Introduction
Women in the world’s developing countries are 300 times more likely to die in childbirth or from pregnancy-related complications than women in developed countries (United Nations Children’s Fund [UNICEF], 2009). It is estimated that approximately 99% of global deaths arising from pregnancy related complications occur in the developing world where there is a prevalence of high fertility rates, a shortage of skilled birth attendants, and weak health systems (UNICEF, 2009). Ten countries in Africa have the highest lifetime risk of maternal death, including Liberia (UNICEF, 2009).
Interventions for the prevention of maternal mortality, many with little success, are as varied as its causes. For example, approaches such as the training of traditional birth attendants have not accomplished stable decreases in maternal mortality (United Nations Population Fund [UNFPA], 2012; World Health Organization [WHO], 2006). Over the past twenty years, governments and aid institutions have reached a consensus that facility-based births managed by skilled birth attendants are the best means to reduce maternal mortality. Recently, the focus has shifted from single, silo interventions to a multi-pronged approach to strengthen health systems and improve access to health facilities and skilled care for improved maternal health (Abou-Zahr and Wardlaw, 2003; Campbell and Graham, 2006; Maine and Rosenfield, 1999; WHO, 2012). However, access to facilities and skilled birth attendants are often insurmountable barriers to many women.
Maternity waiting homes (MWHs) are temporary shelters for pregnant women located near a hospital or health center. MWHs have been endorsed by WHO as one component of a comprehensive package to reduce maternal morbidity and mortality (WHO, 1996). These shelters, also known as maternal waiting homes, waiting homes, or maternal waiting areas are available to pregnant women from rural areas or those at high risk for obstetric complications to help surmount the barriers of distance and time to the health center (Bhutta, et al., 2009; Stekelenburg et al., 2006; van Lonkhuijzen, et al., 2012).
MWHs have existed in various forms for over one hundred years in Europe and North America (Liebmann, 1995). In the developing world, the use of MWHs was mentioned as early as the 1950s when they were introduced in rural Nigeria (Figa-Talamanca, 1996; Liebmann, 1995; Poovan et al., 1990). Beginning in the 1960s the idea of MWHs was reenergized and promoted as a potential intervention to bridge the physical chasm that prevents rural women from receiving skilled maternal healthcare (van Lonkhuijzen et al., 2012).
MWHs are currently located in the Caribbean, South America, Central American, Africa, and Southeast Asia (van Lonkhuijzen et al., 2012). The widespread appeal of MWHs lies in the breadth of their applicability and the simplicity of the concept - a place near a clinic or hospital where women can rest and be monitored until giving birth with a skilled attendant. The use of MWHs as a residential facility near a healthcare facility has the potential to minimize the barrier of distance for pregnant women to access a skilled birth attendant (WHO, 1996).
Background
Liberia, located on the coast of West Africa, has one of the highest maternal mortality rates in the world (WHO, 2012). A Liberian woman faces a 1 in 20 risk of dying from birth-related causes over the course of her reproductive life (UNICEF, 2009). The reproductive portrait of Liberian women is marked by high fertility, early sexual debut and childbirth, and high levels of unmet contraceptive needs (Lori and Boyle, 2011).
In the aftermath of the devastating 14-year civil and rebel wars, Liberia has been left with a shattered infrastructure and some of the poorest health statistics on the continent. At the cessation of the war in 2003, the percentage of health workers was reduced by 60%, leaving only 30 doctors to serve a population of three million (WHO, 2003; United Nations Development Program [UNDP], 2006). Additionally, 95% of the country’s health facilities had been destroyed (WHO, 2003; UNDP, 2006). Basic public health services including hospitals, clinics, electricity, and potable water were ravaged by rebel forces. Many women in Liberia were exposed to gender-based violence and war crimes including sexual assault, rape, and murder (WHO, 2004). WHO estimates that since 2000 the maternal mortality rate in Liberia has almost doubled to 994/100,000 live births in 2007 (Liberia Institute of Statistics and Geo-Information Services [LISGIS], 2008; WHO, 2011). This increase in poor health outcomes is attributed to poor access to health services including such barriers as distance to health facilities, cultural preferences, and a shortage of skilled birth attendants (Lori and Starke, 2012).
In 2010, a four-year study to evaluate the effectiveness of MWHs in Liberia was funded by the United States Agency for International Development as one of six Child Survival Grants. Five clinics were chosen to receive the intervention; a MWH built next to a rural healthcare clinic. Five clinics, matched by size, location, and population demographics were chosen for the comparison group.
The purpose of this study was to examine the impact of MWHs to improve access to facility-based delivery and skilled care in rural areas of a post-conflict country. Focus groups and individual interviews with community members including users of the MWHs, non-users of MWHs, family members, clinic staff, and community leaders were utilized to provide an understanding of the structural and sociocultural factors influencing MWH use through the lens of women, families, and communities. Specifically, this study addressed two research questions:
How do women, family members, and communities understand and describe access to facility care and MWHs?
What are the structural and sociocultural factors that influence access to a MWH?
