Abstract
Background
Despite the initial absolute or relative contraindication of laparoscopic surgery during pregnancy, in the last decade, laparoscopic appendectomy (LA) has been performed in pregnant women. But few studies compare the outcomes of LA compared with open appendectomy (OA). We investigated clinical outcomes to evaluate the safety and efficacy of LA compared with OA in pregnant women.
Methods
We recruited consecutive pregnant patients with a diagnosis of acute appendicitis who were undergoing LA or OA between May 2007 and August 2011 into the study.
Results
Sixty-one patients (22 LA and 39 OA) enrolled in our study. There were no significant differences in duration of surgery, postoperative complication rate and obstetric and fetal outcomes, including incidence of preterm labour, delivery type, gestation age at delivery, birth weight and APGAR scores between the 2 groups. However, the LA group had shorter time to first flatus (2.4 ± 0.4 d v. 4.0 ± 1.7 d, p = 0.034), earlier time to oral intake (2.3 ± 1.6 d v. 4.1 ± 1.9 d, p = 0.023) and shorter postoperative hospital stay (4.2 ± 2.9 d v. 6.9 ± 3.7 d, p = 0.043) than the OA group.
Conclusion
Laparoscopic appendectomy is a clinically safe and effective procedure in all trimesters of pregnancy and should be considered as a standard treatment alternative to OA. Further evaluation including prospective randomized clinical trials comparing LA with OA are needed to confirm our results.
Abstract
Contexte
Malgré une contre-indication initiale absolue ou relative de l’opération laparoscopique durant la grossesse au cours de la dernière décennie, on a eu recours à l’appendicectomie laparoscopique (AL) chez des femmes enceintes. Mais peu d’études ont comparé les résultats de l’AL à ceux de l’appendicectomie ouverte (AO). Nous avons analysé les résultats cliniques pour comparer l’innocuité et l’efficacité de l’AL à celles de l’AO chez les femmes enceintes.
Méthodes
Pour la présente étude, nous avons recruté des patientes enceintes consécutives porteuses d’un diagnostic d’appendicite aiguë qui ont dû subir une AL ou une AO entre mai 2007 et août 2011.
Résultats
Soixante-et-une patientes (22 soumises à l’AL et 39 à l’AO) ont été inscrites à notre étude. Nous n’avons noté aucune différence significative pour ce qui est de la durée de l’intervention chirurgicale, du taux de complications postopératoires et des résultats obstétricaux et fœtaux, y compris l’incidence du travail prématuré, le type d’accouchement, l’âge gestationnel et le poids à la naissance et les indices d’APGAR entre les 2 groupes. Toutefois, le groupe soumis à l’AL a moins tardé à présenter des flatuosités (2,4 ± 0,4 j c. 4,0 ± 1,7 j, p = 0,034), a commencé à s’alimenter par la bouche plus tôt (2,3 ± 1,6 j c. 4,1 ± 1,9 j, p = 0,023) et a connu un séjour hospitalier postopératoire plus bref (4,2 ± 2,9 j c. 6,9 ± 3,7 j, p = 0,043) comparativement au groupe soumis à l’AO.
Conclusion
L’appendicectomie laparoscopique est une intervention sécuritaire et efficace au plan clinique durant les 3 trimestres de la grossesse, et il faut l’envisager comme solution de rechange thérapeutique standard à l’AO. Il faudra une évaluation plus approfondie pour confirmer nos résultats, y compris au moyen d’essais cliniques randomisés prospectifs comparant l’AL à l’AO.
