Abstract
Introduction
Patellofemoral pain (PFP) can cause significant pain leading to limitations in societal participation and physical activity. An international expert group has highlighted the need for a classification system to allow targeted intervention for patients with PFP; we have developed a work programme systematically investigating this. We have proposed six potential subgroups: hip abductor weakness, quadriceps weakness, patellar hypermobility, patellar hypomobility, pronated foot posture and lower limb biarticular muscle tightness. We could not uncover any evidence of the relative frequency with which patients with PFP fell into these subgroups or whether these subgroups were mutually exclusive. The aim of this study is to provide information on the clinical utility of our classification system.
Methods and analysis
150 participants will be recruited over 18 months in four National Health Services (NHS) physiotherapy departments in England. Inclusion criteria: adults 18–40 years with PFP for longer than 3 months, PFP in at least two predesignated functional activities and PFP elicited by clinical examination. Exclusion criteria: prior or forthcoming lower limb surgery; comorbid illness or health condition; and lower limb training or pregnancy. We will record medical history, demographic details, pain, quality of life, psychomotor movement awareness and knee temperature. We will assess hip abductor and quadriceps weakness, patellar hypermobility and hypomobility, foot posture and lower limb biarticular muscle tightness.
The primary analytic approach will be descriptive. We shall present numbers and percentages of participants who meet the criteria for membership of (1) each of the subgroups, (2) none of the subgroups and (3) multiple subgroups. Exact (binomial) 95% CIs for these percentages will also be presented.
Ethics and dissemination
This study has been approved by National Research Ethics Service (NRES) Committee North West—Greater Manchester North (11/NW/0814) and University of Central Lancashire (UCLan) Built, Sport, Health (BuSH) Ethics Committee (BuSH 025). An abstract has been accepted for the third International Patellofemoral Pain Research Retreat, Vancouver, September 2013.
Keywords: Rehabilitation Medicine
Article summary.
Strengths and limitations of this study
Currently the largest randomised controlled trial sample size is 176 patients. Our target sample size of 150 patients for this feasibility study indicates the scale and ambition of our programme of work.
We have also included a comprehensive set of psychosocial and physiological measures as these may also help us to understand differences between potential subgroups. Traditionally patellofemoral research has focused on biomechanical and to some extent pain measures and has paid little attention to the wider holistic picture of a patient's discomfort.
We have not included an assessment of cost or resource use in this study. Therefore, any difference in the resource use of different subgroups will remain unknown.
Qualitative methods would enhance the investigation of psychosocial aspects.
The study is not longitudinal, but importantly will provide key data to inform such studies.
Background
Patellofemoral pain (PFP) can cause significant pain and dysfunction leading to limitations in societal participation and physical activity. Higher body mass indices and higher than expected levels of disability and psychological morbidity have been observed in patients with PFP.1 2 A number of studies provide evidence which challenges the common view that PFP is a relatively trivial and self-limiting condition: 91% of patients had pain and dysfunction at a follow-up of a minimum of 4 years following diagnosis3; 96% reported having problems, a mean of 4 years following diagnosis4; 73% still had pain at an average of 5.7-year follow-up5; and 94% had ongoing problems for on average 16 years following diagnosis.6
It has also been reported that there is a possibility that PFP predisposes people to osteoarthritis in later life; Stathopulu and Baildam3 found that 45% of their patients with PFP, for whom PFP was the first recorded musculoskeletal problem, were later diagnosed with other arthritic conditions. In a study of people with knee pain aged over 50 years, it was found that 507 (64%) had definite radiographic evidence of patellofemoral osteoarthritis, which suggests that there are specific degenerative processes occurring within the patellofemoral joint, which may not be related to the other articular components of the knee. It is unknown how many of these patients had patellofemoral problems when they were younger.7 Utting et al8, reported that 22% of patients (mean age 67) undergoing unicompartmental patellofemoral arthroplasty recalled having PFP as an adolescent. However, a recent systematic review reported that the link between PFP and patellofemoral osteoarthritis should be interpreted with caution due to the paucity of high-quality evidence.9
