Abstract
Background:
Leaving hospital against medical advice may have adverse consequences. Previous studies have been limited by evaluating specific types of patients, small sample sizes and incomplete determination of outcomes. We hypothesized that leaving hospital against medical advice would be associated with increases in subsequent readmission and death.
Methods:
In a population-based analysis involving all adults admitted to hospital and discharged alive in Manitoba from Apr. 1, 1990, to Feb. 28, 2009, we evaluated all-cause 90-day mortality and 30-day hospital readmission. We used multivariable regression, adjusted for age, sex, socioeconomic status, year of hospital admission, patient comorbidities, hospital diagnosis, past frequency of admission to hospital, having previously left hospital against medical advice and data clustering (patients with multiple admissions). For readmission, we assessed both between-person and within-person effects of leaving hospital against medical advice.
Results:
Leaving against medical advice occurred in 21 417 of 1 916 104 index hospital admissions (1.1%), and was associated with higher adjusted rates of 90-day mortality (odds ratio [OR] 2.51, 95% confidence interval [CI] 2.18–2.89), and 30-day hospital readmission (within-person OR 2.10, CI 1.99–2.21; between-person OR 3.04, CI 2.79–3.30). In our additional analyses, elevated rates of readmission and death associated with leaving against medical advice were manifest within 1 week and persisted for at least 180 days after discharge.
Interpretation:
Adults who left the hospital against medical advice had higher rates of hospital readmission and death. The persistence of these effects suggests that they are not solely a result of incomplete treatment of acute illness. Interventions aimed at reducing these effects may need to include longitudinal interventions extending beyond admission to hospital.
Patients leaving hospital against medical advice have been discussed in the medical literature for more than 50 years.1 Reported to occur in 1%–2% of patients in general hospitals,2,3 the numbers are large; in the United States, 368 000 patients left against medical advice in 2007,3 and rates higher than 10% have been documented in certain subgroups, including Canadian patients with HIV and predominantly poor residents of inner city areas.4,5 The main concern over leaving hospital against medical advice is that it may increase morbidity or mortality. Previous studies attempting to assess this effect2,4–13 have all been restricted to specific types of patients, and most studies were limited by small sample sizes and incomplete determination of outcomes. In this study, we used data that avoided these limitations to test the hypothesis that patients who leave hospital against medical advice have higher rates of hospital readmission and death.
Methods
Study design
This retrospective cohort study used population-based administrative data from Manitoba, a province with a population of 1.2 million people. These data are collected by the publicly funded health insurance system and housed at the Manitoba Centre for Health Policy. The data contain information on the use of health services for all provincial residents and are linked to census-based socioeconomic information and vital statistics. Our study was approved by the University of Manitoba Health Research Ethics Board and the Manitoba Health Information Privacy Committee.
Study population
We included all residents of Manitoba 18 years of age or older who were discharged alive from acute care hospitals after an unscheduled admission from Apr. 1, 1990, to Feb. 28, 2009. Because patients can undergo interhospital transfer within a single episode of hospital care, we combined such hospital abstracts to construct complete admissions using previously described criteria,14 with the modification that 2 abstracts were considered to belong to separate admissions if the earlier abstract indicated the patient had left against medical advice.
We designated discharges from hospital as against medical advice (AMA status) and not against medical advice (non-AMA status) according to whether the final hospital abstract from the admission contained the specific discharge separation code for having left against medical advice. We performed external validation of this coding in 291 hospital abstracts where true AMA status was determined from the nursing and physician progress notes in the hospital charts. These abstracts were randomly chosen, in a ratio of about 1:2 (AMA:non-AMA), from a database used for quality-improvement purposes of all admissions to internal medicine wards in 4 hospitals. All 198 discharges that were not patients leaving against medical advice were correctly identified in the abstracts, giving a specificity of 100% (95% confidence interval [CI] 98.2%–100%). However, only 81 of 93 AMA discharges were correctly coded in the abstracts, giving a sensitivity of 87% (95% CI = 78.5%–93.2%).
Outcome measures
Our primary outcomes were unscheduled readmission to hospital within 30 days of discharge and death within 90 days of discharge.
Statistical analysis
To assess their association with leaving against medical advice, we used multivariable regression models to adjust for potential confounding variables.
We categorized year of admission to achieve equality of admissions as 1990–1993, 1994–1998, 1999–2003 and 2004–2009. We identified the 31 comorbid conditions described by Elixhauser and colleagues15 and Quan and colleagues,16 including diagnoses listed during the index admission and admissions up to 1 year before the index admission.17
We collapsed the categories of diabetes with and without chronic complications, because this distinction was unclear in coding in Manitoba before 2006.
As a surrogate measure of socioeconomic status, we quantified average household income in the postal code of residence, divided into separate quintiles for rural and urban residents. People living where the Canadian census does not track incomes formed an eleventh category referred to as “not calculated”; most of these patients resided in nursing homes or other long-term care facilities, with a smaller portion living in penitentiaries.
