Abstract
Objectives
The aim of this study was to quantify the agreement among individual National Dental Practice-Based Research Network dentists’ self-reported treatment decisions for primary occlusal caries, primary proximal caries, and existing restorations.
Methods
Five hypothetical clinical scenarios were presented: primary occlusal caries; primary proximal caries; and whether three existing restorations should be repaired or replaced. We quantified the probability that dentists who recommended later restorative intervention for primary caries were the same ones who recommended that existing restorations be repaired instead of replaced.
Results
Dentists who recommended later restorative treatment of primary occlusal caries and proximal caries at a more-advanced stage were significantly more likely to recommend repair instead of replacement. Agreement among dentists on a threshold stage for the treatment of primary caries ranged from 40 to 68%, while that for repair or replacement of existing restorations was 36 to 43%.
Conclusions
Dentists who recommended repair rather than replacement of existing restorations were significantly more likely to recommend later treatment of primary caries. Conversely, dentists who recommended treatment of primary caries at an earlier stage were significantly more likely to recommend replacement of the entire restoration. Between-dentist agreement for primary caries treatment was better than between-dentist agreement for repair or replacement of existing restorations.
Clinical implications
These findings suggest consistency in how individual dentists approach the treatment of primary caries and existing restorations. However, substantial variation was found between dentists in their treatment decisions about the same teeth.
Keywords: Primary caries, Restoration repair/replacement, Decision-making, Health services research
1. Introduction
Diagnoses and treatment decisions for primary and secondary caries is an everyday activity for general dentists.1 Approximately one-half of these decisions are for the treatment of primary caries and the other half are for the repair or replacement of existing restorations.2–6 Restorative treatment decisions are made as dentists concentrate their attention primarily on the presence of caries and secondarily on the need to repair or replace an existing restoration that either presents secondary caries or fracture.6,7 The principal means employed to diagnose occlusal caries are visual and tactile, and for proximal caries it is bitewing radiography.8–10
Studies of current clinical practice place the threshold for restorative intervention at the penetration of caries through the enamel and into the dentine.11–16 The accuracy of these decisions using the visual examination method on primary dentinal occlusal caries lesions in permanent posterior teeth is reported in the range 0.12–0.95 for sensitivity (accuracy for detecting caries when it is truly present), and 0.41–1.00 for specificity (accuracy for identifying teeth without caries). The accuracy for detection of dentinal proximal caries using radiographs is reported in the range 0.16–0.63 for sensitivity and 0.92–0.99 for specificity.17 Therefore, there is a wide variation for both sensitivity and specificity when dentists diagnose occlusal and proximal caries.
The goal of the treatment planning process is to maximize accuracy using all available information and adjusting the threshold at which restorative treatment is planned for a specific patient.18,19 This information may include the patient’s caries risk assessment, age, compliance with home care instructions, the clinical judgement of the dentist, patient preferences, and attendance history for dental visits. The US Department of Health and Human Services20 reports that approximately 60% of the US adult population visited a dentist in the year 2009. For the 40% who did not visit a dentist and some of the 60% who did, their treatment patterns may be more problem-focused and episodic. In light of these many considerations it is not surprising that agreement between practitioners regarding treatment decisions has been reported as moderate or fair.2,13,21
Furthermore, there are studies showing that lack of agreement is an issue in the treatment planning of both primary and secondary caries.21–23 Studies have demonstrated that treatment decisions on the same teeth with the same amount of caries will vary between dentists. This applies to either the same dentist examining the teeth at different times or two different dentists examining the teeth at nearly the same time.9,18,24–27
Dentists’ restorative treatment thresholds for primary and secondary caries have been reported.11,12,14,15,22,28–32 Using hypothetical clinical scenarios in questionnaire format, The National Dental Practice-Based Research Network has published findings concerning dentists’ treatment recommendations about when to place restorations to treat caries based upon five distinct cases: (1) photographs of progressive stages of primary occlusal caries in a molar tooth15; (2) radiographs of five progressive stages of primary proximal caries in a premolar tooth14; and (3) photographs of three teeth with existing restorations of questionable integrity.30 However, no study has presented findings regarding whether there are significant within-dentist relationships between treatment planning recommendations and the restorative decisions in these cases. To the best of our knowledge, this is the first report in the literature regarding within-dentist treatment planning relationships across primary occlusal caries, primary proximal caries, and secondary caries. The aims of the present investigation are to describe and quantify restorative thresholds and to estimate the relationship between the treatment thresholds for primary occlusal caries, primary proximal caries and the treatment of existing restorations.
