place in the Head Start and Early Head Start Centers, federally-funded preschool settings within Alameda County in the San Francisco Bay Area, and prior to initiation was approved by the University of California San Francisco Institutional Review Board.
Study Design
We utilized a modified interview-based assessment of parental acceptability and preferences for ECC preventive treatments that had originally been developed for Hispanic children (11). To assure the cultural appropriateness of the instrument, we first conducted a focus group with African American families (N=7). We discussed the procedure with participants, presented the English-language versions of the illustrated assessment materials, and asked them to discuss their thoughts and give suggestions for improvements. Participants thought that the assessment was clear and appropriate. Based on their feedback, we modified pictures on the original illustrations so that they depicted African American families and health providers. Materials included illustrated cards accompanied by verbal descriptions of each treatment, samples of products used in each treatment, and computer photos or a video clip showing the treatments being administered.
All interviews were conducted by an African American researcher (author CR), using a computer-aided personal interview (CAPI) program. The complete interview included the acceptability assessment; demographic questions; Dental Knowledge Scale (12) that assesses parental knowledge of children’s oral health; a modified version of the Personal Assisted Employment Services (PAES) Dental Program Patient Satisfaction Survey to assess satisfaction with most recent dental care experience (13); and the Children’s Oral Health Quality of Life Scale, a caregiver report of degree of functional, psychological, and social difficulties related to their child’s oral health status (14).
Participants
A convenience sample (N=48) of caregivers was recruited at the Head Start Center through direct approach during arrival and departure times at the child care centers and flyers placed in children’s backpacks. One caregiver per household with an African American child 1–5 years old enrolled at the center was eligible to participate. Informed consent was obtained at the time of the interview and caregivers were offered a $30.00 gift card as a thank you for their time. We estimated that approximately 50% of those approached for recruitment agreed to participate.
The Acceptability Interview
This assessment evaluates parental acceptability of, and preferences for, 5 preventive treatments known to help prevent ECC. Initially, the interviewer explained that all treatments were safe, effective, required no sedation or restraint, and not intended to replace home care. Each treatment was then described and evaluated individually in the following steps. First, an illustrated card was presented that included what the treatment was, who received it, where it was given, frequency, and the quality of the taste or smell. An accompanying verbal description clarified information on the cards, how treatments work, and how they are given. As an example, for FV, we explained that: fluoride helps prevent cavities by making teeth stronger; FV is a sticky solution that is applied to the teeth with a soft brush and it is usually done two times each year; it is usually done in a dentist’s office; it tastes like bubble gum; it should stay on the teeth overnight; and a parent should help their child brush it off with a regular toothbrush. Treatment supplies were also presented (e.g., an opened package of FV with applicator). Next, a video clip (for FV) or computer photograph (all other treatments) was shown. We showed the video clip only for FV because it is delivered by a professional outside of the home, in contrast to TB, XF, XG and CH, all treatments which are based on common practices in the home and overseen by parents. Prior to assessing acceptability, the interviewer used the “teach back” method to confirm that the participant understood the information given about the treatment. This involved asking the participant to explain the treatment in her or his own words after it had been presented by the interviewer. If the explanation was adequate, the interviewer proceeded with the assessment; if not, he explained the treatment again and asked the participant to explain it again. Materials were developed at the 4th grade reading level and the interviewer reported that there were no problems with participants’ understanding of the content. Participants were asked if they had heard of the treatment prior to the interview. They rated whether the treatment was appropriate for a 1–2 year-old child (yes, no, not sure), for a 3–5 year-old child, and how sure they were that they would want their child to receive the treatment (1–5 scale from very sure I would not want to very sure that I would want) if it were offered to him/her. For the two mother-treatments, participants rated whether the treatment was appropriate for mothers (yes, no, not sure), and how sure they were that they would want the treatment (1–5 scale) if it were offered to them.