Literature Review
Maternity waiting homes have demonstrated such benefits as an increased proportion of facility-based deliveries (Cardoso, 1986), improved maternal health (Cardoso, 1986; Knowles, 1988), a lower risk of perinatal death (Chandramohan et al., 1995), decreased incidence of obstructed labour (Chandramohan et al., 1994), improved access to essential and emergency obstetric care (Eckerman, 2006), good access to healthcare (Spaans et al., 1998), and the potential to decrease rates of stillbirths (Bhutta et al., 2009; Chandramohan et al., 1995; Lee et al., 2009). Systematic reviews have concluded that MWHs have proven to be effective, but the evidence is limited because of a lack of properly designed intervention studies (Stekelenburg et al., 2006; van Lonkhuijzen et al., 2012).
There are also recognized barriers to accessing healthcare within developing countries that apply to MWHs. These include such variables as cost, location, lack of knowledge about the MWH, and cultural barriers. The cost associated with staying in a home can be prohibitive, and for all the risk, home deliveries remain the least expensive birthing option (van Lonkhuijzen et al., 2012). Indirect and direct costs pose significant and often insurmountable challenges to many would-be service users.
In Ghana, a MWH built in an abandoned hospital suffered from very low use (Wilson et al., 1997). The low use of the MWH facility was mainly attributed to its deserted surroundings and distance from the hospital (Wilson et al., 1997). Meanwhile, a MWH in Timor-Leste failed to improve access to facility-based deliveries for women who lived farther from the facility in more remote locations (Wild et al., 2012). In rural or isolated areas, women and communities may be unaware of a home’s existence or its uses. In these contexts, the most expedient manner in which to instill knowledge of the home and its services can be through social networks.
A study of a failed intervention in Kenya revealed the majority of women surveyed stated they would need their husband’s approval to use the MWH (Mramba et al., 2010), indicating the importance of family and community support, regardless of whether the intervention was initiated by the community or an external organization. Homes act as a proxy for facility-based births, yet traditional birthing practices may mean that facility-based births are unacceptable due to separation from family and lack of privacy.
The largest study to date, conducted in Ethiopia, cited that acceptance and support by the local community is vital and attributed the success of their MWH to community links (Kelly et al., 2010). Incorporating women’s needs for comfort by integrating cultural practices helps to negotiate the space between these systems while maintaining positive outcomes. Traditional birth attendants encouraging and referring a woman to MWHs was cited in an Eritrean study as an influential factor in use (Andemichael et al., 2010).
Guiding Framework
Penchansky and Thomas’s (1981) five A’s of access was used as the guiding framework to examine the data. In this model, access is divided into five dimensions: availability, accessibility, accommodation, affordability, and acceptability. This seminal work, from health policy and health service research was undertaken to provide a taxonomy to describe the “fit between the patient and the healthcare system” (Penchansky and Thomas, 1981, p. 127). Specifically, availability refers to the extent a provider or facility has the requisite supplies and personnel to provide adequate services. Accessibility refers to the physical or geographic location of the provider to the patient. Precisely, how able are patients to reach the provider. Accommodation relates to the extent the health services provider and system are organized in relation to the preferences and the constraints of the patient. Affordability is determined by the willingness and ability of the patient to pay for services sought. And finally, acceptability describes how comfortable the patient feels seeking care from the provider and vice versa, especially as it relates to unalterable characteristics such as sex, social class, and ethnicity.
Methods
An exploratory, qualitative study design was used to examine perceptions of access among community members. Data were gathered using focus groups and in-depth individual interviews with key stakeholders in the domains of (a) availability, (b) accessibility, (c) accommodation, (d) affordability, and (e) acceptability. Institutional review board approval was obtained from the Institute of Social Psychology at the London School of Economics and Political Science, the University of Michigan, Health Sciences and Behavioral Sciences Review Board, and cleared with the Liberian Ministry of Health and Social Welfare.
Study Setting and Participants
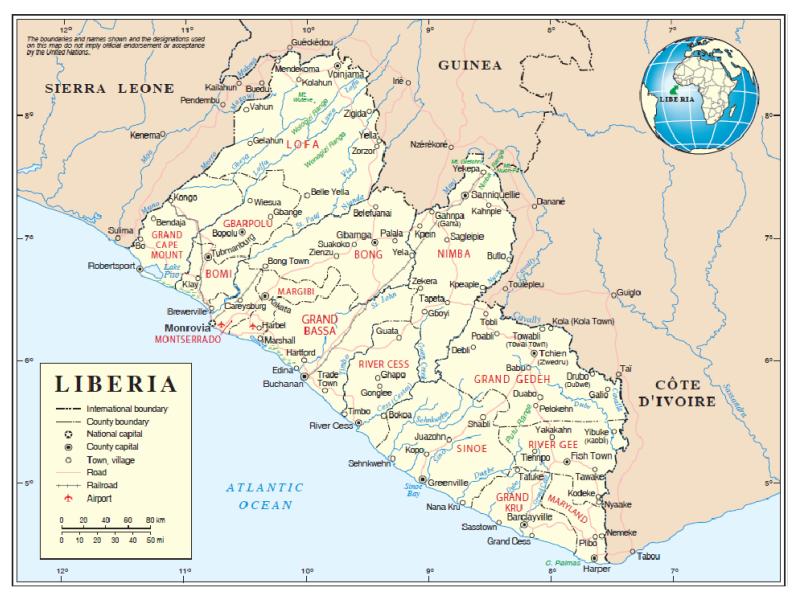
The site of the research, Bong County, is located in north central Liberia with a population of 333,481 (Figure 1). The county is primarily rural and the Kpelle tribe is the principal ethnic group. Focus groups and in-depth individual interviews were conducted over the course of three weeks in four of the five catchment areas with MWHs. In the fifth community, the MWH structure was not yet completed and thus interviews were not conducted. Each clinic serves a population of between 2,300 and 3,700 scattered in 8-12 catchment communities and is typically staffed by one registered nurse and one certified midwife. A catchment community refers to a geographical area constructed around a clinic, describing the population that uses its services (Schuurman et al., 2006).