2. Materials and methods
2.1. Network recruitment process
Practitioner–investigators were recruited into the network through continuing education courses and mass mailings to licensed dentists from the participating regions. The network is composed of dentists in the United States, but at the time of the study mainly concentrated in four regions: Alabama/ Mississippi; Florida/Georgia; dentists in Minnesota, either employed by HealthPartners in Bloomington, Minnesota or in private practice; and Permanente Dental Associates, in cooperation with Kaiser Permanente’s Center for Health Research in Portland, Oregon.33 Information regarding the dentists’ demographics and practice characteristics had been gathered through the enrollment questionnaire. Analyses of the characteristics of network dentists and their practice characteristics suggest that network dentists have much in common with dentists at large34 while at the same time offering substantial diversity within the network with regard to these characteristics.35
2.2. Study design and data collection process
The present study population consisted of dentists working in outpatient dental practices who have completed the network’s Enrollment Questionnaire. The study design was cross-sectional, consisting of a single administration of a questionnaire (“Assessment of Caries Diagnosis and Caries Treatment”) to all network dentist practitioner-investigators who indicated on their enrollment questionnaire that they perform at least some restorative dentistry in their practices. A pilot study documented comprehension and item test–retest reliability for a subset of the dentists.1
Practitioner–investigators were asked to complete the questionnaire by hand and return it to the assigned regional coordinator in a preaddressed envelope. Practitioners were remunerated after they had returned a completed questionnaire and had responded to possible queries from the regional coordinator for clarity of the responses. 901 questionnaires were mailed. 565 (63%) were returned and analysed in the present investigation. The respective institutional review boards of all participating regions approved the study.
We excluded the 57 dentists from the network’s Scandinavian region for this analysis because of certain differences in practice patterns associated in these countries as compared to the US.36 For the purpose of completeness, the Scandinavian results are publicly available at http://www.dpbrn.org/users/publications/Supplement.aspx.
2.3. Main questionnaire content
Three distinct clinical situations from the questionnaire were examined in the present study: primary occlusal caries, primary proximal caries, and treatment of existing restorations. The questionnaire (“Assessment of Caries Diagnosis and Caries Treatment”) with scenarios, photographs, and questions is publicly available at http://www.dpbrn.org/uploadeddocs/Study%201%20questionnaire%20FINAL%20after%20pre-testing%20021306.pdf.
2.4. Primary occlusal caries scenario
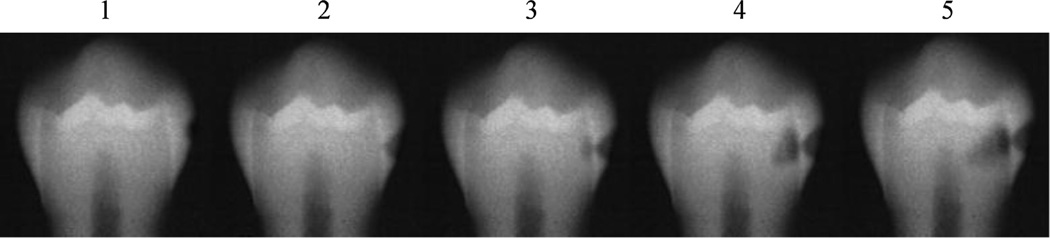
For occlusal caries, the scenario consisted of a description of the patient, treatment options, the patient’s caries risk, and a clinical photograph of the occlusal surface of an unrestored mandibular molar with five progressive stages of caries (Fig. 1).
Fig. 1. Occlusal caries.
Reprinted with permission of the Norwegian Dental Journal.48
The questionnaire requested that the practitioner mark the treatment decision(s) for each photograph under two caries risk scenarios, one that was defined as occlusal low-risk (OLR) and another as occlusal high-risk (OHR). The participants indicated their selection of treatment(s) from among 13 options (a–m) for each of the five stages presented in the scenario. The responses were classified for the analysis into two categories: no operative restorative treatment (options a–j) or operative restorative treatment (options k–m). The lowest-numbered stage (1–5) with a surgical restorative treatment (k–m) was taken to be the surgical restorative threshold.
2.5. Primary proximal caries scenario
For proximal caries, practitioners were asked to indicate from five radiographic stages of progressive proximal caries in a mandibular premolar at which stage they would place a restoration (Fig. 2). The restorative threshold (1–5), i.e., shallowest depth (radiograph) at which the dentist would place a restoration, was requested under both proximal low-risk (PLR) and proximal high-risk (PHR) scenarios.
Fig. 2. Proximal caries.
Reprinted with permission of the Norwegian Dental Journal.48
2.6. Existing restorations scenarios
For existing restorations there were three scenarios that consisted of treatment options, a description of the patient including caries risk, and photographs of the restorations (Figs. 3–5). The practitioner–investigators were asked what type of treatment(s) they deemed appropriate. The nine treatment options covered the spectrum from no treatment to replacement of the entire restoration. The options “a–i” also included different preventive options. The treatment options were classified into three categories: (1) no operative restorative treatment (options a–e and g), (2) operative restorative repair treatment (options f and h), and (3) operative restorative replacement treatment (option i).
