Abstract
Isoflavones have been investigated in detail for their role in the prevention and therapy of prostate cancer. This is primarily because of the overwhelming data connecting high dietary isoflavone intake with reduced risk of developing prostate cancer. A number of investigations have evaluated the mechanism(s) of anticancer action of isoflavones such as genistein, daidzein, biochanin A, equol, etc., in various prostate cancer models, both in vitro and in vivo. Genistein quickly jumped to the forefront of isoflavone cancer research, but the initial enthusiasm was followed by reports on its contradictory prometastatic and tumor-promoting effects. Use of soy isoflavone mixture has been advocated as an alternative, wherein daidzein can negate harmful effects of genistein. Recent research indicates a novel role of genistein and other isoflavones in the potentiation of radiation therapy, epigenetic regulation of key tumor suppressors and oncogenes, and the modulation of miRNAs, epithelial-to-mesenchymal transition, and cancer stem cells, which has renewed the interest of cancer researchers in this class of anticancer compounds. This comprehensive review article summarizes our current understanding of the role of isoflavones in prostate cancer research.
Key words: anticancer, daidzein, genistein, isoflavone, prostate cancer
INTRODUCTION
Isoflavones are compounds related to the isoflavonoids, a class of flavonoid phenolic compounds. These natural agents have been a topic of intense medical research in the last few decades with putative beneficial roles against multiple human diseases, including cancer. Isoflavones from many novel sources are subjects of ongoing investigations, but the ones obtained from soybean are the most widely characterized and studied. In particular, isoflavone genistein (Fig. 1) is the most widely investigated isoflavone. Detailed investigations in the last 6–7 years have pointed out a few risks associated with pure genistein administration. However, a quick survey of recent literature reveals a renewed interest in isoflavones' anticancer activity. In this review article, we present a detailed overview of the anticancer potential of isoflavones, particularly in relation to their chemopreventive/therapeutic action against prostate cancer.
Fig. 1.
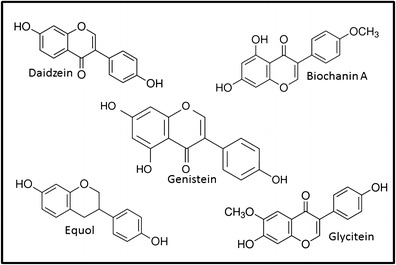
Chemical structure of major isoflavones
EPIDEMIOLOGICAL DATA
A plethora of available literature supports a connection between dietary isoflavone intake and reduced risk of prostate cancer. One of the earliest reports connecting diet with incidence of specific human cancers (1) showed the work done over a period of 10 years which revealed that the typical diets in western countries do not contain sufficient quantities of phenolic compounds from beans, pulses, and other foods, resulting in low concentrations of bioavailable isoflavonic phytoestrogens. As a clinical manifestation, it was confirmed that the subpopulations with high daily intake of isoflavones have low prostate cancer mortality (2). This study looked at urinary excretion of isoflavones in nine Japanese men before coming to the conclusions. Isoflavones were thus hypothesized to be “cancer-protective” agents. To further prove this point, a direct comparison was done between 14 men from Japan and 14 men from Finland for their plasma levels of four soy-derived isoflavones (3). It was determined that the total plasma levels of isoflavones were 7 to 100 times higher in Japanese men, with particularly high concentrations of the isoflavone genistein. An argument was made connecting soy consumption and isoflavones to low mortality from prostate cancer in Japan.
The isoflavone genistein concentration in soy foods ranges from 1 to 2 mg/g (4). Furthermore, oriental populations consume 20–80 mg genistein per day on average whereas the average consumption in the USA is just 1–3 mg genistein per day (4). This huge difference in daily uptake of genistein could explain the observed protective effects of genistein against prostate cancer in oriental populations but not in the western population. Another study (5) that quantitated genistein and genistin (beta-glucoside conjugate of genistein) put the concentrations in typical soy foods at 4.6–18.2 μg/g food for genistein and 200.6–968.1 μg/g food for genistin, in soy milk and tofu at 1.9–13.9 μg/g food for genistein and 94.8–137.7 μg/g food for genistin, and in fermented soybean products at 38.5–229.1 μg/g food for genistein and 71.7–492.8 μg/g food for genistin. This study calculated the average daily intake of genistein and genistin by the Japanese to be 1.5–4.1 and 6.3–8.3 mg/person, respectively, which was estimated to be much higher than the average daily intake by US and Western European populations. It has been estimated that at least 10% of Asians consume up to 25 g of soy protein (100 mg isoflavones)/day with Japan being the leading soy-consuming nation followed by Hong Kong and Singapore (6). The variations in isoflavone levels in different populations have been reported by other research groups as well.
These early observations generated a lot of interest in soy-derived isoflavones as anticancer agents and prompted National Cancer Institute to organize a workshop on such effects of soy foods (7). A review of all the existing data on soy isoflavones at that time indicated pleiotropic effects of genistein such as its effects on the estrogen pathway and inhibition of tyrosine kinases, DNA topoisomerases, and other signaling pathways (7). It was also recognized that a number of investigations, which included in vitro, in vivo as well as epidemiological studies, supported a protective effect of soy-derived isoflavones against human cancers, including prostate cancer. More importantly, no adverse effects of these compounds, such as tumor-promoting effects, were noted. The isoflavones from soy foods became the candidates for further mechanistic studies for their putative anticancer activity.
CELL LINE STUDIES
The realization that soy isoflavones have a role to play in chemoprevention of prostate cancer led to a number of cell line-based investigations aimed at understanding the mechanism of these compounds. In an early report on the effect of isoflavones on the growth of prostate cancer cells (8), it was reported that the isoflavones genistein and biochanin A (Fig 1) can inhibit the growth and proliferation of androgen receptor (AR)-positive LNCaP as well as AR-negative DU145 cells. A major finding of this study was that the effect of studied isoflavones did not seem to include predominantly epidermal growth factor-mediated signaling. Another study (9) looked at the effect of genistein treatment on six human prostate cancer cell lines, DU145, PC3, ND1, LNCaP, ALVA31, and JCA1, and found a growth inhibitory effect of genistein in these cells with possible mechanistic involvement of CD105 (endoglin). Endoglin is a suppressor of prostate cancer cell motility, and its expression is lost during the progression of prostate cancer. It has been demonstrated that genistein induces the reversion to a low-motility phenotype in otherwise aggressive endoglin-deficient prostate cancer cells through activation of ALK2-Smad1 endoglin-associated signaling (10). In a highly metastatic variant of PC3 cells, genistein was found to stimulate binding of focal adhesion kinase (FAK) to beta-1-integrin leading to increased cell adhesion and reduced metastasis (11). A follow-up study (12) found a lack of dependence of cell growth inhibition on cell adhesion, suggesting these to be two independent effects. It was also observed that the effects of genistein are evident at concentrations that are significantly higher than the levels attained in serum. Yet another investigation demonstrated that FAK–beta-1-integrin complex formation is independent of FAK phosphorylation and activation (13). The mechanism of genistein action has also been suggested to involve regulation of androgen receptor, TGF β1-signaling, PI3K-Akt-mTOR signaling, GSK-3 pathway; induction of glutathione peroxidase, breast cancer susceptibility genes BRCA1 and BRCA2, PTEN; and down-regulation of VEGF, MMP-2, COX-2, survivin, wnt signaling, prostate androgen-regulated transcript 1, telomerase, MDM2, uPAR, and proteasome activity.
Deregulated cell cycle and cell growth are the hallmarks of human cancers, and cell cycle arrest is one activity that is desirable for any proposed anticancer agents. Our own investigations with genistein (14) led to the findings that genistein induces apoptosis in prostate cancer cells through G2/M cell cycle arrest with concomitant down-regulation of cyclin B and up-regulation of inhibitory p21WAF1. Such G2/M arrest (15,16) and induction of p21 (16,17) by genistein have been confirmed by other researchers. Additionally, genistein has also been shown to induce inhibitory p27 (15) which also contributes to cell cycle arrest.