Figure 1.
Map of Liberia
*Used with permission from the United Nations Cartographic Section
Focus groups and interviews were conducted between March and April 2012 in the four communities with open MWHs. Focus group participants included a convenience sample of: (a) MWH users with a child aged six months and under; (b) family members of MWH users; (c) MWH non-users with a child aged six months and under; and (d) MWH non-users family members. Focus group participants were recruited by clinic staff and community leaders using the following inclusion criteria: (a) able to speak English or Kpelle and (b) willing to share their own experiences and understanding of MWHs. Eleven individual, in-depth interviews were conducted with clinic staff and community leaders.
Data Collection
Prior to data collection the purpose of the interview – to understand the structural and sociocultural factors influencing MWH use – was explained to participants. Verbal informed consent was obtained and confidentiality was assured. Focus groups and interviews were held in a private space convenient to the participants near the clinic and audio taped. Prior to beginning the interviews, demographic information was collected. A total of eight focus groups were conducted across the four locations with open MWHs, consisting of six to eleven participants each (n=75). Each focus group was conducted with congruent groups including MWH users (n=2), MWH non-users (n=3), family members of MWH users (n=1), or family members of non-MWH users (n=2). An additional 11 individual, in-depth interviews were conducted with 12 clinic staff members or community leaders (one interview included two community leaders) from the four locations.
Focus groups were structured around topic guides consisting of five to eight open-ended questions and were moderated by a research assistant and a certified midwife fluent in both Kpelle and English acting as a translator and cultural broker. In-depth interviews were held with key informants to include a wide sample of individuals with authority in the community as well as knowledge about the topic of interest. Participants were provided with a meal after the completion of the focus group session or interview.
Data Analysis
Quantitative data were analyzed using descriptive statistical analyses. Simple descriptive statistics were completed using SPSS version 20.0 to describe participant demographic characteristics. Quantitative data were entered and then double checked for accuracy.
Qualitative data obtained from focus groups and interviews were transcribed verbatim. Data analysis was guided by the research questions. Using Penchansky and Thomas’s (1981) pre-defined concepts of access, the subtype of qualitative content analysis that compares data to an existing theory, was employed for analysis (Morgan, 1993). Despite this being a less common qualitative analysis approach, content analysis is useful when validating qualitative data against a pre-existing theory. This type of content analysis can also provide an expanded understanding of the concept of interest, access, while affording an opportunity to guide future interventions (Krippendorff, 2013). The analysis of transcripts was conducted using the following steps: (a) transcripts were read by all four authors for general impressions; (b) participant quotes were sorted into preliminary categories guided by the five A’s framework by two authors; (c) coding was double-checked by the two additional authors and any discrepancies were resolved; and (d) consensus on the sorted data was achieved by all four authors. We then examined the influence of each of the five A’s through the lens of promoting or deterring women’s use of the MWHs.
An audit trail and validation among authors contributed to the trustworthiness of our data (Sandelowski and Barroso, 2003). Rigor was maintained by adhering to Burns’ (1989) fours standards for methodological congruence including rigor in documentation, ethical rigor, procedural rigor, and auditability. Keeping detailed memos and notes during analysis allowed for reflection on the process and verification among the four authors. Rigor was further maintained by adhering to the procedures established by the authors, and by keeping all documents for auditability if necessary.
Findings
Sixty-one women with children under the age of six months participated in the focus group sessions (see Table 1 for select demographics). Twenty-nine women had been accommodated at one of the four MWHs and ranged in age from 13-41 years. Thirty-two women did not use a MWH prior to delivery. They ranged in age from 14-36 years.
