Abstract
Objectives
Allergic disease may be increased by climate change. Recent reports have shown that typhoon and heavy rain increase allergic disease locally by concentration of airborne allergens of pollen, ozone, and fungus, which are causes of allergic disease. The objective of this study was to determine whether typhoon and heavy rain increase allergic disease in Korea.
Methods
This study included allergic disease patients of the area declared as a special disaster zone due to storms and heavy rains from 2003 to 2009. The study used information from the Korea Meteorological Administration, and from the National Health Insurance Service for allergic diseases (asthma, allergic rhinitis, and atopic dermatitis).
Results
During a storm period, the numbers of allergy rhinitis and atopic dermatitis outpatients increased [rate ratio (RR) = 1.191; range, 1.150–1.232] on the sixth lag day. However, the number of asthma outpatients decreased (RR = 0.900; range, 0.862–0.937) on the sixth lag day after a disaster period. During a storm period, the numbers of allergic rhinitis outpatients (RR = 1.075; range, 1.018–1.132) and atopy outpatients increased (RR = 1.134; range, 1.113–1.155) on the seventh lag day. However, the number of asthma outpatients decreased to RR value of 0.968 (range, 0.902–1.035) on the fifth lag day.
Conclusion
This study suggests that typhoon and heavy rain increase allergic disease apart from asthma. More study is needed to explain the decrease in asthma.
Keywords: allergy, climate change, heavy rain, typhoon
1. Introduction
1.1. Global warming and extreme weather phenomena
Global warming is one of the most important issues in the environmental sector. International cooperation is needed to address global warming; the Intergovernmental Panel on Climate Change was established by the World Meteorological Organization (WMO) [1]. The fourth report issued by the panel forecasted that greenhouse gases (such as carbon dioxide, methane, and nitrogen dioxide) will increase global temperature by 1.1–6.4°C, and the frequency of extreme weather phenomena (such as a rise in sea level, storms, and heavy rains) will be expected to increase [1]. Korea's average temperature has been increasing, in line with the world trend and, as of 2000, compared to 1970, rose by 0.2°C in summer and 1.3°C in winter. Furthermore, precipitation from 1996 to 2005, compared to the past, increased by 10% to 1485.7 mm, but the number of precipitation days has been decreasing with the strength of heavy rain (heavy rain days) on the rise (Table 1) [2].
Table 1.
The change in temperature, humidity, and precipitation of Korea
| Category | 1970s(1973−1980; a) | 2000s(2001−2008; b) | (b)–(a) |
|---|---|---|---|
| Average temperature in summer (°C) | 23.4 | 23.6 | 0.2 |
| Average temperature in winter (°C) | −0.1 | 1.1 | 1.2 |
| Annual relative humidity (%) | 72.3 | 67.0 | −5.3 |
| Annual precipitation (mm) | 1255.0 | 1414.1 | 159.1 |
Note: From Korea Climate Change Valuation Report 2011 by S.J. Lee, 2010, Seoul: Ministry of Environment, p. 33.
1.2. Extreme weather and allergic disease
Allergic disease is the human body's immune response to allergens, showing symptoms in the respiratory organs and skin, and includes asthma, allergic rhinitis, and atopic dermatitis [3]. These allergic diseases are on the rise in industrialized countries and accompanying burdens have been increasing [4]. Prevalence rates of these allergic diseases are closely related to exposure to allergens. In particular, the increase in concentration of aeroallergen by meteorological phenomenon significantly affects the increase in prevalence rate of allergic diseases [5].
In some studies, the concentration of aeroallergen (such as pollen, ozone, molds, and air pollutant materials) is known to be closely related to meteorological phenomenon (such as storms, hurricanes, and floods), and affects the incidence of allergic diseases in accordance with weather changes [6].
The relationship between typhoons and allergic disease received considerable attention due to Hurricane Katrina, which hit New Orleans in 2005. Houses were flooded causing the growth of mold in more than 50% of houses [7]. Inside houses, concentration of molds in the air was higher than outside of houses and that of other cities [8]. Consequently, prevalence of asthma rose from 14% in 2003 to 18% in 2006 [9]. In the studies of D'Amato et al [10] and Pulimood et al [11], it was reported that thunderstorms increase aeroallergen. Therefore, this study intended to research the change in allergic disease mainly through typhoons and heavy rain.