Fig. 3. Maxillary incisor existing restoration.
Reprinted with permission of Quintessence Publishing Co Inc, Chicago.49
Fig. 5. Mandibular molar existing restoration.
Courtesy of Dr. Ivar Mjör.
2.7. Statistical methods
Means and standard deviations were calculated for continuous variables, and counts and percentages for categorical variables. Paired percentage responses were compared using McNemar’s test. Spearman’s rank correlation coefficient was used to evaluate associations between ordinal variables. Analysis of variance (ANOVA) was used to compare mean scale scores that included a single observation per practitioner–investigator, and mixed-model ANOVA was used for comparisons based on multiple observations per practitioner–investigator, in order to account for correlations among responses from the same dentist. Analysis of residuals confirmed approximate normality prior to use of normal-theory statistical techniques. Analyses of depths of intervention were conducted (1) separately by number of survey scenario responses for which repair, rather than replacement, was indicated (0, 1, 2 or 3), (2) separately for each of the scenarios presented in the survey, and (3) across all scenarios and numbers of responses. SAS statistical software Release 9.2 (SAS, Cary, NC) was used. All statistical tests were conducted using the 95% confidence level.
3. Results
The numbers of practitioners who would recommend operative restorative intervention at each stage for the primary occlusal and primary proximal caries scenarios are shown in Table 1. Each table cell reports the number of practitioner-investigators who chose the particular threshold stage (1–5). The most frequent choices for restoration by scenario and risk were: OLR 4 (48%), OHR 3 (40%), PLR 3 (54%), and PHR 2 (68%). For both the low-risk and high-risk scenarios a significant correlation was found between the occlusal and proximal thresholds for restorative intervention, Spearman’s rho = 0.26; p < 0.0001, Spearman’s rho = 0.25; p < 0.0001, respectively.
Table 1.
Numbers of practitioner-investigators recommending treatment at each occlusal and proximal primary restorative threshold stage for the low- and high-risk scenarios.
| Threshold stage | OLR Occlusal low-risk |
OHR Occlusal high-risk |
PLR Proximal low-risk |
PHR Proximal high-risk |
|---|---|---|---|---|
| 1 | 6 (1%) | 18 (4%) | 9 (2%) | 50 (10%) |
| 2 | 45 (9%) | 101 (21%) | 200 (42%) | 327 (68%) |
| 3 | 164 (34%) | 191 (40%) | 257 (54%) | 102 (21%) |
| 4 | 229 (48%) | 159 (33%) | 12 (3%) | 1 (0%) |
| 5 | 35 (7%) | 12 (2%) | 1 (0%) | 1 (0%) |
Percentages in a column may not equal 100 due to rounding.
The numbers of dentists recommending repair or replacement of the existing restorations are reported in Table 2. A practitioner could respond replace/repair/neither for each of the 3 existing restorations. The first restoration was most frequently chosen for repair (216 dentists, 43%) and replacement (180 dentists, 36%). There were a total of 177 dentists (35%) who chose not to repair any of the three restorations and 114 dentists (23%) who chose not to replace any.
Table 2.
Numbers of practitioner-investigators recommending repairs or replacements of the three existing restorations.
| Number recommended | Repairs | Replacements |
|---|---|---|
| 0 | 177 (35%) | 114 (23%) |
| 1 | 216 (43%) | 180 (36%) |
| 2 | 97 (19%) | 146 (29%) |
| 3 | 16 (3%) | 66 (13%) |
Percentages in a column may not equal 100 due to rounding.
The number of responses reported in Tables 1 and 2 reflect the number of practitioners answering each of the survey questions. Not all of them provided complete data.
Table 3 presents the mean primary caries restorative threshold stage by the number of restorations recommended for repair. Across rows, comparisons can be made among the four combinations with regard to the number of restorations that the practitioners recommended for repair (0–3). Going down the columns allows an appraisal of the changes in primary caries restorative threshold stage that occur as the number of restorations recommended for repair increases. Mean responses for all of the questions with zero repairs were significantly different, as compared to the two-and three-repair answers.
Table 3.