We identified diagnosis as the most responsible hospital diagnosis, defined as the condition responsible for most of the hospital stay,18 and grouped diagnoses into the 18 main chapter headings of the clinical modification of the International Classification of Diseases, 9th revision.19
We evaluated 30-day hospital readmission after all unscheduled admissions to hospital from which patients left alive, referring to this unit of analysis as the index admission. We adjusted for age, sex, year of index admission, comorbid conditions, socioeconomic status, diagnosis at index admission, length of stay, the number of admissions to hospital in the 5 years before the index admission and the existence of any AMA discharges in the 5 years before the index admission.
To account for data clustering, where many patients had multiple admissions over the study period, we used general estimating equations20 with an exchangeable correlation structure and robust standard errors. When dealing with such data, it is important to note that leaving against medical advice may have different within-person and between-person influences on hospital readmission.21 Within-person effects indicate the difference in readmission risk after an AMA discharge and a non-AMA discharge for the same person; between-person effects indicate the difference in readmission risk after an AMA discharge for one person and a non-AMA discharge for a different patient with otherwise identical characteristics. We included separate variables representing these 2 effects, as described in Appendix 1 (available at www.cmaj.ca/lookup/suppl/doi:10.1503/cmaj.130029/-/DC1). We verified the absence of important multicollinearity among independent variables using variance inflation factors, which averaged 1.3 and had a maximum value of 3.3.22 To assess the robustness of our results, we performed 3 sensitivity analyses of the logistic regression modelling of 30-day readmissions by using an autoregressive instead of exchangable correlation structure in the general estimating equations model, by truncating each patient’s included admissions after the first occurrence of leaving against medical advice while omitting the previous AMA discharge covariate and by including only a single randomly chosen index admission per patient, which assessed only the between-person effect.
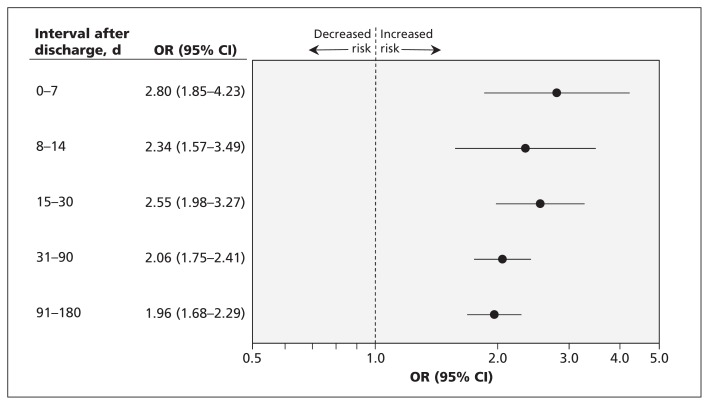
Accurately assessing the association between leaving against medical advice and 90-day mortality necessitates addressing that patients can have multiple admissions to hospital but only die once. For this purpose, we performed adjusted, matched, case–control analysis, with patients as the units of analysis. Cases were all deaths of adults aged 18–90 years that occurred during the study period among people with at least 1 hospital admission from which they were discharged alive in the 90 days before death (the eligibility period). The controls for each case were patients of the same age and sex who were alive on the date of the patient in the case group’s death, and who had at least 1 admission to hospital from which they were discharged alive in the 90 days before that date. We matched each case, without replacement, to up to 5 controls. Patients in each group were required to have survived the recent admission to hospital, because that is a precondition of having left against medical advice. To adjust for confounding in a matched analysis, we used conditional logistic regression,23 adjusting for year of admission, comorbidities, socioeconomic status, the number of admissions to hospital in the 5 years before the eligibility period and the existence of any AMA discharges in the 5 years before the eligibility period. We excluded age and sex from this regression because cases and controls were matched on those parameters. As a preplanned sensitivity analysis, we included the main hospital diagnosis in the 90-day mortality model. To further explore the association of leaving against medical advice and death, we created similar case–control models for admission to hospital within the following nonoverlapping intervals before death: 0–7, 8–14, 15–30, 31–90 and 91–180 days.
We used χ2 tests, t tests, and Mann–Whitney U tests as appropriate for univariate comparisons (SAS Institute, Cary, NC). Our data are presented as mean (± standard deviation), unless otherwise indicated, and we considered p values of less than 0.05 to be statistically significant. Our reported odds ratios (ORs) are adjusted per the multivariable regression models. Analyses were performed with SAS version 9.1.
Results
We identified 1 916 104 index admissions to hospital among 610 187 patients, 229 685 of whom (37.6%) had a single admission. Of the total number of admissions we identified, 21 417 (1.1%) ended with patients leaving against medical advice (i.e., an AMA discharge status). Unscheduled readmission within 30 days occurred after 234 809 index admissions (12.3%).
