Abstract
Objective
To examine whether dietary self-monitoring is related to weight loss in overweight children and whether perceived social support or dietary self-efficacy affects this relation.
Design
Longitudinal, behavioral intervention study.
Subjects
The study population included 153 children, aged 7–12 years, with daily food records from a 20-week weight loss program in San Diego, California, USA, conducted between 1999 and 2002.
Methods
Self-monitoring was assessed using two methods: a weekly index as a measure of competency (possible range −7 to +35) and recording sufficiency for total compliance (percentage of days).
Results
Significantly greater decreases in percentage overweight were found for children with recording competency at or above the median (mean change: −13.4% vs. −8.6%; p < 0.001) or who were compliant in recording ≥50% of the days (mean change: −13.0% vs. −8.4%; p < 0.001). Using hierarchical linear regression, children who had a higher average weekly monitoring index or recorded sufficiently on more days had significantly greater decreases in percent overweight, after adjusting for age, sex, SES, race/ethnicity and baseline percent overweight (p < 0.001). Perceived social support at baseline and dietary self-efficacy were not related to self-monitoring or change in percent overweight in this sample.
Conclusion
As has been demonstrated with adults and adolescents, self-monitoring in children was associated with greater decreases in percent overweight. However, dietary self-efficacy and perceived social support were not related to how frequently or thoroughly they monitored dietary intake.
Introduction
Between 1999 and 2004, childhood overweight, defined as BMI for age ≥95th percentile increased from 15.1–18.8% for 6–11-year olds, and from 14.8–17.4% for 12–19-year olds in the US (1,2). Approximately 24–44% of overweight preschool children in the US become obese adults (3,4). Overweight children are also at risk of developing conditions such as diabetes, hypertension, and cardiovascular disease (5,6). Epidemic increases in overweight across the US (7) and internationally (8) have focused attention on prevention and treatment.
Self-regulation refers to the processes through which individuals self-direct goal achievement (9,10). It encompasses the internal and external influences that guide achievement or failure. Self-monitoring is a major subfunction of self-regulation, providing self-assessment and evaluative information (9). An individual can determine how far they are from their posited goal and how much progress they have made once change has been initiated. Dietary self-monitoring is a component of many behavioral weight loss programs for children, adolescents, and adults. It is the behavior of journaling foods and beverages consumed each data, either in a paper journal or electronically via a web-based application or hand-held personal digital assistant. In studies evaluating adult weight-regulation, self-monitoring has been demonstrated to be central to success (11–13) and suggest that adults need to competently monitor on at least 50% of the days. Similarly, for overweight adolescents, greater compliance with self-monitoring was associated with greater weight loss (14,15). However, this has not yet been fully evaluated in pre-adolescent children.
Perceived social support has been demonstrated to predict increased physical activity and facilitate dietary changes leading to weight loss among pre-adolescent children (16,17). Self-efficacy has also been suggested as a mediator of changes in fruit and vegetable consumption in children which may impact future weight loss (18).
The current study sought to evaluate the effect of dietary self-monitoring on change in percentage overweight among children participating in a 20-week weight loss intervention. Of particular interest was whether this relationship was affected by perceived social support or dietary self-efficacy at baseline. We hypothesize that children who monitor their diet more consistently will experience greater decreases in percentage overweight during the intervention and that this relation may be moderated by baseline perceived social support or dietary self-efficacy.
Methods
Participants
Participants were 204 parent-child pairs, recruited through media outlets, postings and referrals from pediatrician offices, who gave informed consent to enroll in a pediatric obesity treatment study in San Diego, California, USA, between 1999 and 2002 (19). Children were excluded if any of the following were present: current psychopathology or eating disorder, a medical condition for which a structured weight loss program would be contraindicated, a physical limitation or illness that would interfere with adherence to physical activity recommendations, a weight-affecting medication regimen, or self-reported substance abuse. Children considered for participation were between 7 and 12 years of age, classified as overweight (20–100% overweight based on age and sex), spoke and read English at a 3rd grade level or higher and had at least on overweight or obese parent.
Of the 1,161 families who contacted the clinic about the study, 533 completed the phone screen and 314 of those completed the application. Of the 269 selected for clinical interview, 44 decided not to participate, and 21 were found ineligible, leaving 204 eligible for enrollment. Of those, 153 finished the intervention and provided complete weight and food record data. A participant was considered to have complete data if they had anthropometric measurements at the beginning and the end of the weight loss intervention and completed at least one weekly food record. Among the 51 who dropped out before the end of the intervention or had incomplete data, 49.0% were girls, compared to 69.9% of those who completed treatment. The distribution of boys versus girls was significantly different (p = 0.01) for those who provided complete outcome data versus those who did not. No differences between those with and without complete data were found for baseline percent overweight, age, race/ethnicity, SES, perceived social support for enacting dietary change or dietary self-efficacy (see Table I). We certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during this research. Approval was received from the University of California at San Diego Human Research Protections Program and the San Diego State University Institutional Review Board.
Table 1.