To determine preferences among treatments, following the individual assessments, we presented the treatments in pair-combinations (10 unique pairs) and asked participants to choose their preferred treatment within each pair. For both the individual and paired evaluations, treatments were presented in a random order to prevent bias from possible order effects. After preferences had been evaluated within the 10 pairs, the interviewer reviewed each choice within pairs and asked the participant to explain why she or he had chosen the treatment. Due to time restraints, a subsample (70% of sample) completed this latter assessment. This qualitative information was recorded and used to determine the reasons for the treatment preferences.
Analysis
Acceptability of Five Treatments
Means and standard deviations of the acceptability ratings were calculated and differences in ratings using a nonparametric Friedman rank test were assessed. Wilcoxon signed rank tests were calculated to determine whether the treatments for children were more acceptable for 3–5 year olds than 1–2 year olds. We utilized a nonparametric Friedman rank test and paired Wilcoxon signed rank tests with a Bonferroni-Holm correction to compare rates of having previously heard about the preventive treatments.
Preferences Based on Paired Comparisons
We used a Bradley-Terry model (15) to test within-pair preferences and estimate probabilities of preference along with 95% confidence intervals (CIs). To determine an overall preference score, we summed the number of times each treatment was preferred in the 10 pairs (range 0–4) and compared among treatment sums with a nonparametric Friedman rank test. Paired Wilcoxon signed rank tests were conducted to evaluate the summed times a treatment was preferred among the five treatments, two at a time. A Bonferroni-Holm post hoc correction (16) was used to adjust for multiple comparisons with initial alpha*=0.05/10=0.005).
Testing associations between treatment acceptability/preferences and participant characteristics
Pearson correlations were conducted between acceptability and preference scores and participant factors (age, years of education, having heard of treatment prior to study, dental knowledge, satisfaction with past dental care, and child oral health quality of life), using a Bonferroni-Holm adjustment (with the initial alpha*=0.05/35 = 0.0014) to determine the minimum reported significance level to account for multiple testing.
Qualitative assessment of reasons for treatment preferences
Utilizing standard procedures for qualitative data analysis, we coded caregivers’ reasons for preferring treatments utilizing nine major constructs that had been developed in the earlier study (Table 1.) (17). These constructs had been developed through an iterative coding process of data reduction and consensus (18,19). Data reduction consisted of sorting the parents’ reasons for preferences into categories that best described the detailed content of the comment, and then combining similar categories into broader-level themes, until ultimately a construct identifying a single over-arching theme emerged (data reduction). For example, two similar categories: 1) children should develop good brushing habits; and 2) child should not eat sweets every day, were combined into a broader-level theme of “health habits”. Two authors met to reach consensus on the themes and then independently classified the comments into the various constructs, with a minimum of 85% agreement. The number of times each construct appeared in all the comments made about preferences for specific treatments was tallied. The nine constructs were: 1) health habits; 2) who receives treatment; 3) effectiveness; 4) convenience; 5) taste; 6) frequency; 7) organic; 8) current practices; and 9) expense. The explanations given could be either positive comments for choosing the treatment in each pair or negative comments about the alternative treatment not chosen. Multiple reasons could be, and often were, given for a preference and each distinct theme associated with a preference was noted. When descriptions were of the same basic idea or reason, these were regarded as variants of the same construct; e.g. comments “faster to do” and “easier” made by one participant describing the same preference would be counted just once under the “convenience” construct.
Table 1.
Qualitative constructs describing narrative reasons for preferences.
| Construct: | Example of Construct |
|---|---|
| Health Habits |
|
| Effectiveness | “protects the teeth” |
| Who receives treatment |
|
| Convenience | “easier” |
| Frequency | “use every day” |
| Organic | “xylitol is better than regular sugar” |
| Expense | “affordable” |
| Taste | “I like gum” |
| Current practices | “already receives FV” |
RESULTS
Forty eight caregivers (parents/guardians) (94% parents) of African American children attending the childcare programs at the Head Start Centers comprised the sample (Table 2). Ninety-six percent were female and the mean age was 36.1 (SD=12.3). Median caregiver education was 14 years (range= 5–20 years).