Table 1. Characteristics of the Pregnant Women in the Focus Group Sample (n=61).
| Characteristics %(n) | MWH Users (n=29) |
MWH Non- users (n=32) |
Comparing differences between groups |
|---|---|---|---|
| Age | 13 - 41 | 14 - 36 | t=−.43, p=.668 |
| Mean | 22.65 | 23.50 | |
| Years of schooling | 0 - 11 | 0 - 8 | t=1.33, p=.188 |
| Mean | 3.14 | 2.22 | |
| Number of pregnancies | 1 - 7 | 1 - 10 | t=−.52, p=.603 |
| Mean | 2.76 | 3.03 | |
| Number of living children | 1 - 6 | 0 - 6 | t=.15, p=.884 |
| Mean | 2.66 | 2.59 | |
| Number of antenatal visits | 2 - 10 | 2 - 10 | t=.11, p=.912 |
| Mean | 4.76 | 4.71 | |
| Where was your child born? | χ2= 12.16, p=.002 | ||
| Hospital | 0 | 9.4% (3) | |
| Clinic | 100% (29) | 65.6% (21) | |
| Home | 0 | 25.0% (8) | |
| Nearest health clinic in minutes | 20 - 240 | 10 - 210 | t=.93, p=.358 |
| Mean | 113.13 | 96.53 | |
| Number of days at MWH | 1 - 10 | N/A | |
| Mean | 2.59 | N/A | |
| Who accompanied you to MWH? | |||
| TTM | 82.8% (24) | N/A | |
| Family member | 17.2% (5) | N/A | |
| Was TTM paid for her services? | χ2= .124, p=.725 | ||
| Yes | 93.1% (27) | 90.6% (29) | |
| No | 6.9% (2) | 9.4% (3) | |
| Did TTM attend birth? | |||
| Yes | 100% (29) | N/A | |
| No | 0 | N/A |
Additionally, family members (n=14) participated in the focus groups and ranged in age from 27-60 years. Twelve community leaders, six women and six men participated in in-depth individual interviews. See Tables 2 and 3 for select demographics of family members and community leaders.
Table 2. Characteristics of the Family Members in the Focus Group Sample (n=14).
| Characteristics | MWH Users (n=8) |
MWH Non- users (n=6) |
Comparing differences between groups |
|---|---|---|---|
| Age | 27 – 58 | 55 - 60 | t=−2.55, p=.034 |
| Mean | 39.86 | 56.67 | |
| Years of schooling | 0 – 10 | 0 | t=2.75, p=.028 |
| Mean | 3.88 | 0 | |
| Number of living children | 1 – 10 | 2 - 11 | t=−.35, p=.731 |
| Mean | 5.38 | 6.00 |
Table 3. Characteristics of the Participants in Individual Interview Sample (n=14).
| Characteristics %(n) | Participants |
|---|---|
| Type of community health leader | |
| Clinic Staff | 71.5% (10) |
| Community Leader | 14.3% (2) |
| NGO Staff | 7.1% (1) |
| Ministry of Health and Social Welfare Staff | 7.1% (1) |
| Gender | |
| Female | 57.1% (8) |
| Male | 42.9% (6) |
The MWHs were utilized for an average of 2-4.5 days (range 1-33 days) depending on each community. MWH users presented to the MWHs before delivery in order to be near a clinic for delivery and also stayed at the MWH in the post-partum period to recover before they made returned to their communities.
Availability
Availability of services and resources to meet the needs of patients was discussed by several participants. During the war, healthcare services were severely disrupted. There was an acute shortage of providers and clinics often lacked the basic equipment and supplies to care for the population. One Town Chief noted:
During the course of the war, we had nowhere to go. We lived in the bushes; [the rebels] beat us. When the women were pregnant, we were impoverished with nowhere to go. So you would be hiding yourself and there would be no chance of survival for that child. So now it [the maternity waiting home] is here now. We are getting our ladies here [to the maternity waiting home] happily. We are very, very happy in here. The community is very, very happy.
Another participant who worked as a staff member at one of the clinics described how the communities worked together to construct the MWH and the benefit the community is now reaping since its opening:
The community helps because to construct the building, the community provided sand, they provided bricks, they provided gravel. They help a whole lot so that the waiting home can be built, so that their sisters, their cousins, will have access to the place there…The community is very happy with the maternal waiting home being in this area. Other areas do not have access to a place like this, so they are really suffering.
Although the shortage of providers remains a problem in Liberia, rural healthcare facilities have re-opened to begin to meet the needs of the population. The addition of MWHs highlights to community members that there are now additional resources available to assist women during the puerperium. MWHs are providing a bridge for pregnant women to enter the healthcare system.
Accessibility
Accessibility or the relationship between the location of the services and the client’s ability to reach them were reflective of the poor infrastructure and abysmal road conditions faced by those in rural Liberia. Healthcare facilities serve large geographic areas, drawing clients from far afield. The barrier of distance was especially profound for many pregnant women as noted by this MWH non-user:
The community is actually thinking that the [maternity waiting] house will serve the people and will help to relieve some of the problem of women walking distance and not coming to the clinic to deliver. The house is saving the people and they are happy about the house.
Another MWH non-user echoed the concern about distance to the clinic and how the MWH was addressing this issue:
The barriers of distance for some of them to even come for visits with the certified midwife, sometimes they have to stay late and they go back home. So some would just be reluctant. But for the presence of this [maternity waiting] home, they think it will help to serve that purpose. And when women are critical they can stay…so you won’t have that stress of having your relatives transport you at night to the next referral level.