Numbers of repairs recommended and mean primary restorative threshold stage for occlusal and proximal caries.
| Number of repairs (options ‘f or ‘h’) recommended |
OLR Occlusal low-risk* |
OHR Occlusal high-risk* |
PLR Proximal low-risk* |
PHR Proximal high-risk* |
|---|---|---|---|---|
| 0† | 3.30a ± 0.90 | 2.92c ± 0.92 | 2.38e ± 0.60 | 1.97g ± 0.53 |
| l† | 3.55b ± 0.72 | 3.09cd ± 0.87 | 2.63f ± 0.56 | 2.16h ± 0.60 |
| 2† | 3.77b ± 0.77 | 3.32d ± 0.82 | 2.76f ± 0.50 | 2.23h ± 0.51 |
| 3† | 3.87bi ± 0.74 | 3.67di ± 0.72 | 2.93fj ± 0.62 | 2.43hj ± 0.51 |
Mean threshold ± sd.
Means in a column with the same superscript are not significantly different, p < 0.05.
Means in a row with the same superscript are not significantly different, p < 0.05.
The mean restorative threshold stage across each row decreased in the order: OLR, OHR, PLR, PHR, from left to right. Comparisons of the means across each of the four rows revealed significant differences among all of the four groups except for row three where the differences were only between the occlusal and proximal groups.
Table 4 shows primary caries restoration threshold stage by the number of restorations recommended for replacement, instead of repair (as was shown in Table 3). Mean responses for all of the questions with zero replacements were significantly different from those of the two replacements and three replacements answers. Comparisons across each of the four rows (0–3) found the mean depths for groups OLR, OHR, PLR, and PHR to be significantly different in rows 0–2.
Table 4.
Numbers of replacements recommended and mean primary restorative threshold stage for occlusal andproximal caries.
| Number of replacements (option ‘i’) recommended |
OLR | OHR | PLR | PHR |
|---|---|---|---|---|
| Occlusal low-risk* | Occlusal high-risk* | Proximal low-risk* | Proximal high-risk* | |
| 0† | 3.80a ± 0.81 | 3.41d ± 0.87 | 2.80f ± 0.56 | 2.33h ± 0.55 |
| 1† | 3.57ac ± 0.75 | 3.11e ± 0.86 | 2.69f ± 0.57 | 2.18h ± 0.61 |
| 2† | 3.34b ± 0.80 | 2.91e ± 0.84 | 2.40g ± 0.56 | 1.96i ± 0.52 |
| 3† | 3.27bc ± 0.89 | 2.91e ± 0.96 | 2.26g ± 0.48 | 1.94gi ± 0.44 |
Mean threshold ± sd.
Means in a column with the same superscript are not significantly different, p < 0.05.
Means in a row with the same superscript are not significantly different, p < 0.05.
Looking across the rows in Tables 3 and 4, occlusal lesions were treated with restorations at significantly later stages (i.e., at greater lesion depth) than proximal lesions for all numbers of repair and replacement in both caries risk scenarios.
4. Discussion
The practitioners indicated that they would surgically restore primary proximal caries detected on radiographs at an earlier stage than primary occlusal caries detected on visual examination, based on the 5 stages shown in the scenarios. The differences in mean threshold stage between occlusal and proximal were 0.93 for the low-risk patient and 0.97 for the high-risk patient. It is possible that the lower proximal restorative thresholds can be explained by the greater clinical extent of lesions as compared to what is exhibited on radiographs37–39 and the less-frequent radiographic bitewing exposures as compared to visual observations.40,41
The occlusal and proximal scenarios for both the low- and high-risk patients stated that the patient had been attending the dental practice every 2 years for the past 6 years. The mean threshold differences between the low- and high-risk patients were 0.42 for occlusal lesions and 0.46 for proximal lesions. This is less than one-half of the differences found between the occlusal and proximal detection thresholds. This means that for this regular two-year dental visit scenario, the detection method or difference in surface type (occlusal vs. proximal) was found to be a greater factor in the choice of surgical restorative threshold than the caries risk of the patient.
The statistically significant correlations between when to restore primary occlusal caries based upon visual inspection and primary proximal caries based upon radiographs for both the low- and high-risk scenarios indicate that practitioners who recommend restorative treatment of less-advanced occlusal caries were also more likely to recommend restorative treatment of less-advanced proximal caries, and those surgically restoring advanced occlusal caries were also surgically restoring advanced proximal caries. This finding is consistent with reports by Mejáre et al.11 and Espelid et al.12 concerning the relationship between occlusal and proximal treatment thresholds.