Weight-loss program participant characteristics and comparison to dropouts; San Diego, CA 1999 – 2002
| Participants | Dropouts | p | |||
|---|---|---|---|---|---|
| n | % | n | % | ||
| Sex | |||||
| Boys | 46 | 30.1 | 26 | 51.0 | 0.01 |
| Girls | 107 | 69.9 | 25 | 49.0 | |
| Race/ethnicity | |||||
| Caucasian | 105 | 68.6 | 5 | 49.0 | 0.35 |
| Hispanic | 29 | 18.9 | 13 | 25.4 | |
| African-American | 11 | 7.2 | 7 | 13.7 | |
| Other | 8 | 5.3 | 6 | 11.9 | |
| n | Mean | (SD) | n | Mean | (SD) | p | |
|---|---|---|---|---|---|---|---|
|
|
|||||||
| Age (years) | 153 | 9.86 | 1.31 | 51 | 9.67 | 1.44 | 0.37 |
| Baseline percent overweight | 153 | 64.39 | 18.49 | 51 | 66.16 | 18.80 | 0.56 |
| SES (Hollingshead Index) | 144 | 47.11 | 11.32 | 28 | 43.70 | 12.34 | 0.15 |
| Dietary self-efficacy scale | 151 | 7.00 | 5.86 | 42 | 6.69 | 6.74 | 0.77 |
| Social support survey for dietary behaviors | |||||||
| Encouragement | |||||||
| Family | 150 | 16.22 | 4.69 | 49 | 17.22 | 4.21 | 0.18 |
| Friend | 151 | 7.87 | 3.95 | 49 | 8.35 | 4.00 | 0.46 |
| Discouragement | |||||||
| Family | 149 | 11.07 | 4.08 | 48 | 11.04 | 4.28 | 0.97 |
| Friend | 150 | 11.39 | 4.67 | 48 | 10.35 | 4.39 | 0.18 |
| Recording Compliance * | |||||||
| Total days 5 or more items recorded | 153 | 70.20 | 36.40 | 51 | 21.00 | 23.69 | <0.001 |
| Percentage of days 5 or more items recorded | 153 | 50.14 | 25.99 | 51 | 15.00 | 16.93 | <0.001 |
| Recording Competency * | |||||||
| Average weekly monitoring index | 153 | 13.30 | 10.17 | 51 | 5.23 | 12.75 | <0.001 |
SD: Standard Deviation
Dietary monitoring measured during intervention thus differences were expected since dropouts completed fewer food records
Description of the Weight Loss Intervention
Families received weekly 20-min individualized behavioral skills sessions with a trained counselor (graduate students in psychology and doctoral researchers trained in the study protocol) followed by separate 40-min child and parent groups. The intervention was comprised of three components: (i) dietary modification, (ii) increases in physical activity, and (iii) behavior change skills (such as self-monitoring and stimulus control). Participants were instructed to follow the Traffic Light Diet (20), which categorized foods and beverages by the colors of the traffic light according to the amount of dietary fat and/or sugar per serving. RED foods (>5 g of fat/serving, low in nutrient density and/or high in calories) were limited to 15 or fewer per week. Caloric goals for children were 1100–1300 kcal/day. As part of the intervention, participants were trained to self-monitor their dietary intake.
Assessment measures
Demographics
Race/ethnicity, sex and household demographic characteristics were assessed via parent completion of the Hollingshead Demographics Questionnaire (21). The Hollingshead Four Factor Index socioeconomic score (SES score) was calculated using occupation and education codes for each parent. Occupation was coded according to the category in which the listed occupation fell and ranged from 1 (farm laborers/menial service) to 9 (executives, major professionals). Education was coded as highest level of education completed and ranged from 1 (less than a 7th grade education) to 7 (graduate degree). Individual SES scores were calculated for each parent as follows: [(occupation score* 5) + (education score*3)]. If both parents contributed in the household, then the average of each SES score was taken. If the participating parent was divorced and the other parent did not contribute financially, only the participating parent’s SES score was used. Possible scores range from 8–66.
Racial/ethnic categories available for selection included American Indian/Alaska Native; Asian/Pacific Islander; African-American, not of Hispanic origin; Hispanic; White, not of Hispanic origin; or Other. Due to low numbers in certain categories, race/ethnicity was analyzed as White versus All others.
Food records
Child dietary intake was measured via self-reported 7-day food records. To enhance accuracy, participants were given self-monitoring training to carefully record food intake. Although food records were reviewed during weekly sessions, additions made by counselors were disregarded during coding so that the most accurate representation of recording could be made.
Recording competency
Previous research used a self-monitoring index constructed by Kirschenbaum and colleagues (11,22). Calculation of this index involved summing compliance variables {each day participant’s monitoring of all foods eaten (at least 3 distinct entries) + any food eaten + any time recorded when food was eaten + any quantity of food eaten + any grams of fat consumed – not monitoring}. As our participants were asked to record red food servings rather than fat grams, the item “any grams of fat consumed” was replaced with “any red foods eaten.” Scores of the daily monitoring index ranged from −1 to + 5, based on a yes = 1/no = 0 scoring system for each of the index component questions. Weekly summary monitoring indexes were derived by totaling the daily index sums resulting in sums ranging from (−7 to +35) for each 7-day period. Average monitoring index was derived by calculating the mean weekly monitoring index across the 20-week intervention. Because this index scores component behaviors of self-monitoring, it was used to assess recording competency.