Table 2.
Descriptive Statistics of Study Variables (N = 48)
| Characteristic | Mean (SDa)/Median/ Percent | Study Range |
|---|---|---|
| Caregiver age; mean years (SD) | 36.1 (12.3) | 18–71 |
| Caregiver female gender | 95.8% | |
| Education (median years) | 14 | 5–20 |
| Satisfaction with most recent dental care b; mean (SD) | 3.1 (0.7) | 1–4 |
| Dental knowledge survey c; mean(SD) | 8.3 (1.4) | 4–10 |
| Child oral health quality of life (caregiver reported) d; mean (SD) | 16.0 (5.4) | 10–28 |
SD= Standard Deviation;
Low score indicates low satisfaction, scale range= 1–5;
low score indicates low knowledge, scale range = 0–10;
low score indicates high oral health quality of life with a scale range= 10–40.
Ratings of the Five Preventive Treatments
All treatments were rated as acceptable; means ranged from 4.4 (SD=1.0) for XF to 4.9 (SD=0.5) for TB (Table 3). Differences among acceptability ratings were significant, (Friedman Chi Square=15.2, p < 0.01). Ratings for TB (4.9) were significantly higher than FV (4.5) and XF (4.4), both p < 0.05. Other differences were not significant.
Table 3.
Parental Acceptability Ratings for Five Early Childhood Caries Preventive Agents (N=48)
| Treatment: | Had participant heard
of treatment prior to study? |
Acceptability rating for
each treatment (1–5 scale) |
Yes-no acceptability judgment by
child age group and for mother |
||||
|---|---|---|---|---|---|---|---|
| % yes | Friedman Chi Square 94.9 *** |
Mean (SD) | Friedman Chi Square 15.2 ** |
OK for 1–2 year olds % yes |
OK for 3–5 year olds % yes |
Wilcoxon Signed Rank test between age groups(a) |
|
| Child treatments | Wilcoxon Signed Rank (a) | Wilcoxon Signed Rank Test (a) | |||||
| Brushing with fluoride toothpaste (TB) | 91.7 | >FV*** CHX*** XF*** XG*** |
4.9 (0.5) | > FV * XF* | 91.7 | 97.9 | -- |
| Fluoride varnish (FV) | 52.1 | >CHX*** XF*** XG** |
4.5 (1.0) | -- | 60.4 | 93.8 | *** |
| Xylitol in food (XF) | 8.3 | -- | 4.4 (1.0) | -- | 77.1 | 87.5 | -- |
| Mother Treatments | OK for mother (% yes) | ||||||
| Xylitol gum (XG) | 20.8 | -- | 4.7 (0.9) | -- | 97.9 | --- | -- |
| Chlorhexidine (CHX) | 12.5 | -- | 4.7 (0.7) | -- | 97.9 | --- | -- |
p < 0.001;
p < 0.01;
p < 0.05;
with Bonferroni-Holm correction; Varnish = FV; Brushing = TB; CHX = CHX mouth rinse; Food = XF; Gum= XG
Caregivers’ ratings of whether the child-based treatments were acceptable for different age groups (1–2 years or 3–5 years) indicated that acceptability of FV was higher for the older age group than the younger (Bonferroni-Holm p<0.001), but not for TB or XF.
The proportion of participants who had heard of the treatments prior to being in the study ranged from a high of 92% for TB to 8% for XF, Friedman Chi Square = 94.9, p < 0.001 (Table 3). Prior exposure to information about toothbrushing was higher than all other treatments, all p < 0.001. FV (52%) was significantly higher than CHX (13%), XG (21%) and XF (8%), all p <0.01. Having heard of a particular treatment prior to the study was not associated with the ordinal acceptability ratings for that treatment. Likewise, neither participant age, education, dental knowledge, satisfaction with dental care nor child oral health quality of life was associated with acceptability ratings (results not tabled).