Of the practitioners who choose to surgically restore occlusal caries at stage three, 99% (162/164) said that they would surgically restore proximal caries before they pass through the outer 1/3 of the dentine for the low-risk scenario. For the high-risk scenario it also was 99% (190/191). These percentages compare to results from a similar report on Scandinavian dentists who place the treatment threshold for occlusal caries at stage 3. For proximal caries up to the outer 1/ 3 of the dentine, Norwegian dentists surgically restore 85%, Swedish dentists 55%, and Danish dentists 61% of the cases.12
For primary occlusal caries 48% of the practitioners selected the most frequently chosen restorative threshold for OLR. It was 40% for OHR. For proximal caries it was 54% for PLR and 68% for PHR. For secondary caries, 43% of the practitioners selected the most frequently chosen number of repairs while for replacement it was 36%. Thus, in one-half of the primary caries scenarios the best agreement was less than 50% of the practitioners, and in the scenarios for existing restorations less than a simple majority of the practitioners agreed on the number of repairs or replacements. Other authors have reported differences of opinion on the treatment planning of teeth for restorative treatment,22,23 in particular for teeth with existing restorations.21
Inconsistencies in diagnostic and treatment decisions have been reported in other areas of health care. In a retrospective study of women who had mammograms, a 50% chance of experiencing a false positive test was estimated by the authors42 for a woman who has a screening mammogram yearly for 10 years; 20% of these women will undergo biopsies as a result. For every $100 spent on screening, it was estimated that an additional $33 is spent to evaluate the false positive results. This rate of false positives is approximately twice as high as previous estimates.
Agreement concerning when and how to treat initial and secondary caries should start during dental school education, with faculty applying evidence-based caries risk assessment to treatment recommendations. Bervian et al.23 reported a large variation for proximal caries treatment decisions between final-year dental students graduating from private as compared to public schools. A survey of teachers in French dental schools determined that there is a substantial lack of agreement for restorative treatment thresholds for proximal surfaces, opinions on the rate of caries progression, and the need to monitor lesions near the DEJ.13
Even with evidence-based criteria for caries treatment, subjective clinical and radiographic interpretation will be a major component of treatment decisions. Technology may be able to provide more objective information to aid in treatment decisions. Radiographic image analysis, laser, quantitative light fluorescence, and electrical conductance are commercially available aids for the diagnosis of caries. Improvement in diagnostic accuracy may bring with it an increased agreement among practitioners. For low caries risk patients an improvement in agreement could significantly decrease the risk of treatment based upon a false positive diagnosis.43
Through participation in studies, newsletters, and meetings the National Dental PBRN participants receive information that is practice changing.44 Many of the Network participants utilize commercial software for the operation of their offices. A study under consideration would collect data from these systems and could potentially lead to reports on treatment provided that may improve patient care.
Although the five stages of occlusal and proximal caries are not strictly at equivalent lesion depths, Ekstrand et al.45–47 have correlated the visual and histological extent of occlusal caries. Accordingly, the present study classified stages 1 and 2 as caries in the outer and inner enamel and stages 3, 4, and 5 as caries extending into the outer, middle and inner dentine, respectively. The extent of caries lesions on the five-stage radiographic proximal scale is similar to this. The diagnostic material available to the practitioners for proximal caries diagnosis was similar to the radiography employed in clinical practice. While the photographs of the occlusal surfaces presented excellent examples of progressive caries in the occlusal surface of a mandibular molar, the opportunity for probing was absent. This could have affected the results of the present study. However, the contribution of probing to the diagnosis of occlusal caries has been shown to be minimal.9,10
The practitioners who restoratively treated primary occlusal caries at shallower lesion depths tended also to be the ones who treated primary proximal caries at an earlier stage of caries progression. Practitioners with a conservative treatment planning approach indicated that more existing restorations should be repaired instead of replaced and they postponed surgical treatment of both primary occlusal and proximal caries to a more advanced stage. Conversely, those with a more aggressive approach indicated that more restorations should be replaced instead of repaired and they were also more likely to surgically treat both primary occlusal and proximal caries at an earlier stage of caries progression. In contrast to the consistency of an individual practitioner’s treatment planning approach, there was considerable variation between practitioners in their treatment recommendations on the same teeth, especially those with existing restorations.
In conclusion, improved diagnosis and treatment decisions should benefit both low and high caries risk patients. The opportunities exist within the educational system, technology, and professional and network organizations for improved patient treatment and cost savings. When an individual practitioner applied a conservative approach to the treatment of primary caries, a conservative approach to the treatment of secondary caries was also more likely, based on this questionnaire study. An appropriate next step in this line of research would be to confirm these results using actual clinical practice data.
Supplementary Material
Fig. 4. Maxillary cuspid existing restoration.
Reprinted with permission of Quintessence Publishing Co Inc, Berlin.50
Acknowledgments
This investigation was supported by NIH grants U01-DE-16746, U01-DE-16747, and U19-DE-22516. Opinions and assertions contained herein are those of the authors and are not to be construed as necessarily representing the views of the respective organizations or the National Institutes of Health.
Appendix A. Supplementary data
Supplementary data associated with this article can be found, in the online version, at http://dx.doi.org/10.1016/j.jdent.2013.05.014.