Acute appendicitis is the most common nonobstetric condition requiring emergency surgery during pregnancy, with an estimated incidence between 0.05% and 0.13%.1 Although the incidence of acute appendicitis during pregnancy is similar to that in nonpregnant women, the rate of complicated appendicitis is much higher in pregnant women.2 Delay in diagnosis increases the risk of complications in the mother and fetus. When acute appendicitis is suspected, an aggressive approach is recommended.3 In nonpregnant patients, the advantages of laparoscopic appendectomy (LA), including reduced postoperative pain, fewer wound infections, earlier hospital discharge and faster return to work, are widely accepted.4 Despite the initial absolute or relative contraindication of laparoscopic surgical procedures during pregnancy, in the last decade LA has been performed in pregnant women.5 Although there have been no prospective randomized controlled trials studying LA in pregnant women, several reports have documented the feasibility, safety and effectiveness of LA in this population.1,2,4–9 However, these reports include case reports and small series, so their results are limited. In particular, there is very limited information on the outcomes of LA compared with open appendectomy (OA). Therefore, we investigated clinical outcomes to evaluate the safety and efficacy of LA compared with OA in pregnant women.
Methods
We recruited consecutive pregnant women with a diagnosis of acute appendicitis who underwent LA (study cohort) or OA (control cohort) between May 2007 and August 2011. Ultrasounds and complete blood counts (CBC) were routinely obtained preoperatively. We confirmed the diagnosis of acute appendicitis by clinical examination and ultrasonography. All patients received preoperative and postoperative obstetric consultations and fetal monitoring. We retrospectively analyzed the medical records to compare the 2 groups. Preoperative clinical data included age, body mass index (BMI), gestation age at operation, incidence of previous Caesarean section and accuracy of the diagnostic ultrasound. Perioperative data included the duration of surgery, return to normal bowel movement, return to adequate oral intake, length of stay in hospital (LOS), postoperative complications and final pathology. Obstetric and fetal data included gestation age at delivery, incidence of preterm labour, delivery type, birth weight, APGAR scores at 1 minute and 5 minutes, and fetal mortality.
Laparoscopic appendectomy technique in pregnant women
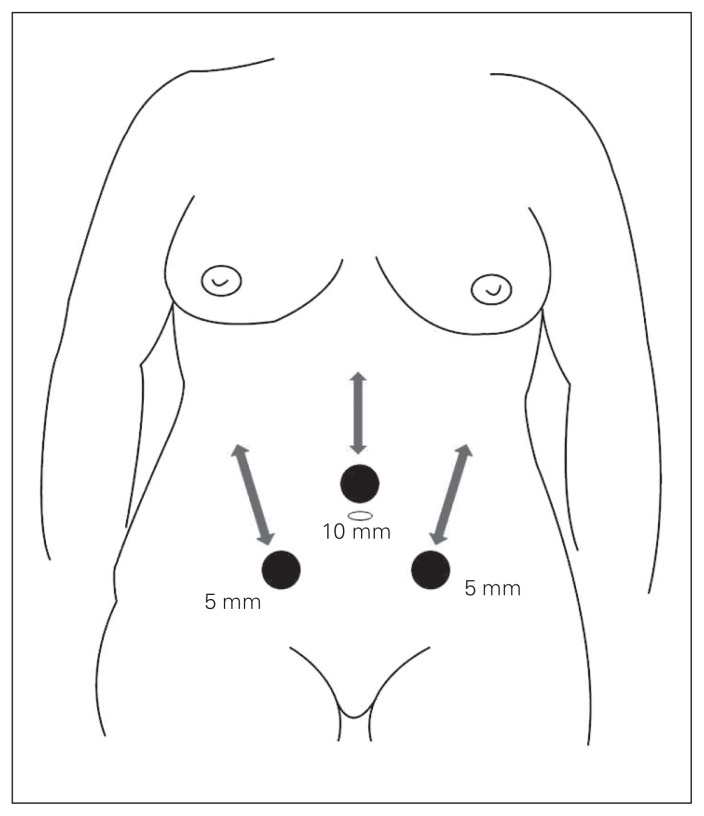
The patient was placed on the table in the supine position with a slight left side tilt (20°–30°). We performed the procedure with the patient under general anesthesia and maintained continuous end-tidal CO2 monitoring within the physiologic range (30–40 mm Hg). Routinely, we inserted a Foley catheter, used pneumatic compression devices on the legs and administered prophylactic antibiotics intravenously before the incision. In all patients, we entered the peritoneal cavity using the Hasson open technique, and the procedure was performed using 3 ports. First, we inserted a 10 mm balloon trocar (telescope route) supraumbilically according to the size of the uterus (3–4 cm above the uterine fundus), and pneumoperitoneum (10–12 mm Hg) was achieved by CO2 insufflation. Subsequently, 2 working 5 mm trocars were inserted, depending on the gestation age (Fig. 1). The appendix was then elevated using a left-handed forceps, and the mesoappendix was divided using a harmonic scalpel (Ethicon). The appendiceal stump was ligated using endo-loop (Ethicon) and transected using endo-scissors. The specimen was then placed in a Lap Bag® (SJM) and removed through the umbilical port site. One closed suction drain was left next to the appendiceal stump.