Once a woman begins labour it is difficult for her to get to the clinic. There are very few cars and roads are often impassible, especially in the rainy season. One clinic staff member noted the following:
Some of the problems that they face, one of them is the distance to walk when they are in their ninth month. To walk the distance can give them a hard time most of the time. But we really advise them that if they are into the ninth, they should come as soon as possible. Do not wait until the last minute to come.
The MWH provides the opportunity for women to come closer to the clinic before labour starts, avoiding the reluctance to walk several miles after contractions begin. It lessens the geographic barrier of distance by making accessibility to skilled care more fluid – women can come early and know they have a place to stay until labour begins.
Accommodation
The relationship of the ability of the facility to meet the client’s needs is a function of accommodation. The women were able to bring their family members, children, and traditional midwives to stay with them in the MWH. There are no restrictions on the number of individuals who can accompany a woman to the MWH since each MWH had four to five rooms with two beds; however, if the MWH is full, women are asked to limit the number of individuals remaining with them. In most cases, the pregnant woman’s other children are cared for by female relatives in their home. The role of traditional midwives in Liberia is central to the positive aspects of accommodation as described here by a clinic staff member:
Because we have our TTMs [trained traditional midwives] that we talk to. Because [the women] relate to the TTMs more than us, because the TTMs are with them in community…. So we talk with our TTMs that as soon as the woman will call you, bring her to the clinic.
The importance of men’s roles was also acknowledged in the ability of a facility to accommodate pregnant women from the community: “Yes, the community is very happy with the maternal waiting home, because the men in the community, when the women are here, they feel free that the women are secure.” A clinic staff member supported this by saying, “They say their husbands tell them they are happy that they have a house. So when they have their next pregnancy, they will come here.”
But men can also prevent a woman from utilizing the MWH as this non-user noted, “And when the husband does not support you coming here, you will not come on your own.” Another family member of a non-user also stated:
So coming to the waiting home for some of them is like creating additional burden for them because their husbands are not in support of it, because they are not prepared to support them when they are [in the maternal waiting home].
Another barrier to accommodation identified by participants was food insecurity. Although there is a kitchen, a water pump for a source of clean water, and cooking facilities with all the necessary utensils and cookware provided at the MWHs, women and their family members are responsible for bringing the food they will consume while staying at the MWH. As noted by this MWH non-user, “And then we should help them with food at the waiting home. When the pregnant women come, what they bring is not sufficient.” The officer in charge at one of the health facilities affiliated with a MWH stated, “The food is really a problem that they think about.”
Affordability
Affordability is a strong influence on use of the MWHs in Liberia. Because most Liberians live on less than $1 per day and make their living as subsistence farmers, it is difficult to pay for healthcare. Currently, services are free at all public facilities. As identified by one clinic staff:
Yes, what really motivated them to come to the maternal waiting home, one, they have access to free lodging. Because most of the women who come here, they face problems with lodging. Two, they have free access to bathing, toilet. And they have free access to the facilities.
The idea of MWHs is spreading by word of mouth in rural Bong County, Liberia. The value of having accommodations while waiting for the birth of a child was articulated by one community leader.
All because they don’t have relatives or they don’t have a place to lodge. But once the person has got a place here or they are told that when you come here there is a place here that you will stay until you give birth, they are always happy. And I’ll tell you, it’s going to really be something great. It will really help our people. These homes are a good idea. Other people are trying to emulate this things, that’s right.
Acceptability
Acceptability reflects the patients’ as well as the providers’ attitudes toward each other’s personal characteristics. It also suggests the comfort women feel with the care they receive while at the MWH. One MWH user stated, “Because when you are close the clinic, the health professional can monitor them.” Another MWH user said the following:
It’s actually a resting place…if you have a headache you can explain to everybody and you can lie down on your bed and you will be served your medication. The [certified midwife] came and asked [us] if there was any problem with anybody, and it was okay. [I] had never had to go a distance after delivery, because [I] rested enough after [I] gave birth. [I] was treated, checked and went home. So [I] had a fine time here.
Disrespectful care and abuse at the facility level can influence acceptability in the opposite direction. The prevalence varies widely and is still not well documented (Bower and Hill, 2010). As one MWH user put it:
Some of the barriers could be women would not want to use the home because if the patient, the staff and client relationship is not built. Where the provider will not interact in a friendly way with women here at that time of their pregnancy.
Another non-user stated. “If women come, women might not want to come and stay if they are not being treated fine from the clinic staff. If the interaction and the relationship is poor, then women will not come to use the home.”
Discussion
Access or entry into the formal healthcare system through the MWHs was viewed as positive by most participants in our study. Availability of services was seen as very positive for the participants in our study. While a shortage of healthcare personnel still exists, access to a functioning clinic has greatly improved since the end of the conflict. Although distance remains a potential barrier to accessibility of healthcare, the MWHs are serving as a bridge to skilled care by providing temporary shelter near a facility staffed by professionals.