REFERENCES
- 1.Gordan W, Riley JL, 3rd, Carvalho RM, Snyder J, Sanderson JL, Anderson M, et al. Methods used by Dental Practice-Based Research Network (DPBRN) dentists to diagnose dental caries. Operative Dentistry. 2011;36:2–11. doi: 10.2341/10-137-CR. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Elderton RJ, Nuttall NM. Variation among dentists in planning treatment. British Dental Journal. 1983;154:201–206. doi: 10.1038/sj.bdj.4805041. [DOI] [PubMed] [Google Scholar]
- 3.Elderton RJ, Davies JA. Restorative dental treatment in the General Dental Service in Scotland. British Dental Journal. 1984;157:196–200. doi: 10.1038/sj.bdj.4805459. [DOI] [PubMed] [Google Scholar]
- 4.Mjör IA, Shen C, Eliasson ST, Richter S. Placement and replacement of restorations in general dental practice in Iceland. Operatiue Dentistry. 2002;27:117–123. [PubMed] [Google Scholar]
- 5.Forss H, Widström E. Reasons for restorative therapy and the longevity of restorations in adults. Acta Odontologica Scandinauica. 2004;62:82–86. doi: 10.1080/00016350310008733. [DOI] [PubMed] [Google Scholar]
- 6.Bernardo M, Luis H, Martin MD, Leroux BG, Rue T, Leitão J, et al. Survival and reasons for failure of amalgam versus composite posterior restorations placed in a randomized clinical trial. Journal of the American Dental Association. 2007;138:775–783. doi: 10.14219/jada.archive.2007.0265. [DOI] [PubMed] [Google Scholar]
- 7.Nascimento MM, Gordan W, Qyist V, Litaker MS, Rindal DB, Williams OD, et al. Reasons for placement of restorations on previously unrestored tooth surfaces by dentists in The Dental Practice-Based Research Network. Journal of the American Dental Association. 2010;141:441–448. doi: 10.14219/jada.archive.2010.0197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kidd EA, Pitts NB. A reappraisal of the value of the bitewing radiograph in the diagnosis of posterior approximal caries. British Dental Journal. 1990;169:195–200. doi: 10.1038/sj.bdj.4807325. [DOI] [PubMed] [Google Scholar]
- 9.Lussi A. Validity of diagnostic and treatment decisions of fissure caries. Caries Research. 1991;25:296–303. doi: 10.1159/000261380. [DOI] [PubMed] [Google Scholar]
- 10.Penning C, van Amerongen JP, Seef RE, ten Cate JM. Validity of probing for fissure caries diagnosis. Caries Research. 1992;26:445–449. doi: 10.1159/000261485. [DOI] [PubMed] [Google Scholar]
- 11.Mejàre I, Sundberg H, Espelid I, Tveit B. Caries assessment and restorative treatment thresholds reported by Swedish dentists. Acta Odontologica Scandinauica. 1999;57:149–154. doi: 10.1080/000163599428887. [DOI] [PubMed] [Google Scholar]
- 12.Espelid I, Tveit AB, Mejàre I, Sundberg H, Hallonsten AL. Restorative treatment decisions on occlusal caries in Scandinavia. Acta Odontologica Scandinauica. 2001;59:21–27. doi: 10.1080/000163501300035724. [DOI] [PubMed] [Google Scholar]
- 13.Tubert-Jeannin S, Doméjean-Orliaguet S, Riordan PJ, Espelid I, Tveit AB. Restorative treatment strategies reported by French university teachers. Journal of Dental Education. 2004;68:1096–1103. [PubMed] [Google Scholar]
- 14.Gordan VV, Garvan CW, Heft MW, Fellows JL, Qyist V, Rindal DB, et al. Restorative treatment thresholds for interproximal primary caries based on radiographic images: findings from The Dental Practice-Based Research Network. General Dentistry. 2009;57:654–663. [PMC free article] [PubMed] [Google Scholar]
- 15.Gordan W, Bader JD, Garvan CW, Richman JS, Qyist V, Fellows JL, et al. Restorative treatment thresholds for occlusal primary caries among dentists in The Dental Practice-Based Research Network. Journal of the American Dental Association. 2010;141:171–184. doi: 10.14219/jada.archive.2010.0136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Vidnes-Kopperud S, Tveit AB, Espelid I. Changes in the treatment concept for approximal caries from 1983 to 2009 in Norway. Caries Research. 2011;45:113–120. doi: 10.1159/000324810. [DOI] [PubMed] [Google Scholar]
- 17.Bader JD, Shugars DA, Bonito AJ. A systematic review of the performance of methods for identifying carious lesions. Journal of Public Health Dentistry. 2002;62:201–213. doi: 10.1111/j.1752-7325.2002.tb03446.x. [DOI] [PubMed] [Google Scholar]