Recording compliance
A newer method was developed to evaluate the relation between total days of dietary self-monitoring compliance and weight loss by rating recording sufficiency (14). Each day was scored as sufficient if there were at least 5 separate food or beverage items recorded on five separate lines. This cut-off was chosen based on previous literature (23) suggesting that adolescents consume three meals and two snacks per day, allowing for the opportunity to log at least one item from each eating episode. As noted by Jahns and colleagues, there has yet to emerge consensus for defining what constitutes a meal or snack. Since the children in this study were of younger age (7–12 years), they did not always note time each food item was eaten so we were unable to determine whether a food item belonged to a meal or snack period. Percentage of days sufficiency was met (out of a possible 140 days) was used to measure compliance.
Perceived social support and self-efficacy for enacting dietary change. The Social Support and Eating Habits Survey and Social Support and Exercise (SSEHS/SSES) is a 43-item self-report questionnaire, used to assess both friend and family support for dietary and physical activity behaviors. The scale is considered valid for use in adults (24) and children (25). Summary variables available for analysis included child ratings of (i) family encouragement, (ii) family discouragement, (iii) friend encouragement, and (iv) friend discouragement of eating habit changes. Each summary subscale had a range of 5–25. Higher scores represented greater perceived social support to make eating habit changes. The Child Dietary Self-Efficacy Scale (CDSS) is a 15-item scale found to be valid and reliable (16,26) in measuring child self-efficacy in choosing healthy, low-fat food items instead of higher fat, higher calorie food items. The range of possible summary score was −15.0 to +15.0.
Body composition
Height and weight were measured at baseline and post-intervention. Height (in meters) was measured using a stationary stadiometer and weight (in kilograms) was measured using a calibrated balance beam scale. Body mass index (BMI) was calculated as weight/height2 (kg/m2). While BMI is considered a reliable and valid measure of adiposity among adults and adolescents (27), it is not the most accurate measure of change in children (28). Percentage overweight was calculated as the ratio of the child’s BMI to the 50th percentile BMI for children according to sex and age (28). The exact formula is as follows:
Statistical analyses
Diagnostic analyses
A series of preliminary descriptive analyses were conducted to examine distributional characteristics. No imputation of missing data was undertaken. No skewness or kurtosis necessitating transformation was found for self-monitoring scores, anthropometric measures, social support or self-efficacy summary measures or age.
Main analyses
Linear regression was used to evaluate the relation between change in percent overweight and self-monitoring, and to determine if recording competency or compliance differed by baseline perceived social support or dietary self-efficacy. Independent sample t-tests were used to determine if change in percent overweight differed by whether a child compliantly recorded on 50% or 75% of the intervention days and whether a child was above or below the median competency score of 13.4.
Finally, stepwise least squares linear regression was used to evaluate whether there was an association between dietary self-monitoring and change in percent overweight. Baseline percent overweight was entered at step 1 for each model, followed in step 2 by the dietary self-monitoring variable. The social support and self-efficacy variables were subsequently available for entry in the last step. Each model was adjusted for age, race/ethnicity (white/non-white), sex and SES.
Results
The participating children had a mean age at baseline of 9.9 years (SD = 1.3) and were predominantly female (69.9%). In our sample, 68.6% of children were Caucasian, 18.9% Hispanic, and 7.2% African-American. Children reported lower perceived encouragement from friends for enacting dietary change (mean = 7.8, range 5–25) compared to encouragement from family (mean = 16.3, range 5–25). Conversely higher perceived discouragement from friends (mean 11.4, range 5–25) was reported as compared to discouragement from parents (mean = 10.9, range 5–25). Mean baseline dietary self-efficacy score was −7.2 (range 7.0 to 15.0). The average number of days for which a child compliantly recorded was 70.2 days out of a possible 140 days (SD = 36.4) equaling a mean percent of 50.1 percent (SD = 25.9). The average recording competency across the 20-week intervention was 13.3 (SD = 10.2) out of a possible 35 (see Table I).
Mean percent overweight among children at baseline was 64.4% (SD = 18.5). At the end of the intervention, mean percent overweight was 53.5% (SD = 18.8), demonstrating a mean decrease of 10.9% (SD = 7.9). Using paired t-tests, statistically significant improvements were seen in perceived family encouragement (p < 0.001). A significant increase in perceived discouragement to make eating changes from friends was reported (p = 0.002). Children reported significant improvement in dietary self-efficacy ratings (p < 0.001) at the end of the intervention as well (see Table II).
Table 2.