Treatment Preferences Based on Paired Comparisons
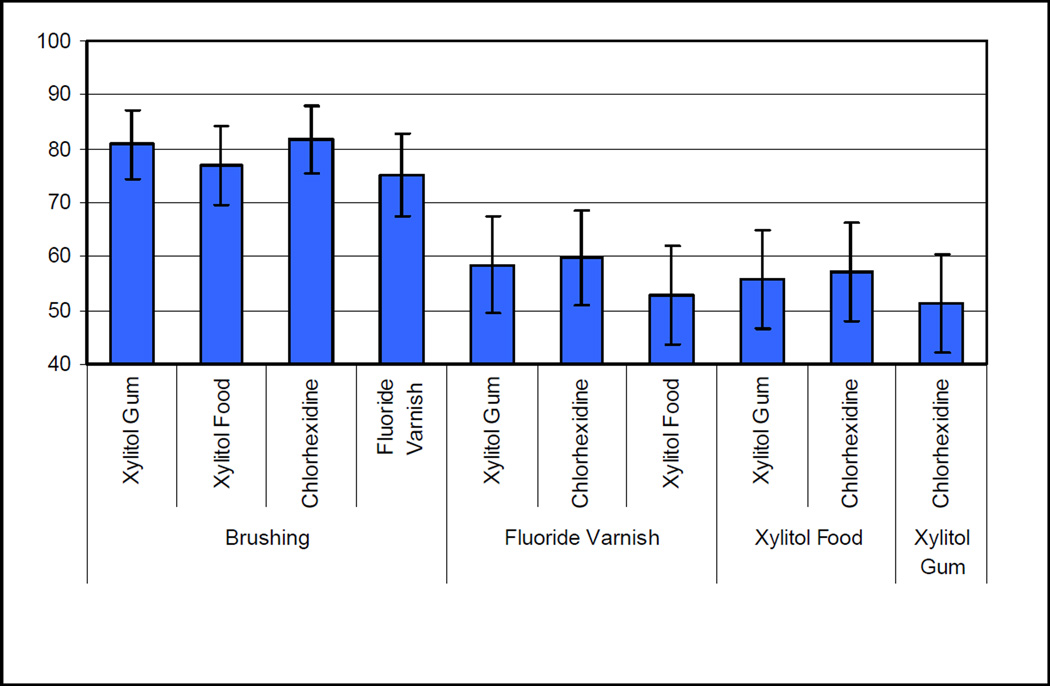
Figure 1 illustrates the sample preferences within each treatment pair; bars with 95% confidence intervals not crossing 50% were significantly more preferred. TB was significantly preferred over each of the four other treatment options (all p < 0.001). FV was significantly preferred over XG and CHX, but not XF. Preferences between XF, XG, and CHX did not differ significantly.
Figure 1.