Fig. 1.
Trocar placement for laparoscopic appendectomy in different stages of pregnancy.
Statistical analysis
Data are presented as means ± standard deviations. We compared the groups using the Mann–Whitney U test or χ2 test, as appropriate. We used SPSS version 14.0 for Windows for all statistical comparisons, and we considered results to be significant at p < 0.05.
Results
Participants
Sixty-one patients enrolled in our study. In all 22 patients who had LA, the procedure was completed laparoscopically without conversion, and 39 OAs were performed in patients who refused LA. The mean age of the LA group was 29.3 ± 3.1 years, and that of the OA group was 31.4 ± 4.3 years (p = 0.45). There were no significant differences in BMI (22.7 ± 2.8 v. 22.8 ± 3.6, p = 0.83) or the gestation age at operation (16.4 ± 5.7 wk v. 16.7 ± 4.8 wk, p = 0.80) between the groups. In the LA group, 6 (27.3%) patients were in the first trimester, 13 (59.1%) were in the second trimester and 3 (13.6%) were in the third trimester. In the OA group, 8 (20.5%) patients were in the first trimester, 20 (51.3%) were in the second trimester and 11 (28.2%) were in the third trimester. The rate of previous Caesarean section in the LA group was 18.2%, and that of the OA group was 20.5% (p = 0.64). In all patients, we obtained an ultrasound preoperatively to clarify the diagnosis of acute appendicitis. There were no significant differences in the rate of false positive (9.1 v. 10.3%, p = 0.65) and false negative results (22.7 v. 17.9%, p = 0.16) between the groups (Table 1). Table 2 demonstrates the postoperative histopathological diagnoses in both groups. In the LA group, 2 (9.1%) patients had a normal appendix, 12 (54.6%) had focal appendicitis, 7 (31.8%) had supparative appendicitis and 1 (4.5%) had gangrenous appendicitis. In the OA group, 4 (10.3%) patients had a normal appendix, 19 (48.7%) had focal appendicitis, 10 (25.6%) had supparative appendicitis and 6 (15.4%) had gangrenous appendicitis.
Table 1.
Demographic and clinical characteristics of pregnant women undergoing laparoscopic or open appendectomy
| Characteristic | Group; mean ± SD or no. (%) | p value | |
|---|---|---|---|
| LA, n = 22 | OA, n = 39 | ||
| Age, yr | 29.3 ± 3.1 | 31.4 ± 4.3 | 0.45 |
| BMI | 22.7 ± 2.8 | 22.8 ± 3.6 | 0.83 |
| Gestation age at operation, wk | 16.4 ± 5.7 | 16.7 ± 4.8 | 0.80 |
| First trimester | 6 (27.3) | 8 (20.5) | |
| Second trimester | 13 (59.1) | 20 (51.3) | |
| Third trimester | 3 (13.6) | 11 (28.2) | |
| Previous Caesarean section | 4 (18.2) | 8 (20.5) | 0.64 |
| Preoperative ultrasonography | 22 (100) | 39 (100) | — |
| False-positive ultrasound | 2 (9.1) | 4 (10.3) | 0.65 |
| False-negative ultrasound | 5 (22.7) | 7 (17.9) | 0.16 |
BMI = body mass index; LA = laparoscopic appendectomy; OA = open appendectomy; SD = standard deviation.