2. Materials and Methods
2.1. Study population and data collection
The study population was selected in the special disaster zone of 16 cities and provinces from 2003 to 2009.
2.2. Meteorological data
This study used meteorological data compiled at the weather observatory of each city from 2003 to 2009. In these data, precipitation (mm) and wind speed (m/s) were reported. For precipitation, total daily precipitation was calculated. In cases where there were several observatories in a subject area, average daily precipitation recorded by each observatory was calculated, and then used as daily mid-level of each area. For wind speed, daily highest wind speed was calculated. Where there were several observatories in a subject area, an average daily highest wind speed was calculated, and then used as daily mid-level of each area.
A special disaster zone designation system was introduced in accordance with natural disaster law in 2002. The Central Disaster Preparedness Center, in the Ministry of Government Administration and Home Affairs, suggested that the President declare, as Special Disaster Protection Zones, such areas as he deemed necessary and the committee allowed [12].
2.3. National Health Insurance Service data
National Health Insurance Service data are materials for a health insurance claim to be submitted to the National Health Insurance Service by medical institutions after the institutions provide medical service. Data of daily outpatients of medical clinics in 16 cities and provinces were collected on three codes: allergic rhinitis (J30), asthma (J45), and atopic dermatitis (L20). The concept of episode was used in order to research incidence rate through daily outpatients' documents [13]. Each episode was measured for 1 month and outpatients visited within 1 month were considered one episode.
2.4. Statistic analysis method
Rate ratios (RRs) were calculated from the number of outpatients during the period of disaster (a), which was collected from meteorological data, and the number of outpatients in the reference periods (b). Formula used for the RR is “RR = a/b”, and 95% confidence level (CI) was calculated by: “95% CI of ” [14]. Person-time of those two periods was assumed to be the same and would not affect RR because the parent population of the research period would not change [15,16]. Up to 7 days of delay effect were allowed (a delay of 0 means the exact days of a disaster period). Reference periods were selected as being days close to a disaster period [15].
3. Results
Yearly average precipitation and average wind speed of a disaster period were calculated by using average daily precipitation and average daily highest wind speed (Table 2). Average precipitation of a disaster period and average daily highest wind speed were both higher than yearly average precipitation and average highest wind speed. During a period of heavy rain, precipitation increased, but wind speed did not increase significantly. Precipitation was higher in a typhoon period than in a period of heavy rain, with 57.86 mm and 33.10 mm, respectively. The same was true for wind speed, with 7.78 m/s and 4.85 m/s, respectively (Table 2).
Table 2.
Weather characteristics of special disasters in the Korea from 2003 to 2009
| Disaster type (period) | No. of areasa | Duration (d) | Rainfall (mm)b |
Wind speed (m/s)c |
||
|---|---|---|---|---|---|---|
| Yearly average | Disaster period | Yearly average | Disaster period | |||
| Typhoon (12−13 Sep 2003)d | 14 | 2 | 5.27 (12.08) | 56.45 (65.29) | 4.34 (1.12) | 10.67 (3.46) |
| Typhoon and heavy rain (9−29 Jul 2006) | 7 | 21 | 5.57 (11.91) | 28.04 (25.38) | 4.31 (1.19) | 3.96 (1.46) |
| Typhoon and heavy rain (13−16 Sep 2007) | 1 | 4 | 9.04 (20.25) | 89.08 (95.38) | 5.70 (1.67) | 8.73 (5.75) |
| Heavy rain (22−24 Oct 2006) | 1 | 3 | 7.97 (19.10) | 38.93 (47.78) | 4.37 (1.19) | 6.53 (2.99) |
| Heavy rain (4−15 Aug 2007) | 2 | 12 | 5.87 (10.25) | 19.40 (18.83) | 4.28 (1.21) | 4.25 (0.96) |
| Heavy rain (23−26 Jul 2008) | 1 | 4 | 4.92 (10.67) | 27.51 (38.74) | 4.10 (1.18) | 3.07 (0.38) |
| Heavy rain (11−16 Jul 2009) | 13 | 6 | 5.62 (12.08) | 46.55 (25.72) | 4.40 (1.12) | 5.55 (1.72) |
| All typhoons | — | — | 6.62 (14.75) | 57.86 (62.02) | 4.78 (1.33) | 7.78 (3.56) |
| All heavy rain | — | — | 6.09 (13.03) | 33.10 (32.77) | 4.29 (1.18) | 4.85 (1.51) |
Cities defined by the government as disaster area.