Changes in outcome measures for 153 children aged 7–12 over the 20 week weight loss intervention, San Diego CA 1999–2002
| Baseline | Post Intervention | Change | t | df | p | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| n | Mean | (SD) | Mean | (SD) | Mean | (SD) | ||||
|
| ||||||||||
| Height, meters | 153 | 1.44 | 0.09 | 1.46 | 0.09 | 0.02 | 0.01 | 35.95 | 152 | <0.001 |
| Weight, kilograms | 153 | 58.17 | 12.42 | 56.65 | 12.68 | 1.54 | 2.79 | 6.85 | 146 | <0.001 |
| Body Mass Index (BMI) | 153 | 27.55 | 3.39 | 26.03 | 3.52 | 1.52 | 1.32 | 14.19 | 146 | <0.001 |
| BMI Z-Score* | 153 | 2.20 | 0.30 | 1.99 | 0.38 | 0.22 | 0.17 | 15.88 | 146 | <0.001 |
| Percent overweight | 153 | 64.39 | 18.49 | 53.49 | 18.75 | 10.91 | 7.92 | 17.04 | 146 | <0.001 |
| Social support survey for dietary behaviors | ||||||||||
| Family encouragement | 145 | 16.26 | 4.74 | 19.54 | 4.55 | 3.28 | 5.56 | −7.09 | 144 | <0.001 |
| Friend encouragement | 144 | 7.87 | 3.99 | 8.06 | 3.71 | 0.19 | 4.83 | −0.46 | 143 | 0.642 |
| Family discouragement | 142 | 10.93 | 4.09 | 10.73 | 4.31 | −0.21 | 5.41 | 0.47 | 141 | 0.642 |
| Friend discouragement | 141 | 11.35 | 4.70 | 12.85 | 4.39 | 1.49 | 5.37 | −3.31 | 140 | 0.001 |
| Dietary self-efficacy scale | 143 | 7.21 | 5.82 | 9.31 | 4.46 | 2.09 | 4.77 | 5.26 | 142 | <0.001 |
SD: Standard Deviation
Calculated using CDC LMS method and reference population
Linear regression was used to examine the relation between dietary self-monitoring and change in percent overweight. A significant inverse relation (p < 0.001) between self-monitoring and change in percent overweight was found, after controlling for baseline percent overweight. Children who recorded on more days (mean = 50.1%, SD = 25.9), indicating better compliance, had greater decreases in percent overweight (mean decrease = −10.9, SD = 7.9; adj R2 = 0.094, partial correlation = −0.276, p < 0.001) than those who recorded less frequently. Similarly, a significant inverse relation (p < 0.001) was found between average recording competency and change in percent overweight (mean = 10.9, SD = 7.9; adj R2 = 0.080, partial correlation = −0.247), controlling for baseline child percent overweight. Thus, children who had better recording competency had greater decreases in percent overweight than children with poorer recording competency.
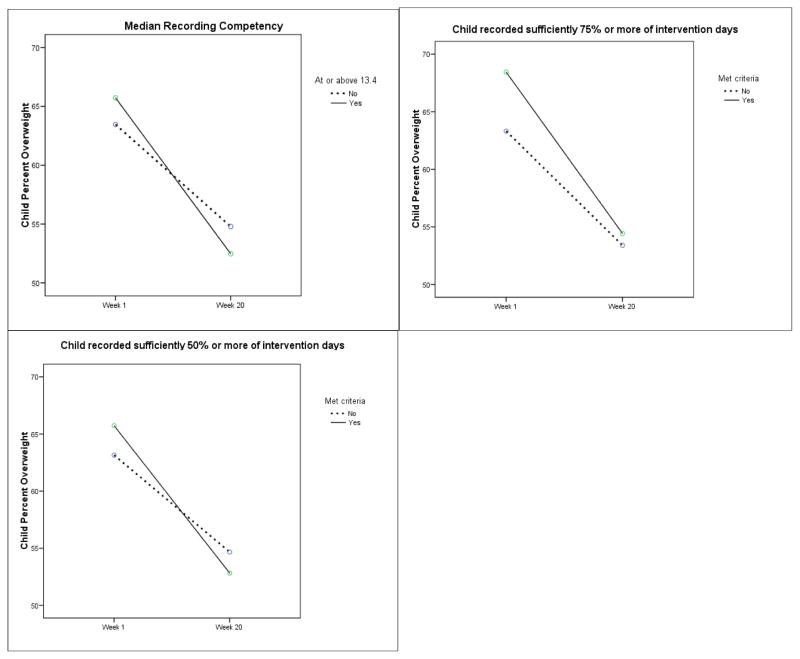
As shown in Table III, the decline in percent overweight was greater for children whose average recording competency was at or above the median of 13.4 (mean change: −13.4% vs. −0.6%; p < 0.001) than those who were below the median. Children who had higher compliance as measured by recording sufficiency on at least 70 days (50%) as compared to those who had inadequate recording had a significantly greater decrease in percent overweight (mean change: −13.0 vs. −8.4; p < 0.001). Those who were compliant on at least 105 days (75%) had even greater decreases in percent overweight as compared to the rest of the sample (mean change: −14.2% vs. −0.9%; p = 0.005). Generalized linear modeling was used to examine graphically the change in percent overweight by the aforementioned recording compliance or competency categories, adjusting for age, sex, baseline perceived social support and dietary self-efficacy (see Figure 1).