Table 2.
Final histopathological diagnosis after operation
| Stage; diagnosis | Group; no. (%) | |
|---|---|---|
| LA, n = 22 | OA, n = 39 | |
| First trimester | 6 (27.3) | 8 (20.5) |
| Normal appendix | 1 | 1 |
| Focal appendicitis | 3 | 4 |
| Supparative appendicitis | 2 | 2 |
| Gangrenous appendicitis | 0 | 1 |
| Second trimester | 13 (59.1) | 20 (51.3) |
| Normal appendix | 1 | 2 |
| Focal appendicitis | 7 | 10 |
| Supparative appendicitis | 4 | 6 |
| Gangrenous appendicitis | 1 | 2 |
| Third trimester | 3 (13.6) | 11 (28.2) |
| Normal appendix | 0 | 1 |
| Focal appendicitis | 2 | 5 |
| Supparative appendicitis | 1 | 2 |
| Gangrenous appendicitis | 0 | 3 |
LA = laparoscopic appendectomy; OA = open appendectomy.
Perioperative outcomes
The mean duration of surgery in the LA group was 44.2 ± 16.4 minutes, and that in the OA group was 47.3 ± 14.7 minutes. The mean time to normal bowel movement in the LA group was significantly shorter than that in the OA group (2.4 ± 0.4 d v. 4.0 ± 1.7 d, p = 0.034). Also, the mean time to adequate oral intake in the LA group was earlier than in the OA group (2.3 ± 1.6 d v. 4.1 ± 1.9 d, p = 0.023). The mean LOS in the LA group was 4.2 ± 2.9 days, and that of the OA group was 6.9 ± 3.7 days (p = 0.043). Three patients experienced complications, including intra-abdominal abscess and wound infection. In the LA group, an intra-abdominal abscess developed in 1 (4.5%) patient after surgery. This 29-year-old woman with a gestation age of 18 weeks was treated successfully with antibiotics and delivered a healthy boy weighing 3720 g at a gestation age of 40 weeks. In the OA group, 2 (5.1%) patients experienced complications (intra-abdominal abscess, wound infection) after surgery. The intra-abdominal abscess developed in a 33-year-old woman at 28 weeks’ gestation. She was treated successfully with percutaneous drainage and delivered a healthy girl weighing 2670 g at a gestation age of 37 weeks. Wound infection was treated conservatively. No statistical difference was observed in the rate of the complication between the groups (Table 3).
Table 3.
Perioperative outcomes of laparoscopic or open appendectomy in pregnant women
| Outcome | Group; mean ± SD* | p value | |
|---|---|---|---|
| LA, n = 22 | OA, n = 39 | ||
| Operation time, min | 44.2 ± 16.4 | 47.3 ± 14.7 | 0.48 |
| Time to first flatus, d | 2.4 ± 0.4 | 4.0 ± 1.7 | 0.034 |
| Time to oral intake, d | 2.3 ± 1.6 | 4.1 ± 1.9 | 0.023 |
| Postoperative LOS, d | 4.2 ± 2.9 | 6.9 ± 3.7 | 0.043 |
| Complication rate, n (%) | 1 (4.5) | 2 (5.1) | 0.76 |
LA = laparoscopic appendectomy; LOS = length of stay in hospital; OA = open appendectomy; SD = standard deviation.
Unless otherwise indicated.
Obstetric and fetal outcomes
No patients were lost to follow-up, and they all had uncomplicated deliveries. There were no significant differences in the incidence of preterm labour (9.1 v. 10.3%, p = 0.66) or delivery type (p = 0.41) between the groups. The LA and OA groups had equivalent fetal outcomes, as demonstrated by gestational age at delivery, birth weight and APGAR scores (Table 4).
Table 4.
