Abstract
Background:
As with most neurologic conditions, stroke involves impairment of the swallowing mechanism. This could be a spectrum of issues, the worst of which is aspiration. At the same time, the prolonged presence of a naso-gastric tube (NGT) has its own morbidity. Flexible endoscopic evaluation of swallowing (FEES) is one reliable method to assess the structural and functional status of the oropharynx and larynx, during the swallowing process.
Objective:
To study the utility of FEES in decision-making with respect to resumption of oral intake in stroke patients. To document the findings of FEES in stroke patients, and to look for correlations between these and the site of stroke.
Materials and Methods:
Protocol insertion of naso-gastric tube in all stroke patients, at presentation. Initial assessment by a neurologist and swallowing therapist, depending on cognitive status of the patient. All patients underwent MRI Brain with diffusion weighted sequences. After detailed clinical examination, they underwent swallow exercises under the supervision of a trained swallowing therapist. The decision to remove NGT was taken clinically by the combined decision of neurologist and swallowing therapist. Then all patients underwent FEES by the ENT surgeon. The final decision for NGT removal was taken as per the FEES findings.
Result:
Sixteen stroke patients underwent the FEES procedure during a period of six months. The oropharyngeal and laryngeal findings varied depending on the area of stroke involvement. Of these, change in decision regarding swallowing rehabilitation or NGT removal was needed in four patients, following the FEES findings.
Conclusions:
FEES is an easy, efficient and reliable method to evaluate the swallowing status in stroke patients. In combination with good bedside clinical examination and swallow exercises, it can be a good tool in assessing patients with post- stroke dysphagia. Post-stroke rehabilitation and prevention of aspiration pneumonia can be effectively done with the help of FEES.
Keywords: Dysphagia, flexible endoscopic evaluation of swallowing, stroke
Introduction
The term dysphagia refers to difficulty in eating due to any malfunction in the swallowing process. It is one of the causes of morbidity following a cerebrovascular accident. The evaluation of swallowing disorders and their rehabilitative modalities are evolving topics. The benefit to the patient, in terms of improvement in quality of life, cannot be underestimated. Many studies have attempted to assess the utility and efficacy of the various methods used to tackle the problem.[1,2]
As with many other neurological disorders, stroke often leads to an impairment of the swallowing mechanism. There is a proven high incidence of aspiration with the potential to cause pneumonia.[3,4] This is a significant factor causing mortality in stroke. Hence, care needs to be taken by the treating stroke team to prevent this complication.
The initial management of dysphagia in stroke often consists of the insertion of a naso-gastric tube (NGT). This is followed by bedside assessment of the return of normal swallowing process, and decision for NGT removal. While this suffices in most cases, occasionally there exists a doubt about aspiration. This necessitates a more precise method of evaluation. Here, two modalities have been described: Flexible endoscopic evaluation of swallowing (FEES) and video-fluoroscopic study of swallowing (VFSS).
It is our contention that FEES suffices to look for laryngeal penetration of oral feeds and to take the final decision about NGT removal, in those patients at risk. We present a report of our experience with FEES assessment. Also, we have documented all the findings, to look for association between the area of involvement of stroke and the type of impairment.
We believe that this is the first such study in India.
Materials and Methods
Sixteen patients with ischemic stroke and dysphagia admitted in the stroke unit of Department of Neurology, Amrita Institute of Medical Sciences and Research Centre, Kochi, a tertiary care centre, were included in this single centre study. This prospective study was completed in six months between January and June 2012. The patients were randomly selected. All of them underwent limited MRI Brain imaging involving FLAIR and diffusion weighted sequences, which we call the MRI Stroke Protocol in our institution.
All patients were initially on NGT. Once fully conscious, alert, able to communicate and sit with support, they were clinically examined especially for lower cranial nerve findings. Dysphagia was confirmed after examination by a neurologist and qualified swallow therapist.
Patients with altered sensorium, receptive aphasia or significant apraxia were excluded from the study.
The patients were then initiated on standard oromotor exercises which helped to increase the range of movement in tongue, lips and jaw and lead to better speech and swallow functions. Once they started swallowing semisolids, postural strategies like chin tuck, head rotation, head tilt, and neck extension along with rehabilitative manoeuvres were taught. They were trained and encouraged to do these exercises at least ten times per day. The bystanders too were instructed to support and encourage these efforts.