NF-κB is a crucial transcription factor that has been implicated in the progression of human cancers (18,19). In a study that investigated AR-positive LNCaP and AR-negative PC3 prostate cancer cells (20), we observed an inhibitory effect of genistein on NF-κB activity as evidenced by its binding to DNA. Genistein was also able to abrogate the activation of NF-κB by DNA-damaging agents. As a mechanism, we determined that genistein inhibited the phosphorylation of inhibitory I kappa B alpha which kept NF-κB bound to the inhibitory protein and unable to translocate to the nucleus. Later, we showed that genistein can inhibit Akt kinase activity which abrogates the epidermal growth factor-induced activation of Akt resulting in inactivation of NF-κB signaling (21). Inactivation of NF-κB signaling has also been linked to the potentiation action of chemotherapeutic drugs by genistein in multiple cancer cell lines, including PC3 prostate cancer cells (22).
Prostate-specific antigen (PSA) is an important biological marker for monitoring the clinical management of prostate cancer patients. In a study using VeCaP prostate cancer cell line that expresses PSA in an androgen-independent manner, we observed differential effects of genistein on PSA expression between LNCaP and VCaP cells (23). Genistein decreased PSA mRNA, protein expression, and secretion, supporting its role as a chemopreventive/therapeutic agent. The inhibitory action of isoflavones/genistein on PSA has been confirmed by other researchers as well (15). In a later study, we showed that genistein decreases the transcriptional activation of PSA by androgen-dependent as well as androgen-independent manner in LNCaP cells (24). However, in a preclinical study where 34 elderly men with elevated PSA levels were administered soy isoflavones, no effect of isoflavones on PSA was observed (25). This suggests that short-term treatment with isoflavones, particularly in people with highly elevated PSA levels, might not be effective. Another report observed a differential effect of genistein on PSA in different prostate cancer cells (26). Genistein inhibited PSA protein expression in both LNCaP and C4-2B cells but altered PSA mRNA expression in only LNCaP cells.
In addition to studies in immortalized prostate cell lines, as discussed above, there is evidence to suggest an inhibitory effect of genistein on the growth of human-patient benign prostatic hypertrophy and prostate cancer tissue as well, at doses ranging from 1.25 to 10 μg/ml (27). A number of other studies support an effect of isoflavones against prostate cancer cell lines, and a detailed discussion is beyond the scope of this article. Our own work elucidated an intricate regulation of Akt/FOXO3a/GSK-3beta/AR signaling in AR-positive prostate cancer cells (28). This study was carried out in LNCaP and C4-2B cells and revealed that isoflavones can inhibit the phosphorylation of Akt and FOXO3a, regulate Src phosphorylation, and increase GSK-3β expression, resulting in the down-regulation of AR and PSA. Furthermore, isoflavones inhibited the binding of FOXO3a to the AR promoter and increased FOXO3a binding to the p27 promoter, which resulted in altered AR and p27 expression leading to cell proliferation inhibition with induction of apoptosis in androgen-sensitive as well as androgen-insensitive prostate cancer cells.
Effect on Invasion and Metastasis
In a study that suggested a more pronounced effect of genistein against highly metastatic cells, PC3 cells were shown to be the most sensitive cells to genistein treatment as compared to less metastatic DU145 and LNCaP cells (29). Genistein was proposed to target urokinase-type plasminogen activator (uPA), a factor known to influence invasion and metastasis of human cancer cells (30). An inhibitory effect of genistein treatment was observed on the transcription of uPA, its receptor uPAR, and few metalloproteinases in PC3 and DU145 cells, demonstrating its ability to inhibit invasion-related genes in prostate cancer models (31). Xu et al. have demonstrated that genistein-mediated inhibition of prostate cancer cell invasion depends on blocking the activation of the MAP kinase-activated protein kinase 2-HSP27 pathway (32). A potent inhibition of MMP-2 in a number of prostate cancer cell lines through modulation of p38 mitogen-activated protein kinase (MAPK) has also been proposed as a mechanism of inhibition of invasion by genistein (33).
Our laboratory conducted a cDNA microarray to list the angiogenesis-, metastasis-, and invasion-related genes that are modulated by genistein in PC3 prostate cancer cells (34). A total of 832 genes were found to show >2-fold change after genistein treatment. Among these, 11 down-regulated genes (MMP-9, protease M, uPAR, VEGF, neuropilin, TSP, BPGF, LPA, TGF-beta2, TSP-1, and PAR-2) and two up-regulated genes (connective tissue growth factor and connective tissue activation peptide) were related to angiogenesis, invasion, and metastasis. Cluster analyses (35) revealed that genistein regulates the expression of genes that are critically involved in the regulation of apoptosis, cell cycle, cellular signaling, angiogenesis, invasion, and metastasis. A similar pleiotropic action of genistein on multiple signaling pathways was observed when cDNA microarray studies were conducted using LNCaP cells (36).
Working on the targets of genistein that influence metastasis in multiple prostate cancer cell lines, Xu et al. (37) observed an inhibitory effect of genistein on mitogen-activated protein kinase 4 (MEK4). MEK4 influences the invasion of cancer cells by inducing MMP-2 expression, and its inhibition by genistein ensured inhibition of invasion. Demonstrating an in vivo inhibition of metastasis of prostate cancer cells in an experimental metastasis model, Lakshman et al. noted a 96% inhibition of lung metastases when athymic mice were put on genistein diet even before the orthotropic implantation of PC3-M cells (38). Genistein was able to induce tumor levels of FAK, p38 MAPK, and HSP27.
Epithelial-to-mesenchymal transition (EMT) is recognized as an important process that is connected to cancer cell invasion and metastasis. In an in vitro study with two prostate cancer cell lines that possess mesenchymal phenotype, IA8-ARCaP and LNCaP/ HIF-1α, low doses of genistein were found to reverse the mesenchymal phenotype to epithelial phenotype, as evidenced by cell morphology and expression of EMT markers (39). As a further indirect proof, genistein treatment has been shown to attenuate insulin-like growth factor-mediated inhibition of E-cadherin, a marker of epithelial phenotype (40). The increased expression of E-cadherin is indicative of reversal of EMT by genistein in invasive PC3 cells. A recent study compared genistein and daidzein (Fig 1) for their ability to influence prostate cancer cell invasiveness, metastatic potential, and membrane fluidity, using the Matrigel system (41). Genistein was found to be better than daidzein in provoking increases in the membrane order parameter and decreasing the invasiveness. It was suggested that genistein might be anti-metastatic by virtue of its ability to modulate the mechanical properties of prostate cancer cells. Collectively, there seems to be ample evidence supporting an inhibitory action of isoflavones against prostate cancer cell invasion and metastasis in vitro.
Oxidative Damage
It has long been recognized that phytoestrogens, such as isoflavones, possess antioxidant properties that are responsible for their anticancer effects. This probably is connected to the fact that the probability of prostate cancer increases with age which also correlates with the accumulated oxidative damage in the elderly subjects. The isoflavones genistein and equol (Fig 1) have been shown to afford protection against oxidative damage at bioavailable concentrations, and such action was reported to be more effective than the established antioxidants ascorbic acid and alpha-tocopherol (42). Genistein was able to protect cells from oxidative damage by its ability to induce antioxidative genes and proteins such as glutathione reductase, microsomal glutathione S-transferase 1, and metallothionein (43). In addition to their antioxidant activity, anticancer agents have also been proposed to possess pro-oxidant activity, particularly in the presence of the transition metal copper. With the reported increased levels of copper in cancer tissues, the pro-oxidant activity leads to effective killing of cancer cells (44–46). Isoflavones genistein and biochanin A have been shown to mobilize nuclear copper in human lymphocytes, resulting in the degradation of cellular DNA. These compounds also served as antioxidants against tert-butylhydroperoxide-induced oxidative breakage (45).
Nuclear factor (erythroid-derived 2)-like 2 (Nrf2) is another transcription factor that plays an important role in the defense of cells against oxidative stress. This factor has also been suggested as a target of many antioxidant anticancer agents (47). Pharmacogenomics and gene expression profiles, influenced by soy isoflavones in the prostates of Nrf2 deficient vs. wild-type mice, revealed that soy isoflavones mainly target genes that affect cell growth, cell cycle, apoptosis, electron transport, mRNA processing, transcription factors, carbohydrate homeostasis, and phase II metabolizing enzymes, all of which are regulated by Nrf2 (48). Thus, it appears that Nrf2 plays a key role in mediating the biological activity of isoflavones.