- 18.Kay EJ, Watts A, Paterson RC, Blinkhorn AS. Preliminary investigation into the validity of dentists’ decisions to restore occlusal surfaces of permanent teeth. Community Dentistry and Oral Epidemiology. 1988;16:91–94. doi: 10.1111/j.1600-0528.1988.tb01850.x. [DOI] [PubMed] [Google Scholar]
- 19.Tulloch JF, Antczak-Bouckoms AA, Berkey CS, Douglass CW. Selecting the optimal threshold for the radiographic diagnosis of interproximal caries. Journal of Dental Education. 1988;52:630–636. [PubMed] [Google Scholar]
- 20.Health, United States, 2010. Hyattsville, MD: US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics; 2011. DHHS publication 2011-1232. [Google Scholar]
- 21.Bader JD, Shugars DA. Agreement among dentists’ recommendations for restorative treatment. Journal of Dental Research. 1993;72:891–896. doi: 10.1177/00220345930720051001. [DOI] [PubMed] [Google Scholar]
- 22.Merrett MC, Elderton RJ. An in vitro study of restorative dental treatment decisions and dental caries. British Dental Journal. 1984;157:128–133. doi: 10.1038/sj.bdj.4805448. [DOI] [PubMed] [Google Scholar]
- 23.Bervian J, Tovo MF, Feldens CA, Brusco LC, Rosa FM. Evaluation of final-year dental students concerning therapeutic decision making for proximal caries. Brazilian Oral Research. 2009;23:54–60. doi: 10.1590/s1806-83242009000100010. [DOI] [PubMed] [Google Scholar]
- 24.Rytömaa I, Järvinen V, Järvinen J. Variation in caries recording and restorative treatment plan among university teachers. Community Dentistry and Oral Epidemiology. 1979;7:335–339. doi: 10.1111/j.1600-0528.1979.tb01243.x. [DOI] [PubMed] [Google Scholar]
- 25.Poulsen S, Bille J, Rugg-Gunn AJ. Evaluation of a calibration trial to increase interexaminer reliability of radiographic diagnosis of approximal carious lesions. Community Dentistry and Oral Epidemiology. 1980;8:135–138. doi: 10.1111/j.1600-0528.1980.tb01274.x. [DOI] [PubMed] [Google Scholar]
- 26.Nuttall NM. Capability of a national epidemiological survey to predict general dental service treatment. Community Dentistry and Oral Epidemiology. 1983;11:296–301. doi: 10.1111/j.1600-0528.1983.tb01897.x. [DOI] [PubMed] [Google Scholar]
- 27.Kay EJ, Silkstone B, Worthington HV. Evaluation of computer aided learning in developing clinical decisionmaking skills. British Dental Journal. 2001;190:554–557. doi: 10.1038/sj.bdj.4801033. [DOI] [PubMed] [Google Scholar]
- 28.Nuttall NM, Pitts NB. Restorative treatment thresholds reported to be used by dentists in Scotland. British Dental Journal. 1990;169:119–126. doi: 10.1038/sj.bdj.4807294. [DOI] [PubMed] [Google Scholar]
- 29.Setcos JC, Khosravi R, Wilson NH, Shen C, Yang M, Mjör IA. Repair or replacement of amalgam restorations: decisions at a USA and a UK dental school. Operative Dentistry. 2004;29:392–397. [PubMed] [Google Scholar]
- 30.Gordan W, Garvan CW, Richman JS, Fellows JL, Rindal DB, Qyist V, et al. How dentists diagnose and treat defective restorations: evidence from The Dental Practice-Based Research Network. Operative Dentistry. 2009;34:664–673. doi: 10.2341/08-131-C. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rindal DB, Gordan VV, Fellows JL, Spurlock NL, Bauer MR, Litaker MS, et al. Differences between reported and actual restored caries lesion depths: results from The Dental PBRN. Journal of Dentistry. 2012;40:248–254. doi: 10.1016/j.jdent.2011.12.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Momoi Y, Hayashi M, Fujitani M, Fukushima M, Imazato S, Kubo S, et al. Clinical guidelines for treating caries in adults following a minimal intervention policy—evidence and consensus based report. Journal of Dentistry. 2012;40:95–105. doi: 10.1016/j.jdent.2011.10.011. [DOI] [PubMed] [Google Scholar]
- 33.Gilbert GH, Williams OD, Rindal DB, Pihlstrom DJ, Benjamin PL, Wallace MC, et al. The creation and development of The Dental Practice-Based Research Network. Journal of the American Dental Association. 2008;139:74–81. doi: 10.14219/jada.archive.2008.0024. [DOI] [PubMed] [Google Scholar]
