Sir,
Epidural fat surrounds dura mater, which engulfs arachnoid mater followed by subarachnoid space, pia mater, and spinal cord. Although not usually found in the cervical region, epidural fat is commonly found along thoracic and lumbo-sacral regions. Epidural fat is soft and protects the spinal cord and dorsal-ventral rami. When epidural fat accumulates, it can impinge on subarachnoid space and restrict nerve movement within the thecal sac. Exogenous steroid use is the most common cause of epidural lipomatosis (non-neoplastic overgrowth of adipose tissue within the epidural space of spinal canal[1]) and accounts for about 55% of cases.[2] The less common causes are obesity (25%), Cushing's syndrome (3%) and idiopathic (17%).[2] Epidural lipomatosis can have various presentations including low back pain with or without lower extremity numbness and weakness. Though, true prevalence of epidural lipomatosis in pain patients is not known, two patients presented to our pain clinic with unrelenting lower back pain and incidental diagnosis of underlying pre-existent epidural lipomatosis that complicated the natural course for their interventional pain management.
Our patients had lower back pain with radiations to bilateral lower extremities. The pains were described as constant throbbing, aching, and cramping that worsened with activity. They were treated with an opioid and non-opioid medications with minimal relief. Per lumbar spine magnetic resonance imaging (MRI), revealed epidural lipomatosis which was impinging on their spinal nerve roots [Figures 1 and 2]. The first patient (a 64-year-old African American female) was treated with a lumbar medial branch blocks without any steroids, but reported no pain relief. The second patient (a 57-year-old African American male) was treated with the lumbar medial branch blocks without any steroids followed by radiofrequency ablations; however, reported no long lasting pain relief. Even though, MRI spine also showed coexistent mild spinal stenosis in the first patient and intervertebral disc herniation in the second patient, epidural lipomatosis was suspected as one of the primary causes for their unrelenting and unresponsive mixed component-back pains. Therefore, due to their poor responses to interventional pain procedures, it was decided to abandon these procedures. Besides counseling for avoidance of exogenous steroids (like inhaled steroids for lung diseases) and enrollment to physical therapy, they were referred to weight loss programs and neurosurgery consultations (weight loss of 15 kg or more required[3]), decompressive laminectomy and fat debulking[4] as definitive treatments for epidural lipomatosis.
Figure 1.
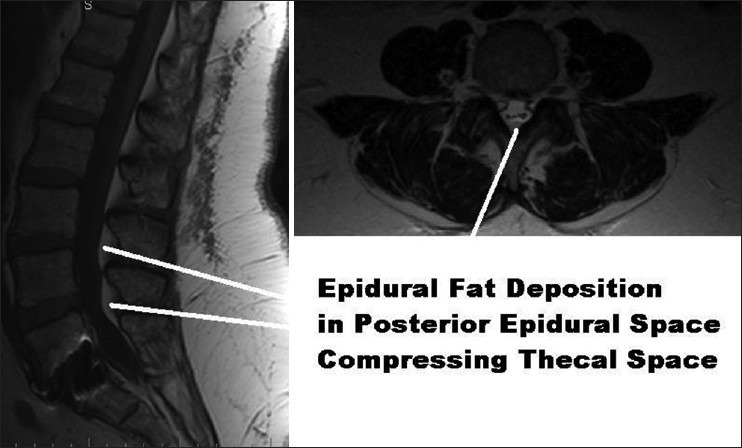
T1-weighted MRI image of lumbosacral spine (sagittal image) and lumbar spine (axial image) showing epidural fat deposition in posterior epidural space compressing thecal space
Figure 2.
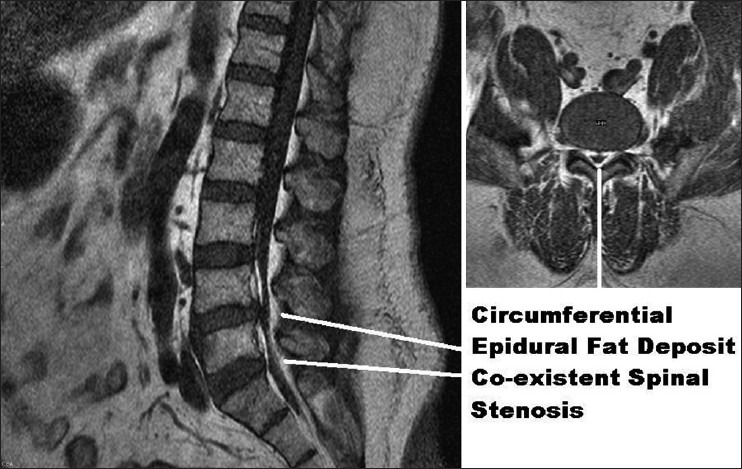
T1-weighted MRI image of lumbosacral spine (sagittal image) and lumbar spine (axial image) showing circumferential epidural fat deposits with co-existent spinal stenosis
In summary, though epidural lipomatosis is one of the many etiologies that complicate pain diagnosis and interventional pain management, all difficult back pains should be evaluated for their multi-factorial (mixed component) underlying mechanisms and consequently receive case-appropriate multimodal pain management that may or may not include interventional pain procedures. The MRI-based early diagnosis and staging[5] of epidural lipomatosis (that may present with or without symptoms) directs pain physicians to consider epidural lipomatosis as an absolute contraindication for interventional pain procedures with steroids because epidural interventions may fail to provide analgesia due to epidural fat stuffing up the spinal canal and epidural steroids may accentuate adipose deposition in the epidural space that can worsen pain and neurological symptoms.
References
- 1.Flisberg P, Thomas O, Geijer B, Schött U. Epidural lipomatosis and congenital small spinal canal in spinal anaesthesia: A case report and review of the literature. J Med Case Rep. 2009;3:128. doi: 10.1186/1752-1947-3-128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fogel GR, Cunningham PY, 3rd, Esses SI. Spinal epidural lipomatosis: Case reports, literature review and meta-analysis. Spine J. 2005;5:202–11. doi: 10.1016/j.spinee.2004.05.252. [DOI] [PubMed] [Google Scholar]
- 3.Robertson SC, Traynelis VC, Follett KA, Menezes AH. Idiopathic spinal epidural lipomatosis. Neurosurgery. 1997;41:68–74. doi: 10.1097/00006123-199707000-00015. [DOI] [PubMed] [Google Scholar]
- 4.Lee RK, Chau LF, Yu KS, Lai CW. Idiopathic spinal epidural lipomatosis. J HK Coll Radiol. 2002;5:105–8. [Google Scholar]
- 5.Borré DG, Borré GE, Aude F, Palmieri GN. Lumbosacral epidural lipomatosis: MRI grading. Eur Radiol. 2003;13:1709–21. doi: 10.1007/s00330-002-1716-4. [DOI] [PubMed] [Google Scholar]