Table 3.
Changes in percent overweight from baseline to post-intervention by self-monitoring categories among 153 children aged 7–12, San Diego CA 1999–2002
| Yes | No | Mean Difference (SE) | df | t | P value | |||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| n | Mean Percent Overweight Change (SD) | n | Mean Percent Overweight Change (SD) | |||||
|
| ||||||||
| Recording competency | ||||||||
| At or above 13.4 (median) | 75 | −13.37 (7.85) | 78 | −8.56 (7.29) | 4.81 (1.22) | 151 | 3.93 | <0.001 |
| Recording compliance | ||||||||
| 50% of the days (70 days) | 83 | −13.02 (8.01) | 70 | −8.41 (7.09) | 4.61 (1.23) | 151 | 3.73 | <0.001 |
| 75% of the days (105 days) | 36 | −14.17 (6.56) | 117 | −9.91 (8.06) | 4.25 (1.47) | 151 | 2.88 | 0.005 |
SD: Standard Deviation; SE: Standard Error; df: Degrees of Freedom
Figure 1.
Change in percent overweight by recording sufficiency and monitoring index category among 153 children aged 7–12, San Diego, CA 1999–2002
Models adjusted for age, sex, baseline perceived social support and dietary self-efficacy.
It was hypothesized that higher baseline perceived social support for change and higher dietary self-efficacy, separately, might predict higher degree of dietary self-monitoring during weight loss treatment. In a regression model that included baseline percent overweight, age, sex, race/ethnicity and SES score, self-efficacy was not found to be related to percentage of days that recording sufficiency criteria were met (F = 0.84, df = 6, 135, p = 0.54). In a second regression model that included the four social support summary variables along with baseline percent overweight, age, sex, race/ethnicity and SES score, none were found to be related to recording sufficiency (F = 1.65, df = 9, 129, p = 0.11). Neither self-efficacy at baseline (F = 0.91, df = 6, 135, p = 0.49) nor perceived social support at baseline (F = 1.85, df = 9, 129, p = 0.07) were related to average weekly recording competency in regression models that included child baseline percent overweight and age.
Finally, multivariate regression models using either percentage of days recorded sufficiently (compliance) or average weekly recording competency to predict change in percent overweight, while adjusting for age, race/ethnicity, sex and SES as well as baseline percent overweight, social support and self-efficacy. Both recording compliance (Adj. R2 = 0.092, R2 change = 0.07, p = 0.001) and competency (Adj. R2 = 0.079, R2 change = 0.057, p = 0.004) were significantly related to change in child percent overweight for children participating in this weight loss intervention. Age and percent overweight at baseline, sex, race/ethnicity, SES, perceived social support to enact dietary change and dietary self-efficacy were not found to contribute significant additional explanation of the variance in child percent overweight change thus ending each model run at the 2nd step (see Table IV).
Table 4.
Linear regression models predicting change in percent overweight among 153 children aged 7–12, San Diego CA 1999–2002
| Model A | Variables included* | Unstandardized Beta | SE | t | p |
|---|---|---|---|---|---|
| Step 1 | Constant | −10.69 | 6.97 | −1.54 | 0.13 |
| Baseline percent overweight | −0.08 | 0.04 | −2.18 | 0.03 | |
| Age | 0.60 | 0.52 | 1.15 | 0.25 | |
| Sex | 1.83 | 1.48 | 1.24 | 0.22 | |
| Race/Ethnicity (Caucasian vs. all others) | −1.94 | 1.49 | −1.21 | 0.19 | |
| SES score | −0.02 | 0.06 | −0.29 | 0.77 | |
|
| |||||
| Step 2 | Constant | −9.28 | 6.79 | −1.37 | 0.18 |
| Baseline percent overweight | −0.07 | 0.04 | −1.96 | 0.05 | |
| Age | 0.61 | 0.51 | 1.20 | 0.23 | |
| Sex | 1.66 | 1.44 | 1.15 | 0.25 | |
| Race/Ethnicity (Caucasian vs. all others) | −1.22 | 1.48 | −0.82 | 0.4 | |
| SES score | 0.02 | 0.06 | −0.26 | 0.79 | |
| Average weekly recording competency | −0.19 | 0.07 | −2.92 | 0.004 | |
|
| |||||
| Model B | |||||
|
| |||||
| Step 1 | Constant | −10.69 | 6.97 | −1.54 | 0.13 |
| Baseline percent overweight | −0.08 | 0.04 | −2.18 | 0.03 | |
| Age | 0.60 | 0.52 | 1.15 | 0.25 | |
| Sex | 1.83 | 1.48 | 1.24 | 0.22 | |
| Race/Ethnicity (Caucasian vs. all others) | −1.94 | 1.49 | −1.21 | 0.19 | |
| SES score | −0.02 | 0.06 | −0.29 | 0.77 | |
|
| |||||
| Step 2 | Constant | −5.28 | 6.54 | −0.81 | 0.42 |
| Baseline percent overweight | −0.06 | 0.04 | −1.58 | 0.12 | |
| Age | 0.45 | 0.49 | 0.91 | 0.36 | |
| Sex | 2.43 | 1.36 | 1.79 | 0.08 | |
| Race/Ethnicity (Caucasian vs. all others) | −0.11 | 1.42 | −0.75 | 0.46 | |
| SES score | 0 | 0.06 | 0.08 | 0.94 | |
| Percentage of days recorded compliantly | −0.14 | 0.03 | −5.04 | <0.001 | |
SE: Standard Error
Variables excluded from stepwise regression include self-efficacy and social support baseline scores due to lack of significant contribution to explanation of variance in outcome.