We found several differences between admissions resulting in AMA and non-AMA discharges (Table 1, Appendix 2, available at www.cmaj.ca/lookup/suppl/doi:10.1503/cmaj.130029/-/DC1). Without adjusting for these differences, AMA discharge status was associated with double the rate of unscheduled readmission to hospital within 30 days (24.0% v. 12.1%, χ2p < 0.001; Table 2). The difference in readmission rates between admissions ending with AMA and non-AMA discharges grew continuously over time; however, most of the higher readmission rate for AMA discharge status manifested early. Twenty-five percent of the cumulative difference in rates at 180 days after the index admission to hospital occurred within 1 day, and 60% occurred within 2 weeks.
Table 1:
Characteristics and outcomes of index admissions to hospital used in the analysis of hospital readmission
| Variable† | Discharge status of index admission, no. (%)* | p value‡ | |
|---|---|---|---|
| AMA n = 21 417 |
Non-AMA n = 1 894 687 |
||
| Any AMA discharges in previous 5 yr | 5 076 (23.7) | 42 537 (2.3) | < 0.001 |
| No. of admissions to hospital in previous 5 yr, mean ± SD | 3.8 (6.4) | 2.3 (4.0) | < 0.001 |
| Median (IQR) | 2 (1–4) | 1 (0–3) | < 0.001 |
| Age, yr, mean ± SD | 42.7 (18.0) | 54.1 (22.2) | < 0.001 |
| Male sex | 10 789 (50.4) | 708 491 (37.4) | < 0.001 |
| Average household income quintile | |||
| Urban 1 (lowest urban stratum) | 5 831 (27.2) | 257 035 (13.6) | < 0.001 |
| Urban 3 | 1 557 (7.3) | 185 133 (9.8) | |
| Urban 5 (highest urban stratum) | 598 (2.8) | 132 683 (7.0) | |
| Rural 1 (lowest rural stratum) | 3 864 (18.0) | 227 971 (12.0) | |
| Rural 3 | 1 534 (7.2) | 194 665 (10.3) | |
| Rural 5 (highest rural stratum) | 1 058 (4.9) | 123 465 (6.5) | |
| Not calculated | 272 (1.3) | 47 764 (2.5) | |
| Comorbid conditions | |||
| Alcohol abuse | 6 010 (28.1) | 74 756 (4.0) | < 0.001 |
| Diabetes | 3 341 (15.6) | 227 715 (12.0) | < 0.001 |
| Drug abuse | 2 397 (11.2) | 26 671 (1.4) | < 0.001 |
| Hypertension, uncomplicated | 1 888 (8.8) | 249 682 (13.2) | < 0.001 |
| Chronic pulmonary disease | 1 863 (8.7) | 174 216 (9.2) | 0.01 |
| Congestive heart failure | 1 431 (6.7) | 176 893 (9.3) | < 0.001 |
| Arrythmia | 1 041 (4.9) | 156 032 (8.2) | < 0.001 |
| Liver disease | 1 014 (4.7) | 23 001 (1.2) | < 0.001 |
| Renal failure | 775 (3.6) | 59 475 (3.1) | < 0.001 |
| Hypertension, complicated | 433 (2.0) | 33 177 (1.8) | 0.003 |
| Obesity | 380 (1.8) | 28 665 (1.5) | 0.002 |
| Solid tumour without metastasis | 346 (1.6) | 86 236 (4.6) | < 0.001 |
| Hypothyroidism | 264 (1.2) | 42 992 (2.3) | < 0.001 |
| Metastatic cancer | 254 (1.2) | 63 205 (3.3) | < 0.001 |
| AIDS/HIV | 112 (0.5) | 1 264 (0.1) | < 0.001 |
| Lymphoma | 79 (0.4) | 14 152 (0.8) | < 0.001 |
| Main diagnosis at index admission | |||
| Mental disorder | 4 645 (21.7) | 102 472 (5.4) | < 0.001 |
| Injury or poisoning | 2 862 (13.4) | 140 146 (7.4) | |
| Complication of pregnancy, childbirth or puerperium | 2 227 (10.4) | 353 508 (18.7) | |
| Disease of the digestive system | 2 196 (10.3) | 215 699 (11.4) | |
| Cardiovascular disorder | 1 921 (9.0) | 249 211 (13.2) | |
| Disease of the respiratory system | 1 445 (6.7) | 137 430 (7.3) | |
| Disease of the musculoskeletal system and connective tissue | 607 (2.8) | 91 314 (4.8) | |
| Neoplasm | 358 (1.7) | 118 334 (6.3) | |
| Disease of nervous system or sense organs | 332 (1.6) | 41 305 (2.2) | |
| Infectious or parasitic disease | 311 (1.5) | 19 007 (1.0) | |
| Disease of blood and blood-forming organs | 129 (0.6) | 13 462 (0.7) | |
| Length of index admission, d, median (IQR) | 3 (2–6) | 5 (3–9) | < 0.001 |
| Deaths within indicated intervals after discharge, d§ | |||
| 7 | 97 (0.5) | 6 956 (0.4) | 0.05 |
| 14 | 165 (0.8) | 13 145 (0.7) | 0.2 |
| 30 | 328 (1.5) | 26 600 (1.4) | 0.1 |
| 90 | 739 (3.5) | 67 860 (3.6) | 0.3 |
| 180 | 1 167 (5.5) | 111 171 (5.9) | 0.001 |
Note: AMA = left hospital against medical advice, IQR = interquartile range, non-AMA = did not leave hospital against medical advice, SD = standard deviation.