PFP is a condition commonly referred for physiotherapy10 and PFP recently emerged as the third highest ranked topic out of 185 in the Chartered Society of Physiotherapy Musculoskeletal Research Priority Project.11 In this national survey, there was 94.9% agreement on the importance of PFP with respect to physiotherapy practice, quality of care, cost-effectiveness and public health. The mean number of National Health Services (NHS) physiotherapy treatment sessions for patients referred with PFP is reported as 8 with the maximum number of sessions reported as 17.12 The Cochrane Library lists four current reviews13–16; two withdrawn reviews17 18 and one protocol,19 which are specific to the conservative management of PFP. Collectively these reviews suggest that there is a weak evidence base for conservative management of PFP, including physiotherapy, mainly due to the poor methodological quality of existing studies. In 2012 we found 52 randomised controlled trials (RCTs) recruiting 2667 participants that investigated interventions for PFP, 60% reported results that were not statistically significant. The average sample size was 51 participants and the largest study20 included 176 participants. As reflected in the number of Cochrane reviews conservative care for PFP is diverse and usually consists of a multimodal package of interventions. The current multimodal approach can include a variety of muscle strengthening and stretching techniques, patellar taping or bracing and foot orthotics. More recent high-quality studies21 22 have proposed that a targeted intervention approach for specific subgroups of patients with PFP may produce improved patient outcomes. Crossley et al21 also discuss the need for developing classification systems of patients with PFP so that “more specific treatment can be designed and evaluated.” The idea of clinically subgrouping patients with PFP and then delivering targeted treatment emerged from the First International PFP Research Retreat.23 One of the questions posed, as part of the consensus-building process, was “Where do we need to go?” The response was “Identification of sub-groups of people with PFP is needed. This may be achieved through the use of high quality Randomised Controlled Trials (RCTs), which should only investigate a few potential subgroups for which there is a credible rationale…High quality RCTs for different conservative treatments (eg, hip muscle retraining, gait re-education) are strongly encouraged. However, these treatments should be targeted to those sub-groups of people who are most likely to benefit.”23 The conference proposed three anatomically based subgroups, proximal (hip and pelvis), local (patella and knee factors) and distal (foot and ankle). The same proximal, local and distal subgrouping approach was adopted by the Second International PFP Research Retreat.24 This subgrouping provides a rationale for researchers to develop targeted treatment interventions. However, until today there have been no studies which have further investigated this premise. Interestingly a separate process of international consensus building about the future direction of research in the field of primary care musculoskeletal studies has been conducted.25 This group has also highlighted the need for future studies to adopt a subgrouping targeted approach in order to improve our understanding of the mechanisms underlying musculoskeletal problems to optimise patient management. They highlight that in previous studies the heterogeneity of patient samples produces a small treatment effect, which masks a wide range of individual responses leading to the conclusion that non-pharmacological interventions in musculoskeletal conditions lead to little patient benefit.
Work plan
We have developed a work programme consisting of a number of phases to investigate subgrouping and the targeted intervention approach in PFP. Phase 1: was the theoretical classification of patients with PFP into distinct clinical groups based on clinical assessment tests, which could be used to target intervention in clinical practice, through the development of a clinical practice framework. Phase 2 (the current phase): is developing and testing the feasibility of using a clinical practice framework to assign patients with PFP into subgroups. Phase 3: RCT evaluating the cost-effectiveness of using the clinical practice framework compared to usual care to improve quality of life of patients with PFP. This will incorporate an internal pilot study, to check assumptions about outcome variability which will inform sample size estimates.
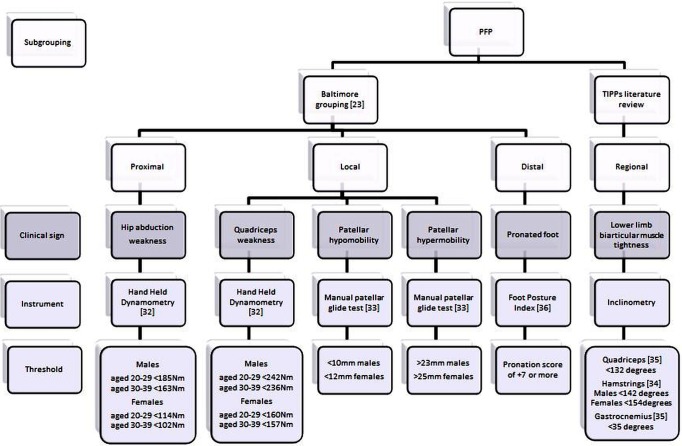
Results of phase 1: identification and development of clinical assessment tests
We have completed phase 1 of this work. This was a literature review, evidence synthesis and clinical mapping undertaken by the targeted interventions for PFP research team to establish supporting evidence for the existence of subgroups. Subgroups were derived from the literature which conformed to the following criteria: (1) they could potentially be identified by simple evidence-based clinical assessment tests; (2) the tests could be used routinely by physiotherapists in a variety of clinical practice settings ranging from primary care facilities to tertiary teaching hospitals; (3) minimal expertise and training was required for competent performance of the tests; (4) any equipment required for the tests needed to be low cost; (5) published thresholds for potentially assigning patients to subgroups had to be available; and (6) any potential subgroup then had to be matched to a specific and credible treatment intervention. Using the First