Paired Preferences Comparing Treatments Within Pairs (Bradley Terry Model Estimated Percents and 95% Confidence Intervals)
Error bars = 95% confidence intervals
Brushing versus all other options significantly greater than 50% (95% CI does not cross 50%)
FV versus CHX & XG significantly greater than 50%
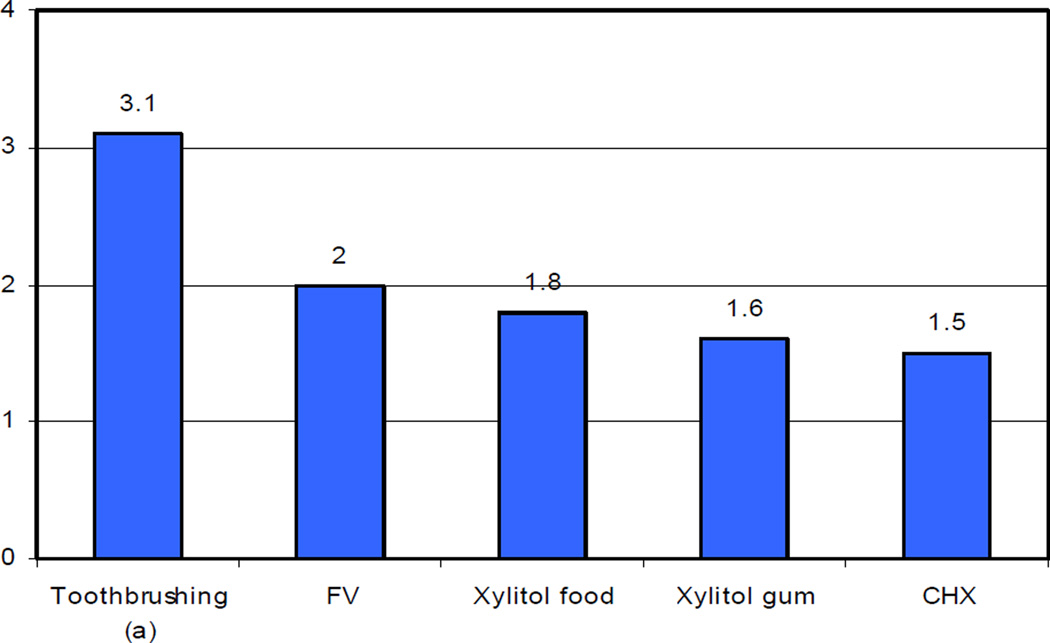
Figure 2 illustrates the summed mean preferences (summed across the 10 comparisons) for each of the five treatments. There were significant differences for the preferences (Friedman Chi Square=128.2, p < 0.001). TB (mean 3.1) was preferred over all four other treatment options (all Bonferroni-Holm p < 0.001). There were no other significant differences among other treatments. There were no significant associations between having heard of a treatment and the summed preference for the treatment. Table 4 presents the summary of the reasons for choosing each ranked treatment when compared to other treatments. Seven of the original nine constructs were present in the comments: health habits; child-target; effectiveness; convenience; multiple users; frequency; and taste. An additional new construct emerged that we labeled “concern”. An example of this was “not sure about XF”.
Figure 2.
Mean Number of Times Treatment Preferred in Paired Assessments
a = significantly greater than FV (fluoride varnish), Xylitol food, Xylitol gum, CHX (chlorhexidine); all p < 0.001;
Table 4.
Reasons for Preferences: Construct Frequencies for Each Treatment Option
| Ranked Treatment |
Total # Comments |
1st
Construct and % |
2nd
Construct and % |
3rd
Construct and % |
4th
Construct and % |
5th
Construct and % |
|||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Brushing | 149 | Healthy Habits | 56 | Child Target | 21 | Effectiveness | 11 | Convenience | 3 | Concerna | 1 |
| 2. Varnish | 84 | Effectiveness | 48 | Child Target | 25 | Convenience | 12 | Concerna | 8 | Healthy Habits | 2 |
| 3. Xylitol in Food | 63 | Child Target | 24 | Convenience | 18 | Effectiveness | 16 | Multiple Users | 11 | Concerna | 8 |
| 4. Xylitol in gum | 58 | Convenience | 41 | Concerna | 19 | Taste | 9 | Frequency | 7 | Effectiveness | 5 |
| 5. Chlorhexidine | 53 | Convenience | 30 | Effectiveness | 26 | Multiple Users | 19 | Concerna | 13 | Unhealthy Habits | 6 |
Note:
Reasons coded as concerns pertained to the treatment in each pair that was not chosen as explanation of choice of the preferred treatment.
Parents stated reasons for choosing TB were: healthy habit promotion (56%); child-targeted treatment (21%); and effectiveness (11%). Effectiveness (48%), child-target (25%) and convenience (12%) were the top three reasons given when FV was preferred. Child-target (24%), convenience (18%) and effectiveness (16%) were the top three reasons given when XF was chosen. Convenience (41%), concerns about the alternative treatment (19%) and taste (9%) were the top three reasons given when XG was chosen. Convenience (30%) effectiveness (26%) and multiple users (19%) were the top three reasons given when CHX was chosen.