IN VIVO STUDIES
In addition to the in vitro evidence in support of the anticancer action of isoflavones, a number of in vivo studies have also been conducted to better understand the beneficial role of isoflavones in various prostate cancer models. In support of a chemopreventive effect of soy isoflavones genistein and daidzein, pretreatment with these compounds was shown to reduce 7,12-dimethylbenz[a]anthracene (DMBA)-induced sister chromatid exchanges in female ICR mice by about 20% (49). As a direct proof in support of the notion that high isoflavone diets reduce the risk of prostate cancer, Lobund–Wistar rats were fed high vs. low isoflavone-supplemented diets before initiation by methylnitrosourea (50). The disease-free period was prolonged by 27% in rats that were fed high isoflavone-supplemented diets compared with rats fed the diet low in isoflavones. AR signaling has a unique role in the development of prostate cancer, and a study by Fritz et al. (51) confirmed the direct inhibition of AR by genistein. Male Sprague Dawley rats were fed genistein in diet, and exposure to genistein resulted in a dose-dependent down-regulation of AR mRNA expression in the dorsolateral prostate.
In a transgenic mouse model of prostate cancer (TRAMP) where all mice develop prostate tumors by 28–30 weeks of age, genistein administration was started at 5–6 weeks of age in an attempt to evaluate the in vivo anticancer efficacy of genistein (52). Serum levels of genistein in mice were observed to be in accordance with the reported serum levels in an Asian population with high soy diet, and no toxic effects were observed. Furthermore, genistein could dose dependently reduce the percentage of TRAMP mice with poorly differentiated prostate adenocarcinoma which provided clear evidence in support of the in vivo anticancer efficacy of genistein. Few other studies have confirmed such chemopreventive action of genistein in the TRAMP model. In one such study (53), dietary genistein significantly down-regulated cell proliferation, EGFR, IGF-1R, ERK-1, and ERK-2 in prostates of TRAMP mice indicating a pleiotropic action of this isoflavone in vivo. In another study (54), inhibitory action of genistein in TRAMP mice was attributed to its ability to inhibit osteopontin expression.
An early observation on the in vitro vs. in vivo discrepancy of genistein activity was noted by Naik et al. when genistein was found to be an effective inhibitor of cell growth, in both human as well as rat prostate cell lines, but failed to inhibit the growth of subcutaneously implanted rat cells in vivo (55). A study by Cohen et al. (56) found no in vivo inhibition of tumor growth by isoflavone-rich soy protein isolate in androgen-independent R-3327-AT-1 rat prostate tumor cells that were inoculated ectopically into male Copenhagen rats. As opposed to the hypothesis that an isoflavone-rich diet should inhibit tumor growth, a significant increase in tumor volume was observed. These results suggested caution before indiscriminate use of isoflavones in clinical studies, particularly in castrate-resistant prostate cancers.
Genistein has also been shown to inhibit prostate cancer stem cells, the determinants of metastasis. In one such study (57), genistein inhibited the hedgehog-gli1 pathway which might explain its ability to inhibit the growth and sustenance of prostate cancer tumorspheres. Metastasis of prostate cancer to distant organs, particularly to bones, is a huge clinical challenge. In an in vivo experimental model to study bone metastases of prostate cancer and the effect of genistein, we injected PC3 cells in human bone fragments already implanted in severe combined immunodeficiency (SCID) mice and administered genistein to these mice (58). A beneficial effect of genistein was observed in both prevention and intervention experimental setting as evidenced by significantly reduced PC3 bone tumor growth. In particular, we observed an inhibitory effect of genistein on the expression of metastasis-influencing matrix metalloproteinase MMP-9. Genistein was also found to potentiate the antitumor activity of docetaxel in the same experimental bone metastasis model through induction of osteoprotegerin and down-regulation of receptor activator of NF-κB (RANK) ligand (RANKL) and MMP-9 (59).
POTENTIATION OF RADIATION THERAPY
Radiation therapy remains an important strategy in the treatment of prostate cancer patients. With the aim to increase the efficacy of radiation therapy, we combined genistein with radiation therapy in vitro and found a significantly enhanced killing of prostate cancer cells by the combination treatment as compared to either treatment option alone (60). Genistein was able to augment the effect of radiations at doses approximately 2-fold lower to observe similar efficacy. Extending our investigations to an orthotropic prostate cancer model (61), we used genistein with and without radiation treatment and observed a significantly reduced tumor growth in mice that underwent combination treatment. These mice also had reduced lymph node metastases and better overall survival. A radiosensitizing effect of genistein on DU145 cells has been demonstrated by Yan et al. (62) where treatment with genistein led to increased cell cycle arrest and apoptosis when combined with ionizing radiation. This in vitro study confirmed our earlier results (60) on augmentation of radiation by genistein. As a mechanism for increased cell cycle arrest and cell death induced by genistein in combination with radiation therapy, we have demonstrated genistein-mediated inhibition of NF-κB activation as the crucial step that leads to altered regulation of cell cycle regulatory proteins such as cyclin B and p21 (63).
Although multiple studies have suggested a radiosensitizing effect of soy isoflavones/genistein (64), it has also been observed that treatment with genistein alone actually results in increased metastases to lymph nodes. In order to rule out the effects of the compromised immune system of SCID mice, the study was repeated in a syngeneic C57BL/6 mouse model (65). Confirming the paradox even in this model, genistein alone induced metastasis to lymph nodes but afforded significant protection when combined with radiation therapy. It was later suggested that induction of metastasis in the lymph nodes by genistein alone involves induction of HIF-1α (66). Also, a mixture of soy isoflavones (genistein + daidzein + glycitein, Fig 1) potentiated radiotherapy almost similar to genistein alone but did not induce metastasis by itself in the absence of radiation therapy. This study suggested the use of soy isoflavones, as opposed to pure genistein alone, in prostate cancer therapeutics, especially for radiosensitization (67). The targets of soy isoflavones in this model were identified to be apurinic/apyrimidinic endonuclease 1/redox factor-1 (APE1/Ref-1) and NF-κB (68). In the context of HIF-1α activation, it has since been shown that radiation induces phosphorylation of Src and STAT3 leading to induction of HIF-1alpha (69) and that pretreatment with isoflavones inhibits this pathway. In a study to elucidate the component of soy isoflavone mixture that might negate the metastasis-inducing effects of genistein alone, daidzein has been shown to be the component that protects against genistein-induced lymph node metastasis (70).
PRECLINICAL AND CLINICAL STUDIES
In a nontherapeutic clinical study designed to evaluate the effect of isoflavone administration on NF-κB activation (71), six healthy male subjects received 50 mg isoflavone mixture twice daily for 3 weeks. The isolated blood lymphocytes were exposed to TNF-α, an inducer of NF-κB, and it was observed that isoflavones afforded protection against TNF-α-induced NF-κB in addition to reducing the levels of oxidative DNA damage marker 5-hydroxymethyl-2′-deoxyuridine. In view of the reports on genetic damage in vitro by genistein, Miltyk et al. (72) recruited 20 prostate cancer patients, administered 300 mg genistein per day to them for 28 days, and then looked for several markers for genotoxicity such as DNA strand breaks, chromosomal damage, and gene translocations. It was concluded that genistein does not induce any unfavorable changes in these patients and could be investigated further in clinics. The safety and nontoxicity of isoflavones in clinical settings has since been verified by several independent investigations. Additionally, there is evidence to suggest that whereas isoflavones are bioavailable in the serum of human subjects, prostate tissue might have the ability to concentrate it further to the levels which have been shown to be protective against prostate cancer (73).
In a phase I study (74) that measured the pharmacokinetic parameters of two distinct unconjugated soy isoflavones preparations, PTI G-2535 and PTI G-4660 (which differ in genistein content—43% and 90%, respectively), cohorts of four patients were given single doses of each preparation, with doses separated by 1 week. No major toxicities were observed, and such oral administration of soy isoflavones was found to result in plasma concentrations that have been demonstrated to exhibit anti-metastatic activity in vitro. In a study that looked at 58 men at high risk of developing prostate cancer, 3 to 6 months of isoflavone intake was not found to alter prostate biomarkers, including PSA, but resulted in reduced rate of prostate cancer (75). Similarly, in a phase II randomized trial in Japanese men aged 50–75 years, isoflavone equol administration for 12 months did not show any impact on the PSA levels but reduced the incidence of prostate cancer significantly in men aged 53–65 years (28% in the isoflavone group vs. 57% in placebo) (76).