According to the 2007 Liberian Demographic and Health Survey, 63.3% of women in the north central region of Liberia, where Bong County is located, received prenatal care from a skilled provider, defined as a doctor, nurse, midwife or physician’s assistant (LISGIS, 2008). However, only 32.6% of women in this region were attended by a skilled provider at delivery (LISGIS, 2008). While increasing numbers of women are accessing prenatal care, fewer of them utilize facilities for delivery. It is therefore plausible that having a MWH located near the clinic could increase access for those women who pursue prenatal care but do not deliver at the clinic due to the barrier of distance.
While treatment at healthcare facilities is free in Liberia, our findings corroborate others who have noted cost of transportation, lost time, and food as barriers to uptake of MWH use (Wild et al., 2009; Wild et al., 2012). Affordability is measured in more detail than merely fee for service. Several participants in our study identified the issue of food insecurity as a barrier to MWH use. To address this issue, the staff at one healthcare facility planted a garden to supplement the food women brought with them to the MWH.
The dimensions of accommodation and acceptability were most impacted by sociocultural factors including the role of men as well as the relationship between providers and patients. These findings support the observation by Mramba et al. (2010) of the important role of men as well as community and family.
Word-of-mouth and referral by social networks both play an important role in how health information is transmitted in low-resource areas, and can either encourage treatment-seeking behaviors or spread misinformation and rumors (Kaler, 2010). Participants in our study discussed how they learned about the MWH from users and community members. Providing education about MWHs to women through traditional birth attendants has been cited as a way of incorporating them into the healthcare process (Kelly et al., 2010). Positive experiences in MWHs mean women will refer their friends and family members, thereby encouraging use and support for homes throughout the community (Prado and Cortez, 2011; WHO, 1996).
Limitations
This study was not without some limitations. First, all focus groups were led by a health worker which may have introduced an element of social desirability bias that influenced participants to speak favorably about the health system and the MWHs. Second, the sample was a convenient sample of individuals from one geographic location therefore results cannot be generalized outside of Bong County, Liberia. Despite the use of an audio recorder and verbatim transcription, all focus groups were translated between English and Kpelle, which may have impacted the messages received by the researchers. Regardless of these limitations, this study details the importance of considering access to maternal health services from a broader sociocultural perspective.
Conclusion
Despite the fact MWHs appear to be a key element in the chain of many maternal health interventions, little evidence exists on the sociocultural factors that influence their use. Examining access as a general concept within the specific dimensions of availability, accessibility, accommodation, affordability, and acceptability provides a way to describe the structural and sociocultural factors that influence access to a MWH and facility based birth.
Communication with target communities is necessary to ascertain the cultural taboos, expectations, barriers, and needs of the community pertaining to healthcare interventions such as MWHs (Stekelenburg et al., 2006). By examining the MWH intervention from a sociocultural perspective, communities were able to describe the contribution of MWHs to accessing skilled care for delivery at a facility level. Incorporating the role of cultural and social conditions in evaluating how, why, and when MWHs work can foster a feedback loop of the experience of users and of those who could not overcome the obstacles for use.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest Statement: The authors have no conflicts of interest to report.
Contributor Information
Jody R. Lori, Division of Health Promotion and Risk Reduction, University of Michigan, School of Nursing, 400 N. Ingalls, Room 3352, Ann Arbor, MI 48109, USA.
Anna C. Wadsworth, Health, Community and Development, Institute of Social Psychology, London School of Economics and Political Science, Houghton Street, London, UK WC2A 2AE, a.c.wadsworth@lse.ac.uk.
Michelle L. Munro, University of Michigan, School of Nursing, 400 North Ingalls, Ann Arbor, MI 48109, USA, mlmunro@umich.edu.
Sarah Rominski, Global REACH, University of Michigan, Medical School, 5124b Medical Science I Building, Ann Arbor, MI 48109, USA, sarahrom@med.umich.edu.
References
- Abou-Zahr C, Wardlaw T. Antenatal care in developing countries: Promises, achievements, and missed opportunities. 2003 Available from http://whqlibdoc.who.int/publications/2003/9241590947.pdf.
- Andemichael G, Haile B, Kosia A, Mufunda J. Maternity waiting homes: A panacea for maternal/neonatal conundrums in Eritrea. Journal of Eritrean Medical Association. 2010:18–21. Available from: http://www.ajol.info/index.php/jema/article/viewFile/52112/40740. [Google Scholar]
- Bhutta ZA, Darmstadt GL, Haws RA, Yakoob MY, Lawn JE. Delivering interventions to reduce the global burden of stillbirths: improving service supply and community demand. BMC Pregnancy Childbirth. 2009;9(Supplement 1):S7. doi: 10.1186/1471-2393-9-S1-S7. doi:10.1186/1471-2393-9-S1-S7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bower D, Hill K. Exploring Evidence for Disrespect and Abuse in Facility-Based Childbirth: A report of a landscape analysis, USAID-TRAction Project. 2010 Available from: http://www.tractionproject.org/sites/default/files/upload/RFA/Respectful%20Care%20at%20Birth%209-20-101%20Final.pdf.