International PFP Research Retreat subgroups as a starting point, we found that there was often more than one clinical problem at the proximal, local and distal sites, and that there were also multiple and sometimes complex clinical assessment tests and multiple interventions. For example, a number of different strength factors have been proposed proximally at the hip.26 27 Patients with proprioceptive deficits have been identified locally at the patella and knee;28 29 however, the problem with this subgroup is that as yet there are no simple and cheap methods to accurately identify proprioceptive deficit in clinical centres that do not have access to dynamometry. Two clinical prediction rules for the likely success of orthotic intervention have been proposed distally at the foot and ankle; however, there is no agreement between the two studies as to the individual clinical items. The first30 lists three items: forefoot valgus alignment; great toe extension; navicular drop test and the second31 lists four different items: age, height, worst pain measured using a visual analogue scale; midfoot width difference from weight bearing to non-weight bearing. Therefore, at the end of this work we have proposed six rather than three subgroups each of which has a specific clinical test which yields a score from which a threshold has previously been published. The threshold scores will be used to assign patients to subgroup membership (figure 1). However, the literature was unable to provide any evidence of the relative frequency with which patients with PFP fell into each of these subgroups and whether these subgroups were mutually exclusive. Therefore, the next stage of our developmental work is an investigation of the distribution of patients into the subgroups when the clinical assessment tests and subsequent threshold scores are applied in routine physiotherapy practice (phase 2). This is the feasibility study which forms the basis of this paper. The main aims of this feasibility study are to assess the relative frequency with which patients fall into each of the subgroups and whether or not the subgroups are mutually exclusive. By the end of this study we would expect to have greater clarity as to whether all, some or none of our proposed subgroups could potentially be useful in clinical practice to form the basis of targeted treatment.
Figure 1.
Targeted interventions for patellofemoral pain groups.
Phase 2: methods
Research question
Do clinically important subgroups of patients with PFP exist?
Aim of study
To provide information on the clinical utility of subgrouping patients with PFP.
Study objectives
This study is designed to provide clinical evidence for theoretically derived subgroups of patients with PFP, which may be appropriate for targeted treatment. In this study we will apply evidence-based routine clinical assessment tests to a representative sample of patients with PFP referred for physiotherapy in order to examine: (1) the relative frequency with which they fall into each of the subgroups; (2) whether the subgroups are mutually exclusive or whether, and how frequently, patients fall into two or more subgroups; (3) whether there are any subgroups which may not be clinically important in the context of targeted treatment because insufficient patients fall into these subgroups; (4) whether patient and clinical characteristics vary between the subgroups. The collection of study data will also allow us to explore the potential for better methods of classifying subgroups by including patient and/or clinical characteristics or by the use of different test thresholds.
Study design
Observational study, at one time point (start of physiotherapy), of adults age 18–40 years with a clinical diagnosis of unilateral or bilateral PFP present for longer than 3 months (for full eligibility criteria see box 1).
Box 1. Eligibility criteria22–37.
Inclusion criteria
Men and women aged 18–40 years able to give informed written consent
Clinical diagnosis of unilateral or bilateral patellofemoral pain longer than 3 months
Anterior or retropatellar pain reported on at least two of the following activities: prolonged sitting, ascending or descending stairs, squatting, running, kneeling and hopping/jumping
- In addition to the above, at least two of the three following clinical examination findings:
- pain during resisted isometric quadriceps contraction
- pain with palpation of the posterior borders of the patella
- pain during squatting
Exclusion criteria
Previous knee surgery and participants awaiting surgery for another lower limb joint problem(s)
Ligamentous instability and/or internal derangement
History of patella subluxation or dislocation
Joint effusion when the midpatellar girth is 5% or more than the non-involved knee
True knee joint locking and/or giving way
Coexistent acute illness or chronic disease
Bursitis, patella or iliotibial tract tendinopathy, Osgood-Schlatter's disease, Sinding-Larsen-Johansson Syndrome, muscle tears or symptomatic knee plicae
Participants already involved in active lower limb training programmes
Pregnancy or breast feeding
Setting
Four NHS physiotherapy departments in England: Central Manchester University Hospitals NHS Foundation Trust; Harrogate and District NHS Foundation Trust; Lancashire Care NHS Foundation Trust; NHS Solent.