Mean (standard deviation) of daily average rainfall.
Mean (standard deviation) of daily maximum wind speed.
Day/month/year.
Table 3 shows RR of allergic diseases in the disaster period and a reference period based on National Health Insurance data. For allergic rhinitis at all ages, RR increased slightly on the seventh lag day to a maximum of 1.075 (range, 1.018–1.132); this was not greatly different at age <15 years, (RR = 1.068; range, 0.971–1.164) on the fifth lag day. For atopic dermatitis at all ages, RR increased to 1.134 (range, 1.113–1.155) on the seventh lag day, and increased for age <15 years to 1.173 (range, 1.147–1.201). RR of asthma was highest on the sixth lag day in the typhoon period, but the number of outpatients decreased, showing overall 0.900 (range, 0.862–0.937), and age <15 years 0.905 (range, 0.842–0.969).
Table 3.
Rate ratios for daily outpatient visits of asthma, allergic rhinitis, and atopic dermatitis during disaster periods and reference periods
| Disaster type (period) | Age (y) | Asthma |
Allergic rhinitis |
Atopic dermatitis |
|||
|---|---|---|---|---|---|---|---|
| Lag d | RR (95% CI) | Lag d | RR (95% CI) | Lag d | RR (95% CI) | ||
| Typhoon (12−13 Sep 2003) | All | 6 | 13.491 (13.212−13.770) | 6 | 9.989 (9.772−10.206) | 6 | 22.367 (22.490−22.244) |
| ≤15 | 6.500 (6.149−6.851) | 8.129 (7.756−8.502) | 21.340 (21.194−21.487) | ||||
| Typhoon and heavy rain (9−29 Jul 2006) | All | 7 | 0.786 (0.767−0.825) | 7 | 1.010 (0.965−1.054) | 5 | 1.104 (1.092−1.117) |
| ≤15 | 0.827 (0.761−0.893) | 1.144 (1.070−1.219) | 1.146 (1.131−1.161) | ||||
| Typhoon and heavy rain (13−16 Sep 2007) | All | 0 | 1.276 (1.021−1.532) | 7 | 1.103 (0.909−1.296) | 7 | 1.488 (1.393−1.583) |
| ≤15 | 1.941 (1.356−2.526) | 1.200 (0.715−1.685) | 1.624 (1.503−1.745) | ||||
| Heavy rain (22−24 Oct 2006) | All | 6 | 1.310 (0.827−1.794) | 7 | 1.381 (1.120−1.643) | 6 | 1.355 (1.173−1.536) |
| ≤15 | 1.500 (0.824−2.176) | 1.300 (0.888−1.712) | 1.638 (1.417−1.859) | ||||
| Heavy rain (4−15 Aug 2007) | All | 1 | 1.274 (1.031−1.516) | 4 | 1.410 (1.128−1.691) | 7 | 1.060 (0.998−1.123) |
| ≤15 | 1.182 (0.718−1.645) | 1.353 (0.910−1.796) | 1.066 (0.989−1.143) | ||||
| Heavy rain (23−26 Jul 2008) | All | 7 | 1.292 (1.015−1.569) | 6 | 1.247 (0.975−1.520) | 6 | 1.085 (1.000−1.169) |
| ≤15 | 1.051 (0.914−1.901) | 1.162 (0.723−1.602) | 1.102 (0.992−1.211) | ||||
| Heavy rain (11−16 Jul 2009) | All | 5 | 0.961 (0.889−1.032) | 7 | 1.050 (0.990−1.110) | 7 | 1.149 (1.126−1.172) |
| ≤15 | 1.071 (0.945−1.197) | 1.005 (0.905−1.106) | 1.191 (1.161−1.221) | ||||
| All typhoons | All | 6 | 0.900 (0.862−0.937) | 6 | 1.191 (1.150−1.232) | 5 | 1.229 (1.217−1.241) |
| ≤15 | 0.905 (0.842−0.969) | 1.278 (1.206−1.348) | 1.267 (1.252−1.281) | ||||
| All heavy rain | All | 5 | 0.968 (0.902−1.035) | 7 | 1.075 (1.018−1.132) | 7 | 1.134 (1.113−1.155) |
| ≤15 | 1.085 (0.968−1.202) | 5 | 1.068 (0.971−1.164) | 1.173 (1.147−1.201) | |||
CI = confidence interval; RR = Rate ratio.