Unless otherwise indicated.
Only selected variables are shown; see Appendix 2 for full results.
χ2 test.
These are not true death rates, because the unit of measure for this analysis was admissions, not patients.
Table 2:
Rates of unscheduled readmissions to hospital after index admissions from which patients were discharged alive, by discharge status
| Time after discharge, d | Cumulative rates, % | ||
|---|---|---|---|
| Discharge status | Difference (95% CI) (AMA v. non-AMA) | ||
| AMA n = 21 417 |
non-AMA n = 1 894 687 |
||
| 1 | 5.5 | 1.2 | 4.3 (4.0–4.6) |
| 7 | 13.6 | 5.1 | 8.5 (8.1–9.0) |
| 14 | 18.1 | 7.9 | 10.2 (9.7–10.7) |
| 30 | 24.0 | 12.1 | 11.9 (11.3–12.4) |
| 60 | 30.5 | 16.9 | 13.6 (13.0–14.3) |
| 90 | 34.9 | 20.1 | 14.8 (14.1–15.4) |
| 180 | 43.3 | 26.4 | 16.9 (16.1–17.5) |
| Interval after discharge, d* | Interval-specific rates, % | ||
| Discharge status | Ratio (95% CI) (AMA:non-AMA) | ||
| AMA n = 21 417 |
non-AMA n = 1 894 687 |
||
| 0–1 | 5.5 | 1.2 | 4.7 (4.4–5.0) |
| 2–7 | 8.1 | 3.9 | 2.1 (2.0–2.2) |
| 8–14 | 4.5 | 2.8 | 1.6 (1.5–1.7) |
| 16–30 | 5.9 | 4.2 | 1.4 (1.3–1.5) |
| 31–60 | 6.6 | 4.8 | 1.4 (1.3–1.5) |
| 61–90 | 4.3 | 3.2 | 1.3 (1.3–1.4) |
| 91–181 | 8.4 | 6.3 | 1.3 (1.3–1.5) |
Note: AMA = left hospital against medical advice, CI = confidence interval, non-AMA = did not leave hospital against medical advice.
Includes first and last days of interval.
Our logistic regression model shows that AMA discharge status was associated with higher odds of readmission within 30 days (Table 3, Appendix 3, available at www.cmaj.ca/lookup/suppl/doi:10.1503/cmaj.130029/-/DC1). The within-person effect was an OR 2.10-fold higher (95% CI 1.99–2.21) when a given patient left against medical advice compared with when he or she did not. The between-person effect shows that for 2 otherwise comparable patients each having a single index admission, the patient who left against medical advice had 3.04-fold higher odds of readmission at 30 days (95% CI 2.79–3.30). Other variables associated with 30-day readmission were older age, male sex, a high number of admissions to hospital in the previous 5 years, low socioeconomic status (among both urban and rural residents), short stay in hospital, admission to hospital later in the study period and certain comorbid conditions and hospital diagnoses. The results of the sensitivity analyses were similar to those of our main model (Appendix 4, available at www.cmaj.ca/lookup/suppl/doi:10.1503/cmaj.130029/-/DC1).