Obstetric and fetal outcomes of laparoscopic or open appendectomy in pregnant women
| Outcome | Group; mean ± SD or no. (%) | p value | |
|---|---|---|---|
| LA, n = 22 | OA, n = 39 | ||
| Gestation age at delivery, wk | 37.1 ± 1.7 | 38.2 ± 3.5 | 0.48 |
| Preterm labour | 2 (9.1) | 4 (10.3) | 0.66 |
| Delivery type | 0.41 | ||
| Vaginal delivery | 16 (72.7) | 25 (64.1) | |
| Caesarean section | 6 (27.3) | 14 (35.9) | |
| Birth weight, g | 2810 ± 293 | 2790 ± 312 | 0.79 |
| APGAR score, 1 min | 9.2 ± 0.1 | 9.3 ± 0.2 | 0.70 |
| APGAR score, 5 min | 9.8 ± 0.2 | 9.9 ± 0.1 | 0.73 |
| Fetal loss | 0 (0) | 0 (0) | — |
LA = laparoscopic appendectomy; OA = open appendectomy; SD = standard deviation.
Discussion
Although acute appendicitis is the most common cause of nonobstetric abdominal surgery during pregnancy and its incidence is similar to that in nonpregnant women, the diagnosis is difficult because of the anatomic and physiologic changes that occur during pregnancy.5 The risk for appendicitis does not appear to be increased by pregnancy, but the incidence of perforated appendicitis in pregnant women is much higher than in the general population.2 The reported rate of appendiceal perforation during pregnancy can be as high as 43%, compared with 19% in the general population.1 Complicated appendicitis can lead to maternal and fetal morbidity and even fetal loss, so pregnant women with suspected appendicitis should undergo surgery immediately, regardless of the gestation age of the fetus.3,10,11 The number of negative laparoscopic and open exploration rates during pregnancy ranges from 0% to 50% and 15% to 50%, respectively.1 In our study, the overall negative appendectomy rate was 9.8% (9.1% for the LA group and 10.3% for the OA group).
Diagnostic imaging studies are often used to clarify a confusing clinical picture. Ultrasonography is widely used as a first-line diagnostic test because of its safety for the mother and fetus and its relatively high sensitivity and specificity for many intra-abdominal processes.12 In our study, ultrasonography was performed in all patients; acute appendicitis was found in 15 (68.2%) patients in the LA group and 28 (71.8%) in the OA group.
Conventionally, the treatment of choice for acute appendicitis during pregnancy has been OA. But there is no evidence that the benefits of OA outweigh those of LA in pregnant women with respect to perioperative morbidity and mortality.13 In the present study, the absence of significant differences in the analysis of clinical details suggests that our 2 groups had relatively similar preoperative conditions. Our study also supports the safety of LA because we found no differences in perioperative morbidity and mortality compared with OA. Moreover, some proven advantages of LA, including better intraoperative visualization, decreased surgical trauma, decreased gravid uterine manipulation, shorter postoperative LOS and faster return to work, may be even more important in pregnant women.7 In our study, the LA group had significantly shorter postoperative LOS, earlier recovery of bowel function and shorter time to oral intake than the OA group.
It has been recommended to position the patient on her left side during surgery to prevent uterine compression of the inferior vena cava and to facilitate access to the appendix.6 Morrell and colleagues14 have suggested lateral rotation of the operating table to displace the uterus for better venous return. In our hospital, all pregnant patients were placed in a supine position with a slight left side tilt (20°–30°).
There is consensus that laparoscopic procedures are safest in the second trimester of pregnancy because the uterus, owing to its small size, is less susceptible to traumatic injuries.1 Some authors have suggested that laparoscopic procedures performed during the first trimester are usually associated with greater risk for fetal loss because of teratogenicity of medications and decreased uterine blood due to the pneumoperitoneum.15 An advanced gestation age was previously regarded as a contraindication for LA because of expected technical difficulties.6 However, Upadhyay and colleagues10 demonstrated that laparoscopic surgery in the third trimester of pregnancy is feasible and can be performed safely, and they recommended laparoscopic surgery in all 3 trimesters. In our study, LA was performed safely in all 3 trimesters without fetal mortality.