A study by deVere et al. (77) did not observe a >50% reduction in PSA levels of prostate cancer patients with mean age of 73.6 years after administration of genistein-rich extracts for 6 months which made them conclude that the use of genistein-rich extract as a sole treatment might not be useful against advanced stage prostate cancer patients. On a similar note, no beneficial effect of a 12-month 83-mg/day isoflavone treatment was seen on serum PSA concentration in seemingly healthy men aged 50–80 years (78). In a double-blind, randomized trial in 53 men who were administered 450 mg genistein, 300 mg daidzein, and other isoflavones for 6 months, no inhibitory effect of any isoflavones was observed on the PSA levels (79). However, Kumar et al. (80) noted a two-point decrease in PSA levels of 19% of patients in a study that enrolled 76 patients and administered soy isoflavones or placebo for 12 weeks. In another randomized, double-blind trial involving prostate cancer patients with rising PSA levels after radical prostatectomy or radiotherapy, administration of dietary supplements, which included soy and isoflavones, resulted in delayed PSA progression (81). A randomized trial with data from 23 men (aged 58.7 ± 7.2 years) found a 14% decline in serum PSA levels when the subjects were on high soy diet (two servings of soy per day) (82). Another phase II trial with isoflavones reported a significantly lowered PSA slope in the intervention group supporting an effect of isoflavones on PSA (83). Whereas the annual increase in PSA levels was 56% before the study, it was reduced to 20% during the year-long study. A similar beneficial effect of genistein was observed in a double-blind, randomized phase II trial where 3 to 6 weeks of administration of genistein prior to prostatectomy resulted in a 7.8% decrease in PSA levels although PSA levels increased by 4.4% in the placebo arm (84).
In a pilot study investigating soy isoflavone supplementation effects on acute and subacute toxicity of external beam radiation therapy in patients with localized prostate cancer, we found that at 3 months as well as 6 months time points, radiation therapy-induced urinary, bowel, and sexual adverse symptoms were decreased in the soy isoflavone group when compared to the radiation alone group (85). Clearly, there are some discrepancies as to the clinical benefits of soy isoflavones, but there also is ample evidence (Table I) to warrant further detailed studies to fully understand the role of either genistein alone or the soy isoflavone mixtures for benefiting prostate cancer patients in the clinical setting.
Table I.
An Overview of Preclinical and Clinical Studies on Isoflavones
| Isoflavone | Sample size | Dose | Conclusions | Ref |
|---|---|---|---|---|
| Genistein/isoflavone mixture (genistein/daidzein/glycitein) | 20 | 300 mg/day for 28 days followed by 600 mg/day for 56 days | No evidence of genetic damage | (72) |
| PTI G-2535 (43% genistein, 21% daidzein, and 3% glycitein) and PTI G-4660 (90% genistein, 9% daidzein, and 1% glycitein) | 12 | Single dose of each preparation to sequentially achieve 2, 4, and 8 mg/kg genistein with 1 week between doses | Pharmacologically relevant plasma concentrations of genistein achieved | (74) |
| Isoflavone mix (10% genistein, 6% diazein, 2% glycetin + carbohydrates/lipids/proteins) | 52 | 5 g of mix/daily for 6 months | PSA levels not reduced by more than 50% | (77) |
| 58 g/day soy drink powder containing 45.6 mg genistein, 31.7 mg daidzein, and 5.5 mg glycitein | 112 | 83 mg/ day (two 29-g packets of soy powder/day) for 12 months | PSA levels not altered in healthy men | (78) |
| Genistein | 59 | 60 mg for 12 weeks | Decrease in serum PSA levels | (80) |
| Soy isoflavones aglycones | 49 | 250 mg /day for 10 weeks | Delay in PSA progression | (81) |
| Isoflavone mixture | 23 | High and low soy diet for 3 months each with intervening 1-month washout | Decline in serum PSA levels | (82) |
| Soy protein (107 mg isoflavones) or alcohol-washed soy protein (<6 mg isoflavones) | 58 | 40 g proteins/day for 6 months | Reduced incidence of prostate cancer | (75) |
| Isoflavone mixture | 20 | 47 mg × 3 times/day for 12 months | Decline in PSA slope | (83) |
| Isoflavones (10.6 mg genistein + 13.3 mg daidzein + 3.2 mg glycitein + trace amounts of others) as 27.2 mg/tablet | 25 | 3 tablets/day for 14 days prior to radical prostatectomy | Isoflavones are concentrated in prostate tissue | (73) |
| GCP containing 9% genistein, 6% daidzein and other isoflavones | 53 | 450 mg genistein and 300 mg daidzein/day for 12 months | PSA levels not lowered | (79) |
| Genistein, daidzein, and glycitein in 1.1:1:0.2 ratio accounting for 40% of total tablet | 42 | 4 tablets (200 mg isoflavones) daily for 6 months | Reduced radiation therapy-induced adverse effects | (85) |
| Genistein (synthetic) | 47 | 30 mg/day for 3–6 weeks | Decrease in serum PSA levels | (84) |
| Isoflavone mix (major constituents in 6 mg tablet—daidzin, 1.91 mg; genistin, 0.35 mg; glycitin, 1.04 mg; malonyl daidzin, 0.81 mg; acetyl daidzin, 0.73 mg; acetyl glycitin, 0.36 mg) | 153 | 10 tablets (60 mg)/day for 12 months | Reduced incidence of prostate cancer | (76) |
PSA prostate-specific antigen, GCP genistein combined polysaccharide
EPIGENETIC REGULATION
In addition to modulation of several signaling pathways discussed above, isoflavones have also been demonstrated to mediate epigenetic changes leading to their cancer chemopreventive/therapeutic action (86). In one such report, genistein was shown to reverse DNA hypermethylation and reactivation of retinoic acid receptor beta in LNCaP and PC3 cells (87). A similar activity of other isoflavones such as daidzein and biochanin A was also observed, but genistein was found to be most effective. In one of the first reports on chromatin remodeling by genistein, Majid et al. (16) reported activation of acetylated histones 3 and 4, and H3/K4 at the p21 and p16 transcription start sites in prostate cancer cells LNCaP and DuPro after treatment with genistein. P21 promoter was found to be demethylated which is in agreement with the induction of this cell cycle-inhibitory protein by genistein. Genistein treatment also resulted in increased expression of histone acetyl transferases. Remodeling of heterochromatin domains at promoters by genistein, leading to the activation of tumor suppressor genes, is yet another way by which genistein induces epigenetic changes (88). Activation of tumor suppressors by genistein included demethylation and acetylation of H3-K9 (histone H3–lysine 9) at PTEN and CYLD promoters, and acetylation of H3-K9 at p53 and FOXO3a promoters. The H3-K9 acetylation by genistein has been confirmed in a prostate cancer model by another research group as well (89).
As epigenetic basis for regulation of AR by genistein (90), it has been reported that HDAC6, a Hsp90 deacetylase, is inhibited by genistein leading to inactivation of Hsp90 through increased acetylation. This leads to increased ubiquitination and down-regulation of AR, which is normally stabilized by chaperone activity of Hsp90. Another epigenetic regulation by which genistein inhibits the growth of prostate cancer is through inhibition of promoter methylation leading to activation of tumor suppressor B cell translocation gene 3 (91). Vardi et al. (92) compared the demethylating effect of genistein and daidzein with that of established demethylating agent 5-azacytidin in the promoter regions of glutathione S-transferase P1 (GSTP1), Ras association domain family 1, ephrin B2 (EPHB2), and BRCA1 genes. Genistein and daidzein were found to effectively induce CpG island demethylation of tumor suppressor genes, particularly GSTP1 and EPHB2 in the tested prostate cancer cell lines. Such demethylating activity of genistein and daidzein on these genes has been confirmed in another report as well (93).