Clinical examinations were done systematically in a stepwise manner and decision to remove the NGT was taken by the treating physician and the swallow therapist together.
Clinical systematic examination
Bedside evaluation of swallowing which includes initial assessment of
Cognitive status
Voluntary cough
Throat clearing
Saliva swallowing
If the above were possible, they were first given 5 ml of distilled water and assessed for the following:
Voice change
Cough during swallowing
Throat clearing
Choking
If all the above steps were successful, they were tried on semisolid diet (thick juice/mashed overcooked rice) and re-assessed for:
Cough during swallow
Drooling
Voice change
Throat clearing
If cleared, the next step was to try solids like dry bread. Once patient was able to swallow dry bread without any signs of aspiration, decision to remove NGT was taken. At this time, the study patients underwent FEES, after taking due consent.[5]
Next, the patient was shifted to the ENT OPD for the procedure. This was mainly to facilitate video recording of the findings.
Procedure
The procedure was done by a single ENT surgeon trained in FEES. Karl Storz flexible adult nasopharyngo-laryngoscope (outer diameter 4.1 mm) was used with an Olympus camera and Pinnacle recording device.
The preferred patient position for FEES is sitting. However, in most stroke cases, this was not possible. Instead, a semi-upright position on the bed or trolley was adopted. The first part of evaluation assessed the anatomic details of all areas of nasopharynx, oropharynx, hypopharynx, and larynx. The latter included observation of mobility of the vocal cords and laryngeal sensation and reflex. Secretions management, as evidenced by pooling of saliva, and effect of dry swallow was noted.
Next, food bolus, in the form of coloured ice cream was given. The salient findings noted were residue and penetration and/or aspiration into the larynx.
Where indicated, the effect of swallowing therapy manoeuvres was also checked. Depending on the findings at FEES, the decision to remove or retain the NGT was taken. After this, the patients were followed up for 1 month. At this time, they had to fill a qualitative questionnaire:
Was the patient able to swallow normally after RT removal?
Did the patient have cough or choking while swallowing/drinking water at any time?
Did he/she need hospitalization or antibiotic intake for chest infection?
Results and Observations
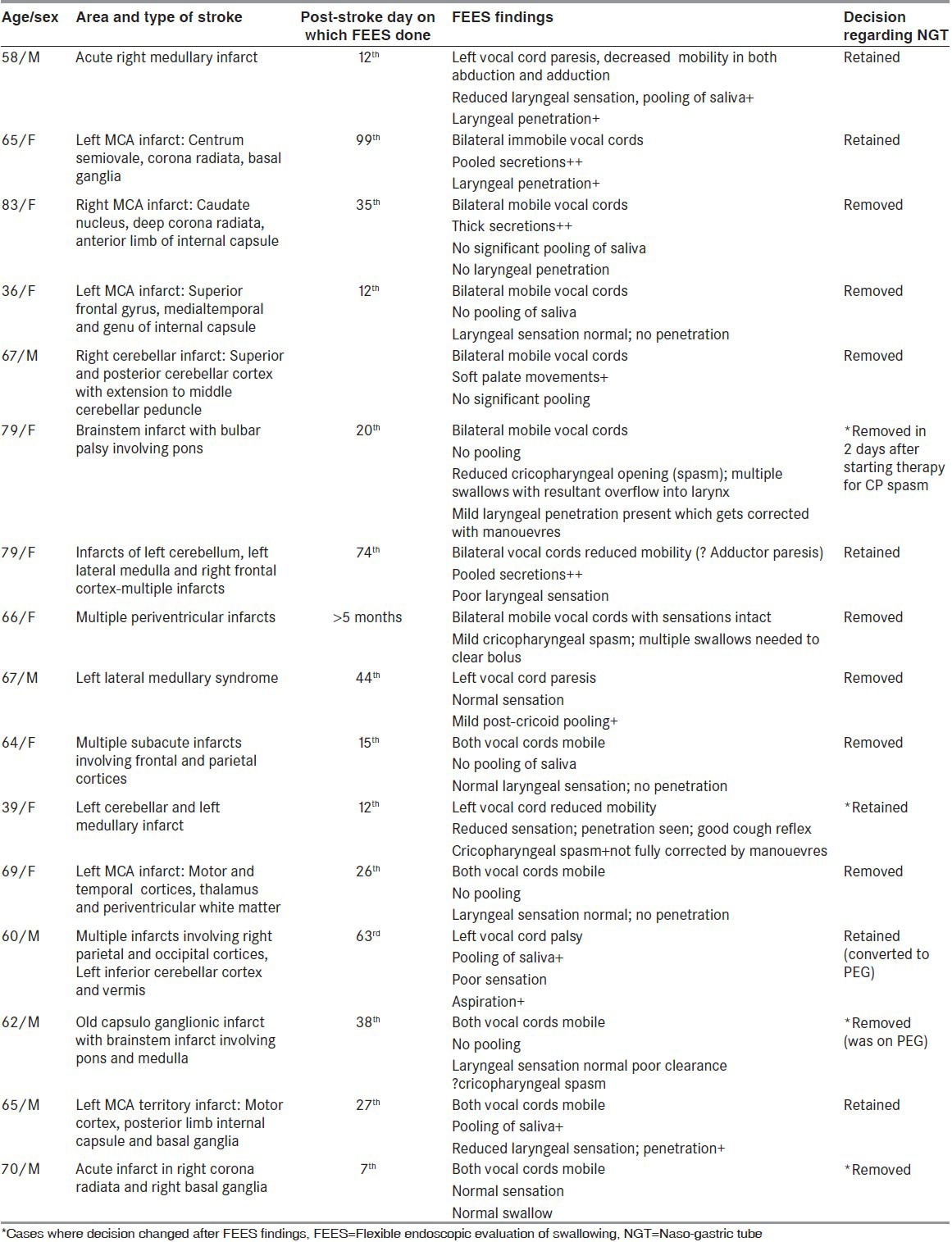
Relevant details, including FEES findings, are tabulated. [Table 1]