Table 3:
Results of the logistic regression model for unscheduled readmission to hospital within 30 days
| Variable* | OR† (95% CI) |
|---|---|
| AMA discharge from index admission‡ | |
| Between-person effect | 3.04 (2.79–3.30) |
| Within-person effect | 2.10 (1.99–2.21) |
| Any AMA discharges in previous 5 yr | 1.25 (1.16–1.34) |
| No. of admissions in previous 5 yr (per admission) | 1.12 (1.11–1.12) |
| Age (per yr) | 1.02 (1.02–1.02) |
| Male sex | 1.08 (1.06–1.10) |
| Household income quintile | |
| Urban 1 (lowest urban stratum) | 1.00 (ref) |
| Urban 3 | 0.93 (0.90–0.95) |
| Urban 5 (highest urban stratum) | 0.82 (0.79–0.84) |
| Rural 1 (lowest rural stratum) | 1.30 (1.26–1.33) |
| Rural 3 | 1.26 (1.22–1.29) |
| Rural 5 (highest rural stratum) | 1.08 (1.05–1.12) |
| Not calculated | 0.99 (0.95–1.03) |
| Comorbid conditions§ | |
| Metastatic cancer | 3.01 (2.91–3.10) |
| Lymphoma | 2.45 (2.31–2.60) |
| AIDS/HIV | 2.41 (1.98–2.94) |
| Renal failure | 1.66 (1.60–1.72) |
| Liver disease | 1.59 (1.51–1.68) |
| Solid tumor without metastasis | 1.45 (1.41–1.50) |
| Congestive heart failure | 1.44 (1.41–1.47) |
| Drug abuse | 1.25 (1.13–1.34) |
| Diabetes | 1.21 (1.19–1.24) |
| Chronic pulmonary disease | 1.17 (1.15–1.20) |
| Arrhythmia | 1.08 (1.06–1.11) |
| Hypertension, complicated | 1.08 (1.03–1.14) |
| Hypothyroidism | 1.05 (1.00–1.10) |
| Alcohol abuse | 1.00 (0.95–1.04) |
| Hypertension, uncomplicated | 0.98 (0.96–0.99) |
| Obesity | 0.95 (0.90–1.00) |
| Main diagnosis at index admission | |
| Cardiovascular disorder | 1.00 (ref) |
| Complication of pregnancy, childbirth or puerperium | 2.11 (2.05–2.18) |
| Disease of blood or blood-forming organs | 1.17 (1.04–1.31) |
| Neoplasm | 0.94 (0.91–0.97) |
| Infectious or parasitic disease | 0.93 (0.89–0.99) |
| Disease of the digestive system | 0.93 (0.91–0.95) |
| Mental disorder | 0.92 (0.89–0.96) |
| Disease of the respiratory system | 0.90 (0.88–0.92) |
| Disease of nervous system or sense organs | 0.75 (0.70–0.80) |
| Injury or poisoning | 0.74 (0.72–0.76) |
| Disease of the musculoskeletal system or connective tissue | 0.74 (0.71–0.76) |
| Length of the index admission (per d) | 0.997 (0.997–0.998) |
Note: AMA = against medical advice, CI = confidence interval, OR = odds ratio. Comorbid conditions and diagnoses at admission are listed in descending order of OR and, thus, influence on odds of readmission.
Only selected variables are shown. Please see Appendix 3 for full results.
Adjusted for between-person and within-person AMA discharge status, age, sex, year of index admission, comorbid conditions, household income, diagnosis of the index admission, length of index admission, number of admissions in the previous 5 yr and existence of any AMA discharges in the previous 5 yr.
Within-person effects indicate the difference in readmission risk after an AMA discharge and a non-AMA discharge for the same patient. Between-person effects indicate the difference in readmission risk after an AMA discharge for one patient and a non-AMA discharge for another patient with otherwise identical characteristics.
Because a patient can have any number of comorbidities, they are represented in the regression model as individual binary indicator variables, thus no reference condition was chosen.
The case–control analysis of 90-day mortality included 45 848 cases, with at least 1 matched control for 44 837 (97.8%); 60% of cases had 5 controls, for a total of 184 210 controls. As expected, cases and controls differed substantially (Appendix 5, available at www.cmaj.ca/lookup/suppl/doi:10.1503/cmaj.130029/-/DC1). With multivariable adjustment, the odds of death were 2.51-fold higher for patients with AMA discharge status (95% CI 2.18–2.89, Table 4, Appendix 6, available at www.cmaj.ca/lookup/suppl/doi:10.1503/cmaj.130029/-/DC1). Other variables associated with death included a low number of admissions to hospital in the previous 5 years, low socioeconomic status (among both urban and rural residents), admission to hospital later in the study period and certain comorbid conditions. The association between leaving against medical advice and death was not changed when we included the main hospital diagnosis in the model (OR 2.49; 95% CI 2.16–2.87). Although the odds of death associated with AMA discharge status generally declined over the nonoverlapping intervals after discharge from hospital, it remained significantly elevated even out to 180 days (p < 0.001 for all, Figure 1).