Patient recruitment
One hundred and fifty potential participants in total will be recruited over an 18-month period across the four collaborating centres. A research physiotherapist based within each of the four physiotherapy departments will check eligibility and obtain informed consent. Each patient that agrees to take part will be assessed once only by a research physiotherapist (one at each participating centre). The research assessment for this feasibility study will consist of two parts. Part 1: assessment of demographic, clinical and psychosocial patient characteristics which will take approximately 20 min to complete (table 1). Data will be collected on characteristics known to have an impact on outcome. These data may help us to further understand differences between potential subgroups or suggest new subgroups. Previous studies have used some of these tools, however no other study has attempted to systematically investigate psychosocial issues in patients with PFP in the comprehensive manner proposed here. Part 2: clinical assessment tests which take approximately 25 min to complete (table 2). Thresholds, for assigning participants to subgroups, for each test are based on normative data from healthy populations ±1 SD (figure 1).
Table 1.
Patient characteristics assessment
| Domain | Questionnaire/items |
|---|---|
| Clinical characteristics | Time since onset Previous treatment History of trauma Physical activity (International Physical Activity Questionnaire IPAQ)38 Physical functioning (Modified Functional Index Questionnaire (MFIQ)39 |
| Sociodemographic characteristics | Age Gender |
| Anthropometry |
Height Weight Body mass Leg length Skin fold over the patellae |
| Psychosocial | |
| Pain measures | Nociceptive pain Short Form McGill Pain Questionnaire (SF-MPQ-2)40 Numeric Pain Rating Scale (NPRS) for average pain during the past week Neuropathic pain Leeds Assessment of Neuropathic Symptoms and Signs (S-LANSS) Questionnaire41 |
| Quality of life | WHO Disability Assessment Scale 2 (WHODAS 2.0)42 EQ-5D-5 L43 Hopkins Symptom Checklist 25 (HSCL-25)44 |
| Psychomotor movement awareness | Movement Specific Reinvestment Questionnaire45 |
| Physiological parameters | Self-reported indicators of cold knees46 skin temperature measurement (over centre of patella and muscle belly of tibialis anterior) |
Table 2.
Clinical assessment tests
| Proposed clinical groups | Tests |
|---|---|
| Hip abductor weakness | Hand-Held Dynamometry32 |
| Quadriceps weakness | Hand-Held Dynamometry32 |
| Patellar hypomobility | Patellar Glide Test33 |
| Patellar hypermobility | Patellar Glide Test33 |
| Pronated foot posture | Foot Posture Index35 |
| Lower limb biarticular muscle tightness | Rectus femoris length test33 Hamstrings length test34 Gastrocnemius length test33 |
Clinical assessment tests
Dynamometer measurement of quadriceps muscle strength using a Lafayette Manual Muscle Test System (range 0–136 kg): The participant will be in a seated position and the hips and knees flexed to 90°. Muscle strength of the knee extensors will be assessed with a portable dynamometer mounted against a stabilisation strap positioned perpendicular to the tibia just above the malleoli. The force exerted against the dynamometer in this position will be recorded and the moment arm of this force around the extension/flexion axis of the knee joint will be measured using a tape measure as the distance from the level of the dynamometer on the tibia to the centre of the knee joint (assumed to coincide with the most prominent point on the femoral epicondyle identified through palpation). These two measurements will be used to calculate the maximum knee extensor moment (Nm) during an isometric maximal voluntary contraction (MVC) test as the product of the force in Newtons (N) and moment arm in metres (m).32
Dynamometer measurement of hip abductors muscle strength: The participant will be in side lying with the tested leg uppermost in the neutral anatomical position. The participant will be asked to abduct their leg sideways (ie, towards the ceiling) from this position; the portable dynamometer mounted against a stabilisation strap will be held perpendicular to the side of the leg at a level just above the knee joint. To ensure that abductor muscle strength is tested and that the lower limb does not rotate externally, the participants will be instructed to ensure their toes are pointed horizontally during the contraction. The force exerted against the dynamometer in this position will be recorded and the moment arm of this force around the adduction/abduction axis of the hip joint will be measured using a tape measure as the distance from the level of the dynamometer on the thigh to the centre of the hip joint. These two measurements will be used to calculate the maximum hip abductor moment (Nm) during an MVC test as the product of the force (N) and moment arm (m).32 Strength testing will be performed to assess functional capacity, in particular we are interested in the relative balance between the quadriceps and hip abductors. This simple clinical test procedure will not enable the peripheral and central components of muscle dysfunction to be identified but will provide a useful indication of contractile performance.