Discussion
As demonstrated with adolescents and adults in previous studies (12,15), self-monitoring of dietary intake was found to be associated with significantly greater decreases in percent overweight in this population of children. We found no support, however, for the hypothesis that children who had greater dietary self-efficacy or perceived social support at baseline would have greater weight loss as defined as decrease in percent overweight. Despite several studies having found associations between social support or self-efficacy and weight change (16,17), inconsistent conclusions as to how well subjects can predict their outcomes are still seen (29). In this sample, perceived ability to make changes or perceived support for these changes were not related to how frequently (percentage of days recording sufficiency criteria was met) or how competently (average monitoring index) dietary intake was self-monitored.
Using food records, self-monitoring behavior was examined for competency and compliance. Calculation of the average weekly monitoring index was used as a measure of compliance over the 20-week intervention. While the participants were given semi-structured food records to complete each week, they were asked to record all component items of this index. The mean competency score among participants in this study was 13.3 (SD = 10.2). While possible average weekly competency could have ranged from −7 to 35, our participants had moderate to high competency and there was variability among the children. However, no equivalent studies using this index to rate child food records were located and thus comparison of results was not possible. Recording compliance was calculated as the percentage of days that at least five items were recorded in the food record. Children in our study met this criteria on average slightly more than half the time (mean = 50.1%) suggesting greater total compliance than was seen among adolescents in Saelens and McGrath’s study (the majority of their participants self-monitored 25% or the time or less) (14).
Along with good adherence to keeping the food records, significant decreases in percent overweight were related to level of self-monitoring, similar to previous research. As seen in Figure 1, average recording competency (average monitoring index at or above the median 13.4) and recording compliance category (at or above 50% of days or at or above 75% of days) were significantly related to change in child percent overweight.
Given the robust findings across age groups and studies, dietary self-monitoring should be considered an integral component of weight loss programs for children. Self-regulatory skills such as self-monitoring act by allowing an individual more aware of their behaviors (9). An individual will be more able to change behavior if self-aware and can visualize progress while making behavioral changes (10). Our participants were able to see the changes enacted in their diet by reviewing their weekly food journals. This tangible change is likely a motivator for change as they are readily seeing change and results tied to that change (weight loss). They would also be able to more readily make course corrections to counteract any negative weight change (gain or maintaining weight). This demonstrates the relation of self-monitoring to self-adjustment. Simple monitoring of behavior won’t elicit change (30). Individuals must evaluate changes made and whether these changes prompted the intended outcome. They likely would measure their achievement against a standard (for example, preferred weight status for their sex and height); comparison to a standard has been posited as an integral aspect of self-monitoring (31). Self-monitoring would have no value if the children had no outward goal to compare with their weight. They, along with their parent and counselor, identified their goal, then self-monitored to assess change and measured against desired weight status as part of the process of weight change. When the intended and perceived preferable outcome is achieved, this facilitates continued monitoring and evaluation. Compliance for monitoring dietary intake as measured by percentage of days achieving recording sufficiency may be a preferable therapeutic goal as it is potentially easier to achieve. Asking children to write down items consumed, rather than additionally asking them to record calories and red food servings may elicit greater adherence to self-monitoring. Baker and colleagues had found when constructing the monitoring index, it was the combination of those items as well as four other items better predicted weight loss and maintenance (22).
However, Saelens and McGrath found that number of items recorded, number of items for which amount or serving sizes were recorded and number of items for which calories were recorded were not significantly associated with weight loss or maintenance among adolescents in their study (14). It may be the action of writing items down rather than specifics about the items that acts as a behavioral prompt to adhere to the dietary recommendations of the intervention. These self-directed activities act in concert to facilitate change in the children’s behavior. Interventions should strive to promote completion of dietary monitoring record for at least 50% of the intervention period as this may be a more achievable goal for children during a weight loss program that could still lead to significant weight loss (15). They should also strive to provide a mechanism by which the participants can receive temporally proximal feedback of their progress as this will increase the opportunity for change (9).
Strengths of this study were that it had a larger sample size and younger age group than most studies evaluating predictors of weight loss in preadolescent children and that it looked to evaluate the interaction of social support and self-efficacy with self-monitoring in relation to weight loss among overweight children participating in a family-based weight loss intervention, something not prevalent in the literature (32–35).