DISCUSSION
This study found that a range of low-cost ECC prevention treatments were acceptable to caregivers of young African American children and that caregivers strongly preferred TB for children over the alternative treatments because it promotes healthy habits, focuses on the child, and is effective. Patient preferences and needs are cited by the American Dental Association as one of three necessary components of evidence-based dentistry, along with the best available scientific evidence and a dentist’s clinical skill and judgment (http://ebd.ada.org/about.aspx). While systematic reviews and clinical recommendations abound in dentistry, little is known about patients’ or caregivers’ treatment preferences and acceptability. This study is the first of which we are aware that identifies caregiver acceptability of and preferences for ECC preventive treatments for young African American children and it extends our earlier research on acceptability involving parents of Hispanic children (10).
Because ECC preventive behaviors should begin during infancy, the issue of parental treatment acceptability for children as early as one year of age is important. Nine out of ten caregivers in the study thought toothbrushing was acceptable for both 1–2 and 3–5 year olds, and most who preferred brushing cited developing healthy habits as the primary reason. Conversely, FV treatments were seen as widely acceptable for 3–5 year olds (94%), but significantly fewer parents (60%) found FV acceptable for 1–2 year-old children, a finding that replicates our earlier results from Hispanic parents. The primary reason given when African American parents preferred FV was that it is an effective treatment. However, the caregivers in this study showed some concern over FV safety as a reason for preferring the alternate treatments in the paired comparisons, possibly contributing to its lower acceptability for 1–2 year-old children. This finding, coupled with the relatively low overall preference rating for FV is of concern since FV is a recommended treatment for young children and infants at high risk for ECC as early as one year of age (20). One could postulate that this concern about safety stems from several distinct sources. African Americans might feel that children aged 1 – 2 years are simply too young to be exposed to any dental treatment. It could also stem from distrusting new treatments, perhaps as a legacy of the Tuskegee Project, a federal research project beginning in the 1940s in which a group of African American males with syphilis were recruited into a study of the natural progression of syphilis but were not told that they had syphilis nor were they treated for the disease. However, a recent study examining trust and willingness to participate in research found those attitudes to be similar among both African American and Hispanic adults (21). Efforts to improve the quality of health care delivery through increasing clinical cultural competence include a focus on eliminating social-cultural barriers including bias, stereotyping, and prejudice, and on providing language-congruent services (22). Such improvements in clinical care may increase trust and acceptability of health care treatments within minority populations.
The significantly lower preferences for the four alternative treatment options- FV, XF, XG and CHX- in comparison to TB, indicate lower interest in these treatments. The overall qualitative findings suggest that only toothbrushing is perceived to be associated with the development of healthy habits. In the same vein, avoiding unhealthy habits was also mentioned, although less frequently. For example, some parents commented that giving children food sweetened with xylitol contributed to the development of unhealthy (sweet tasting) eating habits. Interestingly, perceiving individual treatment effectiveness was important in preferences although we described each treatment as effective and did not indicate relative effectiveness. Convenience did not play a large role in preferring toothbrushing, indicating the relatively low importance of this aspect given the other qualities attributed to the treatment. However, in the lesser preferred treatments aimed at parents, convenience was the most frequently given explanation. In addition to expressing concerns about fluoride, parents also cited concerns about not liking the idea of xylitol, and raised questions about CHX, including its safety and whether it could be used by people who needed to avoid alcohol.