Table 4:
Results of the conditional logistic regression model for 90-day mortality
| Variable* | OR† (95% CI) |
|---|---|
| AMA discharge from index admission | 2.51 (2.18–2.89) |
| Any AMA discharges in previous 5 yr | 0.82 (0.66–1.01) |
| No. of admissions in previous 5 yr (per admission) | 0.69 (0.68–0.69) |
| Household income quintile | |
| Urban 1 (lowest urban stratum) | 1.00 (ref) |
| Urban 2 | 0.95 (0.90–1.00) |
| Urban 3 | 0.89 (0.84–0.94) |
| Urban 4 | 0.85 (0.80–0.90) |
| Urban 5 (highest urban stratum) | 0.81 (0.76–0.87) |
| Rural 1 (lowest rural stratum) | 1.67 (1.58–1.77) |
| Rural 2 | 1.72 (1.63–1.81) |
| Rural 3 | 1.62 (1.53–1.71) |
| Rural 4 | 1.50 (1.41–1.59) |
| Rural 5 (highest rural stratum) | 1.23 (1.15–1.31) |
| Not calculated | 2.24 (2.11–2.38) |
| Comorbid conditions | |
| Metastatic cancer | 27.00 (25.82–28.23) |
| AIDS/HIV | 17.73 (11.77–26.70) |
| Lymphoma | 10.47 (9.52–11.51) |
| Liver disease | 4.51 (4.11–4.96) |
| Solid tumor without metastasis | 4.14 (3.97–4.32) |
| Renal failure | 3.40 (3.19–3.63) |
| Chronic pulmonary disease | 2.26 (2.17–2.35) |
| Drug abuse | 1.89 (1.62–2.20) |
| Diabetes | 1.86 (1.80–1.93) |
| Alcohol abuse | 1.30 (1.20–1.40) |
| Arrythmia | 1.19 (1.14–1.24) |
| Hypothyroidism | 1.05 (0.98–1.13) |
| Obesity | 0.87 (0.77–0.98) |
| Hypertension, uncomplicated | 0.86 (0.83–0.89) |
| Hypertension, complicated | 0.85 (0.78–0.92) |
Note: AMA = against medical advice, CI = confidence interval, OR = odds ratio.
Only selected variables are shown; see online Appendix 6 for full results.
Adjusted for AMA discharge status, year of index admission, comorbid conditions, household income, number of admissions in the previous 5 yr and the existence of any AMA discharges in the previous 5 yr. Exact matching occurred on age and sex.
Figure 1:
Odds of death at given intervals after hospital discharge associated with leaving hospital against medical advice. Values are derived from separate case–control regression analyses. Note: CI = confidence interval, OR = odds ratio.
Interpretation
Leaving the hospital against medical advice was associated with increased risks of readmission to hospital and death that persisted for at least 6 months. Potential mechanisms for these associations directly related to the patients’ acute illness include more severe illness or incomplete treatment of the illness. Such direct effects would be expected to manifest early and decline with time. Other mechanisms could relate to patient characteristics or behaviours that correlate with the tendency to leave hospital against medical advice; such effects could first appear early or later on, but would be expected to persist. The temporal trends we saw allow us to speculate as to these mechanisms. For both hospital readmission and death, the elevated rates among patients who left against medical advice started out high and then declined, but remained elevated to at least 180 days. This trend suggests that mechanisms both directly related to the acute illness (early), and unrelated to the acute illness (persistent) are in effect. The persistent influence may relate to intrinsic, health-related patient characteristics; one possibility is a general tendency to nonadherence with medical recommendations, which has been associated with increased mortality.24–29
Previous studies of the consequences associated with leaving hospital against medical advice, including 2 population-based studies,6,8 were restricted to selected types of patients.2,4–13 Only 4 of these studies included more than 670 AMA discharges,2,6–8 whereas we included more than 21 000 such events. In addition, most previous studies lacked complete follow-up and determination of outcomes. Three studies evaluated death related to leaving against medical advice.2,7,13 In a study involving hospitals under the direction of the US Department of Veterans Affairs, leaving against medical advice was associated with hazard ratios of 1.1 for 30- and 60-day mortality, but was only significant for the latter period.2 In data from a single hospital, 6-month mortality for AMA discharges was 19.4%, compared with 3.2% for non-AMA discharges.13 Lastly, a study involving medical patients in 2 hospitals reported ORs of 2.05–2.46 for 30-day mortality associated with leaving against medical advice, depending on the adjustment method.7 Similar to our results, 10 previous studies reported that leaving against medical advice was associated with elevated rates of readmission to hospital.2,4–12 However, all but 2 of these studies had unreliable determination of readmission rates because they only included readmission to the index hospitals.30 In those 2 studies, leaving against medical advice was associated with an OR of 2.7 for 1 month readmission among women in the postpartum period,6 and an OR of 1.9 among patients admitted for cardiovascular diseases.8
The readmission rates we saw are in line with those reported throughout Canada.31
Strengths and limitations
Our analysis relied on data from a large, population-based sample. Furthermore, we used a validated assessment of leaving against medical advice, engaged in complete follow-up and accounted for data clustering.
However, our validation of AMA discharge status in hospital abstracts was based on a small sample, and our identification of AMA status from hospital abstracts was imperfect. As discussed in Appendix 1, consequent misclassifications are not likely to alter our conclusions that leaving against medical advice is associated with harm, because misclassifications generally bias effects toward the null result of no difference between groups.
We were unable to adjust for the severity of acute illnesses because our data contained no such measure. However, this limitation is ameliorated by the overlap in predictive power between measures of acute physiologic derangement and variables for which we did adjust, including comorbidities and acute diagnosis.32–34 Furthermore, although we assessed all-cause readmissions and deaths, we do not know how many were for the same reason as the index admission.