Figure 1 shows delay effects of allergic diseases occurring during a typhoon period and a period of heavy rain. RR for asthma increased to its highest on the sixth day after a typhoon. By contrast, a heavy rain was thought to have almost no delay effect on asthma. RR of a heavy rain on allergic rhinitis increased in accordance with a delay effect, showing the highest RR on the sixth day. Even if a heavy rain tends to increase RR of allergic rhinitis, its delay effect was not as much as that of a typhoon. When a delay effect was given to changes in allergic dermatitis, RR gradually increased to its highest on the fifth day. As for the effect of a heavy rain on allergic dermatitis, RR was highest on the seventh day and showed the tendency to increase.
Figure 1.
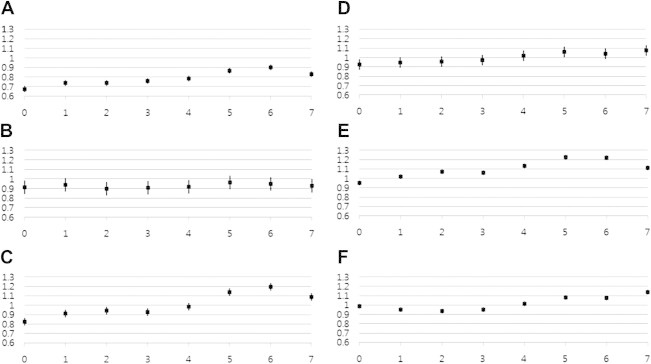
Delayed effect of (A) typhoons, and (B) heavy rain on asthma; (C) typhoons and (D) heavy rain on allergic rhinitis; and (E) typhoons and (F) heavy rain on atopic dermatitis.
4. Discussion
The incidence of asthma by a thunderstorm has been studied frequently. According to Anderson et al [17], during a thunderstorm period, the pollen concentration in the air decreased, but the concentration of mold spores increased, leading to an increase in the incidence of asthma. Langenberg et al [18] showed that as temperature and wind speed increase and humidity decreases, the concentration of mold spores in the air increases. Therefore, it is thought that in the case where an area is declared as a disaster zone only because of heavy rain, and wind speed is similar to the yearly average, precipitation is unlikely to have an affect on allergic diseases. Rao et al [19] showed that -d glucan, bacterial endotoxin, and mold spores inside houses increased after flooding by Hurricane Katrina. Zock et al [20] found that flooded areas showed increased exposure to mold by 3.8-fold 1 year later, compared to unflooded areas. Physical damage such as destruction of houses and injuries, and stress are causes of allergic diseases in addition to molds resulting from floods [21]. Therefore, allergic diseases caused by heavy rain were underestimated and might increase less than those caused by a typhoon because 1 week is a short time for an allergy inductive effect, such as stress and molds of flooded houses, to show up.
Allergic rhinitis and atopic dermatitis increased after a lag time of 5–6 days. Jaakkola et al [22] showed that flooding of a house increased allergic rhinitis by 3.83 times, and when there was a trace observation of mold in a house, the incidence rate of allergic rhinitis was 1.98 times higher. Therefore, this study concluded that allergic rhinitis and atopic dermatitis increased after a typhoon and heavy rain. Established studies have reported that the causes of such induction are the increase in the concentration in the air of mold spores and pollen and the increase in the concentration of molds inside houses caused by flooding. However, further study is needed to discover the cause of allergic diseases occurring after a typhoon and heavy rain because sensitization rates of domestic allergy patients is different from that of other countries.