One of the most important concerns during LA in pregnancy is the potential risk of injury to the gravid uterus. Some debate exists about the best method to access the abdomen. The Veress needle or the Hasson open technique can be used to gain initial abdominal access. Even though complications have been described for all methods, spontaneous puncture of the uterus with a Veress needle is the most serious.16 Friedman and colleagues17 reported results in a young pregnant woman at 21 weeks’ gestation who underwent LA for suspected appendicitis. A Veress needle injury to the serosa of the gravid uterus resulted in postoperative pneumoamnion and subsequent fetal loss. In our hospital, the peritoneal cavity was entered using the Hasson open technique, and there was no injury to the gravid uterus. We consider the Hasson open technique to be completely safe and suggest that it should be the standard method in pregnant women, in accordance with the Society of American Gastrointestinal Endoscopic Surgeons (SAGES) guidelines.12
Achieving pneumoperitoneum during laparoscopy is another concern. The CO2 used for pneumoperitoneum is associated with pulmonary effects in pregnant women and a potential risk for acidosis in the fetus. It has been recommended that intra-abdominal pressure should be maintained at less than 12 mm Hg to avoid worsening pulmonary physiology in pregnant women.18 Previously published animal studies reported no adverse fetal effects of CO2 insufflation when the maximal intra-abdominal pressure was limited to 10–12 mm Hg for less than 60 minutes.13 Although studies have demonstrated that laparoscopic surgery can be performed safely during any trimester with good maternal and fetal outcomes, the long-term effects on the child after delivery have not been well studied.16 In the present study, intra-abdominal pressure was maintained at 10–12 mm Hg and the duration of surgery was less than 60 minutes (mean duration of LA 44.2 ± 16.4 min).
Stasis of blood in the lower extremities is common during pregnancy, so pregnant women are at high risk for thromboembolitic complications. According to the SAGES guidelines, intraoperative and postoperative pneumatic compression devices and early postoperative ambulation are recommended to prevent deep vein thrombosis in pregnant patients.12 In the present study, we routinely used pneumatic compression devices, and there were no thromboembolitic complications.
Conclusion
Our results show that LA is safe and effective in all trimesters and that it is associated with good maternal and fetal outcomes similar to those of OA. In addition, LA is associated with shorter postoperative LOS, earlier recovery of bowel function and shorter time to oral intake. On the basis of our results and considering the general advantages of laparoscopic surgery, LA in pregnant women should be considered as a standard treatment alternative to OA. Further evaluation, including prospective randomized clinical trials comparing LA with OA, are needed to confirm these results.
Footnotes
Competing interests: None declared.
Contributors: J.C. Chung designed the study and wrote the article. G.S. Cho and H.C. Kim acquired the data, which J.C. Chung, E.J. Shin and O.P. Song analyzed. All authors reviewed the article and approved it for publication.