The sample recruited for participation in this intervention was ethnically representative of the residents of San Diego County, a diverse and geographically-expansive locale (36). However, despite the recruited sample being ethnically diverse, the final sample had less ethnic diversity. Another limitation of this study may be that change in social support and self-efficacy were not directly targeted as part of the weight loss intervention, preventing a definitive conclusion regarding the lack of association between these baseline variables and adherence to self-monitoring. Though baseline values of these measures were excluded in the final model steps due to lack of significant relation to outcome, perceived social support and self-efficacy summary measures were found to have changed significantly over the course of the weight loss intervention (Table II). Analyses conducted using change in these measures rather than baseline values did not predict change in percent overweight. The change variables were excluded in stepwise regression just as in the previous models using baseline values.
While recording sufficiently on 75% or more days was associated with greater weight loss, participants were asked to complete a fairly detailed food record. Future research should focus on whether use of a more streamlined food record (excluding calorie counting and fat gram recording) would still demonstrate the same weight loss results in preadolescent children. We know that dietary self-monitoring is an integral part of these programs, but need to determine how to make it simpler for children to self-monitor while still achieving significant weight loss.
Acknowledgments
This research was supported by grant number 5 RO 1 HD 36904, awarded to Denise E. Wilfley, PhD, by the National Institute of Child Health and Human Development, Department of Health and Human Services.
Footnotes
Declaration of interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- Ogden CL, Carroll MD, Curtin LR, McDowell MA, Tabak CJ, Flegal KM. Prevalence of Overweight and Obesity in the United States, 1999–2004. JAMA. 2006;295:1549–55. doi: 10.1001/jama.295.13.1549. [DOI] [PubMed] [Google Scholar]
- Hedley AA, Ogden CL, Johnson CL, Carroll MD, Curtin LR, Flegal KM. Prevalence of overweight and obesity among US children, adolescents, and adults, 1999–2002. JAMA. 2004;291:2847–50. doi: 10.1001/jama.291.23.2847. [DOI] [PubMed] [Google Scholar]
- Eriksson J, Forsen T, Tuomilehto J, Osmond C, Barker D. Size at birth, childhood growth and obesity in adult life. Int J Obes. 2001;25:735–40. doi: 10.1038/sj.ijo.0801602. [DOI] [PubMed] [Google Scholar]
- Serdula MK, Ivery D, Coates RJ, Freedman DS, Williamson DF, Byers T. Do obese children become obese adults? A review of the literature. Prev Med. 1993;22:167–77. doi: 10.1006/pmed.1993.1014. [DOI] [PubMed] [Google Scholar]
- Fall CHD, Osmond C, Barker DJP, et al. Fetal and infant growth and cardiovascular risk factors in women. BMJ. 1995;310:428–32. doi: 10.1136/bmj.310.6977.428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Must A, Spandano J, Coakley EH, Field AE, Colditz GA, Dietz WH. The disease burden associated with overweight and obesity. JAMA. 1999;282:1523–9. doi: 10.1001/jama.282.16.1523. [DOI] [PubMed] [Google Scholar]
- Strauss RD, Pollack HA. Epidemic increase in childhood overweight 1986–1998. JAMA. 2001;286:2845–8. doi: 10.1001/jama.286.22.2845. [DOI] [PubMed] [Google Scholar]
- Prentice AM. The emerging epidemic of obesity in developing countries. Int J Epidemiol. 2006;35:93–99. doi: 10.1093/ije/dyi272. [DOI] [PubMed] [Google Scholar]
- Bandura A. Social cognitive theory of self-regulation. Organizat Behav Human Decis Processes. 1991;50:248–87. CrossRef, Web of Science® Times Cited: 392. [Google Scholar]
- Karoly P. Mechanisms of self-regulation: a systems view. Ann Rev Psychol. 1993;44:23–52. CrossRef, Web of Science® Times Cited: 229. [Google Scholar]
- Baker BC, Kirschenbaum DS. Weight control during the holidays: highly consistent self-monitoring as a potentially useful coping mechanism. Health Psychol. 1998;7:367–70. doi: 10.1037//0278-6133.17.4.367. [DOI] [PubMed] [Google Scholar]
- O’Neil PM. Assessing dietary intake in the management of obesity. Obes Res. 2001;5:373S–4S. [PubMed] [Google Scholar]
- Boutelle KN, Kirschenbaum KN. Further support for consistent self-monitoring as a vital component of successful weight control. Obes Res. 1998;63:219–24. doi: 10.1002/j.1550-8528.1998.tb00340.x. [DOI] [PubMed] [Google Scholar]