Patellar glide: With the participants in supine, the quadriceps muscles relaxed and the knees in extension, the clinician will apply a medially and then a laterally directed force to the patella. The total displacement of the pole of the patella will be recorded in millimetres in the coronal plane.33
Passive knee extension (Hamstrings length): The participant will be positioned supine on a plinth. The lower limb not being tested will be positioned in hip and knee extension. The research physiotherapist will position the hip and knee of the tested side in 90° of flexion, thus marking the starting position for the test. With one hand supporting the participant's distal thigh and the other hand cupping the heel, the research physiotherapist will passively extend the knee until firm resistance is elicited. At this point the angle of the tibia is recorded with a digital inclinometer.34
Passive prone knee bend (quadriceps length): The participant will be positioned in prone lying on the edge of a plinth so that the foot on the non-involved side will be placed on the floor at 90° hip flexion. The knee of the tested leg will be passively maximally flexed until resistance or discomfort is elicited. In this position the angle of the tibia will be recorded with a digital inclinometer.33
Standing method for assessing calf flexibility: The length of the gastrocnemius muscle will be obtained by having the participant lean on a solid support 0.6 m away with the tested leg behind the contralateral leg and keeping the knee of the tested leg extended. The participants will be instructed to maximally flex their tested ankle while keeping their heel on the floor. The angle of the tibia is recorded relative to vertical with a digital inclinometer.33
Foot posture index: There are six component assessments (1) talar head position, (2) supralateral and infralateral malleolar curvature, (3) calcaneal frontal plane position, (4) prominence in the region of the talonavicular joint, (5) congruence of the medial longitudinal arch, (6) abduction/adduction of the forefoot on the rearfoot. Each of the component assessments or observations are graded 0 for neutral, with scores of −2 for clear signs of supination and +2 for clear signs of pronation. Unless the criteria outlined for each of the features are clearly met then the more conservative score will be awarded. When the scores are combined, the aggregate value gives an estimate of the overall foot posture. Large positive aggregate values indicate a pronated posture.35
Training of research therapists
All research physiotherapists will undertake a full day training session during the first month of the study, when they will be provided with training on the research processes and on how to undertake the standardised clinical assessment tests. During the training sessions, all the therapists will be observed by the principal investigator and MC performing each of the clinical test procedures and provided with peer feedback. Intertherapist variability will be examined during these sessions and although it will not be possible to conduct a formal inter-rater reliability assessment during the training it will provide an opportunity to observe any variability in performance and address it. All the physiotherapists will be provided with a comprehensive manual including the standard operating procedures, along with a data recording proforma.
Sample size
Given the nature of the study, power calculations are not applicable. One hundred and fifty participants will enable us to estimate, with 95% CI, the numbers and percentages of participants who meet the criteria for membership of (1) each of the six subgroups individually; (2) none of the subgroups; (3) multiple subgroups (for each represented subgroup combination) to within ±7.5% for well-represented (30% prevalence) subgroups and to within ±3.5% for sparse (5% prevalence) subgroups (or multiple subgroups).
Analysis plan
As the main purpose of the study is to describe the distribution of patients with PFP into the different subgroups following application of the clinical assessment test criteria, including whether patients meet the criteria for multiple subgroups or fail to meet the criteria for any of the subgroups, the primary analytical approach will be descriptive.
We shall present numbers and percentages of participants who meet the criteria for membership of
Each of the six subgroups individually;
None of the subgroups;
Multiple subgroups (for each represented subgroup combination).
Exact (binomial) 95% CIs for these percentages will also be presented. We shall also present descriptive statistics (mean (SD), median (IQR), count (%), as appropriate) of the patient characteristics for each subgroup (including the no clinical subgroup) to indicate how these characteristics vary across subgroups. The data will also enable some further exploratory analyses to be performed. The nature of these analyses will depend on the patterns of the distribution of participants into subgroups. However, we expect that they will include an exploration of the sensitivity of the distribution of subgroup membership to the choices of thresholds, particularly if substantial numbers of patients fall into either multiple subgroups or no subgroup; they are also likely to include explorations of the joint effects of patient characteristics on the distribution of patients into subgroups, using techniques including multiple logistic regression. Demographic, clinical and psychosocial characteristics as previously described may also be included as covariates in later exploratory model-based analyses.
Discussion
Recent literature has strongly promoted the idea of subgrouping patients with PFP and delivering targeted treatment, as it is believed that this may be more beneficial than the current multimodal therapeutic approaches.20–22 Despite these recommendations, this premise has not yet been investigated. The main aims of this feasibility study are therefore to assess the relative frequency with which patients fall into each of the subgroup and whether or not the subgroups are mutually exclusive.