REGULATION OF MICRORNAS
The microRNAs (miRNAs) are increasingly being recognized as the key regulators of major cellular events through their regulation of multiple target genes. In one of the first reports on regulation of miRNAs by isoflavones, genistein was shown to down-regulate miR-221 and miR-222 in PC3 cells leading to the induction of tumor suppressor gene ARHI (94). Increased levels of ARHI inhibited cell proliferation, colony formation, and invasion of prostate cancer cells. Our recent investigations (95) into the mechanisms of bone remodeling and bone metastases of prostate cancer have led to the observation that isoflavones can down-regulate miR-92a, a miRNA that is associated with RANKL signaling. Prostate cancer cells can stimulate differentiation of osteoclasts and osteoblasts via up-regulation of RANKL, RUNX2, and osteopontin, and this can be attenuated by isoflavones through regulation of miR-92a. Inhibition of oncogenic miR-151, resulting in up-regulation of its target tumor suppressor genes, has been proposed as another mechanism by which genistein suppresses the growth of PC3 and DU145 cells (96).
Rabiau et al. (97) confirmed the ability of isoflavones to regulate miRNA expression, when they treated LNCaP, PC3, and DU145 cells with genistein and daidzein for 48 h, and listed a number of miRNAs that were altered for their expression in these cell lines. Interestingly, genistein and daidzein treatments had similar effects as 5-azacytidine on the miRNA modulation, suggesting an epigenetic regulation by these isoflavones. The epigenetic regulation of miRNAs is relatively an untouched field in the area of chemoprevention. Working on this aspect, we recently observed a low expression of miR-29a and miR-1256 in prostate cancer cells which was a result of their methylation status (98). Treatment with isoflavones was found to demethylate the promoter sequence of these miRNAs leading to their up-regulation. This, in turn, led to an inhibition of the target genes of these miRNAs, TRIM68 and PGK-1, and an inhibition of cell growth and invasion of prostate cancer cells.
CONCLUSIONS
The wealth of literature on the anticancer potential of isoflavones, contradictory and counterintuitive at times (99), highlights their enormous potential as nontoxic chemopreventive/therapeutic agents. Moving forward, it seems the best strategy might be to investigate a mixture of these compounds, as opposed to single agents, in more detailed studies. Another strategy might be the use of novel synthetic analogs of soy isoflavones (100) with increased efficacy and reduced adverse effects. The renewed interest in these natural anticancer agents, particularly in light of their ability to modulate miRNAs, EMT, and epigenetic changes, has once again brought them into the limelight with the hope of finding their use in prostate cancer therapeutics.
ACKNOWLEDGMENTS
Part of the work cited in this article was funded by National Cancer Institute, NIH grant 5R01CA083695 (F.H. Sarkar). Further, the authors want to mention that although this is a comprehensive overview on the subject, the journal's policy of limiting the number of cited references to 100 made it extremely challenging to cite all the relevant studies on isoflavones.
Conflict of Interest
All the authors declare no conflict of interest.
REFERENCES
- 1.Adlercreutz H. Western diet and Western diseases: some hormonal and biochemical mechanisms and associations. Scand J Clin Lab Invest Suppl. 1990;201:3–23. doi: 10.3109/00365519009085798. [DOI] [PubMed] [Google Scholar]
- 2.Adlercreutz H, Honjo H, Higashi A, Fotsis T, Hamalainen E, Hasegawa T, et al. Urinary excretion of lignans and isoflavonoid phytoestrogens in Japanese men and women consuming a traditional Japanese diet. Am J Clin Nutr. 1991 Dec;54(6):1093–100. [DOI] [PubMed]
- 3.Adlercreutz H, Markkanen H, Watanabe S. Plasma concentrations of phyto-oestrogens in Japanese men. Lancet. 1993 Nov 13;342(8881):1209–10. [DOI] [PubMed]
- 4.Barnes S, Peterson TG, Coward L. Rationale for the use of genistein-containing soy matrices in chemoprevention trials for breast and prostate cancer. J Cell Biochem Suppl. 1995;22:181–7. [DOI] [PubMed]
- 5.Fukutake M, Takahashi M, Ishida K, Kawamura H, Sugimura T, Wakabayashi K. Quantification of genistein and genistin in soybeans and soybean products. Food Chem Toxicol. 1996 May;34(5):457–61. [DOI] [PubMed]
- 6.Messina M, Nagata C, Wu AH. Estimated Asian adult soy protein and isoflavone intakes. Nutr Cancer. 2006;55(1):1–12. doi: 10.1207/s15327914nc5501_1. [DOI] [PubMed] [Google Scholar]
- 7.Messina MJ, Persky V, Setchell KD, Barnes S. Soy intake and cancer risk: a review of the in vitro and in vivo data. Nutr Cancer. 1994;21(2):113–131. doi: 10.1080/01635589409514310. [DOI] [PubMed] [Google Scholar]
- 8.Peterson G, Barnes S. Genistein and biochanin A inhibit the growth of human prostate cancer cells but not epidermal growth factor receptor tyrosine autophosphorylation. Prostate. 1993;22(4):335–345. doi: 10.1002/pros.2990220408. [DOI] [PubMed] [Google Scholar]
- 9.Rokhlin OW, Cohen MB. Differential sensitivity of human prostatic cancer cell lines to the effects of protein kinase and phosphatase inhibitors. Cancer Lett. 1995 Nov 27;98(1):103–10. [PubMed]
- 10.Craft CS, Xu L, Romero D, Vary CP, Bergan RC. Genistein induces phenotypic reversion of endoglin deficiency in human prostate cancer cells. Mol Pharmacol. 2008 Jan;73(1):235–42. [DOI] [PubMed]
- 11.Bergan R, Kyle E, Nguyen P, Trepel J, Ingui C, Neckers L. Genistein-stimulated adherence of prostate cancer cells is associated with the binding of focal adhesion kinase to beta-1-integrin. Clin Exp Metastasis. 1996 Sep;14(4):389–98. [DOI] [PubMed]
- 12.Kyle E, Neckers L, Takimoto C, Curt G, Bergan R. Genistein-induced apoptosis of prostate cancer cells is preceded by a specific decrease in focal adhesion kinase activity. Mol Pharmacol. 1997 Feb;51(2):193–200. [DOI] [PubMed]
- 13.Liu Y, Kyle E, Lieberman R, Crowell J, Kellof G, Bergan RC. Focal adhesion kinase (FAK) phosphorylation is not required for genistein-induced FAK-beta-1-integrin complex formation. Clin Exp Metastasis. 2000;18(3):203–212. doi: 10.1023/A:1006729106034. [DOI] [PubMed] [Google Scholar]
- 14.Davis JN, Singh B, Bhuiyan M, Sarkar FH. Genistein-induced upregulation of p21WAF1, downregulation of cyclin B, and induction of apoptosis in prostate cancer cells. Nutr Cancer. 1998;32(3):123–131. doi: 10.1080/01635589809514730. [DOI] [PubMed] [Google Scholar]
- 15.Shen JC, Klein RD, Wei Q, Guan Y, Contois JH, Wang TT, et al. Low-dose genistein induces cyclin-dependent kinase inhibitors and G(1) cell-cycle arrest in human prostate cancer cells. Mol Carcinog. 2000 Oct;29(2):92–102. [DOI] [PubMed]