Table 1.
Details of patients, stroke areas and FEES findings
Total number of patients: 16
Mean age: 64.31 years (36-83 years)
Gender distribution: Male female ratio of 1:1.2.
Area/Territory of stroke:
Predominantly anterior circulation (cortical and subcortical): 8
Predominantly posterior circulation: 8
Mean duration of NGT removal from the day of insertion: 29.5 days.
In anterior circulation territory: 27.5 days
In posterior circulation territory: 31.5 days
In multi-infarcts: 36 days
In 6/16 (37.5%) patients, the decision taken after bedside evaluation had to be reversed after unfavourable findings on FEES examination. Hence, the NGTs were retained in them.
In four patients, the FEES procedure was significantly helpful in taking decisions regarding NGT removal. These were as described below:
Case no. 6: The patient had only an occasional cough on swallowing liquids. Clinical decision was taken to remove NGT, but FEES revealed only mild cricopharyngeal spasm due to backflow. This was corrected by additional swallow exercises and the NGT was removed after 2 days.
Case no. 11: A good cough reflex encouraged the thought of possible NGT removal. However, FEES showed significant cricopharyngeal spasm and laryngeal penetration on swallowing. Hence, the decision to remove NGT was reversed.
Case no. 14: The patient was on PEG feeding. Clinically we had a doubt regarding its removal as he had infrequent cough on swallowing. However, the findings at FEES cleared the doubt and the PEG tube was removed.
Case no. 16: Although initiated on semi-solid diet, the patient accidentally removed the NGT. Hence, we were in a dilemma whether to reintroduce it. This was resolved thanks to FEES, which showed the swallowing to be normal.
Discussion
The incidence of dysphagia after stroke can vary. Different studies have reported this to be anywhere between 19% and 81%.[6] This wide variation reflects the difference in the way of assessment of dysphagia after stroke. Studies based on definitive tools like FEES of VFSS could potentially pick a higher incidence of dysphagia.
Silent aspiration and subsequent pneumonia are dreaded complications after stroke. This can lead to significant mortality and morbidity. Mortality alone for dysphagic stroke patients stands between 27% and 37%.[7]
Majority of post stroke patients are able to resume normal swallowing within a month of the ictus. However, around 10% will require additional evaluation tools like FEES or VFS as doing only bedside clinical examination can miss swallowing dysfunction.