As outlined above, the study has a number of strengths and addresses key gaps in current knowledge. It is ambitious in terms of scale and scope. There is often controversy and lack of consensus within the field of patellofemoral research, due to two related factors associated with the nature of the current evidence base. First, there are a relatively large number of normative data; studies conducted on very small samples of healthy participants that do little to enhance our understanding of this complex chronic condition.36 Second, as already discussed, there is a limited number of high-quality, large scale clinical trials. Set against this context, where currently the largest RCT sample size is 176 patients,20 our target sample size of 150 patients for this feasibility study indicates the scale and ambition of our programme of work. In terms of the scope of this study, we have also included a comprehensive set of psychosocial and physiological measures as these may also help us to understand differences between potential subgroups. Traditionally, patellofemoral research has focused on biomechanical and to some extent pain measures and has paid little attention to the wider holistic picture of a patient's discomfort. One study has indicated that psychological morbidity may be important in PFP.2 The more comprehensive data being obtained in the present study will provide us with a unique insight into the patient's experience of the condition which may also help further our understanding of future treatment options. There are also potential limitations in the scope of this study. We have not included an assessment of cost or resource use in this study. Therefore, any differential in the resource use of different subgroups will remain unknown; we plan to address this in phase 3 of our programme of work. In the current feasibility study, there is however, a health economics component as we are collecting EQ-5D-5L data so we will gain some insight into the potential health consequences of different subgroups. Qualitative methods would enhance the investigation of psychosocial aspects. We envisage using mixed methods, as well as more patient and public involvement in subsequent studies. The study is not longitudinal, but importantly will provide key data to inform such studies. The results of the present study are expected in 2014. They will provide answers to a number of questions about the validity and relevance of subgrouping in PFP in clinical practice and will inform future trials.
Status
The study has currently recruited 101/150 patients and is scheduled to be completed by 29 November 2013.
Supplementary Material
Acknowledgments
The authors would like to thank the following physiotherapists for performing the research assessments Steve Hill, Stephen Kirk, Gary McCall, Christine Dewsbury and Sophie Chatwin. They would also like to thank the following service managers for their support Keith Mills, Elaine Nicholls, Barbara Sharp, Chantel Ostler and Kim Patterson. The full targeted interventions for patellofemoral pain syndrome (TIPPS) Research team are JS, Jim Richards, Paola Dey, CS, JJ, Russell Hogarth (all UCLan), MC (Manchester University), EW (Ghent University and Aspetar, Qatar), JD and DM (Teesside University), MS (University of Southampton), Nigel Arden (University of Oxford), ER (Harrogate and District National Health Services (NHS) Foundation Trust), Bill Baltzopoulos (Brunel University), DT (University of East Anglia), Rich Masters (Hong Kong University), Remco Polman (Victoria University, Melbourne, Australia).
Footnotes
Contributors: JS, JR, EW, MC and ER contributed to study conception, design and attained project funding. MPD, CS, JD, DM, MS and DT contributed to study design and attained project funding. JJ contributed to project management and study design. All authors contributed to manuscript preparation and have read and approved the final version of the manuscript.
Funding: This work was supported by Arthritis Research UK (grant number 19950) and involves collaboration with the Arthritis Research UK Centre for Sport, Exercise and Osteoarthritis. Arthritis Research UK Musculoskeletal Pain clinical studies group (CSG) also funded a Think Tank meeting where the research group consisting of academics with expertise in patellofemoral pain, biomechanists, psychosocial aspects related to injury rehabilitation adherence, experts in neuromuscular function, patient representative and practicing physiotherapists started to review the literature to identify clinical groups.
Competing interests: None.
Ethics approval: This study has been approved by National Resarch Ethics Service (NRES) Committee North West—Greater Manchester North, REC reference: 11/NW/0814 and University of Central Lancashire (UCLan) Built, Sport, Health (BuSH) Ethics Committee Reference Number: BuSH 025. All relevant Research and Governance approvals have been secured at the 4 NHS Trusts where data collection is taking place and all licenses obtained for the questionnaire instruments were required.
Provenance and peer review: Not commissioned; internally peer reviewed.