Unlike other allergic disease, the number of asthma outpatients was lower than in the reference period. Asthma, allergic rhinitis, and atopic dermatitis are acute inflammation response shown when exposed after sensitization to allergen, and thus share physiological fundamentals [23]. Therefore, it may be presumed that when other diseases increase because of a specific allergen, asthma will also increase. Many other studies have shown that asthma and allergic diseases increase after thunderstorms and typhoons [10,11,24], but in this study, asthma decreased and the causes for such decrease should be investigated. There are several reasons. First, there is the possibility of underestimation of patients because of missing hospital records or documents for emergency room visits. Asthma patients are advised to go to the emergency room when an asthma attack occurs while controlling it as a chronic disease. Therefore, without documents on emergency department visits, exact occurrence of asthma cannot be found. Second, when referring to community health research documents of 2009, in cases where patients were diagnosed with asthma by a doctor, treatment rate was 50.9%, but allergic rhinitis and atopic dermatitis were 30.7% and 35.6, respectively, which indicates that asthma, compared to other diseases, is well managed [25]. Therefore, if data are processed on a monthly basis, even if patients revisited the hospital within 1 month because of worsening condition, these revisiting patients, compared to the other two diseases, have less effect on the increase in the number of patients, which may lead to underestimation of the number of asthma patients. Third, along with its allergic response, asthma presents with a more serious respiratory infection caused by a virus [26]. Therefore, unlike winter, in summer, prevalence rate of asthma might have not increased because viral infection is less. Fourth, the effect of Typhoon Ewiniar might have not reflected on the change in the number of patients because its period was much longer than other disasters and the number of patients was greater. When observed separately, in many cases, it is indicated that the number of patients increased, even if not statistically significantly.
4.1. Limitations of this study
This study is limited in that it used health insurance data, which have problems such as incorrect coding of diagnosed disease. Furthermore, because emergency room visiting data were dropped, it may not be possible to discover the exact pattern in the occurrence of allergic diseases. Therefore, a follow-up study should inquire into the effect of typhoons and heavy rain on allergic diseases with more precisely processed National Health Insurance data.
Acknowledgments
This study was supported by Climate Change Adaptation Research Program through Korean Environment Policy Institute by the Ministry of Environment.
Footnotes
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
References
- 1.Intergovernmental Panel on Climate Change . Intergovernmental Panel on Climate Change; Geneva: 2007. IPCC fourth assessment report: climate change; pp. 44–53. [Google Scholar]
- 2.Lee S.J. Ministry of Environment; Seoul: 2010. Korea climate change valuation report 2010; pp. 19–73. [Google Scholar]
- 3.Reid C.E., Gamble J.L. Aeroallergens, allergic disease, and climate change: impacts and adaptation. Ecohealth. 2009 Sep;6(3):458–470. doi: 10.1007/s10393-009-0261-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yang H.J., Jeon Y.H., Min T.K. The impact of climate change on aeroalleregen and pediatric allergic diseases. J Korean Med Assoc. 2011 Sep;54(9):971–978. [Google Scholar]
- 5.Sheffield P.E., Weinberger K.R., Kinney P.L. Climate change, aeroallergens, and pediatric allergic disease. Mt Sinai J Med. 2011 Jan–Feb;78(1):78–84. doi: 10.1002/msj.20232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Shea K.M., Truckner R.T., Weber R.W., Peden D.B. Climate change and allergic disease. J Allergy Clin Immunol. 2008 Sep;122(3):443–453. doi: 10.1016/j.jaci.2008.06.032. [DOI] [PubMed] [Google Scholar]
- 7.Centers for Disease Control and Prevention (CDC) Health concerns associated with mold in water-damaged homes after Hurricanes Katrina and Rita: New Orleans area, Louisiana, October 2005. MMWR Morb Mortal Wkly Rep. 2006 Jan;55(2):41–44. [PubMed] [Google Scholar]