In our study, we have tried to highlight the usefulness of a combined approach, involving the neurologist and the otolaryngologist, employing bedside evaluation and FEES, respectively, in aiding decision-making regarding removal of NGT.
Incidence of dysphagia tends to be lower after hemispheric as compared to brainstem stroke. Statistical analyses have revealed a significant association between poor outcome and diseases involving medulla.[8] In our study also, we noted this trend. The mean time to NGT removal in posterior circulation territory strokes was 31.5 days, as compared to 27.5 days in anterior circulation strokes.
In our study, the four patients with multi-infarct stroke fared the worst.
The location of stroke in the brain can predict the outcome of dysphagia to some extent. Some generalizations in case of single territory strokes have been described in Jeri Logemann's book.[9] He mentions that medullary and pontine strokes tend to have motor deficits; mainly pharyngeal weakness, adductor paresis and occasional cricopharyngeal spasm. Subcortical strokes result in mild oral and pharyngeal delays as well as mild aspiration. Cortical stroke effects depend on the side of involvement with left hemispheric strokes resulting in significant oral and pharyngeal apraxia and right hemispheric ones resulting in features similar to subcortical stroke. In our case series some of these patterns were evident, as detailed later in the discussion.
FEES was developed and popularized by Susan Langmore et al.[10,11] It has proved to be a significant tool in the assessment of the hypopharyngeal and laryngeal stages of the swallow process. Numerous studies have highlighted its utility in this regard.[12,13] The other modality is VFSS. This is a radiological investigation which looks at all the stages of the swallow process, and has been termed as the ‘gold standard’. However, it has the obvious drawback of radiation exposure. In most centres, it also involves shifting the patient to a radiological department. Whether this latter investigation is needed in every stroke patient with a swallowing issue is a moot point. There have been studies comparing FEES with VFSS.[14,15] One study has favoured FEES.[16]
Most stroke patients recover their swallowing faculty in a month. In the remaining few, the timing of removal of the NGT can be a challenge, especially keeping in mind the threat of aspiration pneumonia. One study has reported a sevenfold risk of the latter.[17] These are the cases where the neurophysician and the swallow therapist need to base their decision on the findings of additional investigations. Many studies have concluded the same.[18,19,20] However, one study has concluded that oxygen desaturation test combined with the 50-ml water swallow test is sufficient.[21] Since the focus is on the larynx and whether there is aspiration, FEES becomes an excellent procedure of choice as it allows direct visualization of these structures without undue risk of radiation.
In the present study, about 10% of the total stroke patients were taken up for FEES.
An ENT surgeon with special interest in swallowing disorders has done all the FEES procedures in the study. From the ENT point of view, it would be ideal to do FEES at the earliest. This would also help in assessing the changes in the swallowing mechanism. However, one of the requirements of a complete FEES procedure mandates the patient to be in good cognitive status. This would not be the case in most early stroke patients. Onset of dysphagia in a stroke patient would be coincident with the onset of stroke. And, at that point in time, it would not be feasible to do FEES. At the most, a flexible laryngoscopy could be attempted.
In all the cases, FEES was sufficient to clear the doubt about feasibility of NGT removal and initiation of oral feeds. None of our patients had any significant complications during or after the procedure. Studies have reported the safety of FEES in post stroke patients.[22,23]
In our case series, there were four cases where we had to reverse our original decision to remove NGT after the FEES findings of the ENT surgeon. The finding which discouraged NGT removal varied from decreased laryngeal sensation, pooling of secretions, immobile vocal cords, cricopharyngeal spasm and multiple swallow attempts which were directly visualized via the flexible endoscope. In the rest, FEES findings correlated with the clinical decision.