References
- 1.Kirshtein B, Perry ZH, Avinoach E, et al. Safety of laparoscopic appendectomy during pregnancy. World J Surg. 2009;33:475–80. doi: 10.1007/s00268-008-9890-4. [DOI] [PubMed] [Google Scholar]
- 2.Corneille MG, Gallup TM, Bening T, et al. The use of laparoscopic surgery in pregnancy: evaluation of safety and efficacy. Am J Surg. 2010;200:363–7. doi: 10.1016/j.amjsurg.2009.09.022. [DOI] [PubMed] [Google Scholar]
- 3.McGory ML, Zingmond DS, Tillou A, et al. Negative appendectomy in pregnant women is associated with a substantial risk of fetal loss. J Am Coll Surg. 2007;205:534–40. doi: 10.1016/j.jamcollsurg.2007.05.025. [DOI] [PubMed] [Google Scholar]
- 4.de Bakker JK, Dijksman LM, Donkervoort SC. Safety and outcome of general open and laparoscopic procedures during pregnancy. Surg Endosc. 2011;25:1574–8. doi: 10.1007/s00464-010-1441-z. [DOI] [PubMed] [Google Scholar]
- 5.Moreno-Sanz C, Pascual-Pedreño A, Picazo-Yeste JS, et al. Laparoscopic appendectomy during pregnancy: between personal experiences and scientific evidence. J Am Coll Surg. 2007;205:37–42. doi: 10.1016/j.jamcollsurg.2007.01.068. [DOI] [PubMed] [Google Scholar]
- 6.Curet MJ, Allen D, Josloff RK, et al. Laparoscopy during pregnancy. Arch Surg. 1996;131:546–50. doi: 10.1001/archsurg.1996.01430170092017. [DOI] [PubMed] [Google Scholar]
- 7.Lyass S, Pikarsky A, Eisenberg VH, et al. Is laparoscopic appendectomy safe in pregnant women? Surg Endosc. 2001;15:377–9. doi: 10.1007/s004640000368. [DOI] [PubMed] [Google Scholar]
- 8.Sadot E, Telem DA, Arora M, et al. Laparoscopy: a safe approach to appendicitis during pregnancy. Surg Endosc. 2010;24:383–9. doi: 10.1007/s00464-009-0571-7. [DOI] [PubMed] [Google Scholar]
- 9.Hannan MJ, Hoque MM, Begum LN. Laparoscopic appendectomy in pregnant women: experience in Chittagong, Bangladesh. World J Surg. 2012;36:767–70. doi: 10.1007/s00268-012-1445-z. [DOI] [PubMed] [Google Scholar]
- 10.Upadhyay A, Stanten S, Kazantsev G, et al. Laparoscopic management of a nonobstetric emergency in the third trimester of pregnancy. Surg Endosc. 2007;21:1344–8. doi: 10.1007/s00464-006-9104-9. [DOI] [PubMed] [Google Scholar]
- 11.Carver TW, Antevil J, Egan JC, et al. Appendectomy during early pregnancy: What is the preferred surgical approach? Am Surg. 2005;71:809–12. [PubMed] [Google Scholar]
- 12.Yumi H. Guidelines for diagnosis, treatment, and use of laparoscopy for surgical problems during pregnancy: this statement was reviewed and approved by the Board of Governors of the Society of American Gastrointestinal and Endoscopic Surgeons (SAGES), September 2007. It was prepared by the SAGES Guidelines Committee. Surg Endosc. 2008;22:849–61. doi: 10.1007/s00464-008-9758-6. [DOI] [PubMed] [Google Scholar]
- 13.Park SH, Park MI, Choi JS, et al. Laparoscopic appendectomy performed during pregnancy by gynecological laparoscopists. Eur J Obstet Gynecol Reprod Biol. 2010;148:44–8. doi: 10.1016/j.ejogrb.2009.09.026. [DOI] [PubMed] [Google Scholar]
- 14.Morrell DG, Mullins JR, Harrison PB. Laparoscopic cholecystectomy during pregnancy in symptomatic patients. Surgery. 1992;112:856–9. [PubMed] [Google Scholar]
- 15.Cohen-Kerem R, Railton C, Oren D, et al. Pregnancy outcome following non-obstetric surgical intervention. Am J Surg. 2005;190:467–73. doi: 10.1016/j.amjsurg.2005.03.033. [DOI] [PubMed] [Google Scholar]
- 16.Machado NO, Grant CS. Laparoscopic appendectomy in all trimesters of pregnancy. JSLS. 2009;13:384–90. [PMC free article] [PubMed] [Google Scholar]
- 17.Friedman JD, Ramsey PS, Ramin KD, et al. Pneumoamnion and pregnancy loss after second-trimester laparoscopic surgery. Obstet Gynecol. 2002;99:512–3. doi: 10.1016/s0029-7844(01)01664-7. [DOI] [PubMed] [Google Scholar]
- 18.Malangoni MA. Gastrointestinal surgery and pregnancy. Gastroenterol Clin North Am. 2003;32:181–200. doi: 10.1016/s0889-8553(02)00072-9. [DOI] [PubMed] [Google Scholar]