The present study replicates some of our previous findings with Hispanic families (10). Both sets of parents found the five treatments acceptable in individual assessments and both expressed significant preferences among the 5 treatments. While African American parents expressed strong preference for TB only, Hispanic parents equally preferred TB and FV treatments. Both sets of parents were less likely to rate varnish as acceptable for 1–2 year olds. However, while African American parents were equally favorable about toothbrushing for 1–2 year olds and 3–5 year olds, Hispanic families were less likely to find toothbrushing for 1–2 year olds acceptable than for 3–5 year olds. Reasons explaining preferences tended to be similar between the groups, however, no concerns were raised about the safety of treatments in the Hispanic group (17). Viewed together, our present and past research findings highlight the importance of studying acceptability issues in a manner that takes into account potential racial/ethnic differences that may affect oral health outcomes. This is consistent with previous literature addressing cultural differences among families from different racial/ethnic backgrounds that may affect dental care utilization and outcomes (23).
This study has several strengths, including the inclusion of both quantitative and qualitative responses from participants that have allowed us to gain a deeper understanding of the basic findings regarding acceptability and preferences for these preventive dental treatments. These findings add support for programs that emphasize early oral hygiene education for young children and families and may contribute to the development of future oral health promotion programs for African American families in low-income settings. The assessment methodology (11) provides a solid basis on which acceptability for additional treatments can easily be adapted.
The study also has limitations. Designed as a pilot study, the sample was small, and thus should be replicated using a larger and more socio-economically diverse sample to generalize to a broader population. In the assessment, parents were shown a video clip of FV versus a computer picture of the other treatments. It is possible that this might introduce a bias in responses, however our previous research found no indication of that (10). Additionally, more preventive treatments are available than could be included in the choices provided families for ECC prevention, and treatments that were assessed may now be available in more settings, which could influence perceptions of acceptability.
Conclusion
The strong preference for toothbrushing in this sample suggests that providing support and education in community settings about proper TB could effectively prevent ECC in low-income African American families. Efforts to increase FV acceptability in this population, in part by focusing on safety may be important to increase FV utilization. Ultimately, a decrease in ECC rates in this population will depend on the ability of researchers, educators, and dental professionals to develop and provide culturally appropriate education and care for families so that they can fully participate in the available resources and services. Optimal preventive efforts from a young age during childhood and across the life span involve important home care routines and receiving preventive dental treatments, increasingly available in a wider array of professional health care settings.
Acknowledgements
We are grateful for the support of the Berkeley-Albany YMCA Early Childhood Services Head Start Center.
The project described was supported by Award Number U54 DE14251 and a research supplement to promote Diversity in Health-Related Research from the National Institute of Dental & Craniofacial Research and Award U45 MC00023 from the Maternal and Child Health Bureau. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Dental & Craniofacial Research or the National Institutes of Health.
Footnotes
Prior Presentation: Findings in this manuscript were presented at the National Oral Health Conference in April, 2009 in Portland, OR.
References
- 1.Amercian Academy of Pediatric Dentistry. [Accessed Nov. 23, 2011]; http://www.aapd.org/media/Policies_Guidelines/D_ECC.pdf.
- 2.US Department of Health and Human and Services. Oral health in America: a report of the Surgeon General. Rockville, MD: NIDCR/NIH; 2000. [Google Scholar]
- 3.Dye BA, Tan S, Smith V, Lewis BG, Barker LK, et al. Thornton-Evans G, Trends in oral health status: United States, 1988–1994 and 1999–2004. National Center for Health Statistics. Vital Health Stat. 2007;11(248) [PubMed] [Google Scholar]
- 4.Edelstein BL. Putting Teeth in CHIP: 1997–2009 retrospective of congressional action on children’s oral health. Academic Pediatrics. 2009;(9):467–475. doi: 10.1016/j.acap.2009.09.002. [DOI] [PubMed] [Google Scholar]
- 5.Healthy Kids. [Accessed March 2011]; http://www.ihps-ca.org/publications/pdfs/Dentalutildiringerexecsum.pdf.