References
- 1.Clark DI, Downing N, Mitchell J, et al. Physiotherapy for anterior knee pain: a randomised controlled trial. Ann Rheum Dis 2000;59:700–4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jensen R, Hystad T, Baerheim A. Knee function and pain related to psychological variables in patients with long-term patellofemoral pain syndrome. J Orthop Sports Phys Ther 2005;35:594–600 [DOI] [PubMed] [Google Scholar]
- 3.Stathopulu E, Baildam E. Anterior knee pain: a long-term follow-up. Rheumatology 2003;42:380–2 [DOI] [PubMed] [Google Scholar]
- 4.Price AJ, Jones J, Allum R. Chronic traumatic anterior knee pain injury. Injury 2000;31:373–8 [DOI] [PubMed] [Google Scholar]
- 5.Blond L, Hansen L. Patellofemoral pain syndrome in athletes: a 5.7 year retrospective follow-up study of 250 athletes. Acta Orthop Belg 1998;64:393–400 [PubMed] [Google Scholar]
- 6.Sandow MJ, Goodfellow JW. The natural history of anterior knee pain in adolescents. J Bone Joint Surg Br 1985;67:36–8 [DOI] [PubMed] [Google Scholar]
- 7.Peat G, Thomas E, Handy J, et al. The Knee Clinical Assessment Study—CAS(K). A prospective study of knee pain and knee osteoarthritis in the general population: baseline recruitment and retention at 18 months. BMC Musculoskelet Disord 2006;7:30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Utting MR, Davies GJ, Newman JH. Is anterior knee pain a predisposing factor to patellofemoral osteoarthritis? Knee 2005;12:362–5 [DOI] [PubMed] [Google Scholar]
- 9.Thomas M, Wood L, Selfe J, et al. Anterior knee pain in younger adults as a precursor to subsequent patellofemoral osteoarthritis: a systematic review. BMC Musculoskelet Disord 2010;11:201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Callaghan MJ, Selfe J. Has the prevalence of patellofemoral pain in the general population in the United Kingdom been properly evaluated? Phys Ther Sport 2007;8:37–43 [Google Scholar]
- 11.CSP Physiotherapy research priority project: musculoskeletal topics. London: Chartered Society of Physiotherapy, 2010 [Google Scholar]
- 12.Brown J. Physiotherapists knowledge of patellofemoral pain syndrome. Br J Ther Rehabil 2000;7:346–53 [Google Scholar]
- 13.Hossain M, Alexander P, Burls A, et al. Foot orthoses for patellofemoral pain in adults. Cochrane Database Syst Rev 2011;1:CD008402. [DOI] [PubMed] [Google Scholar]
- 14.Callaghan MJ, Selfe J. Patellar taping for patellofemoral pain syndrome in adults. Cochrane Database Syst Rev 2012;4:CD006717. [DOI] [PubMed] [Google Scholar]
- 15.Heintjes EM, Berger M, Bierma-Zeinstra SMA, et al. Pharmacotherapy for patellofemoral pain syndrome. Cochrane Database Syst Rev 2004;3:CD003470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Heintjes EM, Berger M, Bierma-Zeinstra SMA, et al. Exercise therapy for patellofemoral pain syndrome. Cochrane Database Syst Rev 2003;4:CD003472. [DOI] [PubMed] [Google Scholar]
- 17.Brosseau L, Casimiro L, Welch V, et al. Therapeutic ultrasound for treating patellofemoral pain syndrome. Cochrane Database Syst Rev 2001;2:CD003375. [DOI] [PubMed] [Google Scholar]
- 18.D'hondt NE, Aufdemkampe G, Kerkhoffs G, et al. Orthotic devices for treating patellofemoral pain syndrome. Cochrane Database Syst Rev 2009;1:CD002267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.van der Heijden RA, Lankhorst N, Van Linschoten R, et al. Exercise for treating patellofemoral pain syndrome. Cochrane Database Syst Rev 2013;2:CD010387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Collins N, Crossley K, Darnell R, et al. Foot orthoses and physiotherapy in the treatment of patellofemoral pain syndrome: randomised clinical trial. BMJ 2008;337:a1735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Crossley K, Bennel K, Green S, et al. Physical therapy for patellofemoral pain. A randomized double blinded placebo controlled trial. Am J Sports Med 2002;30:857–65 [DOI] [PubMed] [Google Scholar]
- 22.Syme G, Rowe P, Martin D, et al. Disability in patients with chronic patellofemoral pain syndrome: a randomised controlled trial of VMO selective training versus general quadriceps training. Manual Ther 2009;14:252–63 [DOI] [PubMed] [Google Scholar]
- 23.Davis I, Powers C. Patellofemoral pain syndrome: proximal, distal, and local factors. An International Retreat. J Orthop Sports Phys Ther 2010;40:A1–48 [DOI] [PubMed] [Google Scholar]