Although we have speculated that health behaviours correlated with leaving against medical advice may be causally related to elevated mortality, we did not have data on such characteristics. In addition, ethnicity is associated with leaving against medical advice,6,35 but our administrative data do not allow its identification. This is particularly relevant in Manitoba, because the province’s large Aboriginal population is known to have poorer health outcomes than those seen in the general population.36
Patients with cancer were overrepresented in our case–control mortality analysis, but this is unlikely to have led to spurious findings because our regression model adjusted for this comorbidity. In addition, any residual bias would tend to be toward the null, because patients with malignant disease had a low rate of leaving against medical advice (0.3%) and high mortality (OR 4.1–27.0, Table 4).
Finally, our results derive from a Canadian province with a publicly-funded universal health care system and may not be generalizable to other settings.
Conclusion
Leaving hospital against medical advice can have deleterious consequences for patients, including subsequent readmisson to hospital and death. Although strategies targeted at trying to convince patients not to leave prematurely might diminish the early effects of leaving against medical advice, reducing the persistently elevated risk will likely require longitudinal interventions extending beyond hospital admission.
Supplementary Material
Acknowledgements
The authors thank the Manitoba Centre for Health Policy for use of the Population Health Research Data Repository, and Dr. Arjuna Ponnampalam for assisting with data analysis. The results and conclusions are those of the authors and no official endorsement by the Manitoba Centre for Health Policy or Manitoba Health should be inferred.
Footnotes
Competing interests: All of the authors received grant funding from the Winnipeg Health Sciences Centre Foundation and the Manitoba Health Research Council. No other competing interests were declared.
This article has been peer reviewed.
Contributors: Allan Garland, Clare Ramsey, Kendiss Olafson, Randy Fransoo, Daniel Chateau and Allen Kraut designed the study. Allan Garland drafted the article. Allan Garland, Randy Fransoo, Daniel Chateau and Marina Yogendran analyzed and interpreted the data, and revised the article for important intellectual content. Clare Ramsey, Kendiss Olafson and Allen Kraut interpreted the data and revised the article for important intellectual content. All of the authors approved the final version submitted for publication.
Funding: This study was supported by grants from the Manitoba Health Research Council and the Winnipeg Health Sciences Centre Foundation/Department of Research, which had no role in the design of the study; collection, analysis or interpretation of data; writing of the report; or the decision to submit the article for publication.
References
- 1.Roracaugh ME, Guthrie G. The personality characteristics of tuberculous patients who leave the tuberculosis hospital against medical advice. Am Rev Tuberc 1953;67:432–9 [DOI] [PubMed] [Google Scholar]
- 2.Glasgow JM, Vaughn-Sarrazin M, Kaboli P. Leaving against medical advice (AMA): risk of 30-day mortality and hospital readmission. J Gen Intern Med 2010;25:926–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Stranges E, Wier L, Merrill C, et al. Hospitalizations in which patients leave the hospital against medical advice (AMA), 2007. Rockville (MD): Agency for Healthcare Research and Quality; 2009 [PubMed] [Google Scholar]
- 4.Anis AH, Sun H, Guh D, et al. Leaving hospital against medical advice among HIV-positive patients. CMAJ 2002;167:633–7 [PMC free article] [PubMed] [Google Scholar]
- 5.Choi M, Kim H, Qian H, et al. Readmission rates of patients discharged against medical advice: a matched cohort study. PLoS ONE 2011;6:e24459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fiscella K, Meldrum S, Franks P. Postpartum discharge against medical advice: Who leaves and does it matter? Matern Child Health J 2007;11:431–6 [DOI] [PubMed] [Google Scholar]
- 7.Southern WN, Nahvi S, Arnsten J. Increased risk of mortality and readmission among patients discharged against medical advice. Am J Med 2012;125:594–602 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Onukwugha E, Mullins CD, Loh FE, et al. Readmissions after unauthorized discharges in the cardiovascular setting. Med Care 2011;49:215–24 [DOI] [PubMed] [Google Scholar]
- 9.Baptist AP, Warrier I, Arora R, et al. Hospitalized patients with asthma who leave against medical advice: characteristics, reasons, and outcomes. J Allergy Clin Immunol 2007;119:924–9 [DOI] [PubMed] [Google Scholar]
- 10.Hwang SW, Li J, Gupta R, et al. What happens to patients who leave hospital against medical advice? CMAJ 2003;168:417–20 [PMC free article] [PubMed] [Google Scholar]