- 6.Berg J, Riedy CA, Tercero A. Patient and parental perception of a new fluoride varnish. Compendium. 2006;27(11):614–619. [PubMed] [Google Scholar]
- 7.Lam M, Riedy CA, Coldwell SE, Milgrom P, Craig R. Children’s acceptance of xylitol-based foods. Community Dent Oral Epidemiol. 2000;28:97–101. doi: 10.1034/j.1600-0528.2000.028002097.x. [DOI] [PubMed] [Google Scholar]
- 8.Tickle M, Milsom KM, Humphris GM, Blinkhorn AS. Parental attitudes to the care of the carious primary dentition. Br Dent J. 2003;195(8):451–255. doi: 10.1038/sj.bdj.4810600. [DOI] [PubMed] [Google Scholar]
- 9.Peretz B, Ram D. Restorative material for children’s teeth: preferences of parents and children. ASDC J. Dent Child. 2002;68(3):243–248. [PubMed] [Google Scholar]
- 10.Adams SH, Hyde S, Gansky SA. Caregiver acceptability and preferences for early childhood caries preventive treatments for Hispanic children. J Public Health Dent. 2009;69(4):217–224. doi: 10.1111/j.1752-7325.2009.00125.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hyde S, Gansky SA, Gonzalez-Vargas MJ, Husting SR, Cheng NF, Millstein SG, Adams SH. Developing an acceptability assessment of preventive dental treatments. J Public Health Dent. 2009 Winter;69(1):18–23. doi: 10.1111/j.1752-7325.2008.00088.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Reisine S, Litt M. Social and psychological theories and use for dental practice. Int Dent J. 1993;43:279–287. [PubMed] [Google Scholar]
- 13.Hyde S, Weintraub JA, Satariano WA. An evaluation of the San Francisco Department of Human Services Welfare Dental Program. J Public Health Dent. 2005;65(2):104–109. doi: 10.1111/j.1752-7325.2005.tb02794.x. [DOI] [PubMed] [Google Scholar]
- 14.Filstrup SL, Briskie D, da Fanseca M, Lawrence L, Wandera A, Inglehart MR. Early childhood caries and quality of life: child and parent perspectives. Pediatric Dent. 2003;25(5):431–440. [PubMed] [Google Scholar]
- 15.Agresti A. Categorical data analyses. 2nd Edition. New York: Wiley; 2002. [Google Scholar]
- 16.Holm S. A simple sequentially rejective multiple test procedure. Scandinavian Journal of Statistics. 1979;6:65–70. [Google Scholar]
- 17.Hyde S. Written communication. 2011 Feb [Google Scholar]
- 18.Miles MB, Huberman AM. Qualitative data analysis: an expanded sourcebook. Thousand Oaks, CA: Sage Publishers; 1994. [Google Scholar]
- 19.Bernard R. Research methods in anthropology: qualitative and quantitative approaches. Walnut Creek, London & New Delhi: AltaMira Press; 2005. [Google Scholar]
- 20.Association of State and Territorial Dental Directors. [Accessed June 9, 2011]; http://www.astdd.org/docs/Fluoride_Varnish_Policy_Statement_April_25_2010_New_Logo_2010-10.pdf.
- 21.Katz RV, Kegeles SS, Kressin NR, et al. The Tuskegee Legacy Project: willingness of minorities to participate in biomedical research. J Health Care Poor Underserved. 2006;17:698–715. doi: 10.1353/hpu.2006.0126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Betancourt JR, Green AR, Carrillo JE, Ananeh-Firempong O. Defining cultural competence: a practical framework for addressing racial/ethnic disparities in health and health care. Public Health Reports. 2003;118:293–302. doi: 10.1016/S0033-3549(04)50253-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hilton IV, Stephen S, Barker JC, Weintraub JA. Cultural factors and children’s oral health care: a qualitative study of carers of young children. Community Dent Oral Epidemiol. 2007 Dec;35(6):429–438. doi: 10.1111/j.1600-0528.2006.00356.x. [DOI] [PubMed] [Google Scholar]