- 16.Majid S, Kikuno N, Nelles J, Noonan E, Tanaka Y, Kawamoto K, et al. Genistein induces the p21WAF1/CIP1 and p16INK4a tumor suppressor genes in prostate cancer cells by epigenetic mechanisms involving active chromatin modification. Cancer Res. 2008 Apr 15;68(8):2736–44. [DOI] [PubMed]
- 17.Rao A, Coan A, Welsh JE, Barclay WW, Koumenis C, Cramer SD. Vitamin D receptor and p21/WAF1 are targets of genistein and 1,25-dihydroxyvitamin D3 in human prostate cancer cells. Cancer Res. 2004 Mar 15;64(6):2143–7. [DOI] [PubMed]
- 18.Karin M. Nuclear factor-kappaB in cancer development and progression. Nature. 2006 May 25;441(7092):431–6. [DOI] [PubMed]
- 19.Baud V, Karin M. Is NF-kappaB a good target for cancer therapy? Hopes and pitfalls. Nat Rev Drug Discov. 2009 Jan;8(1):33–40. [DOI] [PMC free article] [PubMed]
- 20.Davis JN, Kucuk O, Sarkar FH. Genistein inhibits NF-kappa B activation in prostate cancer cells. Nutr Cancer. 1999;35(2):167–174. doi: 10.1207/S15327914NC352_11. [DOI] [PubMed] [Google Scholar]
- 21.Li Y, Sarkar FH. Inhibition of nuclear factor kappaB activation in PC3 cells by genistein is mediated via Akt signaling pathway. Clin Cancer Res. 2002 Jul;8(7):2369–77. [PubMed]
- 22.Li Y, Ahmed F, Ali S, Philip PA, Kucuk O, Sarkar FH. Inactivation of nuclear factor kappaB by soy isoflavone genistein contributes to increased apoptosis induced by chemotherapeutic agents in human cancer cells. Cancer Res. 2005 Aug 1;65(15):6934–42. [DOI] [PubMed]
- 23.Davis JN, Muqim N, Bhuiyan M, Kucuk O, Pienta KJ, Sarkar FH. Inhibition of prostate specific antigen expression by genistein in prostate cancer cells. Int J Oncol. 2000 Jun;16(6):1091–7. [DOI] [PubMed]
- 24.Davis JN, Kucuk O, Sarkar FH. Expression of prostate-specific antigen is transcriptionally regulated by genistein in prostate cancer cells. Mol Carcinog. 2002 Jun;34(2):91–101. [DOI] [PubMed]
- 25.Urban D, Irwin W, Kirk M, Markiewicz MA, Myers R, Smith M, et al. The effect of isolated soy protein on plasma biomarkers in elderly men with elevated serum prostate specific antigen. J Urol. 2001 Jan;165(1):294–300. [DOI] [PubMed]
- 26.Peternac D, Klima I, Cecchini MG, Schwaninger R, Studer UE, Thalmann GN. Agents used for chemoprevention of prostate cancer may influence PSA secretion independently of cell growth in the LNCaP model of human prostate cancer progression. Prostate. 2008 Sep 1;68(12):1307–18. [DOI] [PubMed]
- 27.Geller J, Sionit L, Partido C, Li L, Tan X, Youngkin T, et al. Genistein inhibits the growth of human-patient BPH and prostate cancer in histoculture. Prostate. 1998 Feb 1;34(2):75–9. [DOI] [PubMed]
- 28.Li Y, Wang Z, Kong D, Li R, Sarkar SH, Sarkar FH. Regulation of Akt/FOXO3a/GSK-3beta/AR signaling network by isoflavone in prostate cancer cells. J Biol Chem. 2008 Oct 10;283(41):27707–16. [DOI] [PMC free article] [PubMed]
- 29.Santibanez JF, Navarro A, Martinez J. Genistein inhibits proliferation and in vitro invasive potential of human prostatic cancer cell lines. Anticancer Res. 1997 Mar;17(2A):1199–204. [PubMed]
- 30.Dass K, Ahmad A, Azmi AS, Sarkar SH, Sarkar FH. Evolving role of uPA/uPAR system in human cancers. Cancer Treat Rev. 2008 Apr;34(2):122–36. [DOI] [PubMed]
- 31.Skogseth H, Follestad T, Larsson E, Halgunset J. Transcription levels of invasion-related genes in prostate cancer cells are modified by inhibitors of tyrosine kinase. APMIS. 2006 May;114(5):364–71. [DOI] [PubMed]
- 32.Xu L, Bergan RC. Genistein inhibits matrix metalloproteinase type 2 activation and prostate cancer cell invasion by blocking the transforming growth factor beta-mediated activation of mitogen-activated protein kinase-activated protein kinase 2-27-kDa heat shock protein pathway. Mol Pharmacol. 2006 Sep;70(3):869–77. [DOI] [PubMed]
- 33.Huang X, Chen S, Xu L, Liu Y, Deb DK, Platanias LC, et al. Genistein inhibits p38 map kinase activation, matrix metalloproteinase type 2, and cell invasion in human prostate epithelial cells. Cancer Res. 2005 Apr 15;65(8):3470–8. [DOI] [PubMed]
- 34.Li Y, Sarkar FH. Down-regulation of invasion and angiogenesis-related genes identified by cDNA microarray analysis of PC3 prostate cancer cells treated with genistein. Cancer Lett. 2002 Dec 5;186(2):157–64. [DOI] [PubMed]
- 35.Li Y, Sarkar FH. Gene expression profiles of genistein-treated PC3 prostate cancer cells. J Nutr. 2002 Dec;132(12):3623–31. [DOI] [PubMed]
- 36.Takahashi Y, Lavigne JA, Hursting SD, Chandramouli GV, Perkins SN, Barrett JC, et al. Using DNA microarray analyses to elucidate the effects of genistein in androgen-responsive prostate cancer cells: identification of novel targets. Mol Carcinog. 2004 Oct;41(2):108–19. [DOI] [PubMed]
- 37.Xu L, Ding Y, Catalona WJ, Yang XJ, Anderson WF, Jovanovic B, et al. MEK4 function, genistein treatment, and invasion of human prostate cancer cells. J Natl Cancer Inst. 2009 Aug 19;101(16):1141–55. [DOI] [PMC free article] [PubMed]
- 38.Lakshman M, Xu L, Ananthanarayanan V, Cooper J, Takimoto CH, Helenowski I, et al. Dietary genistein inhibits metastasis of human prostate cancer in mice. Cancer Res. 2008 Mar 15;68(6):2024–32. [DOI] [PubMed]
- 39.Zhang LL, Li L, Wu DP, Fan JH, Li X, Wu KJ, et al. A novel anti-cancer effect of genistein: reversal of epithelial mesenchymal transition in prostate cancer cells. Acta Pharmacol Sin. 2008 Sep;29(9):1060–8. [DOI] [PubMed]
- 40.Lee J, Ju J, Park S, Hong SJ, Yoon S. Inhibition of IGF-1 signaling by genistein: modulation of E-cadherin expression and downregulation of beta-catenin signaling in hormone refractory PC-3 prostate cancer cells. Nutr Cancer. 2012;64(1):153–162. doi: 10.1080/01635581.2012.630161. [DOI] [PubMed] [Google Scholar]
- 41.Ajdzanovic V, Mojic M, Maksimovic-Ivanic D, Bulatovic M, Mijatovic S, Milosevic V, et al. Membrane fluidity, invasiveness and dynamic phenotype of metastatic prostate cancer cells after treatment with soy isoflavones. J Membr Biol. 2013;246:307–314. doi: 10.1007/s00232-013-9531-1. [DOI] [PubMed] [Google Scholar]
- 42.Sierens J, Hartley JA, Campbell MJ, Leathem AJ, Woodside JV. Effect of phytoestrogen and antioxidant supplementation on oxidative DNA damage assessed using the comet assay. Mutat Res. 2001 Mar 7;485(2):169–76. [DOI] [PubMed]
- 43.Raschke M, Rowland IR, Magee PJ, Pool-Zobel BL. Genistein protects prostate cells against hydrogen peroxide-induced DNA damage and induces expression of genes involved in the defence against oxidative stress. Carcinogenesis. 2006 Nov;27(11):2322–30. [DOI] [PubMed]
- 44.Hadi SM, Asad SF, Singh S, Ahmad A. Putative mechanism for anticancer and apoptosis-inducing properties of plant-derived polyphenolic compounds. IUBMB Life. 2000 Sep;50(3):167–71. [DOI] [PubMed]
- 45.Ullah MF, Shamim U, Hanif S, Azmi AS, Hadi SM. Cellular DNA breakage by soy isoflavone genistein and its methylated structural analogue biochanin A. Mol Nutr Food Res. 2009 Nov;53(11):1376–85. [DOI] [PubMed]