- 24.Powers C, Bolgla LA, Callaghan MJ, et al. Patellofemoral pain: proximal, distal, and local factors, 2nd International Research Retreat. J Orthop Sports Phys Ther 2012;42:A1–54 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Foster NE, Dziedzic KS, Van der Windt DAWM, et al. Research priorities for non-pharmacological therapies for common musculoskeletal problems: nationally and internationally agreed recommendations. BMC Musculoskelet Disord 2009;10:3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ireland ML, Willson JD, Ballantyne BT, et al. Hip strength in females with and without patellofemoral pain. J Orthop Sports Phys Ther 2003;33:671–6 [DOI] [PubMed] [Google Scholar]
- 27.Bolgla L, Malone T, Umberger B, et al. Hip strength and knee kinematics during stair descent in females with and without patellofemoral pain syndrome. J Orthop Sports Phys Ther 2008;38:12–18 [DOI] [PubMed] [Google Scholar]
- 28.Baker V, Bennell K, Stillman B, et al. Abnormal knee joint position sense in individuals with patellofemoral pain syndrome. J Orthop Res 2002;20:208–14 [DOI] [PubMed] [Google Scholar]
- 29.Callaghan M, Selfe J, McHenry A, et al. Effects of patellar taping on knee joint proprioception in patients with patellofemoral pain syndrome. Man Ther 2008;13:192–9 [DOI] [PubMed] [Google Scholar]
- 30.Sutlive T, Mitchell S, Maxfield S, et al. Identification of individuals with patellofemoral pain whose symptoms improved after a combined programme of foot orthosis use and modified activity: a preliminary investigation. Phys Ther 2004;84:49–61 [PubMed] [Google Scholar]
- 31.Vincenzino B, Collins N, Cleland J, et al. A clinical prediction rule for identifying patients with patellofemoral pain who are likely to benefit from foot orthoses: a preliminary determination. Br J Sports Med 2010;44:862–6 [DOI] [PubMed] [Google Scholar]
- 32.Maffiuletti NA. Assessment of hip and knee muscle function in orthopaedic practice and research. J Bone Joint Surg Am 2010;92:220–9 [DOI] [PubMed] [Google Scholar]
- 33.Witvrouw E, Lysens R, Bellemans J, et al. Intrinsic risk factors for the development of anterior knee pain in an athletic population: a two year prospective study. Am J Sports Med 2000;28:480–9 [DOI] [PubMed] [Google Scholar]
- 34.Youdas JW, Krause DA, Hollman JH, et al. The influence of gender and age on hamstring muscle length in healthy adults. J Orthop Sports Phys Ther 2005;35:246–52 [DOI] [PubMed] [Google Scholar]
- 35.Redmond AC, Crane YZ, Menz HB. Normative values for the foot posture index. J Foot Ankle Res 2008;1:1–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Herrington L, Malloy S, Richards J. The effect of patella taping on vastus medialis oblique and vastus laterialis EMG activity and knee kinematic variables during stair descent. J Electromyogr Kinesiol 2005;15:604–7 [DOI] [PubMed] [Google Scholar]
- 37.Cook C, Hegedus E, Hawkins R, et al. Diagnostic accuracy and association to disability of clinical test findings associated with patellofemoral pain syndrome. Physiother Can 2010;62:17–24 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Short last 7 days self-administered version of the IPAQ. https://sites.google.com/site/theipaq/questionnaire_links (accessed 12 Aug 2013).
- 39.Selfe J, Harper L, Pedersen I, et al. Four outcome measures for patellofemoral joint problems: part 1 development and validity. Physiotherapy 2001;87:507–15 [Google Scholar]
- 40.Melzack R. SF-MPQ-2©: the Initiative on Methods, Measurement, and Pain Assessment in Clinical Trials (IMMPACT). http://www.immpact.org (accessed 12 Aug 2013).
- 41.Bennett MI, Smith BH, Torrance N, et al. The S-LANSS Score for identifying pain of predominantly neuropathic origin: validation for use in clinical and postal research. J Pain 2005;6:149–58 [DOI] [PubMed] [Google Scholar]
- 42.WHO Disability Assessment Schedule 2.0 http://www.who.int/classifications/icf/whodasii/en/index.html (accessed 12 Aug 2013).
- 43.EQ-5D. http://www.euroqol.org/home.html (accessed 12 Aug 2013).
- 44.Derogatis LR, Lipman R, Rickels K, et al. The Hopkins Symptom Checklist (HSCL): a self-report symptom inventory. Behav Sci 1974;19:1–15 [DOI] [PubMed] [Google Scholar]
- 45.Masters RSW, Eves FF, Maxwell J. Development of a movement specific reinvestment scale. In: Morris T, Terry P, Gordon S, Hanrahan S, Levleva L, Kolt G, Tremayne P. eds Proceedings of the ISSP 11th World Congress of Sport Psychology; 14–19 August 2005, Sydney, 2005 [Google Scholar]
- 46.Selfe J, Sutton C, Hardaker N, et al. Anterior knee pain and cold knees: a possible association in women. Knee 2010;17:319–23 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.