- Burns N. Standards for qualitative research. Nursing Science Quarterly. 1989;2:44–52. doi: 10.1177/089431848900200112. doi: 10.1177/089431848900200112. [DOI] [PubMed] [Google Scholar]
- Campbell OMR, Graham W. Strategies for reducing maternal mortality: getting on with what works. The Lancet. 2006;368:1284–1299. doi: 10.1016/S0140-6736(06)69381-1. [DOI] [PubMed] [Google Scholar]
- Cardoso UF. Giving birth is safer now. World Health Forum. 1986;7:348–52. [Google Scholar]
- Chandramohan D, Cutts F, Chandra R. Effects of a maternity waiting home on adverse maternal outcomes and the validity of antenatal risk screening. International Journal of Gynecology & Obstetrics. 1994;46:279–284. doi: 10.1016/0020-7292(94)90406-5. [DOI] [PubMed] [Google Scholar]
- Chandramohan D, Cutts F, Millard P. The effect of stay in a maternity waiting home on perinatal mortality in rural Zimbabwe. Journal of Tropical Medicine and Hygiene. 1995;98(4):261–267. [PubMed] [Google Scholar]
- Eckermann E. Finding a ‘Safe’ Place on the Risk Continuum: A case study of pregnancy and birthing in Lao PDR. Health Sociology Review. 2006;15(4):374–386. [Google Scholar]
- Figà-Talamanca I. Maternal mortality and the problem of accessibility to obstetric care; The strategy of maternity waiting homes. Social Science & Medicine. 1996;42(10):1381–1390. doi: 10.1016/0277-9536(95)00286-3. [DOI] [PubMed] [Google Scholar]
- Kaler A. Health interventions and the persistence of rumour: The circulation of sterility stories in African public health campaigns. Social Science & Medicine. 2009;68(9):1711–1719. doi: 10.1016/j.socscimed.2009.01.038. [DOI] [PubMed] [Google Scholar]
- Kelly J, Kohls E, Poovan P, Schiffer R, Redito A, Winter H, MacArthur C. The role of a maternity waiting area (MWA) in reducing maternal mortality and stillbirths in high-risk women in rural Ethiopia. British Journal of Obstetrics and Gynaecology. 2010;117(11):1377–1383. doi: 10.1111/j.1471-0528.2010.02669.x. doi:10.1111/j.1471-0528.2010.02669. [DOI] [PubMed] [Google Scholar]
- Knowles JK. A shelter that saves mothers’ lives. World Health Forum. 1988;9:387–388. [PubMed] [Google Scholar]
- Krippendorff K. Content analysis: An introduction to methodology. 3rd ed. SAGE Publications; Thousand Oaks, CA: 2013. [Google Scholar]
- Lee A, Lawn J, Cousens S, Kumara V, Osrind D, Bhuttae Z, Wallb S, Nandakumarf A, Syedb U, Darmstata G. Linking families and facilities for care at birth: What works to avert intrapartum-related deaths? International Journal of Gynecology & Obstetrics. 2009;107(Supplement):S65–S88. doi: 10.1016/j.ijgo.2009.07.012. doi:10.1016/j.ijgo.2009.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liberia Institute of Statistics and Geo-Information Services Liberia Demographic and Health Survey 2007. 2008 Available from: http://www.measuredhs.com/pubs/pdf/FR201/FR201.pdf.
- Liebmann G. Back to the maternity home. The American Enterprise. 1995;6(1):49–55. [Google Scholar]
- Lori JR, Boyle JS. Cultural childbirth practices, beliefs and traditions in postconflict Liberia. Health Care for Women International. 2011;32(6):454–473. doi: 10.1080/07399332.2011.555831. [DOI] [PubMed] [Google Scholar]
- Lori JR, Starke A. A critical analysis of maternal morbidity and mortality in Liberia, West Africa. Midwifery. 2012;28(1):67–72. doi: 10.1016/j.midw.2010.12.001. [DOI] [PubMed] [Google Scholar]
- Maine D, Rosenfield A. The Safe Motherhood Initiative: Why has it stalled? American Journal of Public Health. 1999;89(4):480–482. doi: 10.2105/ajph.89.4.480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morgan DL. Qualitative content analysis: A guide to paths not taken. Qualitative Health Research. 1993;3:112–121. doi: 10.1177/104973239300300107. [DOI] [PubMed] [Google Scholar]
- Mramba L, Nassir F, Ondieki C, Kimanga D. Reasons for low utilization of a maternity waiting home in rural Kenya. International Journal of Gynecology and Obstetrics. 2010;108:152–153. doi: 10.1016/j.ijgo.2009.08.029. [DOI] [PubMed] [Google Scholar]
- Penchansky R, Thomas JW. The concept of access: Definition and relationship to consumer satisfaction. Medical Care. 1981;XIX(2):127–140. doi: 10.1097/00005650-198102000-00001. [DOI] [PubMed] [Google Scholar]
- Poovan P, Kifle F, Kwast B. A maternity waiting home reduces obstetric catastrophes. World Health Forum. 1990;11(4):440–445. Available from: whqlibdoc.who.int/whf/…/WHF_1990_11(4)_p440-446.pdf. [PubMed] [Google Scholar]