- 46.Ullah MF, Ahmad A, Zubair H, Khan HY, Wang Z, Sarkar FH, et al. Soy isoflavone genistein induces cell death in breast cancer cells through mobilization of endogenous copper ions and generation of reactive oxygen species. Mol Nutr Food Res. 2011 Apr;55(4):553–9. [DOI] [PubMed]
- 47.Hu R, Saw CL, Yu R, Kong AN. Regulation of NF-E2-related factor 2 signaling for cancer chemoprevention: antioxidant coupled with antiinflammatory. Antioxid Redox Signal. 2010 Dec 1;13(11):1679–98. [DOI] [PMC free article] [PubMed]
- 48.Barve A, Khor TO, Nair S, Lin W, Yu S, Jain MR, et al. Pharmacogenomic profile of soy isoflavone concentrate in the prostate of Nrf2 deficient and wild-type mice. J Pharm Sci. 2008 Oct;97(10):4528–45. [DOI] [PubMed]
- 49.Giri AK, Lu LJ. Genetic damage and the inhibition of 7,12-dimethylbenz[a]anthracene-induced genetic damage by the phytoestrogens, genistein and daidzein, in female ICR mice. Cancer Lett. 1995 Aug 16;95(1–2):125–33. [DOI] [PubMed]
- 50.Pollard M, Luckert PH. Influence of isoflavones in soy protein isolates on development of induced prostate-related cancers in L-W rats. Nutr Cancer. 1997;28(1):41–5. [DOI] [PubMed]
- 51.Fritz WA, Wang J, Eltoum IE, Lamartiniere CA. Dietary genistein down-regulates androgen and estrogen receptor expression in the rat prostate. Mol Cell Endocrinol. 2002 Jan 15;186(1):89–99. [DOI] [PubMed]
- 52.Mentor-Marcel R, Lamartiniere CA, Eltoum IE, Greenberg NM, Elgavish A. Genistein in the diet reduces the incidence of poorly differentiated prostatic adenocarcinoma in transgenic mice (TRAMP). Cancer Res. 2001 Sep 15;61(18):6777–82. [PubMed]
- 53.Wang J, Eltoum IE, Lamartiniere CA. Genistein alters growth factor signaling in transgenic prostate model (TRAMP). Mol Cell Endocrinol. 2004 Apr 30;219(1–2):171–80. [DOI] [PubMed]
- 54.Mentor-Marcel R, Lamartiniere CA, Eltoum IA, Greenberg NM, Elgavish A. Dietary genistein improves survival and reduces expression of osteopontin in the prostate of transgenic mice with prostatic adenocarcinoma (TRAMP). J Nutr. 2005 May;135(5):989–95. [DOI] [PubMed]
- 55.Naik HR, Lehr JE, Pienta KJ. An in vitro and in vivo study of antitumor effects of genistein on hormone refractory prostate cancer. Anticancer Res. 1994 Nov;14(6B):2617–9. [PubMed]
- 56.Cohen LA, Zhao Z, Pittman B, Scimeca J. Effect of soy protein isolate and conjugated linoleic acid on the growth of Dunning R-3327-AT-1 rat prostate tumors. Prostate. 2003 Feb 15;54(3):169–80. [DOI] [PubMed]
- 57.Zhang L, Li L, Jiao M, Wu D, Wu K, Li X, et al. Genistein inhibits the stemness properties of prostate cancer cells through targeting Hedgehog-Gli1 pathway. Cancer Lett. 2012 Oct 1;323(1):48–57. [DOI] [PubMed]
- 58.Li Y, Che M, Bhagat S, Ellis KL, Kucuk O, Doerge DR, et al. Regulation of gene expression and inhibition of experimental prostate cancer bone metastasis by dietary genistein. Neoplasia. 2004 Jul;6(4):354–63. [DOI] [PMC free article] [PubMed]
- 59.Li Y, Kucuk O, Hussain M, Abrams J, Cher ML, Sarkar FH. Antitumor and antimetastatic activities of docetaxel are enhanced by genistein through regulation of osteoprotegerin/receptor activator of nuclear factor-kappaB (RANK)/RANK ligand/MMP-9 signaling in prostate cancer. Cancer Res. 2006 May 1;66(9):4816–25. [DOI] [PubMed]
- 60.Hillman GG, Forman JD, Kucuk O, Yudelev M, Maughan RL, Rubio J, et al. Genistein potentiates the radiation effect on prostate carcinoma cells. Clin Cancer Res. 2001 Feb;7(2):382–90. [PubMed]
- 61.Hillman GG, Wang Y, Kucuk O, Che M, Doerge DR, Yudelev M, et al. Genistein potentiates inhibition of tumor growth by radiation in a prostate cancer orthotopic model. Mol Cancer Ther. 2004 Oct;3(10):1271–9. [PubMed]
- 62.Yan SX, Ejima Y, Sasaki R, Zheng SS, Demizu Y, Soejima T, et al. Combination of genistein with ionizing radiation on androgen-independent prostate cancer cells. Asian J Androl. 2004 Dec;6(4):285–90. [PubMed]
- 63.Raffoul JJ, Wang Y, Kucuk O, Forman JD, Sarkar FH, Hillman GG. Genistein inhibits radiation-induced activation of NF-kappaB in prostate cancer cells promoting apoptosis and G2/M cell cycle arrest. BMC Cancer. 2006;6:107. doi: 10.1186/1471-2407-6-107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Hillman GG, Singh-Gupta V. Soy isoflavones sensitize cancer cells to radiotherapy. Free Radic Biol Med. 2011 Jul 15;51(2):289–98. [DOI] [PubMed]
- 65.Wang Y, Raffoul JJ, Che M, Doerge DR, Joiner MC, Kucuk O, et al. Prostate cancer treatment is enhanced by genistein in vitro and in vivo in a syngeneic orthotopic tumor model. Radiat Res. 2006 Jul;166(1 Pt 1):73–80. [DOI] [PubMed]
- 66.Raffoul JJ, Banerjee S, Che M, Knoll ZE, Doerge DR, Abrams J, et al. Soy isoflavones enhance radiotherapy in a metastatic prostate cancer model. Int J Cancer. 2007 Jun 1;120(11):2491–8. [DOI] [PubMed]
- 67.Raffoul JJ, Sarkar FH, Hillman GG. Radiosensitization of prostate cancer by soy isoflavones. Curr Cancer Drug Targets. 2007 Dec;7(8):759–65. [DOI] [PubMed]
- 68.Raffoul JJ, Banerjee S, Singh-Gupta V, Knoll ZE, Fite A, Zhang H, et al. Down-regulation of apurinic/apyrimidinic endonuclease 1/redox factor-1 expression by soy isoflavones enhances prostate cancer radiotherapy in vitro and in vivo. Cancer Res. 2007 Mar 1;67(5):2141–9. [DOI] [PubMed]
- 69.Singh-Gupta V, Zhang H, Banerjee S, Kong D, Raffoul JJ, Sarkar FH, et al. Radiation-induced HIF-1alpha cell survival pathway is inhibited by soy isoflavones in prostate cancer cells. Int J Cancer. 2009 Apr 1;124(7):1675–84. [DOI] [PMC free article] [PubMed]
- 70.Singh-Gupta V, Zhang H, Yunker CK, Ahmad Z, Zwier D, Sarkar FH, et al. Daidzein effect on hormone refractory prostate cancer in vitro and in vivo compared to genistein and soy extract: potentiation of radiotherapy. Pharm Res. 2010 Jun;27(6):1115–27. [DOI] [PubMed]
- 71.Davis JN, Kucuk O, Djuric Z, Sarkar FH. Soy isoflavone supplementation in healthy men prevents NF-kappa B activation by TNF-alpha in blood lymphocytes. Free Radic Biol Med. 2001 Jun 1;30(11):1293–302. [DOI] [PubMed]
- 72.Miltyk W, Craciunescu CN, Fischer L, Jeffcoat RA, Koch MA, Lopaczynski W, et al. Lack of significant genotoxicity of purified soy isoflavones (genistein, daidzein, and glycitein) in 20 patients with prostate cancer. Am J Clin Nutr. 2003 Apr;77(4):875–82. [DOI] [PubMed]
- 73.Gardner CD, Oelrich B, Liu JP, Feldman D, Franke AA, Brooks JD. Prostatic soy isoflavone concentrations exceed serum levels after dietary supplementation. Prostate. 2009 May 15;69(7):719–26. [DOI] [PMC free article] [PubMed]
- 74.Takimoto CH, Glover K, Huang X, Hayes SA, Gallot L, Quinn M, et al. Phase I pharmacokinetic and pharmacodynamic analysis of unconjugated soy isoflavones administered to individuals with cancer. Cancer Epidemiol Biomarkers Prev. 2003 Nov;12(11 Pt 1):1213–21. [PubMed]