- 8.Solomon G.M., Hjelmroos-Koski M., Rotkin-Ellman M., Hammond S.K. Airborne mold and endotoxin concentrations in New Orleans, Louisiana, after flooding, October through November 2005. Environ Health Perspect. 2006 Sep;114(9):1381–1386. doi: 10.1289/ehp.9198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Epstein P.R., Mills E., Frith K., Linden E., Thomas B., Weireter R. Center for Health and the Global Environment; Boston: 2005. Climate change futures: health, ecological and economic dimensions; p. 142. [Google Scholar]
- 10.D'Amato G., Liccardi G., Frenguelli G. Thunderstorm-asthma and pollen allergy. Allergy. 2007 Jan;62(1):11–16. doi: 10.1111/j.1398-9995.2006.01271.x. [DOI] [PubMed] [Google Scholar]
- 11.Pulimood T.B., Corden J.M., Bryden C., Sharples L., Nasser S.M. Epidemic asthma and the role of the fungal mold Alternaria alternata. J Allergy ClinImmunol. 2007 Jan;120(3):610–617. doi: 10.1016/j.jaci.2007.04.045. [DOI] [PubMed] [Google Scholar]
- 12.Kim K.J. National Emergency Management Agency; Seoul: 2010. Annual report of disaster 2010; pp. 41–73. [Google Scholar]
- 13.Hornbrook M.C., Hurtado A.V., Johnson R.E. Health care episodes: definition, measurement and use. Med Care Rev. 1985 Fall;42(2):163–218. doi: 10.1177/107755878504200202. [DOI] [PubMed] [Google Scholar]
- 14.Rothman K.J., Greenland S., Lash T.L. Lippincott Williams & Wilkins; Philadelphia: 2008. Modern epidemiology; pp. 148–167. [Google Scholar]
- 15.Knowlton K., Rotkin-Ellman M., King G. The 2006 California heat wave: impacts on hospitalizations and emergency department visits. Environ Health Perspect. 2009;117(1):61–67. doi: 10.1289/ehp.11594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ma W., Xu X., Peng L., Kan H. Impact of extreme temperature on hospital admission in Shanghai, China. Sci Total Environ. 2011 Sep;409(19):3634–3637. doi: 10.1016/j.scitotenv.2011.06.042. [DOI] [PubMed] [Google Scholar]
- 17.Anderson W., Prescott G.J., Packham S., Mullins J., Brookes M., Seaton A. Asthma admissions and thunderstorms: a study of pollen, fungal spores, rainfall, and ozone. QJM. 2001 Aug;94(8):429–433. doi: 10.1093/qjmed/94.8.429. [DOI] [PubMed] [Google Scholar]
- 18.Langenberg W.J., Sutton J.C., Gillespie T.J. Relation of weather variables and periodicities of airborne spores of Alternaria dauci. Phytopathology. 1977 Jul;67(7):879–883. [Google Scholar]
- 19.Rao C.Y., Riggs M.A., Chew G.L. Characterization of airborne molds, endotoxins, and glucans in homes in New Orleans after Hurricanes Katrina and Rita. Appl Environ Microbiol. 2007 Mar;73(5):1630–1634. doi: 10.1128/AEM.01973-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zock J.P., Jarvis D., Luczynska C., Sunyer J., Burney P. European Community Respiratory Health Survey. Housing characteristics, reported mold exposure, and asthma in the European Community Respiratory Health Survey. J Allergy ClinImmunol. 2002 Aug;110(2):285–292. doi: 10.1067/mai.2002.126383. [DOI] [PubMed] [Google Scholar]
- 21.Rhoads J., Pearman T., Rick S. Clinical presentation and therapeutic interventions for posttraumatic stress disorder post-Katrina. Arch Psychiatr Nurs. 2007 Oct;21(5):249–256. doi: 10.1016/j.apnu.2007.05.002. [DOI] [PubMed] [Google Scholar]
- 22.Jaakkola J.J., Hwang B.F., Jaakkola M.S. Home dampness and molds as determinants of allergic rhinitis in childhood: a 6-year, population-based cohort study. Am J Epidemiol. 2010 Aug;172(4):451–459. doi: 10.1093/aje/kwq110. [DOI] [PubMed] [Google Scholar]
- 23.Wahn U. What drives the allergic march? Allergy. 2000 Jul;55(7):591–599. doi: 10.1034/j.1398-9995.2000.00111.x. [DOI] [PubMed] [Google Scholar]
- 24.Wardman A.E., Stefani D., MacDonald J.C. Thunderstorm-associated asthma or shortness of breath epidemic: a Canadian case report. Can Respir J. 2002 Jul–Aug;9(4):267–270. doi: 10.1155/2002/728257. [DOI] [PubMed] [Google Scholar]
- 25.Jeon B.Y. Korea Center for Disease Control; Cheongwon: 2012. Community health survey data guide book; pp. 104–207. [Google Scholar]
- 26.Eder W., Ege M.J., von Mutius E. The asthma epidemic. N Engl J Med. 2006 Nov;355(21):2226–2235. doi: 10.1056/NEJMra054308. [DOI] [PubMed] [Google Scholar]