- Prado A, Cortez R. Maternity waiting homes and institutional birth in Nicaragua: policy options and strategic implications. International Journal of Health Planning and Management. 2011;27(2):150–166. doi: 10.1002/hpm.1107. doi: 10.1002/hpm.1007. [DOI] [PubMed] [Google Scholar]
- Sandelowski M, Barroso J. Writing the proposal for a qualitative research methodology project. Qualitative Health Research. 2003;13:781–820. doi: 10.1177/1049732303013006003. doi: 10.1177/1049732303013006003. [DOI] [PubMed] [Google Scholar]
- Schuurman N, Fiedler R, Grzybowski S, Grund D. Defining rational hospital catchments for non-urban areas based on travel-time. International Journal of Health Geographics. 2006;17(4):277–293. doi: 10.1186/1476-072X-5-43. doi:10.1186/1476-072X-5-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spaans WA, van Roosmalen J, Van Wiechen CMAG. A maternity waiting home experience in Zimbabwe. International Journal of Gynecology & Obstetrics. 1998;61(2):179–80. doi: 10.1016/s0020-7292(98)00027-7. [DOI] [PubMed] [Google Scholar]
- Stekelenburg J, van Lonkhuijzen L, Spaans W, van Roosmalen J. Maternity waiting homes in rural districts in Africa; A cornerstone of safe motherhood? Current Women’s Health Reviews. 2006;2:235–238. [Google Scholar]
- United Nations. Millennium Development Goals. 2000 Available from: http://www.un.org/millenniumgoals/
- United Nations Cartographic Section Map No. 3775, Rev. 7 United Nations, Department of Peacekeeping Operations, Cartographic Section, October 2010. Available from: http://www.un.org.proxy.lib.umich.edu/Depts/Cartographic/map/profile/liberia.pdf.
- United Nations Children’s Fund. The state of the world’s children: Maternal and newborn health. 2009 Available from: http://www.unicef.org/sowc09/docs/SOWC09-FullReport-EN.pdf.
- United Nations Development Program, Liberia and Republic of Liberia, Ministry of Planning and Economic Affairs National Human Development Report 2006. 2006 Available from: http://hdr.undp.org/en/reports/nationalreports/africa/liberia/name,3319,en.html.
- United Nations Population Fund. Safe motherhood: Overview. 2012 Available from: http://www.unfpa.org/public/cache/offonce/home/mothers/pid/4381;jsessionid=BB420E831A3CFB2063CA6E50E5E3467D.jahia01.
- van Lonkhuijzen L, Stekelenburg J, van Roosmalen J. Maternity waiting facilities for improving maternal and neonatal outcome in low-resource countries (review) Cochrane Database of Systematic Reviews. 2012:10. doi: 10.1002/14651858.CD006759.pub3. Available from: http://www.thecochranelibrary.com. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wild K, Barclay L, Kelly P. The importance of outreach birthing services: lessons from the implementation of maternity waiting homes in Timor-Leste; Paper presented at Understanding Timor-Leste: A Research Conference; Dili, Australia. 2009; Available from: http://tlstudies.org/pdfs/chp_42.pdf. [Google Scholar]
- Wild K, Barclay L, Kelly P, Martins N. The tyranny of distance: maternity waiting homes and access to birthing facilities in rural Timor-Leste. Bulletin of the World Health Organization. 2012;90:97–103. doi: 10.2471/BLT.11.088955. doi: 10.2471/BLT.11.088955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson J, Collison A, Richardson D, Kwofie G, Senah K, Tinkorang E. The maternity waiting home concept: the Nsawam, Ghana experience. International Journal of Gynecology & Obstetrics. 1997;59(2):S165–S172. doi: 10.1016/s0020-7292(97)00162-8. [DOI] [PubMed] [Google Scholar]
- Word Health Organization Country cooperation strategy at a glance: Liberia. 2011 Available from: http://www.who.int/countryfocusWHO/DGR/CCO/11.05/Liberia.
- World Health Organization Liberia. 2004 Available from: http://www.who.int/hac/crises/lbr/background/2004/LiberiaNov04.pdf.
- World Health Organization Liberia: Health/nutrition sector report. 2003 Available from: http://reliefweb.int/report/liberia/liberia-healthnutrition-sector-report.
- World Health Organization Making a difference in countries: Strategic approach to improving maternal and newborn survival and health. 2006 Available from: http://www.who.int/maternal_child_adolescent/documents/wa3102006ma/en/index.html.
- World Health Organization Maternity waiting homes: A review of experiences. 1996 Available from: http://www.who.int/reproductivehealth/publications/maternal_perinatal_health/MSM_96_21/en/index.html.
- World Health Organization Trends in maternal mortality: 1990 to 2010, WHO, UNICEF, UNFPA, and The World Bank. 2012 Available from: http://www.who.int/reproductivehealth/publications/monitoring/9789241503631/en/index.html.