- 75.Hamilton-Reeves JM, Rebello SA, Thomas W, Kurzer MS, Slaton JW. Effects of soy protein isolate consumption on prostate cancer biomarkers in men with HGPIN, ASAP, and low-grade prostate cancer. Nutr Cancer. 2008;60(1):7–13. doi: 10.1080/01635580701586770. [DOI] [PubMed] [Google Scholar]
- 76.Miyanaga N, Akaza H, Hinotsu S, Fujioka T, Naito S, Namiki M, et al. Prostate cancer chemoprevention study: an investigative randomized control study using purified isoflavones in men with rising prostate-specific antigen. Cancer Sci. 2012 Jan;103(1):125–30. [DOI] [PMC free article] [PubMed]
- 77.deVere White RW, Hackman RM, Soares SE, Beckett LA, Li Y, Sun B. Effects of a genistein-rich extract on PSA levels in men with a history of prostate cancer. Urology. 2004;63(2):259–263. doi: 10.1016/j.urology.2003.09.061. [DOI] [PubMed] [Google Scholar]
- 78.Adams KF, Chen C, Newton KM, Potter JD, Lampe JW. Soy isoflavones do not modulate prostate-specific antigen concentrations in older men in a randomized controlled trial. Cancer Epidemiol Biomarkers Prev. 2004 Apr;13(4):644–8. [PubMed]
- 79.DeVere White RW, Tsodikov A, Stapp EC, Soares SE, Fujii H, Hackman RM. Effects of a high dose, aglycone-rich soy extract on prostate-specific antigen and serum isoflavone concentrations in men with localized prostate cancer. Nutr Cancer. 2010;62(8):1036–1043. doi: 10.1080/01635581.2010.492085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Kumar NB, Cantor A, Allen K, Riccardi D, Besterman-Dahan K, Seigne J, et al. The specific role of isoflavones in reducing prostate cancer risk. Prostate. 2004 May 1;59(2):141–7. [DOI] [PubMed]
- 81.Schroder FH, Roobol MJ, Boeve ER, De MR, Zuijdgeest-van Leeuwen SD, Kersten I, et al. Randomized, double-blind, placebo-controlled crossover study in men with prostate cancer and rising PSA: effectiveness of a dietary supplement. Eur Urol. 2005;48(6):922–30. [DOI] [PubMed]
- 82.Maskarinec G, Morimoto Y, Hebshi S, Sharma S, Franke AA, Stanczyk FZ. Serum prostate-specific antigen but not testosterone levels decrease in a randomized soy intervention among men. Eur J Clin Nutr. 2006 Dec;60(12):1423–9. [DOI] [PubMed]
- 83.Pendleton JM, Tan WW, Anai S, Chang M, Hou W, Shiverick KT, et al. Phase II trial of isoflavone in prostate-specific antigen recurrent prostate cancer after previous local therapy. BMC Cancer. 2008;8:132. doi: 10.1186/1471-2407-8-132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Lazarevic B, Boezelijn G, Diep LM, Kvernrod K, Ogren O, Ramberg H, et al. Efficacy and safety of short-term genistein intervention in patients with localized prostate cancer prior to radical prostatectomy: a randomized, placebo-controlled, double-blind phase 2 clinical trial. Nutr Cancer. 2011;63(6):889–898. doi: 10.1080/01635581.2011.582221. [DOI] [PubMed] [Google Scholar]
- 85.Ahmad IU, Forman JD, Sarkar FH, Hillman GG, Heath E, Vaishampayan U, et al. Soy isoflavones in conjunction with radiation therapy in patients with prostate cancer. Nutr Cancer. 2010;62(7):996–1000. doi: 10.1080/01635581.2010.509839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Molinie B, Georgel P. Genetic and epigenetic regulations of prostate cancer by genistein. Drug News Perspect. 2009 Jun;22(5):247–54. [DOI] [PubMed]
- 87.Fang MZ, Chen D, Sun Y, Jin Z, Christman JK, Yang CS. Reversal of hypermethylation and reactivation of p16INK4a, RARbeta, and MGMT genes by genistein and other isoflavones from soy. Clin Cancer Res. 2005 Oct 1;11(19 Pt 1):7033–41. [DOI] [PubMed]
- 88.Kikuno N, Shiina H, Urakami S, Kawamoto K, Hirata H, Tanaka Y, et al. Genistein mediated histone acetylation and demethylation activates tumor suppressor genes in prostate cancer cells. Int J Cancer. 2008 Aug 1;123(3):552–60. [DOI] [PubMed]
- 89.Phillip CJ, Giardina CK, Bilir B, Cutler DJ, Lai YH, Kucuk O, et al. Genistein cooperates with the histone deacetylase inhibitor vorinostat to induce cell death in prostate cancer cells. BMC Cancer. 2012;12:145. doi: 10.1186/1471-2407-12-145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Basak S, Pookot D, Noonan EJ, Dahiya R. Genistein down-regulates androgen receptor by modulating HDAC6-Hsp90 chaperone function. Mol Cancer Ther. 2008;7(10):3195–3202. doi: 10.1158/1535-7163.MCT-08-0617. [DOI] [PubMed] [Google Scholar]
- 91.Majid S, Dar AA, Shahryari V, Hirata H, Ahmad A, Saini S, et al. Genistein reverses hypermethylation and induces active histone modifications in tumor suppressor gene B-cell translocation gene 3 in prostate cancer. Cancer. 2010 Jan 1;116(1):66–76. [DOI] [PMC free article] [PubMed]
- 92.Vardi A, Bosviel R, Rabiau N, Adjakly M, Satih S, Dechelotte P, et al. Soy phytoestrogens modify DNA methylation of GSTP1, RASSF1A, EPH2 and BRCA1 promoter in prostate cancer cells. In Vivo. 2010 Jul;24(4):393–400. [PubMed]
- 93.Adjakly M, Bosviel R, Rabiau N, Boiteux JP, Bignon YJ, Guy L, et al. DNA methylation and soy phytoestrogens: quantitative study in DU-145 and PC-3 human prostate cancer cell lines. Epigenomics. 2011 Dec;3(6):795–803. [DOI] [PubMed]
- 94.Chen Y, Zaman MS, Deng G, Majid S, Saini S, Liu J, et al. MicroRNAs 221/222 and genistein-mediated regulation of ARHI tumor suppressor gene in prostate cancer. Cancer Prev Res (Phila). 2011 Jan;4(1):76–86. [DOI] [PMC free article] [PubMed]
- 95.Li Y, Kong D, Ahmad A, Bao B, Sarkar FH. Targeting bone remodeling by isoflavone and 3,3′-diindolylmethane in the context of prostate cancer bone metastasis. PLoS One. 2012;7(3):e33011. doi: 10.1371/journal.pone.0033011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Chiyomaru T, Yamamura S, Zaman MS, Majid S, Deng G, Shahryari V, et al. Genistein suppresses prostate cancer growth through inhibition of oncogenic microRNA-151. PLoS One. 2012;7(8):e43812. doi: 10.1371/journal.pone.0043812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Rabiau N, Trraf HK, Adjakly M, Bosviel R, Guy L, Fontana L, et al. miRNAs differentially expressed in prostate cancer cell lines after soy treatment. In Vivo. 2011;25(6):917–921. [PubMed] [Google Scholar]
- 98.Li Y, Kong D, Ahmad A, Bao B, Dyson G, Sarkar FH. Epigenetic deregulation of miR-29a and miR-1256 by isoflavone contributes to the inhibition of prostate cancer cell growth and invasion. Epigenetics. 2012 Aug;7(8):940–9. [DOI] [PMC free article] [PubMed]
- 99.Andres S, Abraham K, Appel KE, Lampen A. Risks and benefits of dietary isoflavones for cancer. Crit Rev Toxicol. 2011 Jul;41(6):463–506. [DOI] [PubMed]
- 100.Sarkar FH, Adsule S, Padhye S, Kulkarni S, Li Y. The role of genistein and synthetic derivatives of isoflavone in cancer prevention and therapy. Mini Rev Med Chem. 2006 Apr;6(4):401–7. [DOI] [PubMed]