- 11.Jeremiah J, O’Sullivan P, Stein MD. Who leaves against medical advice? J Gen Intern Med 1995;10:403–5 [DOI] [PubMed] [Google Scholar]
- 12.Valevski A, Zalsman G, Tsafrir S, et al. Rate of readmission and mortality risks of schizophrenia patients who were discharged against medical advice. Eur Psychiatry 2012;27:496–9 [DOI] [PubMed] [Google Scholar]
- 13.Corley MC, Link K. Men patients who leave a general hospital against medical advice; mortality rate within six months. J Stud Alcohol 1981;42:1058–61 [DOI] [PubMed] [Google Scholar]
- 14.Garland A, Fransoo R, Olafson K, et al. Creating episodes of hospital and ICU care. Winnipeg (MB): Manitoba Centre for Health Policy; 2012 [Google Scholar]
- 15.Elixhauser A, Steiner C, Harris DR, et al. Comorbidity measures for use with administrative data. Med Care 1998;36:8–27 [DOI] [PubMed] [Google Scholar]
- 16.Quan H, Sundararajan V, Halfon P, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care 2005;43:1130–9 [DOI] [PubMed] [Google Scholar]
- 17.Stukenborg GJ, Wagner D, Connors A., Jr Comparison of the performance of two comorbidity measures, with and without information from prior hospitalizations. Med Care 2001;39: 727–39 [DOI] [PubMed] [Google Scholar]
- 18.DAD Resource Intensity Weights and Expected Length of Stay. Ottawa, Ontario: Canadian Insitute for Health Information;2005 [Google Scholar]
- 19.ICD-9-CM official guidelines for coding and reporting. Washington (DC): Centers for Medicare and Medicaid Services; 2005 [Google Scholar]
- 20.Kleinbaum DG, Klein M. Logistic regression: a self-learning text. New York (NY): Springer-Verlag; 2002:327–75 [Google Scholar]
- 21.Begg MD, Parides MK. Separation of individual-level and cluster-level covariate effects in regression analysis of correlated data. Stat Med 2003;22:2591–602 [DOI] [PubMed] [Google Scholar]
- 22.Fox J. Regression diagnostics. London (UK): Sage Publications; 1991 [Google Scholar]
- 23.Kleinbaum DG, Klein M. Logistic regression: a self-learning text. New York (NY): Springer-Verlag; 2002:235–8 [Google Scholar]
- 24.Simpson SH, Eurich D, Majumdar S, et al. A meta-analysis of the association between adherence to drug therapy and mortality. BMJ 2006;333:15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.van der Wal MH, van Veldhuisen D, Veeger N, et al. Compliance with non-pharmacological recommendations and outcome in heart failure patients. Eur Heart J 2010;31:1486–93 [DOI] [PubMed] [Google Scholar]
- 26.Faught E, Duh M, Weiner J, et al. Nonadherence to antiepileptic drugs and increased mortality: findings from the RANSOM Study. Neurology 2008;71:1572–8 [DOI] [PubMed] [Google Scholar]
- 27.Ho PM, Rumsfeld J, Masoudi F, et al. Effect of medication non-adherence on hospitalization and mortality among patients with diabetes mellitus. Arch Intern Med 2006;166:1836–41 [DOI] [PubMed] [Google Scholar]
- 28.Unruh ML, Evans I, Fink N, et al. ; Choices for Healthy Outcomes in Caring for End-Stage Renal Disease (CHOICE) Study Skipped treatments, markers of nutritional nonadherence, and survival among incident hemodialysis patients. Am J Kidney Dis 2005; 46:1107–16 [DOI] [PubMed] [Google Scholar]
- 29.Vik SA, Hogan D, Patten S, et al. Medication nonadherence and subsequent risk of hospitalisation and mortality among older adults. Drugs Aging 2006;23:345–56 [DOI] [PubMed] [Google Scholar]
- 30.Nasir K, Lin Z, Bueno H, et al. Is same-hospital readmission rate a good surrogate for all-hospital readmission rate? Med Care 2010;48:477–81 [DOI] [PubMed] [Google Scholar]
- 31.Canadian Hospital Reporting Project CHRP key findings: 30-day readmission. Ottawa (ON): Canadian Institute for Health Information; 2012. Available: www.cihi.ca/cihi-ext-portal/internet/en/document/health+system+performance/indicators/performance/chrp_ireport_findings_a (accessed 2012 Apr. 17). [Google Scholar]
- 32.Quach S, Hennessy D, Faris P, et al. A comparison between the APACHE II and Charlson Index Score for predicting hospital mortality in critically ill patients. BMC Health Serv Res 2009;9:129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.van Walraven C, Austin P, Jennings A, et al. A modification of the Elixhauser comorbidity measures into a point system for hospital death using administrative data. Med Care 2009;47:626–33 [DOI] [PubMed] [Google Scholar]
- 34.Johnston JA, Wagner DP, Timmons S, et al. Impact of different measures of comorbid disease on predicted mortality of intensive care unit patients. Med Care 2002;40:929–40 [DOI] [PubMed] [Google Scholar]
- 35.Franks P, Meldrum S, Fiscella K. Discharges against medical advice: Are race/ethnicity predictors? J Gen Intern Med 2006;21: 955–60 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Martens PM, Sanderson D, Jebamani L. Mortality comparisons of First Nations to all other Manitobans: a provincial population-based look at health inequalities by region and gender. Can J Public Health 2005;96:S33–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.