- Saelens BE, McGrath AM. Self-monitoring adherence and adolescent weight control efficacy. Children’s Health Care. 2003;322:137–52. [Google Scholar]
- Kirschenbaum DS, Germann JN, Rich BH. Treatment of morbid obesity in low-income adolescents: effects of parental self-monitoring. Obes Res. 2005;13:1529–1537. doi: 10.1038/oby.2005.187. [DOI] [PubMed] [Google Scholar]
- Edmundson E, Parcel GS, Feldman HA, et al. The effects of the Child and Adolescent Trial for Cardiovascular Health upon psychosocial determinants of diet and physical activity behavior. Prev Med. 1996;25:442–54. doi: 10.1006/pmed.1996.0076. [DOI] [PubMed] [Google Scholar]
- Vega WA, Sallis JF, Patterson TL, Rupp JW, Morris JA, Nader PR. Assessing knowledge of cardiovascular health-related diet and exercise behaviors in Anglo- and Mexican-Americans. Am J Prev Med. 1988;4:197–9. doi: 10.1016/0091-7435(87)90052-1. [DOI] [PubMed] [Google Scholar]
- Reynolds KD, Yaroch AL, Frankin FA, Maloy J. Testing mediating variables in a school-based nutrition intervention program. Health Psychol. 2002;211:51–60. [PubMed] [Google Scholar]
- Wilfley DE, Stein RI, Saelens BE, et al. The efficacy of maintenance treatment approaches for childhood overweight. JAMA. 2007;298:1661–1673. doi: 10.1001/jama.298.14.1661. [DOI] [PubMed] [Google Scholar]
- Epstein LH, Wing RR, Koeske R, Valoski A. A comparison of lifestyle exercise, aerobic exercise, and calisthenics on weight loss in obese children. Behav Ther. 1985;16:345–56. CrossRef, Web of Science® Times Cited: 116. [Google Scholar]
- Hollingshead AB. Four factor index of social status. New Haven: Yale University; 1975. [Google Scholar]
- Baker RC, Kirschenbaum DS. Self-monitoring may be necessary for successful weight control. Behav Ther. 1993;24:377–394. [Google Scholar]
- Jahns L, Siega-Riz AM, Popkin BM. The increasing prevalence of snacking among US children from 1977 to 1996. J Pediatrics. 2001;138:493–8. doi: 10.1067/mpd.2001.112162. [DOI] [PubMed] [Google Scholar]
- Sallis JF, Grossman RM, Pinski RB, Patterson TL, Nader PR. The development of scales to measure social support for diet and exercise behaviors. Prev Med. 1987;16:825–36. doi: 10.1016/0091-7435(87)90022-3. [DOI] [PubMed] [Google Scholar]
- Pietrobelli A, Leone MA, Heymsfield SB, Faith MS. Association of physical-activity-teasing with reported activity and activity-attitudes in pediatric sample. Int J Obes. 1998;22:S8. [Google Scholar]
- Parcel GS, Edmundson E, Perry CL, et al. Measurement of self-efficacy for diet-related behaviors among elementary school children. J Sch Health. 1995;65:23–7. doi: 10.1111/j.1746-1561.1995.tb03335.x. [DOI] [PubMed] [Google Scholar]
- Dietz WH, Robinson TN. Use of the body mass index BMI as a measure of overweight in children and adolescents. J Pediatrics. 1998;132:191–3. doi: 10.1016/s0022-3476(98)70426-3. [DOI] [PubMed] [Google Scholar]
- Cole TJ, Faith MS, Pietrobelli A, Heo M. What is the best measure of adiposity change in growing children: BMI, BMI %, BMI z-score or BMI centile? Eur J Clin Nutrit. 2005;59:419–25. doi: 10.1038/sj.ejcn.1602090. [DOI] [PubMed] [Google Scholar]
- White MA, Martin PD, Newton RL, et al. Mediators of weight loss in a family-based intervention presented over the internet. Obes Res. 2004;127:1050–9. doi: 10.1038/oby.2004.132. [DOI] [PubMed] [Google Scholar]
- Kanfer FH, Karoly P. Self-control: a behavioristic excursion into the lion’s den. Behav Ther. 1972;3:398–416. [Google Scholar]
- Baumeister RF, Vohs KD. Self-regulation, ego depletion, and motivation. Soc Personal Psychol Compass. 2007;1:115–28. [Google Scholar]
- Braet C. Patient characteristics as predictors of weight loss after an obesity treatment for children. Obesity. 2006;14:148–55. doi: 10.1038/oby.2006.18. [DOI] [PubMed] [Google Scholar]
- Epstein LH, Paluch RA, Raynor HA. Sex differences in obese children and siblings in family-based obesity treatment. Obes Res. 2001;9:746–53. doi: 10.1038/oby.2001.103. [DOI] [PubMed] [Google Scholar]
- Stein RI, Epstein LH, Raynor HA, Kilanowski CK, Paluch RA. The influence of parenting change on pediatric weight control. Obes Res. 2005;13:1749–55. doi: 10.1038/oby.2005.213. [DOI] [PubMed] [Google Scholar]
- Wrotniak BH, Epstein LH, Paluch RA, Roemmich JN. The relationship between parent and child self-reported adherence and weight loss. Obes Res. 2005;13:1089–96. doi: 10.1038/oby.2005.127. [DOI] [PubMed] [Google Scholar]
- U.S. Census Bureau. Demographic comparison data – US, California and San Diego. Available at the SANDAG website: http:www.sandag.orgresourcesdemographics_and_other_datademographicscensuspdfsprofiles_may02.pdf.