- 34.Makhija SK, Gilbert GH, Rindal DB, Benjamin PL, Richman JS, Pihlstrom DJ, et al. Dentists in practice-based research networks have much in common with dentists at large: evidence from The Dental Practice-Based Research Network. General Dentistry. 2009;57:270–275. [PMC free article] [PubMed] [Google Scholar]
- 35.Makhija SK, Gilbert GH, Rindal DB, Benjamin P, Richman JS, Pihlstrom DJ, et al. Practices participating in a dental PBRN have substantial and advantageous diversity even though as a group they have much in common with dentists at large. [[accessed 25.11.12]];BioMed Central Oral Health. 2009 9:26. doi: 10.1186/1472-6831-9-26. http://www.biomedcentral.com/1472-6831/9/26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Burt BA. Prevention policies in the light of the changed distribution of dental caries. Acta Odontologica Scandinavica. 1998;56:179–186. doi: 10.1080/000163598422956. [DOI] [PubMed] [Google Scholar]
- 37.Kooistra S, Dennison JB, Yaman P, Burt BA, Taylor GW. Radiographic versus clinical extension of Class II carious lesions using an F-speed film. Operative Dentistry. 2005;30:719–726. [PubMed] [Google Scholar]
- 38.Bin-Shuwaish M, Dennison JB, Yaman P, Neiva G. Estimation of clinical axial extension of Class II caries lesions with ultraspeed and digital radiographs: an in-vivo study. Operative Dentistry. 2008;33:613–621. doi: 10.2341/07-167. [DOI] [PubMed] [Google Scholar]
- 39.Nascimento MM, Bader JD, Qyist V, Litaker MS, Williams OD, Rindal DB, et al. Concordance between preoperative and postoperative assessments of primary caries lesion depth: results from The Dental PBRN. Operative Dentistry. 2010;35:389–396. doi: 10.2341/09-363-C. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.The selection of patients for dental radiographic examinations. Chicago, IL: American Dental Association; [Google Scholar]
- 41.Patel S, Bay RC, Glick M. A systematic review of dental recall intervals and incidence of dental caries. Journdl of the Amerkdn Dental Association. 2010;141:527–539. doi: 10.14219/jada.archive.2010.0225. [DOI] [PubMed] [Google Scholar]
- 42.Elmore JG, Barton MB, Moceri VM, Polk S, Arena PJ, Fletcher SW. Ten-year risk of false positive screening mammograms and clinical breast examinations. New England Journdl of Medicine. 1998;338:1089–1096. doi: 10.1056/NEJM199804163381601. [DOI] [PubMed] [Google Scholar]
- 43.Heaven TJ, Firestone AR, Weems RA. The effect of multiple examinations on the diagnosis of approximal caries and the restoration of approximal surfaces. Oral Surgery Oral Medicine Oral Pathology Oral Radiology and Endodontology. 1999;87:386–391. doi: 10.1016/s1079-2104(99)70229-5. [DOI] [PubMed] [Google Scholar]
- 44.Gilbert GH, Richman JS, Gordan VV, Rindal DB, Fellows JL, Benjamin PL, et al. Lessons learned during the conduct of clinical studies in the dental PBRN. Journal of Dental Education. 2011;75:453–465. [PMC free article] [PubMed] [Google Scholar]
- 45.Ekstrand KR, Kuzmina I, Bj0rndal L, Thylstrup A. Relationship between external and histologic features of progressive stages of caries in the occlusal fossa. Cdries Research. 1995;29:243–250. doi: 10.1159/000262076. [DOI] [PubMed] [Google Scholar]
- 46.Ekstrand KR, Ricketts DN, Kidd EA, Qyist V, Schou S. Detection, diagnosing, monitoring and logical treatment of occlusal caries in relation to lesion activity and severity: an in vivo examination with histological validation. Cdries Research. 1998;32:247–254. doi: 10.1159/000016460. [DOI] [PubMed] [Google Scholar]
- 47.Ekstrand KR, Martignon S, Ricketts DJ, Qyist V. Detection and activity assessment of primary coronal caries lesions: a methodologic study. Operative Dentistry. 2007;32:225–235. doi: 10.2341/06-63. [DOI] [PubMed] [Google Scholar]
- 48.Espelid I, Tveit AB, Mejàre I, Nyvad B. Caries: new knowledge or old truths? Norwegian Dental Journal. 1997;107:66–74. [Google Scholar]
- 49.Ericson D, Kidd E, McComb D, Mjör I, Noack MJ. Minimally invasive dentistry—concepts and techniques in cariology. Oral Health & Preventive Dentistry. 2003;1:59–72. [PubMed] [Google Scholar]
- 50.Mjör IA, Toffenetti F. Secondary caries: a literature review with case reports. Quintessence International. 2000;31:165–179. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.