Overall, we have noted much better recovery of all swallowing issues in anterior circulation as compared to posterior circulation stroke. Specifically, in this small series, 4/5 (80%) MCA territory (anterior) strokes had near normal swallow within a month's time. One cortical stroke recovered as early as the 15th day. One cerebellar stroke had normal swallow by the 40th day. It has been suggested that the latter cases tend to have cricopharyngeal spasm. All posterior area stroke cases have shown much greater delay in recovery of swallowing. Medullary infarcts are the worst affected; in our series 4/5 (80%) had residual laryngeal motor and sensory deficits on FEES. Two cases of bulbar palsy and one pontine infarct showed cricopharyngeal spasm as the only finding. The latter has been reported to be a significant issue in lateral medullary strokes (Wallenberg's syndrome). This could be an area of research in the future.
None of the patients in whom NGT was successfully removed had any symptoms of aspiration on telephonic follow up after a month.
Conclusion
The management of dysphagia, including prevention of aspiration pneumonia, is one of the key issues in stroke patients. Clinical bedside evaluation along with swallow exercises initiated by a trained swallow therapist are sufficient to successfully remove NGT in a majority of cases. However, in a few patients, these may not be enough. An additional modality becomes necessary to aid in the decision. In such cases, a combination of bedside evaluation and FEES is the best way to prevent silent aspiration. This procedure can be done bedside. In trained hands, it is easy, safe and reliable. The other modality is VFSS, which involves radiation exposure. Both FEES and VFSS have similar sensitivity to detect laryngeal penetration and aspiration. Hence, the former is sufficient in stroke cases.
Our study is a prospective case series involving a small number of patients, in whom the above combination was tried. In a search of literature, we did not come across any such study from India. We present this to emphasize an important concept in the treatment of poststroke dysphagia, whereby a team approach involving the neurophyscian, swallowing pathologist, and ENT surgeon is optimal in the management.
Acknowledgment
Nisha B, Physician Assistant, Department of Neurology.
Footnotes
Source of Support: Nil
Conflict of Interest: Nil
References
- 1.Daniels SK, Ballo LA, Mahoney MC, Foundas AL. Clinical predictors of dysphagia and aspiration risk: Outcome measures in acute stroke patients. Arch Phys Med Rehabil. 2000;81:1030–3. doi: 10.1053/apmr.2000.6301. [DOI] [PubMed] [Google Scholar]
- 2.Ramsey DJ, Smithard DG, Kalra L. Early assessments of dysphagia and aspiration risk in stroke patients. Stroke. 2003;34:1252–7. doi: 10.1161/01.STR.0000066309.06490.B8. [DOI] [PubMed] [Google Scholar]
- 3.Katzan IL, Cebul RD, Husak SH, Dawson NV, Baker DW. The effect of pneumonia on mortality among patients hospitalized for acute stroke. Neurology. 2003;60:620–5. doi: 10.1212/01.wnl.0000046586.38284.60. [DOI] [PubMed] [Google Scholar]
- 4.Martino R, Foley N, Bhogal S, Diamant N, Speechley M, Teasell R. Dysphagia after stroke: Incidence, diagnosis and pulmonary complications. Stroke. 2005;36:2756–63. doi: 10.1161/01.STR.0000190056.76543.eb. [DOI] [PubMed] [Google Scholar]
- 5.Langmore SE. Endoscopic evaluation of oral and pharyngeal phases of swallowing. GI Motility Online. 2006 nature.com. [Google Scholar]
- 6.Barer DH. The natural history and functional consequences of dysphagia after hemispheric srotke. J Neurol Neurosurg Psychiatry. 1989;52:236–41. doi: 10.1136/jnnp.52.2.236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Smithard DG, O’Neill PA, Parks C, Morris J. Complications and outcome after acute stroke: Does dysphagia matter? Stroke. 1996;27:1200–4. doi: 10.1161/01.str.27.7.1200. [DOI] [PubMed] [Google Scholar]
- 8.Meng NH, Wang TG, Lien IN. Dysphagia in patients with brainstem stroke: incidence and outcome. Am J Phys Med Rehabil. 2000;79:170–5. doi: 10.1097/00002060-200003000-00010. [DOI] [PubMed] [Google Scholar]
- 9.Logemann JA. Swallowing disorders caused by neurologic lesions from which some recovery can be anticipated. In: Berman D, editor. Evaluation and treatment of swallowing disorders. 2nd ed. Texas: Pro.ed; 1998. pp. 308–11. [Google Scholar]
- 10.Langmore SE, Logemann JA. After the clinical bedside swallowing examination: What next? Am J Speech Lang Pathol. 1991;1:13–20. [Google Scholar]
- 11.Langmore SE, Kenneth SMA, Olsen N. Fiberoptic endoscopic examination of swallowing safety: A new procedure. Dysphagia. 1988;2:216–9. doi: 10.1007/BF02414429. [DOI] [PubMed] [Google Scholar]
- 12.Dziewas R, Warnecke T, Olenberg S, Teismann I, Zimmermann J, Kramer C, et al. Towards a basic endoscopic assessment of swallowing in acute stroke – development and evaluation of a simple dysphagia score. Cerebrovasc Dis. 2008;26:41–7. doi: 10.1159/000135652. [DOI] [PubMed] [Google Scholar]
- 13.Warnecke T, Ritter MA, Kroger B, Oelenberg S, Teismann I, Heuschmann PU, et al. Fiberoptic endoscopic dysphagia severity scale predicts outcome after acute stroke. Cerebrovasc Dis. 2009;28:283–9. doi: 10.1159/000228711. [DOI] [PubMed] [Google Scholar]
- 14.Kelly AM, Leslie P, Beale T, Payten C, Drinnan MJ. Fibreoptic endoscopic evaluation of swallowing and videofluoroscopy: Does examination type influence perception of pharyngeal residue severity? Clin Otolaryngol. 2006;31:425–32. doi: 10.1111/j.1749-4486.2006.01292.x. [DOI] [PubMed] [Google Scholar]
- 15.Kelly AM, Drinnan MJ, Leslie P. Assessing penetration and aspiration: How do videofluoroscopy and fiberoptic endoscopic evaluation of swallowing compare? Laryngoscope. 2007;117:1723–7. doi: 10.1097/MLG.0b013e318123ee6a. [DOI] [PubMed] [Google Scholar]
- 16.Aviv JE. Prospective, randomized outcome study of endoscopy versus modified barium swallow in patients with dysphagia. Laryngoscope. 2000;110:563–74. doi: 10.1097/00005537-200004000-00008. [DOI] [PubMed] [Google Scholar]
- 17.Singh S, Hamdy S. Dysphagia in stroke patients. Postgrad Med J. 2006;82:383–91. doi: 10.1136/pgmj.2005.043281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hinchey JA, Shephard T, Furie K, Smith D, Wang D, Tonn S. Formal dysphagia screening protocols prevent pneumonia. Stroke. 2005;36:1972–6. doi: 10.1161/01.STR.0000177529.86868.8d. [DOI] [PubMed] [Google Scholar]
- 19.Leder SB, Espinosa JF. Aspiration risk after acute stroke: Comparison of clinical examination and fiberoptic endoscopic evaluation of swallowing. Dysphagia. 2002;17:214–8. doi: 10.1007/s00455-002-0054-7. [DOI] [PubMed] [Google Scholar]
- 20.Daniels SK, Anderson JA, Willson PC. Valid items for screening dysphagia risk in patients with stroke: A systematic review. Stroke. 2012;43:892–7. doi: 10.1161/STROKEAHA.111.640946. [DOI] [PubMed] [Google Scholar]
- 21.Lim SH, Lieu PK, Phua SY, Seshadri R, Venketasubramanian N, Lee SH, et al. Accuracy of bedside clinical methods compared with FEES in determining the risk of aspiration in acute stroke patients. Dysphagia. 2001;16:1–6. doi: 10.1007/s004550000038. [DOI] [PubMed] [Google Scholar]
- 22.Warnecke T, Teismann I, Oelenberg S, Hamacher C, Ringelstein EB, Schabitz WR, et al. The safety of fiberoptic endoscopic evaluation of swallowing in acute stroke patients. Stroke. 2009;40:482–6. doi: 10.1161/STROKEAHA.108.520775. [DOI] [PubMed] [Google Scholar]
- 23.Aviv JE, Kaplan ST, Langmore SE. The safety of endoscopic swallowing evaluations. In: Seils A, editor. Endoscopic evaluation and treatment of swallowing disorders. NY: Thieme; 2001. pp. 235–42. [Google Scholar]


